Abstract
Objective
The quality of cardiopulmonary resuscitation (CPR) affects outcomes from cardiac arrest, yet manual CPR is difficult to administer. Although mechanical CPR (mCPR) devices offer high quality CPR, only limited data describe their deployment, their interaction with standard manual CPR (sCPR), and the consequent effects on chest compression continuity and patient outcomes. We sought to describe the interaction between sCPR and mCPR and the impact of the sCPR‐mCPR transition upon outcomes in adult out‐of‐hospital cardiac arrest (OHCA).
Methods
We analyzed all adult ventricular fibrillation OHCA treated by the Anchorage Fire Department (AFD) during calendar year 2016. AFD protocols include the immediate initiation of sCPR upon rescuer arrival and transition to mCPR, guided by patient status. We compared CPR timing, performance, and outcomes between those receiving sCPR only and those receiving sCPR transitioning to mCPR (sCPR + mCPR).
Results
All 19 sCPR‐only patients achieved return of spontaneous circulation (ROSC) after a median of 3.3 (interquartile range 2.2–5.1) minutes. Among 30 patients remaining pulseless after sCPR (median 6.9 [5.3–11.0] minutes), transition to mCPR occurred with a median chest compression interruption of 7 (5–13) seconds. Twenty‐one of 30 sCPR + mCPR patients achieved ROSC after a median of 11.2 (5.7–23.8) additional minutes of mCPR. Survival differed between groups: sCPR only 14/19 (74%) versus sCPR + mCPR 13/30 (43%), P = 0.045.
Conclusion
In this series, transition to mCPR occurred in patients unresponsive to initial sCPR with only brief interruptions in chest compressions. Assessment of mCPR must consider the interactions with sCPR.
Keywords: cardiac arrest, cardiopulmonary resuscitation, mechanical CPR, resuscitation
1. INTRODUCTION
1.1. Background
The quality of the cardiopulmonary resuscitation (CPR) provided to victims of out‐of‐hospital cardiac arrest (OHCA) affects their chances of survival. Real‐world manual chest compressions suffer from poor quality: compressions are often too shallow, administered at incorrect rates, and frequently interrupted. 1 , 2 Mechanical CPR (mCPR) devices deliver chest compressions with consistent depth and rate, full recoil, and high compression fraction.
1.2. Importance
The use of mCPR involves not only the device but also its application, entailing positioning of the device back plate under the patient, connection and adjustment of compression mechanism, and actuation of the device. Most important, application of the mCPR device must be coordinated with ongoing resuscitation efforts entailing standard manual CPR (sCPR). The time and manner of device application may potentially influence resuscitation quality and outcomes. Neither the large randomized controlled trials (RCTs) nor the majority of observational trials on mCPR devices report or analyze these important parameters. 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 A detailed analysis of a small subset of cases in 1 RCT revealed that the median pause in CPR for device deployment was over 30 seconds. 14
1.3. Goals of this investigation
We sought to describe the interaction between sCPR and mCPR and the impact of the sCPR‐to‐mCPR transition upon resuscitation of adult OHCA.
2. METHODS
2.1. Study design and setting
The study is a retrospective analysis of out‐of‐hospital ventricular fibrillation (VF) cardiac arrests treated by the Anchorage Fire Department (AFD). The University of Alaska Anchorage Institutional Review Board reviewed the study and found it not to be human subject research and to be exempt from further oversight.
The AFD provides all 911 emergency medical service (EMS) responses and transports for the Municipality of Anchorage, Alaska, a community of 300,000. A cardiac arrest response is initiated by dispatch with concurrent telecommunicator CPR and is attended by a minimum of 5 professional EMS responders, at least 2 of whom are paramedics. As part of a broader program of high‐performance CPR, mCPR devices have been used by AFD since 2007. 15 , 16 Resuscitated patients are preferentially taken to tertiary care hospitals with 24‐hour access to interventional cardiology and typical intensive care treatment including routine targeted temperature management.
2.2. Selection of subjects
We included all adult VF OHCA receiving sustained CPR by AFD during 2016. We excluded patients with Do Not Resuscitate orders and those for whom the defibrillator's electronic record was unavailable.
2.3. Interventions
During this study, 15 LUCAS 2 Chest Compression Systems (Stryker/Jolife AB, Lund, Sweden) were carried by Advanced Life Support (ALS) vehicles. CPR provided by the AFD typically starts with 2‐minute cycles of manual CPR, sometimes followed by transition to the mCPR device, a decision made by the lead paramedic. The decision on whether to use mCPR is dynamic and includes such parameters as patient size, initial response to treatment such as transient return of spontaneous circulation (ROSC) suggesting that the event may successfully terminate early, and other scene considerations. Protocols allow for scene termination and transport with mCPR in progress is uncommon but occurs occasionally.
The AFD applies mCPR devices following a strict protocol that is reinforced by frequent in‐station training. All members adhere to the tenet of minimizing the interruption in chest compressions to apply the device; recordings of the monitor‐defibrillator impedance signal are routinely reviewed to determine whether this pause has met the goal of being < 10 seconds. The AFD incorporates the use of mCPR into its high‐performance CPR training with weekly in‐station training.
2.4. Outcomes and measurements
The primary outcomes were (1) duration of sCPR, and (2) duration of CPR interruption for transition to mCPR; these measures were abstracted from continuous ECG and transthoracic impedance recordings from the monitor‐defibrillator (LIFEPAK 12 or LIFEPAK 15, Physio‐Control, Redmond, WA, USA). We differentiated sCPR from mCPR by identifying the differences in impedance morphology characteristic of sCPR and mCPR (Figure 1). Two investigators (BMH and DY) used CODE‐STAT 10.0 Advanced CPR Analytics software (Physio‐Control, Redmond, WA, USA) to analyze these recordings independently, then resolved discrepancies through consensus discussion. We defined the sCPR‐to‐mCPR transition as the duration from the last manual compression to the first mechanical chest compression.
FIGURE 1.
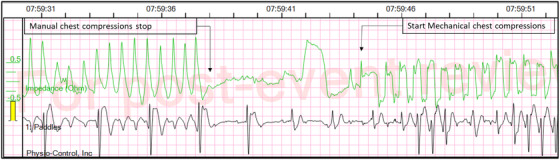
Monitor/defibrillator data from a patient with pulseless electrical activity following defibrillation showing a 22‐second interval during which the cardiopulmonary resuscitation (CPR) transitioned from manual chest compressions to mechanical chest compressions with a pause in compressions of about 6 seconds. Figure illustrates change in impedance morphology on transition to mechanical chest compressions, with waveforms becoming more square and having a consistent, precise rate. The top green curve shows the transthoracic impedance signal; the bottom black curve shows the ECG. Time format is HH:MM:SS.
Secondary outcomes include ROSC and survival to hospital discharge. ROSC was defined as the restoration of a sustained palpable pulse, and the point in time at which it occurred was determined by an event marker and cessation of CPR. Survival was defined as alive vital status upon discharge from the hospital. The patient's discharge neurological status was defined using the cerebral performance category (CPC) scoring method at the time of discharge.
Other variables used in the analysis included patient characteristics (age, sex), arrest characteristics (location, witnessed status, cardiac cause, type of bystander CPR/automated external defibrillator use prior to AFD arrival, who initiated CPR), resuscitation characteristics (advanced airway, resuscitation drugs, out‐of‐hospital therapeutic hypothermia) and response times.
2.5. Analysis
We divided the cohort into 2 groups: (1) sCPR‐only, patients who received only manual CPR, and (2) sCPR + mCPR, patients who transitioned to mCPR after initial standard CPR. Because the AFD protocol requires that all resuscitations begin with standard manual CPR, there were no cases that received only mCPR. We compared patient characteristics between sCPR‐only and sCPR + mCPR. We determined the elapsed time of sCPR, the interruption in CPR for transition from sCPR to mCPR, and the duration of subsequent resuscitation. We compared outcome between sCPR‐only and Scpr + mCPR using Fisher's exact test.
3. RESULTS
3.1. Characteristics of study subjects
During the study period, AFD treated 248 OHCA, including 53 (21%) presenting with VF/ventricular tachycardia (VT). We excluded 3 patients with pre‐existing Do Not Resuscitate orders and 1 who received neither CPR nor defibrillation, leaving 49 in the analysis: 19 sCPR‐only and 30 sCPR + mCPR.
The patients included in our analysis were 56 (51–65) years old; 63% were male. The cardiac arrests were of cardiac cause in most (92%), were witnessed in most (80%), and occurred in a home or residence in the majority (69%) of patients.
The Bottom Line
Although prior studies describe cardiac arrest outcomes with the use of mechanical cardiopulmonary resuscitation (CPR) devices, few have described the details of the coordination between standard manual and mechanical chest compressions. This series of 49 adult out‐of‐hospital cardiac arrests from Anchorage, Alaska provides detailed perspectives of the complex transition from standard manual to mechanical chest compressions. These findings highlight the intricacies of studying mechanical chest compressions, including the potential influence of resuscitation time bias.
3.2. Comparison of sCPR‐only and sCPR + mCPR groups
Compared to sCPR‐only, sCPR + mCPR patients were less likely to experience OHCA in a public setting and had CPR initiated less often by a layperson. Other characteristics of patients and arrests did not differ between groups.
The duration of manual CPR and the total duration of CPR were both significantly longer in the sCPR + mCPR group than the sCPR‐only group (Figure 2, Table 2). The response to CPR differed significantly between groups even before device application. All sCPR‐only patients achieved ROSC, doing so after 3.3 (2.2‐5.1) minutes of manual CPR. Patients in the sCPR + mCPR group remained pulseless through 6.9 (5.3–11.0) minutes of manual CPR; the 21 sCPR + mCPR patients who got ROSC did so after 11.2 (5.7–23.8) additional minutes of CPR, delivered by the mCPR device (Figure 3).
FIGURE 2.
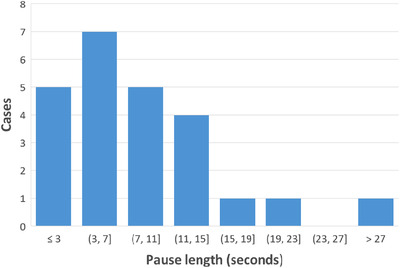
Histogram of the length of the interruption of chest compressions for application of the mechanical compression device to the patient. The patient in the far‐right bin had an interruption time of 28 seconds. Data are missing for 6 patients; in 1 case the device was placed prior to connection of the defibrillator electrodes and in 5 cases the impedance channel was unavailable.
TABLE 2.
CPR intervals, chest compression parameters, and defibrillation parameters
| All (N = 49) | sCPR‐only (N =19) | sCPR + mCPR (N= 30) | P | |
|---|---|---|---|---|
| Time in manual CPR | 6.0 [3.4‐9.4] | 3.3 [2.2‐5.1] | 6.9 [5.3‐11.0] | < 0.001 |
| Time in mechanical CPR | NA | NA | 13.2 [7.6‐26.5] | NA |
| Total time in CPR min | 14.5 [4.6‐28.5] | 3.3 [2.2‐5.1] | 25.2 [15.0‐34.2] | < 0.001 |
| CPR times for patients achieving ROSC (minutes, Median [Q1‐Q3]) | ||||
| Time in manual CPR | 5.1 [2.9‐8.8] | 3.3 [2.2‐5.1] | 6.8 [4.8‐11.9] | 0.006 |
| Time in mechanical CPR | NA | NA | 11.2 [5.7‐23.8] | NA |
| Total time of CPR | 11.6 [3.8‐23.9] | 3.3 [2.2‐5.1] | 22.3 [12.5‐28.8] | < 0.001 |
| CPR times for surviving patients (minutes, Median [Q1‐Q3]) | ||||
| Time in manual CPR | 5.0 [2.6‐7.4] | 3.4 [2.1‐5.1] | 6.4 [5.1‐10.4] | 0.01 |
| Time in mechanical CPR | NA | NA | 8.4 [4.2‐24.9] | NA |
| Total time in CPR | 9.1 [3.3‐14.8] | 3.4 [2.1‐5.1] | 14.8 [12.5‐29.2] | < 0.001 |
| When did ROSC occur? (N [%]) | ||||
| After only EMS CPR and defibrillation shocks | 15 (31%) | 14 (74%) | 1 (3%) | <0.001 |
| After ALS | 25 (51%) | 5 (26%) | 20 (67%) | 0.009 |
| Never | 9 (18%) | 0 (0%) | 9 (30%) | 0.008 |
| Chest compression parameters (Median [Q1‐Q3]) | ||||
| Interruption in chest compression for device deployment 7 (5‐13) | NA | 7 [5‐13] | NA | |
| Longest chest compression interruption during the resuscitation attempt (s) | 12 [9‐16] | 10 [7‐12] | 14 [10‐19] | 0.007 |
| Compression fraction (%) | 95 [93‐96] | 94 [92‐98] | 95 [93‐96] | 0.86 |
| Compression rate cc/min | 106 [102‐119] | 121 [110‐128] | 102 [102‐109] | < 0.001 |
| Defibrillation parameters (Median [Q1‐Q3]) | ||||
| Number of shocks (N) | 3 [1‐4] | 1 [1‐2] | 4 [3‐5] | < 0.001 |
| Time from start of manual chest compressions to first shock (mm:ss) | 01:18 [00:34‐02:11] | 00:47 [00:18‐01:54] | 01:25 [00:54‐02:12] | 0.074 |
| Pre shock compression interruption (s) | 4 [3‐6] | 4 [3‐8] | 3 [3‐6] | 0.74 |
| Post shock compression interruption (s) | 0 [0‐1] | 0 [0‐1] | 0 [0‐0] | 0.43 |
CPR, cardiopulmonary resuscitation; EMS, emergency medical services; ALS, advanced life support; ROSC, return of spontaneous circulation; NA, not applicable; sCPR, standard manual CPR; VF/VT, ventricular fibrillation/ventricular tachycardia.
Chest compression parameters, CPR intervals, and defibrillation parameters for patients presenting with VF/VT treated during 2016 by the Anchorage Fire Department (All) and for subgroups of patients receiving only manual chest compressions (sCPR‐only) and patients receiving manual chest compressions followed by mechanical compressions (sCPR + mCPR).
FIGURE 3.

Overview of cardiopulmonary resuscitation (CPR) timing and clinical outcome, with 1 row for each patient in the final analysis group, showing the durations of manual CPR (yellow) and mechanical CPR (mCPR; black) from the start of CPR until either first return of spontaneous circulation or termination of resuscitation. Patients in the standard manual CPR (sCPR)‐only group received only manual chest compressions; patients in the sCPR + mCPR group transitioned from manual chest compressions to mechanical chest compressions. Vertical (red) dashed lines show median manual CPR time for sCPR‐only and sCPR + mCPR groups. ED, emergency department; ROSC, return of spontaneous circulation.
Among the 30 patients who transitioned to mCPR, the transition occurred in a median of 7 (5–13) seconds (Figure 2). The longest interruption in chest compressions for any reason was slightly longer for sCPR + mCPR than sCPR‐only: 14 (10–19) versus 10 (7–12) seconds, P = 0.007. sCPR + mCPR patients received more resuscitation medications and defibrillation shocks than sCPR‐only did (Tables 1 and 2). Time to ED arrival and time on scene were longer in the sCPR + mCPR group.
TABLE 1.
Characteristics of cardiac arrests, resuscitation attempts, and outcomes
| Cardiac arrest related parameters (N [%]) | All (N = 49) | sCPR‐only (N = 19) | sCPR + Mcpr (N = 30) | P |
|---|---|---|---|---|
| Witnessed | 39 (80%) | 17 (89%) | 22 (73%) | 0.28 |
| Cardiac cause | 45 (92%) | 18 (95%) | 27 (90%) | >0.99 |
| Out‐of‐hospital therapeutic hypothermia | 37 (76%) | 15 (79%) | 22 (73%) | 0.74 |
| Who initiated CPR (N [%]) | ||||
| Layperson | 38 (78%) | 18 (95%) | 20 (67%) | 0.03 |
| Family member | 29 (59%) | 12 (63%) | 17 (57%) | 0.77 |
| First responder | 2 (4%) | 0 (0%) | 2 (7%) | 0.52 |
| Responding EMS personnel | 8 (16%) | 1 (5%) | 7 (23%) | 0.13 |
| Physician or nurse | 3 (6%) | 2 (11%) | 1 (3%) | 0.55 |
| Location of arrest (N [%]) | ||||
| Home/residence | 34 (69%) | 11 (58%) | 23 (77%) | 0.21 |
| Health facility | 2 (4%) | 1 (5%) | 1 (3%) | > 0.99 |
| Public building/place of recreation/industrial/transport center | 9 (18%) | 7 (37%) | 2 (7%) | 0.02 |
| Street/highway | 3 (6%) | 0 (0%) | 3 (10%) | 0.27 |
| Type of bystander CPR/AED (N [%]) | ||||
| Chest compressions only | 37 (76%) | 17 (89%) | 20 (67%) | 0.09 |
| Chest compressions and ventilation | 2 (4%) | 1 (5%) | 1 (3%) | > 0.99 |
| Unknown | 9 (18%) | 1 (5%) | 8 (27%) | 0.13 |
| Dispatch assisted CPR | 37 (76%) | 15 (79%) | 22 (73%) | 0.74 |
| AED use prior to EMS | 5 (10%) | 2 (11%) | 3 (10%) | > 0.99 |
| Advanced airway (N [%]) | 41 (84%) | 15 (79%) | 26 (87%) | 0.69 |
| Oral/nasal endotracheal tube | 30 (61%) | 13 (68%) | 17 (57%) | 0.55 |
| Laryngeal Mask Airway/King Airway | 11 (22%) | 2 (11%) | 9 (30%) | 0.16 |
| Impedance threshold device (ITD) | 45 (92%) | 17 (89%) | 28 (93%) | 0.64 |
| Resuscitation‐related drugs used (N [%]) | 37 (76%) | 7 (37%) | 30 (100%) | < 0.001 |
| Epinephrine | 32 (65%) | 4 (21%) | 28 (93%) | < 0.001 |
| Amiodarone | 21 (43%) | 2 (11%) | 19 (63%) | < 0.001 |
| Sodium bicarbonate | 16 (33%) | 1 (5%) | 15 (50%) | 0.001 |
| Other drugs used | 18 (37%) | 8 (42%) | 10 (33%) | 0.56 |
| Time variables (mm:ss and Median [Q1‐Q3]) | ||||
| Time from arrest to first chest compressions | 03:11 [02:07‐05:30] | 03:03 [02:00‐03:59] | 04:27 [02:51‐05:55] | 0.06 |
| Time from arrest to call | 01:00 [01:00‐02:00] | 01:00 [00:34‐02:00] | 01:00 [01:00‐02:00] | 0.37 |
| Time from arrest to first responder on scene | 06:44 [05:44‐07:48] | 06:15 [05:46‐07:04] | 07:01 [05:44‐07:59] | 0.51 |
| Time from arrest to ambulance on scene | 07:49 [06:19‐09:35] | 07:15 [05:46‐09:21] | 08:09 [07:00‐09:55] | 0.22 |
| Time from arrest to EMS at patient side | 09:00 [07:44‐10:55] | 09:30 [06:46‐10:38] | 08:53 [07:58‐11:40] | 0.57 |
| Time from arrest to ambulance left scene | 33:27 [26:57‐37:24] | 29:39 [25:36‐34:48] | 36:18 [28:49‐45:32] | 0.04 |
| Time from arrest to emergency department arrival | 41:06 [33:36‐49:24] | 37:12 [32:08‐41:37] | 44:41 [36:55‐54:23] | 0.01 |
| Outcome parameters (N [%]) | ||||
| Return of spontaneous circulation (ROSC) anytime | 40 (82%) | 19 (100%) | 21 (70%) | 0.008 |
| Survived to hospital admission, all VF/VT | 36 (73%) | 18 (95%) | 18 (60%) | 0.008 |
| Discharged alive, all VF/VT | 27 (55%) | 14 (74%) | 13 (43%) | 0.045 |
| Good cerebral performance, CPC 1 | 23 (47%) | 13 (68%) | 10 (33%) | 0.02 |
| Moderate disability, CPC 2 | 3 (6%) | 1 (5%) | 2 (7%) | > 0.99 |
| Severe disability, CPC 3 | 1 (2%) | 0 (0%) | 1 (3%) | > 0.99 |
| Discharged alive, witnessed VF/VT | 23/39 (59%) | 12/17 (71%) | 11/22 (50%) | 0.32 |
CPC, cerebral performance category; EMS, emergency medical services; AED, automated external defibrillator; VF/VT, ventricular fibrillation/ventricular tachycardia; CPR, cardiopulmonary resuscitation; mCPR, mechanical CPR; sCPR, standard manual CPR.
Characteristics of cardiac arrests, parameters of resuscitation attempts, and outcomes for patients presenting with VF/VT treated during 2016 by the Anchorage Fire Department (All), and for subgroups of patients receiving only manual chest compressions (sCPR‐only) and patients receiving manual chest compressions followed by mechanical compressions (sCPR + mCPR).
Overall, 73% of the VF/VT patients survived to hospital admission. Survival to admission differed between the sCPR‐only and sCPR + mCPR; 18/19 (95%) versus 18/30 (60%), P = 0.008. Overall, 55% survived to hospital discharge. Survival to hospital discharge differed between the sCPR‐only and sCPR + mCPR: 14/19 (74%) versus, 13/30 (43%), P = 0.045 (Table 1).
4. LIMITATIONS
This study is relatively small because it focuses on VF/VT cardiac arrests instead of including all arrests, and it limits enrollment to a single EMS system and a single year. Because of the small sample size, we did not perform multivariate risk adjustment. These results reflect performance at a single EMS agency and may not generalize to other systems. The AFD system, where this study took place, allows 5 personnel on scene and, by protocol, does at least 2 cycles of manual CPR before deciding whether to apply the mCPR device. These and other factors, such as whether resuscitation may be terminated in the field and whether the system transports with ongoing CPR, can all be expected to influence the details of device use and the relationship between device use and clinical outcomes. We did not include children in the analysis.
5. DISCUSSION
In this study we characterized the interaction of sCPR and mCPR, determining the resuscitation duration before transitioning from sCPR to mCPR as well as the duration of CPR interruption necessary to transition from sCPR to mCPR. Our findings highlight some important perspectives on mCPR device use and post event analysis and provide new understanding that is helpful in interpreting previous studies of these devices.
We found important differences in resuscitation time course between patients with manual CPR and patients receiving manual and then mCPR. In retrospect, the patients who received only manual CPR were patients who responded quickly to resuscitation efforts and, by definition, were easier to resuscitate. They had more favorable circumstances surrounding their initial care; their CPR was started more often by a layperson, and chest compressions were started significantly sooner after their arrest (in 3.1 vs 4.5 minutes). These patients who received only manual CPR got ROSC relatively quickly, after receiving a median of 3.3 minutes of manual CPR. In contrast, the patients who received mCPR were those who failed to get ROSC during manual CPR (median 6.9 minutes) and then received mCPR, intravenous drugs, and additional defibrillation shocks as part of their more prolonged resuscitation attempts. We were also able to objectively demonstrate that mCPR device use did not appreciably affect the chest compression fraction in those patients, eliminating one potential cause of the decreased survival rate in the sCPR + mCPR group.
In general, the probability of favorable outcome from cardiac arrest is known to decrease as the duration of the resuscitation attempt increases; patients most likely to survive regain a pulse within the first few minutes, whereas less viable patients often remain pulseless through many minutes of CPR. 17 , 18 , 19 Consequently, therapies to treat pulselessness applied later in the resuscitation will necessarily be applied to patients with lower chances of survival, giving rise to “resuscitation time bias” tending to make these therapies appear potentially harmful in results of observational studies. 20 For example, in our study, survival is significantly lower in the sCPR + mCPR group than in the sCPR‐only group, a difference that would be consistent with resuscitation time bias; the decision to apply the device was not made until the patient had remained pulseless through at least 2 cycles of CPR. Because of factors that tend to delay use of mCPR devices until after the initial minutes of resuscitation, this same bias likely affects the results of the many observational studies that have attempted to compare manual and mCPR; unfortunately, this cannot be confirmed because these studies did not measure or report timing metrics. 7 , 8 , 9 , 10 , 11 , 12 , 13
Three RCTs conducted between 2008 and 2013 compared manual and mechanical chest compression in OHCA; primary end points of those trials found that survival was similar for manual CPR and mCPR. 3 , 4 , 5 Since then, much has been learned about how to monitor and optimize use of the devices, but those improvements have not yet been tested in a randomized controlled trial. A new randomized trial should compare care with and without mechanical chest compressions, with particular attention to pitfalls related to the 2 time metrics on which our study focused: interrupting chest compressions for too long when applying the device and using the mCPR device too early or too late in the resuscitation. In the previous RCTs, the mCPR devices were applied as early as possible rather than initially focusing on high‐quality manual basic life support (BLS), and the interruptions in compressions to apply the devices were over 30 seconds in the few patients for whom this metric was reported. 3 , 4 , 5 , 14 Detailed review of monitor data, as we have done in this study, would serve to confirm and provide feedback on these important aspects of care.
This study demonstrates that mechanical chest compression device application times can and should be measured to reinforce minimizing chest compression interruptions. When to apply the device can be controlled by protocol to capitalize on early BLS success while also placing it in a time frame when the patient is still potentially viable. The timing of device application should be considered when interpreting observational studies of outcomes of patients who did and did not receive mechanical chest compressions, realizing that mCPR devices are used primarily on patients requiring prolonged resuscitation attempts, which are known to be independently associated with worse outcome.
CONFLICTS OF INTEREST
Michael Levy has received compensation from Physio‐Control, now a part of Stryker, for ECG over‐reading and for speaking at a Physio‐Control sponsored dinner discussion and is chief medical advisor for Stryker Physio‐Control. Karl B. Kern is a compensated member of the Science Advisory Board for Physio‐Control, and has received investigator‐initiated grant funding from Physio‐Control. Dana Yost has received compensation from Resurgent Biomedical Consulting LLC. (RBC) for ECG over read and CPR data analysis. RBC consults with Physio‐Control. Fred Chapman is employed by Stryker/Physio‐Control, the manufacturer producing the LUCAS chest compression device, LIFEPAK 15 Monitor/Defibrillator and CODE‐STAT Data Review Software. At the time of this study, Bjarne Madsen‐Hardig was employed by Physio‐Control/Lund, the manufacturer producing the LUCAS chest compression device, LIFEPAK 15 Monitor/Defibrillator, and CODE‐STAT Data Review Software.
ACKNOWLEDGMENTS
Michael Levy: I would like to gratefully acknowledge the assistance of Jenny Shin MPH and Mark Monfore, MICP in data collection as well as the women and men of the Anchorage Fire Department.
Biography
Michael Levy, MD, practices emergency medicine and EMS medicine in Anchorage, Alaska. He is the medical director for the Anchorage Fire Department.
Levy M, Kern KB, Yost D, Chapman FW, Hardig BM. Metrics of mechanical chest compression device use in out‐of‐hospital cardiac arrest. JACEP Open. 2020;1:1214–1221. 10.1002/emp2.12184
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Henry E. Wang, MD, MS
REFERENCES
- 1. Hostler D, Everson‐Stewart S, Rea TD, et al. Effect of real‐time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster‐randomised trial. BMJ. 2011;342:d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Krarup NH, Terkelsen CJ, Johnsen SP, et al. Quality of cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest is hampered by interruptions in chest compressions—a nationwide prospective feasibility study. Resuscitation. 2011;82:263‐269. [DOI] [PubMed] [Google Scholar]
- 3. Rubertsson S, Lindgren E, Smekal D, et al. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest. The LINC Randomized Trial. JAMA. 2014;311(1):53‐61. [DOI] [PubMed] [Google Scholar]
- 4. Wik L, Olsen J, Persse D, et al. Manual vs. integrated automatic load‐distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85:741‐748. [DOI] [PubMed] [Google Scholar]
- 5. Perkins GD, Lall R, Quinn T, et al. Mechanical versus manual chest compression for out‐of‐hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015;385(9972):947‐955. [DOI] [PubMed] [Google Scholar]
- 6. Wang PL, Brooks SC. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2018;. (8):CD007260. doi: 10.1002/14651858.CD007260.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buckler DG, Burke RV, Naim MY, et al. Association of mechanical cardiopulmonary resuscitation device use with cardiac arrest outcomes: a population‐based study using the CARES Registry (Cardiac Arrest Registry to Enhance Survival). Circulation. 2016;134:2131‐2133. [DOI] [PubMed] [Google Scholar]
- 8. Hayashida K, Tagami T, Fukuda T, et al. Mechanical cardiopulmonary resuscitation and hospital survival among adult patients with nontraumatic out‐of‐hospital cardiac arrest attending the emergency department: a prospective multicenter, observational study in Japan (SOS‐KANTO [Survey of Survivors after Out‐of‐Hospital Cardiac Arrest in KANTON Area] 2012 Study). J Am Heart Assoc. 2017;6(11):e007420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schmidbauer S, Herlitz J, Karlsson T, et al. Use of automated chest compression devices after out‐of‐hospital cardiac arrest in Sweden. Resuscitation. 2017;120:95‐102. [DOI] [PubMed] [Google Scholar]
- 10. Youngquist ST, Ockerse P, Hartsell S, et al. Mechanical chest compression devices are associated with poor neurological survival in a statewide registry: a propensity score analysis. Resuscitation. 2016;106:102‐107. [DOI] [PubMed] [Google Scholar]
- 11. Axelsson C, Herrera MJ, Fredriksson M, et al. Implementation of mechanical chest compression in out‐of‐hospital cardiac arrest in an emergency medical service system. Am J Emerg Med. 2013;31:1196‐200. [DOI] [PubMed] [Google Scholar]
- 12. Zeiner S, Sulzgruber P, Datler P, et al. Mechanical chest compression does not seem to improve outcome after out‐of‐hospital cardiac arrest. A single center observational trial. Resuscitation. 2015;96:220‐225. [DOI] [PubMed] [Google Scholar]
- 13. Newberry R, Redman T, Ross E, et al. No benefit in neurologic outcomes of survivors of out‐of‐hospital cardiac arrest with mechanical compression device. Prehosp Emerg Care. 2018;22:338‐344. [DOI] [PubMed] [Google Scholar]
- 14. Esibov A, Banville I, Chapman FW, Boomars R, Box M, Rubertsson S. Mechanical chest compressions improved aspects of CPR in the LINC trial. Resuscitation. 2015;91:116‐121. [DOI] [PubMed] [Google Scholar]
- 15. Yost D, Philips RH, Gonzales L, et al. Assessment of CPR interruptions from transthoracic impedance during the use of the LUCAS™ mechanical chest compression system. Resuscitation. 2012;83:961‐965. [DOI] [PubMed] [Google Scholar]
- 16. Levy M, Yost D, Walker RG, et al. A quality improvement initiative to optimize use of a mechanical chest compression device within a high‐performance CPR approach to out‐of‐hospital cardiac arrest resuscitation. Resuscitation. 2015;92:32‐37. [DOI] [PubMed] [Google Scholar]
- 17. Reynolds JC, Grunau BE, Rittenberger JC, et al. Association between duration of resuscitation and favorable outcome after out‐of‐hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016;134:2084‐2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grunau B, Reynolds J, Scheuermeyer F, et al. Relationship between time‐to‐ROSC and survival in out‐of‐hospital cardiac arrest ECPR candidates: When is the best time to consider transport to hospital? Prehosp Emerg Care. 2016;20:615‐622. [DOI] [PubMed] [Google Scholar]
- 19. de Graaf C, Donders DNV, Beesems SG, Henriques JPS, Koster RW. Time to return of spontaneous circulation and survival: when to transport in out‐of‐hospital cardiac arrest? Prehosp Emerg Care. 2020;7:1‐11. doi:10.1080/10903127.2020.1752868. [DOI] [PubMed] [Google Scholar]
- 20. Andersen LW, Grossestreuer AV, Donnino MW. "Resuscitation time bias"‐ A unique challenge for observational cardiac arrest research. Resuscitation. 2018;125:79‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]


