Abstract
Objective
Given the increase in narcotic addiction and diversion, understanding how patients use their opioid prescriptions and store or dispose of any remainders is important. We set out to determine the frequency in which patients had leftover opioid quantities from prescriptions received in the emergency department (ED). In addition, we sought to describe patients’ reasons for taking or not taking all of their prescribed medications and their strategies to manage and/or dispose of any excess or leftovers.
Methods
This cross‐sectional study took place at an academic center in an urban environment in mid‐Missouri with an annual emergency department volume of 55,000 patients. Potential participants were identified using a patient discharge prescription log and consisted of adult patients who received opioid prescriptions. A single researcher recruited participants via phone and invited them to participate in the study by completing a short phone survey.
Results
The discharge log included 301 patient encounters; of those, 170 potential participants were successfully contacted by phone and 89 agreed to participate in the survey. A majority of the participants indicated that they did not take the full prescription amount. Only 4.1% of participants disposed of their leftover opioids according to U.S. Food and Drug Administration recommendations. Those who did not dispose of their leftover opioids most frequently stored their remaining medication in a medicine cabinet or box, and a majority (77%) indicated that this storage location was unlocked.
Conclusions
A majority of patients discharged from the emergency department have leftover opioids, and almost all of these leftover medications were not disposed of or stored in compliance with US Food and Drug Administration recommendations. Future research to determine what interventions could increase proper storage and disposal of leftover opioids is recommended.
Keywords: disposal, narcotics, opioids, prescriptions
1. INTRODUCTION
1.1. Background
The number of opioid prescriptions dispensed by retail pharmacies in the United States has nearly tripled in the past 30 years, increasing from 79 million total prescriptions in 1991 to 217 million total prescriptions in 2012. 1 Some attribute this to the American Pain Society's 1995 recommendation to add pain as the fifth vital sign. 2 Others cite the 2000 congressional approval of House Resolution 3244, Section 1603 that preempted the “decade of pain control and research” or The Joint Commission's 2001 release of standards for pain management. 3 , 4
With this rise in opioid prescribing, there has been an unfortunate rise in overdoses and death. 5 In 2017, the odds of dying from an accidental overdose were 1 in 96, the fifth most likely cause of death. 6 This surpassed the odds of dying in a motor vehicle collision or fall, which were 1 in 103 and 1 in 114, respectively. 6
A systematic review of studies describing opioid oversupply after adult surgical procedures found that 67% to 92% of patients reported unused opioids. 7 In another study, patients discharged after caesarean section and thoracic surgery were surveyed; it was found that 53% of postoperative caesarean‐section patients reported taking none or <5 prescribed pills, whereas only 17% reported taking all or nearly all of their prescribed amount. 8
In efforts to improve safety, the US Food and Drug Administration (FDA) and medical specialty organizations have made recommendations on the storage and disposal of opioids. 9 , 10 The mainstay of these recommendations is to dispose of unused medications following an approved disposal technique. If such disposal is not possible, then recommendations are to store medications in a locked cabinet where they are not easily accessible to children or others who might use them inappropriately. It has been reported that after surgical procedures, adults reported low compliance with these recommendations. 7
1.2. Importance
In the emergency department (ED) setting, the overall number of opioid prescriptions has decreased between 2005 and 2015 in all age groups. 11 However, despite these declines, approximately 1 in 10 ED patients nationwide received an opioid prescription. 11 A recent large‐scale, retrospective study found that 25% of ED patients treated for ankle sprains received an opioid prescription with a median of 15 tablets. 12 It was also found that patients receiving more opioids at discharge had higher rates of prolonged use after 30 days. 12 To our knowledge, there have not been studies similar to those discussed previously in the ED setting. This investigation aims to characterize the prevalence of leftover opioids as well as patient management strategies for leftover medications in our specialty.
1.3. Goals of this investigation
Our primary goal was to determine the frequency in which patients had leftover opioids from prescriptions received in the ED. Additional goals included describing patients’ reasons for taking or not taking all of their prescribed medications and their strategies to manage any excess or leftover medications.
2. METHODS
2.1. Study design and setting
This cross‐sectional study took place at an academic center in an urban environment in mid‐Missouri with an annual ED volume of approximately 55,000 patients. The study was approved by the local institutional review board with a waiver of documentation of consent.
The Bottom Line
Leftover opioids are potential contributors to misuse and overdose. A recent survey of emergency department patients discharged with opioid prescriptions found that only 4% disposed of leftover medicine appropriately, with most (77%) storing unfinished medication unlocked.
A previously validated survey tool was unavailable for use in this study. However, the previously published survey by Bartels et al 8 was evaluated by study investigators and determined to be suitable for the population and purpose of our study. The survey instrument was implemented as previously published and consisted of 7 questions 7 (Figure 1). The respondents could select multiple answers to questions if applicable.
FIGURE 1.
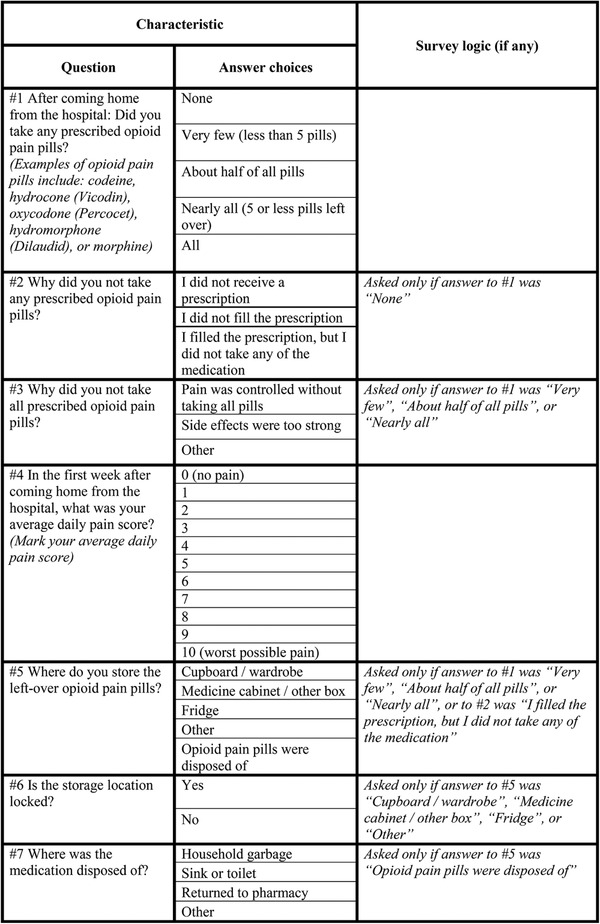
The survey instrument was designed to determine participant use, storage, and disposal of opioid medication (from Bartels et al 7 )
2.2. Participant selection, recruitment, and consent
Potential participants were identified using an ED patient discharge prescription log and consisted of adult patients who received 1 or more opioid prescriptions between May 2018 and July 2018. Nurses identified patients who were discharged with a prescription for an opioid, and the patient's visit number was recorded to identify pertinent contact information in the electronic medical record. Participants were excluded if they were younger than 18 years of age, did not have correct contact information documented in the electronic medical record, did not speak English as a primary language, or were deceased. Participants did not receive compensation for their participation in this study.
A single researcher (C.Y.) recruited participants via phone and invited them to participate in the study by completing a short phone survey. The waiver of documentation of consent was read aloud, and all questions were addressed to each participant's satisfaction. If a participant could not be reached, a voicemail recording was left whenever possible. The voicemail script included the reason for our call, provided a callback date and time, and provided a contact number if the patient preferred not to participate or receive further phone calls about the study (Appendix 1). Contact with each participant was attempted at least once during morning hours, once during afternoon hours, and once during evening hours as well as once on a weekend day. All calls were made from an institutional number. A maximum of 5 attempts were made to contact each potential participant.
After completion of the survey, the electronic medical record was reviewed for prescription data (which included medication, dose, quantity, and days of supply), initially reported pain scores in the ED, and potential follow‐up data with either a primary care or specialist physician, physician assistant or nurse practitioner.
2.3. Statistics and analysis
All potential participants within the defined timeframe were attempted to be contacted. Statistical analyses were performed by analysis of variance with Tukey post hoc testing for multiple comparisons using GraphPad (La Jolla, CA) Prism 7 software. A Kruskal‐Wallis test for multiple comparisons using Dunn's post hoc testing was performed to compare the average pain score to the percentage of prescription taken. Two‐sided P values < 0.05 were considered significant.
3. RESULTS
3.1. Characteristics of study participants
The ED patient discharge prescription log identified 301 eligible participants. Of those, 170 potential participants were successfully contacted by phone, whereas the remainder either met 1 of the aforementioned exclusion criteria or were not able to be contacted after 5 attempts. A total of 89 participants agreed to participate in the survey (Figure 2). These surveyed participants included 43 men and 46 women who had a mean age of 51.9 years. The majority of these participants (91%) had an emergency severity index triage acuity that was 1, 2, or 3. One patient who elected to enroll in this study received opioid prescriptions on more than 1 visit to the ED during the enrollment period. On callback, the patient elected to respond to the survey in the context of his or her original visit.
FIGURE 2.
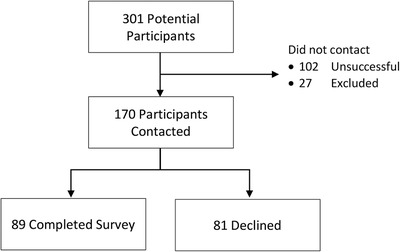
Flow diagram showing patient enrollment
3.2. Leftover opioids
A majority of the participants indicated that they did not take the full prescription amount (Table 1). Participants who did not take all of their prescribed opioid prescription selected adequate pain control as the main reason for not finishing the prescription. Other reasons for not finishing their prescription included adverse side effects, concerns of developing an opioid addiction, and alternative pain management prescribed by either a primary care physician or a specialist. Participants who reported taking none of their prescription either denied receiving a prescription, did not fill their prescription, or filled their prescription, but did not taken any of the medication (Table 1).
TABLE 1.
Survey responses to opioid prescription action questions
| Questions/responses | Respondents, n (%) |
|---|---|
| 1. Did you take any prescribed opioid medication? | |
| None | 13/89 (14.6) |
| About 25% | 20/89 (22.5) |
| About 50% | 12/89 (13.5) |
| About 75% | 12/89 (13.5) |
| All | 32/89 (36.0) |
| 2. Why did you not take any prescribed opioid medication? | |
| Denies receiving prescription | 4/13 (30.8) |
| Received but did not fill prescription | 5/13 (38.5) |
| Filled but did not take prescription | 4/13 (30.8) |
| 3. Why did you not take all prescribed opioid pain medication? | |
| Pain was controlled a | 29/44 (65.9) |
| Adverse side effects a | 11/44 (25.0) |
| Other | 9/44 (20.5) |
respondents selected both pain was well controlled and adverse side effects. These respondents are included in both groups.
Participants were asked to rate their average daily pain score in the first week after discharge on a scale ranging from 0 (no pain) to 10 (worst possible pain; Figure 3). The median reported pain score was 7, and the most frequently reported pain score was 8. A Kruskal‐Wallis test for multiple comparisons using Dunn's post hoc testing was performed to compare average pain score to percentage of prescription taken. Participants who reported a lower average pain rating were more likely to take fewer or none of their prescription (Figure 4).
FIGURE 3.
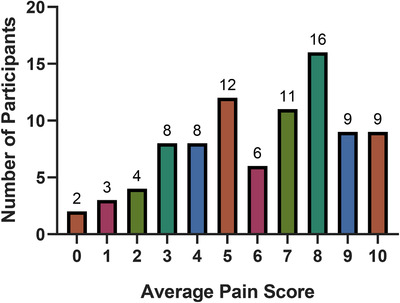
Self‐reported average daily pain score in the first week after discharge ranging from 0 (no pain) to 10 (worst possible pain). One participant refused to answer this question
FIGURE 4.
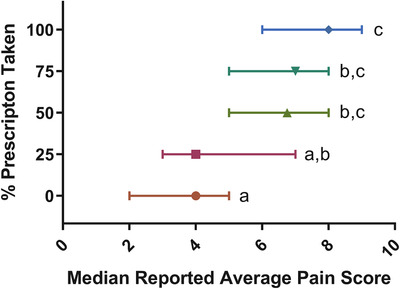
Kruskal‐Wallis test (P < 0.01) using Dunn's post hoc testing comparing average self‐reported pain during the first week to percentage of prescription taken displayed as median with interquartile range. Letter distinctions indicate significant differences among groups after post hoc testing
Participant ages ranged from 20 to 82, with an average age of 51.9 years and a median age of 55 years. It was found that those between ages 60 and 70 were most likely to have leftover prescription amounts; only 17% of respondents in this age group reported that they took all of their prescribed medication, whereas 76% of respondents reported that they took half or less of their total prescription. In addition, prescriptions in this age range had an average total milligram morphine equivalent of 99.0. This was higher than the average milligram morphine equivalent among all age groups of 90.4 and was the second highest among all decades of life examined.
3.3. Storage and disposal methods
Respondents who did not finish their entire prescription were asked about storage and/or disposal methods of their leftover medications. This included the 44 study participants who took some, but not all, of their prescribed opioid medication, and the 4 study participants who filled their prescription, but did not take any of the medication.
Only 2 participants (4.2%) responded that they returned their excess medication to a pharmacy or police station (Table 2). Participants who reported that they did not dispose of their prescription most frequently stored their remaining medication in a medicine cabinet or box. A majority indicated that this storage location was unlocked (Table 2). Other storage locations included a cupboard, in a purse, or in a safe. Participants who disposed of their medication most frequently did so by putting their medications into either the sink or the toilet. Other disposal methods included dissolving the excess pills in acid.
TABLE 2.
Survey responses to opioid prescription storage and disposal questions
| Questions/responses | Respondents, n (%) |
|---|---|
| 5. Where do you store the leftover opioid pain medication? | |
| Cupboard | 6/48 (12.5) |
| Medicine cabinet/box a | 27/48 (56.3) |
| Fridge | 0/48 (0) |
| Other | 2/48 (4.2) |
| Disposed a | 14/48 (29.2) |
| 6. Is the storage location locked? | |
| Yes | 7/35 (20) |
| No | 27/35 (77.1) |
| No response | 1/35 (2.9) |
| 7. Where was the medication disposed of? | |
| Garbage | 3/14 (21.4) |
| Sink or toilet | 6/14 (42.9) |
| Returned to pharmacy or police station | 2/14 (14.3) |
| Other | 3/14 (21.4) |
One respondent reported disposing of some pills and storing the remainder in a cabinet.
Participants between the ages of 40 and 60 were the least likely to dispose of their leftover medications. Only 18.2% of participants in this age range disposed of their medications versus 25.5% of participants among all ages.
In an effort to evaluate if participants had adequate pain control, the electronic medical record was reviewed for additional visits and prescriptions. A total of 33 participants reported an average pain score of 8 or more during the first week after discharge. Of these participants, only 3 (9%) returned to the ED within 2 weeks for additional pain management. Of these 33 participants, 7 (21%) received neither a refill nor a new prescription for an opioid pain medication during their scheduled follow‐up; most often these participants’ physicians noted that the participants had adequate pain control with over‐the‐counter medications. Of these participants, 4 (12%) were lost to follow‐up. The remainder of participants received another opioid prescription and/or refill during their scheduled follow‐up visit.
When examining all participants regardless of average pain score, 8 of the 87 participants (9%) returned to the ED within 2 weeks for additional pain management. Only 26 of the 87 participants (30%) followed up with either their primary care physician or a specialist after their discharge.
4. LIMITATIONS
Our study's participation rate, 29.5% of the potential sample, creates the possibility for selection bias. This participation rate is similar to what has been reported by other studies examining leftover opioid prescriptions. 8 , 11 Respondents may have differed from non‐respondents in their average pain after discharge, use of their opioid prescription, and storage and disposal methods. Further potential for selection bias is introduced in that only patients who provided a valid contact number during ED registration could be reached and enrolled in this study. Each potential participant was attempted in the morning, afternoon, and evening as well as during weekdays and weekends to reduce the potential for work or lifestyle availability to create selection bias. Enrolling patients before discharge, procurement of multiple contact numbers, or the ability to send out a letter or email survey for participants who were not successfully reached via phone to complete could be implemented in future studies to further decrease this bias.
In addition, participants may have had recall bias regarding their average pain and their opioid use given the length of time between their discharge from the ED and their enrollment in this study. Patients were called within a month of their discharge date to minimize this bias. Further efforts to minimize this bias in future studies may include enrolling patients and establishing a follow‐up phone call time before discharge from the ED.
Our study design was based on convenience sampling and nurse participation. The eligible participants may not represent all patients discharged within the enrollment period with a prescription for an opioid.
Data were collected between May and July and may be not be representative of annual trends.
We realize that this sample population may therefore not represent global opioid prescription and patient use from our ED.
Follow‐up data are based on information available in our health system's electronic medical record, and patients could have had additional medical contact outside of our system. Patients who had recent visits before the study start date were included and may represent a repeat or follow‐up visit.
Patients were contacted based on receiving a medication classified as an opioid, not based on medical indication. Therefore, patients could have received an opioid for a non‐pain indication (eg, cough).
Although used in other disciplines to evaluate patient opioid use, the survey instrument has not been validated.
5. DISCUSSION
Our objectives were to characterize leftover opioid quantities from the ED and patient strategies to manage these leftovers. Approximately two‐thirds of the participants discharged from the ED with a prescription for an opioid narcotic did not use all of their prescription. More than 95% of participants did not dispose of their leftover medications per FDA recommendations.
These results are consistent with literature from other specialties and showed that most patients used fewer amounts of opioid prescriptions than originally prescribed. 8 , 11 Adequate pain control was the most frequently cited reason for patients not taking their entire prescription; however, patients electing to terminate their continued pain management with opioids as a result of side effects may or may not have had their pain adequately controlled with the originally prescribed amount. Further evidence in our study showed strong statistical associations between average pain within the first week of discharge and the percentage of prescription taken. Additional research is needed to identify patient or injury characteristics that correlate with an increased prescription quantity.
The quantity of tablets taken was used as a surrogate measure for adequate pain control. To further evaluate if patients had adequate pain control, the electronic medical record was reviewed for additional visits and prescriptions. For patients with the most profound reported pain a week after discharge, <10% of patients returned to the ED within 2 weeks for additional acute pain management. Therefore, the majority of patients with the most profound pain were able to manage their acute pain crisis with the medications prescribed in the ED and appropriately follow‐up with their primary care physician or consulting service for continued pain management. This is consistent with the policy statement of the American College of Emergency Physicians on acute pain management in the ED with regard to prescribing opioids in the lowest effective dose for the shortest reasonably practical course and in only the minimal amount needed for a reasonable follow‐up interval. 13
Concerning findings that were reported in other studies include the limited use of secured storage locations for the opioids. A previous pilot study in North Carolina found that no participants among the 20 ED patients surveyed properly stored their opioid medications. 14 Keeping opioids unsecured increases the risk of diversion, theft, or abuse. National Survey on Drug Use and Health data from 2013 and 2014 show that approximately 65% of all abused prescription pain relievers come from a known friend or relative. 15 A 2019 investigation showed that opioid prescriptions to family members were associated with overdose among individuals who did not receive opioid prescriptions. 16
Current FDA recommendations are to return leftover pain medications to an authorized permanent collection site, such as a retail pharmacy, hospital, clinic, or law enforcement facility. 17 If such a take‐back program does not exist, the FDA recommends storing the leftover opioids in a locked cabinet. 17 Standardized discharge medication paperwork from our hospital electronic medical record includes information that encourages patients to ask their pharmacist about locating a drug take‐back program. Despite these recommendations, fewer than 1 in every 20 leftover prescriptions were returned to a take‐back program. One suggestion to improve compliance with proper storage is greater communication with patients on these important practices during the discharge process. Several of our participants inquired about proper disposal methods and were unaware of these take‐back programs, further suggesting that patient education may be key in improving adherence to FDA recommendations. Patient education efforts may be most useful for those between the ages of 40 to 60 as they are the least likely to dispose of their leftovers in any manner.
Similar to other studies looking at opioid prescriptions in the outpatient setting, this study showed that most patients used fewer amounts of opioid prescriptions to adequately control their pain than originally prescribed from the ED. 8 , 11 Most patients did not dispose of or store their leftover medication in compliance with FDA recommendations. Further studies examining prescription quantities and amounts of leftover medications in relationship to acuity of initial presentation or other patient characteristics may encourage more judicious prescription habits in the ED setting. Future research to determine what interventions, such as patient education regarding proper return and disposal of unused opioid medications, could serve to decrease the potential for future abuse and misuse is recommended.
CONFLICT OF INTEREST
The authors report no conflicts of interest.
AUTHOR CONTRIBUTIONS
Christopher Yang, Julie A.W. Stilley, Starr‐Mar'ee C. Bedy, Kara B. Goddard, and Christopher S. Sampson contributed to the design and implementation of the research. Julie A.W. Stilley conducted all statistical analysis. Christopher Yang wrote the manuscript with support from Kara B. Goddard, Julie A.W. Stilley, and Christopher S. Sampson. All authors discussed the results and contributed to the final manuscript.
Biography
Christopher Sampson, MD, is an Associate Clinical Professor of Emergency Medicine and Director of Education and Clinical Research at the University of Missouri–Columbia.
APPENDIX 1. UNSUCCESSFUL CONTACT VOICEMAIL SCRIPT
1.1.
“Hello, my name is _____. I am a researcher with the Department of Emergency Medicine at the University of Missouri calling to invite you to participate in a short phone survey about medications prescribed to you during a recent visit. I am sorry I was unable to reach you at this time. I or another member of our research team will be calling you again on _____ (example: Monday, April 9th at 6:00 pm). If you prefer not to participate or receive further phone calls about this survey, please call [Department Main Number].”
Yang C, Stilley JAW, Bedy S‐MC, Goddard KB, Sampson CS. Leftover narcotic analgesics among emergency department patients and methods of disposal. JACEP Open 2020;1:1486–1492. 10.1002/emp2.12161
Prior presentations: Abstract, American Academy of Emergency Medicine Scientific Assembly, March 2019.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Christian A. Tomaszewski, MD, MBA.
REFERENCES
- 1. Baker DW. The Joint Commission's pain standards: origins and evolution. https://www.jointcommission.org/assets/1/6/Pain_Std_History_Web_Version_05122017.pdf. Published 2017. Accessed November 8, 2018.
- 2. Campbell J. APS 1995 presidential address Speech presented at the 14th Annual Scientific Meeting of the American Pain Society. Los Angeles, CA; 1995. https://www.jpain.org/article/S1082-3174(96)80076-6/abstract. Accessed March 1, 1996. [Google Scholar]
- 3. Victims of Trafficking and Violence Protection Act of 2000, HR 3244, S 1603, 106th Cong (2000). [Google Scholar]
- 4. Joint Commission on Accreditation of Healthcare Organizations . Pain standards for 2001. https://www.jointcommission.org/assets/1/6/2001_Pain_Standards.pdf. Published 2001. Accessed November 8, 2018.
- 5. CDC . WONDER [database online]. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. Accessed February 26, 2020. [Google Scholar]
- 6. National Safety Council. Injury facts. https://injuryfacts.nsc.org/all-injuries/overview/. Accessed January 15, 2019.
- 7. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery. JAMA Surgery. 2017;152 (11):1066‐1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS One. 2016;11(1):e014972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Society of Regional Anesthesia and Pain Medicine. Safe opioid storage, tapering, and disposal. https://www.asra.com/page/2725/safe-opioid-storage-tapering-and-disposal. Accessed January 29, 2019.
- 10. American Academy of Family Physicians. Promote safe storage and disposal of opioids and all medications. https://www.aafp.org/dam/AAFP/documents/patient_care/pain_management/safe-storage.pdf. Accessed January 29, 2019.
- 11. Marra EM, Mazer‐Amirshahi M, Mullins P, Pines JM. Opioid prescribing in older adults in U.S emergency departments. WestJEM. 2018;19(4):678‐688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Delgado MK, Huang Y, Meisel Z, Yokell M, Polsky D, Perrone J. National variation in opioid prescribing and risk of prolonged use for opioid‐naïve patients treated in the emergency department for ankle sprain. Ann Emerg Med. 2018;72(40):389‐400.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. American College of Emergency Physicians . Policy Statement. Optimizing the Treatment of Acute Pain in the Emergency Department. April 2017. https://www.acep.org/globalassets/new-pdfs/policy-statements/optimizing-the-treatment-of-acute-pain-in-the-ed.pdf. Accessed December 11, 2019.
- 14. Tanabe P, Paice JA, Stancati J, Fleming M. How do emergency department patients store and dispose of opioids after discharge? A pilot study. J Emerg Nurs. 2012;38(3):273‐279. [DOI] [PubMed] [Google Scholar]
- 15. Lipari RN, Hughes A. How people obtain the prescription pain relievers they misuse. https://www.samhsa.gov/data/sites/default/files/report_2686/ShortReport-2686.html. Accessed December 11, 2019. [PubMed]
- 16. Khan NF, Bateman BT, Landon JE, Gagne JJ. Association of opioid overdose with opioid prescriptions to family members. JAMA Intern Med. 2019;179(9):1186‐1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Food and Drug Administration . Disposal of unused medications: what you should know. https://www.fda.gov/drugs/resourcesforyou/consumers/buyingusingmedicinesafely/ensuringsafeuseofmedicine/safedisposalofmedicines/ucm186187.html. Accessed January 29, 2019.


