Abstract
Objectives
Emergency department (ED) crowding is a major problem across the world. Studies investigating the association between crowding and mortality are many, but the quality is inconsistent and there are very few large, high‐quality multicenter studies that are properly designed to deal with confounding due to case mix. The aim of this study is to investigate the association between ED crowding and 30‐day mortality.
Methods
We conducted an observational cohort study at all 7 EDs in Stockholm Region, Sweden 2012–2016. The crowding exposure was defined as the mean hourly ED census during the shift that the exposed patient arrived, divided with the expected ED census for this shift. The expected ED census was estimated using a separate linear model for each hospital with year and shift as predictors. The exposure was categorized in 3 groups: reference (lowest 75% of observations), moderate (75%–95% of observations), and high (highest 5% of observations). Hazard ratios (HR) for all‐cause mortality within 30 days were estimated with a Cox proportional hazards model. The model was adjusted for age, sex, triage priority, arrival hour, weekend, arrival mode, chief complaint, number of prior hospital admissions, and comorbidities.
Results
884,228 patients who visited the ED 2,252,656 times were included in the analysis. The estimated HR (95% confidence interval) for death within 30‐days was 1.00 (0.97–1.03) in crowding category 75%‐95% and 1.08 (1.03–1.14) in the 95%‐100% category.
Conclusions
In a large cohort study including 7 EDs in Stockholm Region, Sweden we identified a significant association between high levels of ED crowding and increased 30‐day mortality.
Keywords: crowding, emergency department, emergency service, health policy, hospital, mortality, patient safety
1. INTRODUCTION
1.1. Background
A large body of research provides evidence that emergency department (ED) crowding has negative consequences on patients, staff, and the healthcare system. 1 It is expected and intuitive that this imbalance between demand and capacity in the ED should have a negative impact on patients. Studies investigating the association between crowding and mortality are many, but the quality is inconsistent. We identified 8 high‐quality articles 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 that we could learn from when designing our study. Three of these 8 articles 3 , 6 , 7 both included a large enough sample from multiple EDs and were properly designed to manage confounding due to case mix. Even if these 3 studies were well performed, none was based outside of the United States or Canada and there was still room for methodological improvements. Studying the association between crowding and mortality is challenging for a number of reasons. First of all, the research question is demanding as crowding is intangible and requires a proxy‐measure. In addition, the exposure is likely to be rare because we hypothesize that the association is non‐linear, with only the highest levels of crowding being associated with increased mortality. Furthermore, the outcome, mortality within 30 days after an ED visit, is also rare, often around 1% – 2%. Finally, there are many natural causes for short‐term mortality after an ED visit not related to crowding, and previous high‐quality studies have estimated odds ratios in the range of 1.03 – 1.05. 6 , 7 A well‐defined proxy‐measure for crowding that limits the possibility of confounding due to case mix together with a very large number of observations will be required to identify a potential association between crowding and mortality.
1.2. Importance
The ED is a critical part of the healthcare system. Our study includes 2,252,656 visits by 884,228 individual patients to the 7 EDs in the Stockholm Region. This means that roughly half of the total adult population of 1,722,351 in the Stockholm Region required ED care during the 5‐year study period, indicating the importance to society.
1.3. Goals of this investigation
The aim of this study is to investigate the association between ED crowding and all‐cause mortality within 30 days of an ED visit.
The Bottom Line
Emergency department crowding can adversely affect patient care and outcomes. In this study of 2.2M ED visits at 7 EDs during 2012–2016 in Stockholm, Sweden, ED crowding was associated with increased 30‐day mortality. This article affirms the association between ED crowding and poor outcomes while also presenting methodological improvements for future research.
2. METHODS
2.1. Study design and setting
We conducted an observational cohort study at all 7 EDs in Stockholm Region, Sweden 2012–2016 including 884,228 unique patients with 2,252,656 visits during the period.
This included 1 university hospital with 2 large EDs at different locations with slightly below 70,000 visits per year in each site during the study; 4 public teaching hospitals with 107,000, 82,000, 28,000, and 22,000 visits per year; and finally a private but publicly funded teaching hospital with 75,000 visits per year. Data were extracted from the electronic healthcare records (EHR) in the hospitals. The public hospitals used the EHR system CGM TakeCare and the private hospital used Cambio COSMIC. This dataset was then linked to national registries.
2.2. Selection of Participants
We included all patients aged 18 years or older who visited any of the 7 EDs from January 1, 2012 to December 31, 2016. We excluded patients who required specialized emergency care within gynecology and obstetrics because these patient flows are separated from the main ED. Visits with missing or incorrect information required to calculate the exposure were removed from the analysis.
2.3. Exposure
The crowding exposure was based on the hourly number of patients present in the ED (ED census 10 ) in relation to the expected ED census. The exposure for each patient was defined as the mean hourly ED census during the shift that the exposed patient arrived divided by the expected ED census for this shift. The expected ED census was estimated using a separate linear model for each hospital with year and shift as predictors.
As sensitivity analysis we performed the same analysis using an alternative definition of the exposure. The exposure was defined as the mean length of stay for all other patients arriving during the same shift as the exposed patient, divided by the expected mean length of stay for these other patients. The expected length of stay for the other patients is estimated using a linear model with hospital, year, shift, age, sex, triage priority at arrival, arrival mode, and chief complaint as predictors. With this definition there is no link between the length of stay of the exposed patient and the crowding exposure that may introduce bias.
Both the primary and alternative measure of exposure were categorized into 3 groups as our hypothesis is that there is a non‐linear association between ED crowding and patient outcomes with only the highest levels of crowding affecting outcomes. Categories are reference (lowest 75% of observations), medium (75%–95% of observations), and high (highest 5% of observations).
2.4. Outcome
The outcome was all‐cause mortality within 30 days.
2.5. Data sources/measurement
Patient information from the electronic health record included arrival date/time, age, sex, arrival mode (grouped into emergency medical services and other), triage priority (1 highest – 5 lowest), and chief complaint. The 12 chief complaints representing the largest absolute number of deaths within 30 days were separated and all other chief complaints were grouped into “other.” Using the unique 10‐digit personal identity number (PIN) assigned to each person residing in Sweden, we linked information on disposition, comorbidities, and number of hospitalizations last year from the National Swedish Patient Register. Information regarding date of death was linked from the Cause‐of‐Death Register and we used the Prescription Drug Registry to identify patients with diabetes. The validity of the PIN and these registers is high. 11 International Classification of Diseases 10th edition (ICD‐10) codes retrieved from the Swedish National Patient Register were used to define comorbidities: myocardial infarction (I21‐I22, primary position), stroke (I61–I64, primary position), heart failure (I50, primary position), active cancer (C00‐C99, primary position, within last 2 years), chronic kidney disease (N18, any position), and chronic obstructive pulmonary disease (J44, any position). Diabetes was defined as recorded previsit filled prescription of Anatomical Therapeutic Chemical (ATC) code A10 in the Prescription Drug Registry.
2.6. Study size
In order to achieve a statistical power of 90% and a certainty of 95% with an expected mortality of 1.5% we need 1,434,291 visits to identify a hazard ratio of 1.10 in the highest category of exposure including top 5% of visits. 12
2.7. Statistical methods
The baseline data on patient characteristics are presented as absolute numbers and column percentage of ED visits by crowding category and variable. Hazard ratios with 95% confidence intervals (CI) were estimated with a Cox stratified proportional hazards model. This model allows for independent baseline hazards across hospitals but assume that the hazard ratio is the same for all hospitals. We have chosen calendar date as the underlying time dimension in the model, to handle seasonality effects like flu season, holidays, and other known or unknown seasonality effects that may otherwise introduce bias. Follow‐up started at the date of the ED visit and ended at death or at 30 days following the visit. A person could have more than 1 visit within a 30‐day period and if so, the later visits were ignored until the date after the previous 30‐day period ended (eg, left‐truncated), ensuring that no person contributed risk time more than once for each date. The model was adjusted for age, sex, triage priority, hour of arrival, weekend, arrival mode, chief complaint, hospital admissions last year, and comorbidities. Estimates were also calculated using a simplified model that did not include previous hospitalizations and comorbidities. Sensitivity analysis using the alternative exposure based on mean shift ED length of stay versus expected was performed using the same methodology as in the main analysis but with a different exposure. P value threshold for significance was set to 0.05. The original database linking registries was constructed with SAS software 9.4; further data management and statistical analyses were done with R version 3.6.1 using RStudio 1.1.463.
2.8. Ethical approval
The study was approved by the regional ethics committee in Stockholm. (2014/1822‐31/4)
3. RESULTS
3.1. Participants
Information from a total of 2,266,106 visits to the 7 EDs in Stockholm Region were included in the original database. In total 13,450 visits were excluded leaving 2,252,656 visits by 884,228 patients in the study population representing 99.4% of the original visits (Figure 1). In these remaining visits, there were 86,140 visits or 3.8% of the included visits that had no information on triage priority. The triage priority information was not missing at random as there was a higher proportion of missing values when the ED was crowded. These observations were therefore not removed from the dataset, instead an explicit category “missing” was introduced.
FIGURE 1.
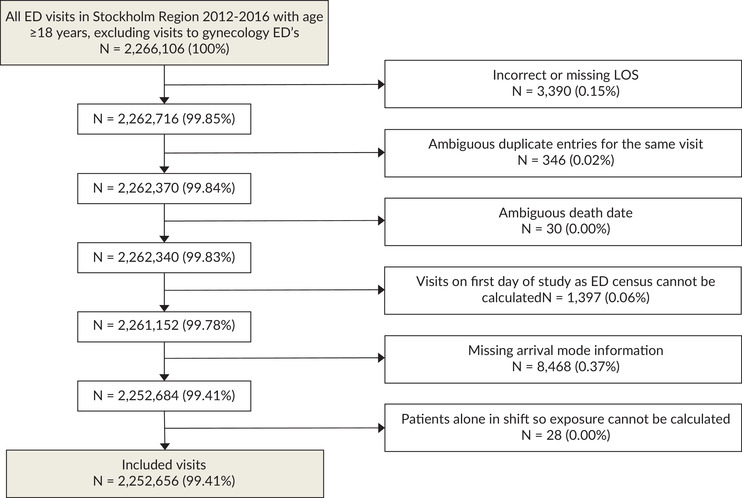
Process for inclusion and exclusion of patient visits. LOS, length of stay
3.2. Descriptive data
Median (Q1‐Q3) age for visits was 55 (36–72) years with 52% female visits. Patient characteristics were similar across the different categories of crowding with only a few exceptions. The proportion of visits with missing information on triage priority was higher in the higher categories of crowding, and the proportion of visits in the highest categories of crowding was higher during night and lower during the day. Crowding was also more common during weekdays and varied slightly between different years (Table 1).
TABLE 1.
Patient visit characteristics by crowding category
| Crowding category (ED census vs expected during shift) | |||||
|---|---|---|---|---|---|
| 0%–75% | 75%–95% | 95%–100% | Total | ||
| All visits, n | 1,689,520 | 450,535 | 112,601 | 2,252,656 | |
| Demographics, n (%) | |||||
| Age | 18–39 | 505,152 (29.9) | 131,954 (29.3) | 34,356 (30.5) | 671,462 (29.8) |
| 40–59 | 455,313 (26.9) | 122,598 (27.2) | 30,604 (27.2) | 608,515 (27.0) | |
| 60–79 | 471,814 (27.9) | 127,518 (28.3) | 31,573 (28.0) | 630,905 (28.0) | |
| 80 or older | 257,241 (15.2) | 68,465 (15.2) | 16,068 (14.3) | 341,774 (15.2) | |
| Sex | Female | 874,994 (51.8) | 233,895 (51.9) | 57,687 (51.2) | 1,166,576 (51.8) |
| Male | 814,526 (48.2) | 216,640 (48.1) | 54,914 (48.8) | 1,086,080 (48.2) | |
| Patient presentation at ED, n (%) | |||||
| Arrival mode | Emergency medical services | 466,224 (27.6) | 120,742 (26.8) | 31,834 (28.3) | 618,800 (27.5) |
| Walk‐in or other | 1,223,296 (72.4) | 329,793 (73.2) | 80,767 (71.7) | 1,633,856 (72.5) | |
| Priority | 1 | 93,306 (5.5) | 23,861 (5.3) | 5,994 (5.3) | 123,161 (5.5) |
| 2 | 206,249 (12.2) | 54,083 (12.0) | 14,243 (12.6) | 274,575 (12.2) | |
| 3 | 617,299 (36.5) | 166,440 (36.9) | 41,471 (36.8) | 825,210 (36.6) | |
| 4 | 564,839 (33.4) | 150,643 (33.4) | 38,270 (34.0) | 753,752 (33.5) | |
| 5 | 146,330 (8.7) | 36,134 (8.0) | 7,354 (6.5) | 189,818 (8.4) | |
| Missing | 61,497 (3.6) | 19,374 (4.3) | 5,269 (4.7) | 86,140 (3.8) | |
| Chief complaint | Abdominal pain | 191,552 (11.3) | 51,217 (11.4) | 13,498 (12.0) | 256,267 (11.4) |
| Arrythmia | 44,820 (2.7) | 12,440 (2.8) | 2,835 (2.5) | 60,095 (2.7) | |
| Cardiac arrest | 1,839 (0.1) | 479 (0.1) | 120 (0.1) | 2,438 (0.1) | |
| Chest pain | 136,716 (8.1) | 39,111 (8.7) | 9,680 (8.6) | 185,507 (8.2) | |
| Dyspnea | 106,693 (6.3) | 29,660 (6.6) | 7,696 (6.8) | 144,049 (6.4) | |
| Fever | 42,366 (2.5) | 10,908 (2.4) | 2,767 (2.5) | 56,041 (2.5) | |
| Head injury | 50,112 (3.0) | 12,870 (2.9) | 3,272 (2.9) | 66,254 (2.9) | |
| Hip injury | 28,838 (1.7) | 7,742 (1.7) | 1,857 (1.6) | 38,437 (1.7) | |
| Low consciousness | 3,205 (0.2) | 840 (0.2) | 196 (0.2) | 4,241 (0.2) | |
| Malaise | 41,548 (2.5) | 10,799 (2.4) | 2,424 (2.2) | 54,771 (2.4) | |
| Neurological deficit, stroke | 32,642 (1.9) | 8,687 (1.9) | 1,814 (1.6) | 43,143 (1.9) | |
| Peripheral edema | 94,518 (5.6) | 25,970 (5.8) | 5,469 (4.9) | 125,957 (5.6) | |
| Other | 914,671 (54.1) | 239,812 (53.2) | 60,973 (54.1) | 1,215,456 (54.0) | |
| Timing of visit, n (%) | |||||
| Shift | Day | 849,537 (50.3) | 224,887 (49.9) | 39,321 (34.9) | 1,113,745 (49.4) |
| Evening | 635,199 (37.6) | 170,027 (37.7) | 42,286 (37.6) | 847,512 (37.6) | |
| Night | 204,784 (12.1) | 55,621 (12.3) | 30,994 (27.5) | 291,399 (12.9) | |
| Weekend | Weekday | 1,023,246 (60.6) | 390,341 (86.6) | 93,620 (83.1) | 1,507,207 (66.9) |
| Weekend or holiday | 666,274 (39.4) | 60,194 (13.4) | 18,981 (16.9) | 745,449 (33.1) | |
| Year | 2012 | 338,987 (20.1) | 83,533 (18.5) | 24,354 (21.6) | 446,874 (19.8) |
| 2013 | 332,135 (19.7) | 91,281 (20.3) | 23,190 (20.6) | 446,606 (19.8) | |
| 2014 | 324,593 (19.2) | 90,447 (20.1) | 18,669 (16.6) | 433,709 (19.3) | |
| 2015 | 343,710 (20.3) | 93,580 (20.8) | 21,956 (19.5) | 459,246 (20.4) | |
| 2016 | 350,095 (20.7) | 91,694 (20.4) | 24,432 (21.7) | 466,221 (20.7) | |
| Patient history and comorbidities, n (%) | |||||
| Hospital admissions last year | 0 | 1,125,914 (66.6) | 302,007 (67.0) | 75,240 (66.8) | 1,503,161 (66.7) |
| 1 | 273,234 (16.2) | 72,824 (16.2) | 17,994 (16.0) | 364,052 (16.2) | |
| 2 | 116,198 (6.9) | 30,733 (6.8) | 7,699 (6.8) | 154,630 (6.9) | |
| 3 or more | 174,174 (10.3) | 44,971 (10.0) | 11,668 (10.4) | 230,813 (10.2) | |
| Comorbidities | Active cancer | 57,005 (3.4) | 14,929 (3.3) | 3,615 (3.2) | 75,549 (3.4) |
| Chronic kidney disease | 9,297 (0.6) | 2,664 (0.6) | 654 (0.6) | 12,615 (0.6) | |
| COPD | 24,782 (1.5) | 6,520 (1.4) | 1,675 (1.5) | 32,977 (1.5) | |
| Diabetes | 151,410 (9.0) | 40,712 (9.0) | 10,394 (9.2) | 202,516 (9.0) | |
| Heart failure | 45,756 (2.7) | 12,225 (2.7) | 3,155 (2.8) | 61,136 (2.7) | |
| Myocardial infarction | 62,039 (3.7) | 16,719 (3.7) | 4,345 (3.9) | 83,103 (3.7) | |
| Stroke | 68,613 (4.1) | 18,037 (4.0) | 4,549 (4.0) | 91,199 (4.0) | |
Characteristics of 884,228 patients with 2,252,656 visits to 7 emergency departments in Stockholm Region, Sweden, from 2012 to 2016, by crowding category. COPD, chronic obstructive pulmonary disease; ED, emergency department.
3.3. Outcome data/main results
There were 32,720 deaths within 30 days of the visit to the ED. The total time at risk was 156,836 person‐years and the average follow‐up time was 25 days. The overall incident rate was 20.9 cases/100 person‐years, with an incidence rate of 20.9 in the reference category 0%–75%, 20.6 in the category 75%–95% and 21.4 in the category 95%–100% (Table 2). The estimated hazard ratio (95% CI) in the adjusted model including prior hospital admissions and comorbidities was 1.00 (0.97–1.03) in the crowding category 75%–95% and 1.08 (1.03–1.14) in the 95%–100% category. The estimated hazard ratio (95% CI) in the reduced model without adjustments for hospitalizations and comorbidities was 1.00 (0.98–1.03) in the crowding category 75%‐95% and 1.08 (1.03–1.14) in the 95%‐100% category (Table 2).
TABLE 2.
Association between 30‐day mortality and crowding category (based on ED census vs expected)
| Crowding category (ED census vs expected during shift) | ||||
|---|---|---|---|---|
| 0%–75% | 75%–95% | 95%–100% | ||
| 30‐day mortality | Number of deaths, n | 24,551 | 6,482 | 1,687 |
| Person‐years at risk, n | 117,540 | 31,423 | 7,872 | |
| Incidence rate, cases/100 person‐years | 20.9 | 20.6 | 21.4 | |
| Adjusted a HR (95% CI) | Reference | 1.00 (0.98–1.03) | 1.08 (1.03–1.14) | |
| Adjusted b HR (95% CI) | Reference | 1.00 (0.97–1.03) | 1.08 (1.03–1.14) | |
Significant association between 30‐day mortality and the highest category of crowding 95%–100%, among 884,228 patients with 2,252,656 visits to 7 emergency departments in Stockholm Region, Sweden, from 2012 to 2016. Crowding category was based on ED census versus expected during the shift that the patient arrived
CI, confidence interval; ED, emergency department; HR, hazard ratio.
stratified by hospital, adjusted for age, sex, priority, weekend, hour, arrival mode, and chief complaint.
stratified by hospital, adjusted for age, sex, priority, weekend, hour, arrival mode, chief complaint, prior hospital admissions, and comorbidities.
3.4. Other analyses
When using the alternative exposure based on mean shift ED length of stay versus expected, the incidence rate was 20.5 cases/100 person‐years in the reference category 0%–75%, 21.5 in the category 75%–95% and 23.1 in the category 95%–100%. The estimated hazard ratio (95% CI) in the adjusted model including prior hospital admissions and comorbidities was 1.01 (0.98–1.04) in the crowding category 75%–95% and 1.08 (1.03–1.14) in the 95%–100% category (Table 3).
TABLE 3.
Association between 30‐day mortality and crowding category (based on ED LOS vs expected)
| Crowding category (ED LOS vs expected during shift) | ||||
|---|---|---|---|---|
| 0%–75% | 75%–95% | 95%–100% | ||
| 30‐day mortality | Number of deaths, n | 24,132 | 6,764 | 1,824 |
| Person‐years at risk, n | 117,511 | 31,440 | 7,885 | |
| Incidence rate, cases/100 person‐years | 20.5 | 21.5 | 23.1 | |
| Adjusted a HR (95% CI) | Reference | 1.01 (0.98–1.04) | 1.08 (1.02–1.14) | |
| Adjusted b HR (95% CI) | Reference | 1.01 (0.98–1.04) | 1.08 (1.03–1.14) | |
Significant association between 30‐day mortality and the highest category of crowding 95%‐100%, among 884,228 patients with 2,252,656 visits to 7 emergency departments in Stockholm Region, Sweden, from 2012 to 2016. Crowding category was based on mean ED LOS versus expected during the shift that the patient arrived.
CI, confidence interval; ED, emergency department; HR, hazard ratio; LOS, length of stay.
stratified by hospital, adjusted for age, sex, priority, weekend, hour, arrival mode, and chief complaint.
stratified by hospital, adjusted for age, sex, priority, weekend, hour, arrival mode, chief complaint, prior hospital admissions, and comorbidities.
4. LIMITATIONS
The key limitation of the study is the use of a retrospective observational study design that limits our causal inference and results may have been affected by unmeasured confounding. The study is based on extracts from the electronic health record with quality being dependent on the manual input of data. Although this may introduce bias we deem this risk to be small because of the large number of observations, past reliability of the data sources, 11 and the continual logical testing to ensure the quality and integrity of the data.
An important risk when investigating the association between crowding and mortality is if the proxy‐measure of crowding is associated with the severity and/or complexity of the patient. ED length of stay on its own is an example of a flawed proxy‐measure because older, sicker, and more complex patients tend to have both longer length of stay and higher mortality. We reduced the risk of similar bias through careful design of the proxy‐measures and by adjusting for potential confounding in the analysis phase. A strength of the proxy‐measure used is that patient characteristics are very similar across exposure categories with the exception of the timing of the visit. However, our definition of crowding based on ED census in relation to expected is new and has not been tested before, and we may have defined our exposure in a way that creates an unknown bias. We therefore performed a sensitivity analysis using an alternative crowding measure based on mean ED length of stay in relation to expected that yielded similar results. For both measures, we choose to define crowding on an ED‐level even if the internal resourcing of the ED may be organized in separate streams within the ED. This choice of methodology limits the complexity but may have reduced sensitivity as the workstreams within the EDs in the Stockholm Region are typically organized around medical specialities and one speciality may be relatively crowded while the rest of the ED is running at normal workload.
5. DISCUSSION
In a large cohort study in Stockholm, Sweden during 2012–2016 including 884,228 patients with 2,252,656 visits to any of the 7 EDs in the region, we found an association between crowding and increased all‐cause mortality within 30 days. Sensitivity analysis performing the same analysis but with a different definition of the exposure yielded similar results. The strengths of our study are the large number of observations, from multiple EDs, including all ED visits in the region for 5 years, sensitivity analysis using an alternative method for measuring crowding together with the high quality of our national patient registries.
Sun et al 6 studied 995,379 ED visits across California in 2007, resulting in an admission to inpatient care. The exposure to crowding was defined as those days within the top quartile of ambulance diversion hours for a specific facility. They found a 5% increased risk of inpatient mortality among the exposed. McCusker et al 6 studied 677,475 patient visits to 42 EDs in Quebec in 2005. The primary measure of crowding was the daily relative occupancy ratio for ED beds. They found that a 10% increase in the relative occupancy ratio was associated with a 3% increase in 30‐day mortality. We had different proxy‐measure of crowding and a richer dataset with information on patient acuity and intraday variation of crowding, but results were similar with a small, significant association between crowding and mortality. Guttmann et al 3 studied crowding through the association between ED waiting times and 7‐day mortality in a large cohort including almost 14 million patient visits in Ontario, Canada during 2003–2007. The study included only patients who were not admitted to inpatient care. Adjusted odds ratios for death within 7 days were significantly higher when mean ED length of stay during the same shift increased. This is also in line with our results, even if their choice of reference category for the exposure makes the relative risk difficult to compare. Verelst et al 9 performed a cohort study including 108,229 patient visits to an academic teaching hospital in Belgium that was highlighted in the most recent review. 1 In contrast to our results there was no significant association between their proxy‐measure for crowding and mortality. However, the study was from a single hospital and did not include enough observations to rule out an association at the level that we identified.
The simplified proportional hazards model that did not adjust for prior hospitalizations and comorbidities returned almost identical results as the fully adjusted model. This is an exciting finding as this radically reduces the complexity for researchers in other healthcare systems if they want to replicate the study in their own setting. The minimum data requirements in addition to information on mortality are patient age, sex, priority, arrival mode, chief complaint, and time of arrival. These data points are often available in the ED electronic health record without the need to capture historical care episodes across the entire healthcare system.
If our results were causal, it would imply 125 (95% CI: 49–207) excess deaths in the Stockholm region because of ED crowding during 2012–2016 equivalent to 6 (2–9) excess deaths per 100,000 ED visits. As a comparison, the cause‐of‐death statistics 13 for adults in Stockholm Region during the same period include 178 deaths related to transportation and 82 cases due to assault by another person. Furthermore, mortality may only be the tip of the iceberg. Behind each case there are likely to be more cases of morbidity 14 and mistakes 15 , causing pain 16 and suffering for patients together with stress 17 , burnout, and disatisfaction 18 among healthcare professionals.
In summary, we identified a significant association between ED crowding and 30‐day mortality in a large, multicenter cohort covering 99,4% of all adult ED visits for 5 years in the Stockholm region. Overcoming the combined limitations of previous studies, we included all patients visiting the ED and used 2 different types of exposure with a reference category that represented a normal state at the ED. Additionally we were able to control for detailed patient characteristics and intraday variation of crowding. Finally, we did not assume a linear relationship between crowding and mortality. A simplified methodology without comorbidities and previous hospital admissions was tested and resulted in similar results as the primary analysis. This enables researchers in other healthcare systems to replicate the study with less detailed covariate information. The study strengthens the evidence that ED crowding is associated with increased mortality.
AUTHOR CONTRIBUTIONS
Björn af Ugglas initiated the study. Martin J. Holzmann gained necessary ethical approvals. Björn af Ugglas, Therese Djärv, Petter L.S. Ljungman, and Martin J. Holzmann contributed to the design of the study. Björn af Ugglas and Martin J. Holzmann gathered and structured the dataset, Björn af Ugglas performed the analysis of the data with support from Martin J. Holzmann. Björn af Ugglas, Therese Djärv, Petter L.S. Ljungman, and Martin J. Holzmann did the interpretation of results. Björn af Ugglas drafted the manuscript. Björn af Ugglas, Therese Djärv, Petter L.S. Ljungman, and Martin J. Holzmann critically revised the manuscript and approved the manuscript to be submitted. Björn af Ugglas affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. Björn af Ugglas is the guarantor.
Biography
Björn af Ugglas, MSc, is a PhD student at Karolinska Institutet, Täby, Sweden.

af Ugglas B, Djärv T, Ljungman PLS, Holzmann MJ. Emergency department crowding associated with increased 30‐day mortality: a cohort study in Stockholm Region, Sweden, 2012 to 2016. JACEP Open. 2020;1:1312–1319. 10.1002/emp2.12243
Funding and support: The construction of the database used in this study was funded by an unrestricted grant from Idorsia Pharmaceutical. Dr. Djärv was supported by the Stockholm County Council (clinical research appointment). Dr. Ljungman was supported by Karolinska Institutet Strategic Research Area in Epidemiology (SFO Epidemiology), the Swedish Society for Medical Research, and the Swedish Research Council for Health, Working Life and Welfare (FORTE). Dr. Holzmann reports receiving consultancy honoraria from Actelion, Idorsia, and Pfizer. He holds research positions funded by the Swedish Heart‐Lung Foundation (grant 20170804) and the ALF agreement between the Stockholm County Council and Karolinska Institutet (grant 20170686).
[Correction added on 17 September 2020, after first online publication: the text “(95%‐100% of expected bed capacity)” is deleted from “The Bottom Line”.]
Supervising Editor: Elizabeth Donnelly, PhD, MPH.
REFERENCES
- 1. Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Berg LM, Ehrenberg A, Florin J, Ostergren J, Discacciati A, Goransson KE. Associations between crowding and ten‐day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019;74(3):345‐356. [DOI] [PubMed] [Google Scholar]
- 3. Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jo S, Jin YH, Lee JB, Jeong T, Yoon J, Park B. Emergency department occupancy ratio is associated with increased early mortality. J Emerg Med. 2014;46(2):241‐249. [DOI] [PubMed] [Google Scholar]
- 5. Mataloni F, Pinnarelli L, Perucci CA, Davoli M, Fusco D. Characteristics of ED crowding in the Lazio Region (Italy) and short‐term health outcomes. Intern Emerg Med. 2019;14(1):109‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCusker J, Vadeboncoeur A, Levesque JF, Ciampi A, Belzile E. Increases in emergency department occupancy are associated with adverse 30‐day outcomes. Acad Emerg Med. 2014;21(10):1092‐1100. [DOI] [PubMed] [Google Scholar]
- 7. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605‐11.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van der Linden N, van der Linden MC, Richards JR, Derlet RW, Grootendorst DC, van den Brand CL. Effects of emergency department crowding on the delivery of timely care in an inner‐city hospital in the Netherlands. Eur J Emerg Med. 2016;23(5):337‐343. [DOI] [PubMed] [Google Scholar]
- 9. Verelst S, Wouters P, Gillet JB, Van den Berghe G. Emergency department crowding in relation to in‐hospital adverse medical events: a large prospective observational cohort study. J Emerg Med. 2015;49(6):949‐961. [DOI] [PubMed] [Google Scholar]
- 10. Waxman DA, Husk G, Akhtar S, Krishnamurthy C. Hourly emergency department census: a simple measure of crowding. Ann Emerg Med. 2004;44(4):S19. [Google Scholar]
- 11. Ludvigsson JF, Otterblad‐Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659‐667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rothman KJ, Boice JD. Epidemiologic Analysis with a Programmable Calculator. U.S. Department of Health, Education, and Welfare, Public Health Service, National Institutes of Health; 1979. [Google Scholar]
- 13. The Swedish National Board of Health and Welfare. Cause of Death Statistics Available at: https://sdb.socialstyrelsen.se/if_dor/val.aspx. Accessed January 23, 2020.
- 14. Pines JM, Pollack CV Jr, Diercks DB, Chang AM, Shofer FS, Hollander JE. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009;16(7):617‐625. [DOI] [PubMed] [Google Scholar]
- 15. Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010;28(3):304‐309. [DOI] [PubMed] [Google Scholar]
- 16. Mills AM, Shofer FS, Chen EH, Hollander JE, Pines JM. The association between emergency department crowding and analgesia administration in acute abdominal pain patients. Acad Emerg Med. 2009;16(7):603‐608. [DOI] [PubMed] [Google Scholar]
- 17. Eriksson J, Gellerstedt L, Hillerås P, Craftman Åsa G. Registered nurses’ perceptions of safe care in overcrowded emergency departments. J Clin Nurs. 2018;27(5‐6):e1061‐e1067. [DOI] [PubMed] [Google Scholar]
- 18. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987‐1993. [DOI] [PubMed] [Google Scholar]


