Abstract
During the COVID‐19 pandemic, one of the major changes that has occurred in emergency medicine is the evolution of telemedicine. With relaxation of regulatory and administrative barriers, the use of this already available technology has rapidly expanded. Telemedicine provides opportunity to markedly decrease personal protective equipment (PPE) and reduce healthcare worker exposures. Moreover, with the convenience and availability of access to medical care via telemedicine, a more fundamental change in healthcare delivery in the United States is likely. The implementation of telemedicine in the emergency department (ED) in particular has great potential to prevent the iatrogenic spread of COVID‐19 and protect health care workers. Challenges to widespread adoption of telemedicine include privacy concerns, limitation of physical examination, and concerns of patient experience. In this clinical review, we discuss ED telemedicine applications, logistics, and challenges in the COVID‐19 era as well as recent regulatory and legal changes. In addition, examples of telemedicine use are described from 2 institutions. Examples of future applications of telemedicine within the realm of emergency medicine are also discussed.
Keywords: COVID‐19, emergency department, emergency medicine, healthcare worker, personal protective equipment, telecommunication, telehealth, telemedicine
1. INTRODUCTION
The terms “telemedicine” and “telehealth” are often used interchangeably. Some organizations have applied the term telehealth to describe broader use of technology beyond physician clinical encounters, for which telemedicine has been the preferred term. 1 However, there is much overlap in general. According to the American Telemedicine Association, the terms are synonyms and both refer to “use of remote health care technology to deliver clinical services.” 2 In addition, Centers for Medicare and Medicaid Services (CMS) states “Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from 1 site to another through electronic communication to improve a patient's health.” 3 As such for this report, the terms will be considered synonymous.
Telemedicine adaptation in the emergency department (ED) has been a slow process in the United States even though the technology has been available for decades. Factors impeding the adoption of telemedicine have included reluctance of the medical community to adapt to new technology, governmental regulation, and lack of financial incentive or reimbursement for use of telemedicine. 4 In the ED in particular, telemedicine has not been accepted for widespread use beyond a few specific applications. Telestroke, for example, has been used in EDs since the 1990s. 5 This modality is often used in critical access hospitals where neurology stroke specialists are lacking. The COVID‐19 pandemic has significantly expanded the opportunity for EDs to use telemedicine because of need and has been aided by significant changes in regulations and billing.
The COVID‐19 pandemic has presented unique challenges to the healthcare system in the United States. Specifically, lack of personal protective equipment (PPE) has been an issue. On April 9, 2020, the US Food and Drug Administration confirmed that some distributors have placed certain types of PPE on allocation and has issued surgical mask and gown conservation strategies to healthcare organizations. 6 The Centers for Disease Control and Prevention (CDC) has even recommended the use of a home bandana or scarf as a last resort. 7 In addition, the risk to healthcare workers of contracting COVID‐19 is real. Considering their close contact with the COVID‐19 patients and repeated exposure, the “front‐line” providers in the ED are at especially high risk. Twenty‐nine percent of the initial patients in Wuhan, China were healthcare workers. 8 In addition, of the initial 77,262 patients infected with COVID‐19 in China, 3387 were healthcare workers (4.4%), and of these, 23 died with median age of 55 years (range, 29–72). 9 In Italy, 20% of healthcare professionals were infected and some died. 10 The most recent estimates report at least 9282 COVID‐19 cases in healthcare workers in the United States. 11
Telemedicine is an important tool that has been proposed to both protect healthcare workers and save PPE. 12 By limiting as many points of contact as possible, all professionals who interact with ED patients could benefit, including registration personnel, nurses, social workers, advanced practice providers (APP), and language translators. In addition, the extensive regulatory changes regarding telemedicine use in the United States present EDs with the opportunity to explore new adaptations of the technology. If changes are made permanent, emergency medicine healthcare delivery will need to rapidly adjust to the changing digital landscape and integrate telemedicine into routine care moving forward.
2. TELEMEDICINE APPLICATIONS
Prior to the COVID‐19 global pandemic, telemedicine in the United States had primarily been deployed to improve patients’ access to specialist care and decrease time to decisionmaking in critical illness. Telecommunication for the provision of medical care has been evolving since its first implementation during an earthquake in Armenia in the late 1980s. 13 Many emergency physicians are familiar with telemedicine from its application to care sites without physical specialist coverage. Telemedicine has been effectively implemented to improve burn and trauma transfer decisions, 14 rural trauma care, 15 acute myocardial infarction management in atypical cases, 16 acute stroke care, 17 and ultrasound applications. 18
The COVID‐19 global pandemic presents unique challenges to the US healthcare system and to emergency physicians managing patients. Hospital systems need to develop infection prevention and disaster preparedness plans with minimal guidance and maximal urgency. This is further compounded by the nationwide and worldwide shortage of appropriate PPE. In an effort to reduce healthcare worker exposure to infected patients, limit consumption of PPE, and protect vulnerable healthcare workers, multiple applications for telemedicine have been identified (Table 1).
TABLE 1.
Emergency department applications for telemedicine
| Location | Applications |
|---|---|
| Triage |
1. Initial intake 2. Entirety of physician interaction with lowest acuity patients 3. Disposition planning and result discussion |
| Supervision of residents or advanced practice providers |
1. Discussion of patient care plans 2. Direct patient contact 3. Supervision of low risk procedures 4. Disposition planning |
| Respiratory isolation area |
1. Initial patient evaluation 2. Healthcare workers with mild illness 3. Supervision of non‐emergentologists 4. Reassessment of patients 5. Disposition planning |
2.1. Triage
Many EDs have moved a physician or advanced practice provider to participate in the triage process to decrease wait times and left‐without‐being‐seen rates. 19 In this capacity, they help to facilitate the rapid identification of patients needing immediate interventions and also to initiate imaging and laboratory testing. Frequently, they are able to evaluate, treat, and discharge many lower acuity patients from the waiting room. As the threat of a COVID‐19 infection surge increased, it would be anticipated that patients would present along the entire spectrum of illness and that many would need minimal or no testing. 20 Telemedicine provides a medium for evaluating, educating, and reassuring these patients with mild illness, and reduces the expenditure of PPE. Discharge instructions, referral to outpatient testing facilities, and return precautions could be communicated.
2.2. Supplement to clinical care
Patients requiring interventions or more extensive evaluations (laboratory or imaging studies) also require the presence of healthcare workers to perform these studies. Although the initial evaluation, exam, laboratory draws, and imaging studies can often be “batched” together to avoid the risk of donning/doffing PPE, these patients often require reassessments, vital sign measurements, and communication of results and disposition planning. These interventions also presented an opportunity to employ telemedicine mobile carts for communication, observation of respiratory status, performing “walk tests” and other forms of reassessment. Similarly, discussions with patients either regarding discharge planning or admission rationale could be discussed virtually. These devices can also be used for specialty consultation; for instance, the evaluation of a patient by psychiatric personnel in the ED.
2.3. Resident and advanced practice provider oversight
Because of the increased risk of morbidity and mortality for older physicians and the immunocompromised, 21 several emergency physician groups have taken measures to decrease the risk of COVID‐19 exposure for these healthcare professionals. Anecdotal reports exist of departmental policies aimed at protecting high‐risk personnel including those older than 60–65, immunocompromised, or pregnant from contact with suspected COVID‐19 patients. Some kept physicians older than 50 out of higher risk aerosolizing procedures, such as endotracheal intubation. 22 Telemedicine offers a potential option for emergency physician groups that have at least double coverage and are interested in decreasing the exposure of this at‐risk group of physicians. This strategy uses a dedicated telemedicine cart. Many institutions are familiar with these devices as they are often used to provide telestroke capabilities. However, instead of providing a remote neurologist, a physically present emergency physician is replaced by a virtual remote physician.
The requirement for this process to be successful is that the remote emergency physicians duties are predominantly supervisory. Remote access to the institutions electronic medical record allows the emergency physician the ability to chart and place orders. This could be useful in academic institutions with emergency or other residents staffing the ED. In support of this, the Accreditation Council for Graduate Medical Education (ACGME) released a position statement that states “effective immediately, the ACGME will permit residents/fellows to participate in the use of telemedicine to care for patients affected by the pandemic.” 23 Included in the position is the allowance of direct supervision via telemedicine. Primary care by APPs could also be supervised by this modality. There must be at least double coverage in the ED so that a physically present emergency physician is always available to perform procedures, intubations, and resuscitations. The virtual remote use of telemedicine could also be used by an emergency physician infected with COVID‐19 who is well enough to work a shift from home, but not yet beyond the recovery period allowing him/her to return to physical work. 24
2.4. Specialty consultation/COVID‐19 cohorted treatment area
As preparations for the surge of COVID‐19 illness increased, plans to cohort patients under investigation for COVID‐19 within the ED led many institutions to develop COVID‐19 pods. Some hospitals' plan was to incorporate other medical specialties (internal medicine, anesthesia, trauma surgery, pulmonary and critical care medicine) into the ED workforce with a board‐certified emergency medicine attending available for consultation via telemedicine. Additionally, within the COVID‐19 persons under investigation (PUI) cohorted unit, those testing positive for SARS‐CoV‐2 who manifest mild symptoms may be able to continue to provide care via telemedicine. Telemedicine becomes part of an innovative and integrated strategy to expand critical ED operations despite a temporarily unavailable workforce.
3. LOGISTICS OF IMPLEMENTATION
As stated above, multiple challenges existed prior to COVID‐19 with 1 of the largest being the rural/urban billing restrictions instituted by Medicare. However, other challenges exist with the majority of these surrounding operations and technology. One of the first operational hurdles that must be overcome is that of platform choice. Although many video conferencing platforms exist and are able to be used currently, it is unlikely that the grace we have been given with the relaxation of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will continue after the national emergency ends. As such, HIPAA‐compliant video conferencing solutions are ideal to ensure no large changes to protocol are needed. Furthermore, video conferencing platforms can vary. Some only offer video itself, which requires significant logistic operation to ensure the physician knows when a consult is needed. Others will automate the process of contacting the appropriate physician by integrating call schedules directly into the platform. There are pros and cons to both types of solutions largely related to cost. Programs serving a large number of external sites would be better served to have logistics in the platform versus those only trying to serve 1 or 2 locations that would not be able to justify the cost of anything but video alone.
The type of videoconferencing device must also be evaluated. For instance, tablet‐based solutions are inexpensive and portable. They make excellent devices. However, the speakers in tablet‐based solutions may be very difficult for patients to hear over the din of the emergency department. Laptop computers with external speakers may improve on sound, but because of the inability to move the camera in a ready fashion, may have limitations when it comes to performing a physical examination. This would require an external handheld camera to fully be able to assist with the remote physical examination. Cart‐based solutions are expensive but usually are equipped with cameras that have full pan/tilt/zoom and remote camera control.
Training of staff is one of the biggest logistical hurdles that must be undertaken and typically requires multiple training sessions. Once trained, the acceptance into general use of the technology is best achieved by establishing a telemedicine champion in the department.
4. REGULATORY AND LEGAL CHANGES
As the evolving COVID‐19 pandemic imposes unprecedented pressures on EDs across the nation, the CMS has revised federal regulations governing the use of telemedicine, enabling dramatically expanded use in the ED setting (Table 2). These modifications, granted in part due to advocacy from the American College of Emergency Physicians (ACEP) and other national physician organizations, 25 provide the legal and billing framework for broad and creative application of telemedicine within the ED. Additionally, CMS has authorized temporary modifications to aspects of Emergency Medical Treatment and Labor Act (EMTALA) infusing flexibility to telemedicine strategies. 4
TABLE 2.
Recent regulatory and legal changes related to the COVID‐19 global pandemic and telemedicine
| Original policy | Temporary COVID‐19 provision |
|---|---|
| Telemedicine: originating site restricted to rural medical sites outside of the patient's home. Physician and patient may not be in the same physical location. | Telemedicine: all geographic requirements suspended, permitting telehealth encounters on the same premises, such as within an ED. |
| EMTALA: MSE must be performed at point of contact within the ED and inperson. | EMTALA: MSE may be performed via telehealth. Patients may be redirected to offsite screening locations. |
| Billing: emergency medicine services not billable if provided through telemedicine. | Billing: all ED services, including critical care, may be provided and billed through telemedicine. |
Note: Modified from American College of Emergency Physicians (ACEP) informatic: “COVID‐19 response: Medicare telehealth coverage expansion during COVID‐19 public health emergency.” 25
Abbreviations: ED, emergency department; EMTALA, Emergency Medical Treatment and Labor Act; MSE, medical screening exam.
4.1. Originating site restriction changes
Federal policy in place before the current pandemic has limited the widespread implementation of telemedicine in the ED. Restrictions have hitherto required that the physician and the beneficiary be in geographically separate locations and for the beneficiary to be in a designated rural area. For example, a specialist in an office clinic setting who remotely evaluates a patient located at a rural skilled nursing facility would fulfill the geographic requirement. A scenario not permitted, however, included emergency physician assessment of a patient located in the same department (such as a nearby isolation room) via video feed. In addition, before the changes, ED services and their corresponding evaluation and management (E/M) codes were not billable through telehealth encounters. 4 , 25
4.2. Billing changes
In response to the COVID‐19 crisis, and as part of a broad expansion including more than 80 healthcare services, CMS now allows all ED services provided via telehealth to be billed as if they occurred in person. This applies to all common emergency department E/M codes (CPT 99281 to 99285) as well as critical care codes (CPT 99291 and 99292). For Medicare patients, telemedicine services are reimbursed on par with those provided inperson. The geographic requirement is eliminated. Included in the permitted use of telehealth is attending physician remote supervision of resident services, including procedures. 4
4.3. Device and interface changes
New guidance allows the use of any 2‐way real‐time audio‐visual interface between physician and patient. The Office of Civil Rights at the Department of Health and Human Services (HHS) announced discretionary enforcement and elimination of penalties for potential HIPAA violations that occur during the good faith provision of healthcare services using non‐public facing technologies such as Skype and FaceTime. 26 This effectively enables the use of widely available mobile applications that may not fully adhere to standard HIPAA requirements.
4.4. Medical screening exam via telemedicine
The requirement under EMTALA for all patients presenting for evaluation to the ED to receive a medical screening exam has not changed. However, CMS has approved a temporary 1135 waiver for the duration of the COVID‐19 pandemic that allows the medical screening exam to be conducted via telemedicine. Redirection at the point of ED triage to alternative hospital‐controlled screening sites (whether on‐ or off‐campus) for the medical screening exam is also permitted. This off‐site screening site may be staffed via telemedicine. Critically, this provision enables the early separation of patients with COVID‐19 symptoms from the general ED population and unlocks additional patient flow options in EDs faced with surging patient volumes. These screening sites must be staffed with qualified medical practitioners trained to perform a medical screening exam.
In summary, the federal response to the COVID‐19 global pandemic allows EDs to use telemedicine to perform a medical screening exam (within the ED or offsite) and can now bill traditional E/M codes based on services provided entirely via telemedicine. Through a temporary waiver to EMTALA, patient flow at the point of initial contact has expanded to include redirection to offsite screening and triage centers, which can also be staffed via telemedicine. Use of telemedicine for primary evaluation and treatment of selected patients is supported by a legal and billing framework authorized for the duration of the COVID‐19 national emergency.
5. INSTITUTIONAL EXPERIENCE
5.1. University of Alabama at Birmingham
The University of Alabama at Birmingham Hospital is a level 1 trauma center located in central Alabama with an annual adult ED census of 80,000. We have successfully used a novel approach to telemedicine that came out of the desire of our academic faculty to protect the more vulnerable in the group from exposure to COVID‐19. The virtual remote physician model that replaces 1 physically present supervising attending with a virtual remote attending was implemented in April 2020. In our university ED with a fully accredited emergency medicine residency, our staffing model provides full‐time triple attending physician coverage. Each attending physician covers one of 3 resident pods, each made up of 9–11 patient rooms. This level of physician staffing permits the replacement of 1 physically present attending with a remote attending in one of the pods. The remote physician‐staffed pod is also covered by a senior EM resident and is in a central location, which allows the physically present attending to be immediately available for any critically ill patients or to assist with the performance of a necessary procedure.
The remote physician, through a secure website, can sign into the telemedicine cart from home or other secure location (Figure 1). Remote access to the facility electronic medical record is also optimal. The attending can use the camera, audio, and 2‐way communication capabilities of the cart to see patients with the resident or APP and supervise care. The physically present physician takes the telehealth cart (with the embedded telemedicine attending) into the patient room (Figure 2). This process allows the virtual attending to observe the entire initial history, physical examination, and assessment. This remote physician can also ask additional history questions. The camera allows close views of the physical examination and can direct the resident or APP to expand physical examination aspects as needed. Discussion of plan of care, evaluation test results, and patient disposition can occur using the audio capabilities of the cart or can be performed telephonically.
Our experience has been positive; although we understand that it is not as optimal as in‐person supervision, it has proven to be a viable method to provide resident supervision in an academic emergency medicine residency program during this difficult time. Although there are some drawbacks, we have also found advantages in this mode of supervision. We feel we can provide appropriate resident supervision, teaching, and feedback. 22
We have also used telemedicine carts in our triage area to perform no‐touch physician evaluations in isolation rooms and to provide access for patient evaluations by specialists in the ED.
FIGURE 1.
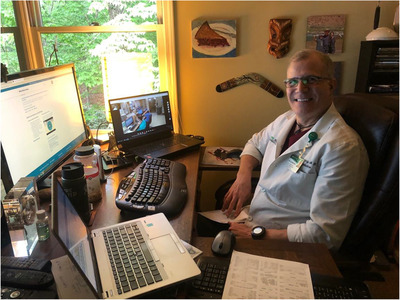
Remote physician supervising resident physicians from home. The near laptop is displaying the electronic medical record, the distant laptop provides the camera and audio view of the emergency department (ED)
FIGURE 2.
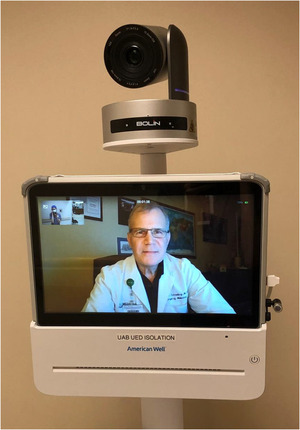
Patient experience with telemedicine
5.2. The University of Kentucky
A COVID‐19 pod was created at the University of Kentucky Chandler Medical Center, a level 1 trauma center located in central Kentucky with an annual adult ED census of 62,000. Patients arrive at the door and are immediately screened by the “forward triage” nurse with a predefined set of criteria to identify COVID‐19 PUI patients. If a patient positively screens, the SARS‐CoV2 PCR test is automatically ordered as well as airborne, contact, and eye protection precautions. The patient is then brought back to the respiratory ED. The respiratory ED is separate from the main ED and consists of 24 discrete rooms. To assess the patient in these rooms, telemedicine has been implemented. Each room is outfitted with a tablet on a stand with an adjustable clamp and that can be moved for ease of communication with the patient. The physician is able to “enter” the room along with the APP or resident, scribe, and nurse. During this interview, a determination is made as to whether an “in‐person” or “no‐touch” exam will be needed. If an “in‐person” exam is required, they will enter the room in full PPE and conduct the examination. They also has the option to do a “no‐touch” examination and document the medical screening examination completed using the telemedicine encounter. In addition, there is the option to do reassessments and discharge planning over telemedicine. The portable system is easily cleaned after each use with cleansing wipes.
There has been a marked decrease in all healthcare worker contacts with potentially infected patients. Registration, social work, language interpretation, and reassessments may all be completed by telemedicine. Along with this has come a significant decrease in PPE use given fewer healthcare worker contacts. To date, only a few healthcare workers who work in the University of Kentucky Chandler Medical Center ED have tested positive for COVID‐19.
6. CHALLENGES OF TELEMEDICINE
Many mistake telemedicine as just the installation of a videoconferencing solution. However, the challenges, implementation, and scaling are akin to starting a new service line or clinic. How to provide appropriate care should be the number 1 goal of any telemedicine program. Auscultatory exams can be performed using any number of tele‐stethoscopes. Incorporation of point‐of‐care ultrasound and imaging seems like a very logical next step but largely due to cost of the devices and time needed to perform the examination have not been implemented on a large‐scale basis. Other operational options include relying on an onsite resident, RN or APP to do the physical examination. Peripheral telemedicine devices should be assessed for their advantages and disadvantages based on the needs of the system. These devices can add to the complexity to the system. Technology failures and time delays in the patient visit are risks. Patients may not be accepting of the use of telemedicine and this may generate complaints. Finally, the use of more telemedicine devices may require more staff or alternative staffing models.
Patient experience must also be taken into account when evaluating telemedicine. The best planned programs benefit the patients, the physician, and are atleast cost neutral. Those only benefiting one party are unlikely to be sustainable. The patient experience will change over time as technology literacy changes and acceptance increases. The ability to do a physical examination over telemedicine will likely increase patient acceptance. Specifically, the auscultatory examination not only improves the ability to address medical problems, but also lends validity to the idea that many older patients have who associate the stethoscope with receiving care. In the era of COVID‐19 with both physician and patients wearing masks, telemedicine allows the patient to see the face of at least 1 physician. Our experience with telemedicine and the unprecedented changes that our patients experience when seeking care in our EDs seem to indicate that patients are accepting of interacting with a physician in this fashion.
Largely, the challenge has been with the economic model. The economic model has improved greatly for telemedicine given the changes in reimbursement, but should we see a regression of reimbursement, then much of the progress that has been made may unfortunately stall. Another challenge may be the initial cost of hardware and software; however, the efficiency gained from department patient flow and throughput should cover this cost over time. Finally, if there is no concern for exposure, some of the applications may be unnecessary.
7. FUTURE APPLICATIONS
The success of telemedicine across EDs in the COVID‐19 outbreak has been an important litmus test for future applications of this technology. This pandemic has highlighted the necessity and utility of telemedicine when the well‐being of healthcare workers is at stake, and also when resources, such as PPE, are limited. Setting this framework now is invaluable and, unfortunately, will likely need to be implemented similarly during future pandemics. As federal laws and regulations rush to accommodate what is now accepted as a necessary and powerful tool in fighting this public health crisis, we should consider other applications of the technology.
A salient parallel to the current struggle of our EDs can be drawn to critical access hospitals, where physicians lack access to subspecialists among many other resources. Telemedicine could prove crucial to connecting them in real time to board‐certified emergency medicine specialists for assistance with resuscitation and stabilization of severely ill COVID‐19 patients prior to transfer. Likewise, our nation's critical care capabilities could be expanded by providing remote hospitals with access to pulmonologists and nephrologists, among other subspecialists often scarce in rural settings. The use of telemedicine to connect with specialists was pioneered over 20 years ago with remote neurologists assessing the need for thrombolysis in acute ischemic stroke (AIS). 27 Several countries around the world, including the United States, have implemented these strategies for AIS37 27 , 28 , 29 but little innovation has been made in the field since that time. Using telemedicine to expand access to specialists has the potential to improve patient outcomes, and in the scenario that our regional healthcare system becomes overwhelmed during this pandemic, sets a framework to effectively triage which patients will need to be transferred to a tertiary care center emergently.
The application to critical access hospitals in the United States can be extrapolated 1 step further to international EDs in resource‐limited settings. The technology has fostered an ease of collaboration never before seen that gives us the power to begin addressing health disparities. In many African countries that have upward of 1 million citizens for each ventilator access to emergency medicine, critical care, and infectious disease specialists may be instrumental in stemming the flow of infection and managing critical COVID‐19 patients. 30
If the regulatory changes remain permanent after the global pandemic, telemedicine would necessarily be integrated into ED operations. One potential application would be patients using telemedicine to consult an emergency physician from home. Another possibility would be scheduling a 24–48 hour follow‐up telemedicine visit after an in‐person ED visit. As healthcare has been slow to adapt to the digital revolution, the many abrupt changes since the onset of the pandemic have the potential to lead to more permanent changes in how patients access emergency medical care. As we continue to explore this technology and its use in the medical field becomes more facile, we will undoubtedly uncover more applications for telemedicine that enable us to better serve our patients and collaborate with our colleagues.
The widespread application of telemedicine in EDs is novel and requires careful scrutiny. A national work group is needed to conduct research and track outcomes for COVID‐19 patients seen by in‐person physicians and those seen by a remote physician. Very ill patients typically require multiple life‐sustaining procedures that often necessitates a multi‐disciplinary team to be physically present. Many of the recent applications are novel adaptations to meet the urgent needs in this crisis and have yet to be validated. Future research should focus on the role of telemedicine in a global pandemic response. Additionally, many of the billing requirements that CMS have lifted to facilitate the use of telemedicine are specific to the COVID‐19 outbreak and are likely temporary.
8. CONCLUSION
The COVID‐19 global pandemic has significantly strained the emergency care delivery system in the United States. EDs across the States are creating novel approaches of telemedicine implementation to support this stressed system. The strengths of telemedicine help us meet the needs of our patients and have proven to be one important tool in our toolbox to help us navigate the most significant public health crisis of this century.
Hamm JM, Greene C, Sweeney M, et al. Telemedicine in the emergency department in the era of COVID‐19: front‐line experiences from 2 institutions. JACEP Open. 2020;1:1630–1636. 10.1002/emp2.12204
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Henry E. Wang, MD, MS.
REFERENCES
- 1. Flannery D, Jarrin R. Building a regulatory and payment framework flexible enough to withstand technological progress. Health Affairs. 2018;37(12):2052‐2059. [DOI] [PubMed] [Google Scholar]
- 2. Telemedicine Opportunities and Developments in Member States. World Health Organization . Page 8. Available at: https://www.who.int/goe/publications/goe_telemedicine_2010.pdf
- 3. About Telemedicine. American Telemedicine Association . 2020. Available at: http://legacy.americantelemed.org/main/about/about-telemedicine/telemedicine-faqs
- 4. CMS Fact Sheet “Medicare Telemedicine Health Care Provider Fact Sheet”. Released March 17, 2020
- 5. Demaerschalk B, Berg J, Chong B, et al., American Telemedicine Assoication: telestroke guidelines. Telemedicine e‐Health. 2017. 23:5:376–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Surgical Mask and Gown Conservation Strategies—Letter to Healthcare Providers. Food and Drug Administration . 2020. Available at: https://www.fda.gov/medical-devices/letters-health-care-providers/surgical-mask-and-gown-conservation-strategies-letter-healthcare-providers
- 7. COVID‐19 Facemasks Updates. Centers for Disease Control and Prevention . 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html [PubMed]
- 8. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhan M, Qin Y, Xue X, Zhu S. Death from COVID‐19 of 23 health care workers in China. N Engl J Med. 2020:NEJMc2005696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet, 395 10231: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. MMWR characteristics of health care personnel with COVID‐19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hollander JE, Carr BG., Virtually perfect? Telemedicine for Covid‐19. N Engl J Med. 2020;382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 13. Doarn CR, Merrell RC, Spacebridge to Armenia: a look back at its impact on telemedicine in disaster response. Telemed J E Health 2011,17(7):546–552. [DOI] [PubMed] [Google Scholar]
- 14. Wallace DL, Smith RW, Pickford MA A cohort study of acute plastic surgery trauma and burn referrals using telemedicine. J Telemed Telecare. 2007;13(6):282–287. [DOI] [PubMed] [Google Scholar]
- 15. Rogers FB, Ricci M, Caputo M, et al, The use of telemedicine for real‐time video consultation between trauma center and community hospital in a rural setting improves early trauma care: preliminary results. J Trauma 2001,51(6):1037–1041. [DOI] [PubMed] [Google Scholar]
- 16. Brunetti ND, De Gennaro L, Amodio G, et al, Telecardiology improves quality of diagnosis and reduces delay to treatment in elderly patients with acute myocardial infarction and atypical presentation. Eur J Cardiovasc Prev Rehabil 2010,17(6):615–620. [DOI] [PubMed] [Google Scholar]
- 17. Agarwal S, Day DJ, Sibson L, et al., Thrombolysis delivery by a regional telestroke network–experience from the U.K. National Health Service. J Am Heart Assoc 2014,3(1):e000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Britton N, Miller MA, Safadi S, Siegel A, Levine AR, McCurdy MT. Tele‐ultrasound in resource‐limited settings: a systematic review. Front Public Health. 2019;7:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chan TC, Killeen JP, Kelly D, Guss DA. Impact of rapid entry and accelerated care at triage on reducing emergency department patient wait times, lengths of stay, and rate of left without being seen. Ann Emerg Med 2005;46:491‐497 [DOI] [PubMed] [Google Scholar]
- 20. Pandemic Influenza Triage Tools . Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/cpr/healthcare/pan-flu-app/desktop/pita.html. Accessed March 19, 2020.
- 21. Severe outcomes among patients with coronavirus disease 2019 (COVID‐19) – United States, February 12‐March 16, 2020. Morbidity and Mortality Weekly Report (MMWR). Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm Accessed April 11, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schrading W, Pigott D, Thompson L. Virtual remote attending supervision in an academic emergency department during the COVID‐19 pandemic. Accepted for publication AEM Educ Train. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Accreditation Council for Graduate Medical Education . ACGME Response to COVID‐19: Clarification regarding Telemedicine and ACGME Surveys. Date released March 18, 2020. Available at: https://www.acgme.org/Newsroom/Blog/Details?articleId=10125
- 24. COVID‐19 RESPONSE. ACEP . Medicare Telehealth Coverage Expansion During the COVID‐19 Public Health Emergency. 2020. Available at https://www.acep.org/globalassets/new-pdfs/advocacy/summary-of-covid-19-telehealth-waivers-3-26.pdf.
- 25. MS Memorandum “Emergency Medical Treatment and Labor Act (EMTALA) Requirements and Implicated Related to Coronavirus Disease 2019 (COVID‐19)”. Released March 30, 2020 (revised August 4, 2020) Available at https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
- 26. Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID‐19 Nationwide Public Health Emergency. Health and Human Service/Office of Civil Rights Memorandum. Released March 17, 2020. Available at: https://www.facs.org/-/media/files/covid19/ocr_update_031720_hipaa_communications.ashx
- 27. Akbik F, Hirsch JA, Chandra RV, et al, Telestroke—the promise and the challenge. Part one: growth and current practice. J NeuroInterve Surge 2017;9:357–360. [DOI] [PubMed] [Google Scholar]
- 28. Ang SH, Tan C, Singh R. Telestroke: rapid treatment of acute ischemic stroke patients using telemedicine in a Singapore emergency department, European J Emerge Med. 2013;20 5:322–326 [DOI] [PubMed] [Google Scholar]
- 29. Audebert HJ, Kukla C, Clarmann Von Claranau S, et al. Telemedicine for safe and extended use of thrombolysis in stroke: the Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria. Stroke 2005;36:287–291. [DOI] [PubMed] [Google Scholar]
- 30. Maclean R, Marks S. 10 African Countries Have No Ventilators. That's Only Part of the Problem. New York Times. April 18, 2020. Available at: https://www.nytimes.com/2020/04/18/world/africa/africa-coronavirus-ventilators.html


