Abstract
Objective
The objective of this study was to determine whether instituting an alternative to opioids (ALTO) protocol significantly reduced opioid use in emergency departments (EDs). The secondary objective was to determine whether patient‐reported pain and satisfaction were affected.
Methods
Electronic health records for 10 EDs in Colorado were retrospectively examined for the 6 months before the intervention and for the same 6 months the following year after the intervention, which consisted of systemic and educational initiatives in line with the Colorado American College of Emergency Physicians 2017 Opioid Prescribing and Treatment Guidelines.
Results
Of the total preintervention and postintervention unique patient visits, 47.2% received 1 of the drugs of interest, an opioid or ALTO, while in the ED. In aggregate, the EDs decreased opioid usage, measured in morphine equivalent units per 1000 ED visits, by 37.4% (95% confidence interval, 33.6%–76.2%; P < 0.0001) after the intervention. Statistically significant decreases were seen in every type of opioid. Statistically significant increases in ALTO usage were also noted across all study hospitals. There were no significant changes observed in Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction scores before and after the intervention in the hospitals with Hospital Consumer Assessment of Healthcare Providers and Systems data (preintervention mean, 3.74; postintervention mean, 3.74; P = 0.637), and there was a small but statistically significant improvement in pain scores (preintervention mean, 3.62; postintervention mean, 3.66; P = 0.002). In a subgroup analysis of patients presenting with chief complaints of long bone fractures and malignant neoplasms, there were no significant reductions in opioid use.
Conclusions
This study demonstrated the feasibility and effectiveness of implementing ALTO protocols to reduce opioid use in the ED setting without an overall reduction in patient perception of pain or satisfaction with care.
Keywords: ALTO, emergency department, opioid reduction, opioids, pain
1. INTRODUCTION
1.1. Background
The Joint Commission called for healthcare organizations to improve pain control in 2000 following reports from the American Pain Association and the Veterans Health Administration that recommended pain be treated as a “fifth vital sign.” 1 An unintended consequence was a dramatic increase in the rate of opioid prescribing by physicians followed by equally dramatic increases in rates of opioid use disorders and overdose deaths. From 1999 to 2017, >218,000 Americans died from prescription opioid overdoses. In 2017, there were 58.5 opioid prescriptions for every 100 Americans. 2 Furthermore, from 2008 to 2010, more than 4 of 5 frequent nonmedical opioid pain reliever users who also used heroin in the previous year started using prescription opioids prior to heroin, 3 and a 2008 to 2009 study of young urban injection drug users found 86% used non‐medical prescription opioids prior to heroin, with the sources including family, friends, and personal prescriptions. 4 In 2016, the Centers for Disease Control and Prevention released guidelines for prescribing opioids for chronic pain, noting that non‐opioid therapy is preferred. 5 Even a single‐day prescription of opioids has been shown to have a 6% chance of continued opioid use at 1 year 6 ; 2001 to 2010 saw an ≈50% increase in opioid prescriptions from emergency departments (EDs), 7 and clinical guidelines in 2012 acknowledged the lack of evidence to guide many therapeutic decisions to use opioids. 8
1.2. Importance
There are >135 million ED visits per year, 9 and more than half of ED patients report pain as a complaint. 10 , 11 More educated patients are less likely to receive opioids from the ED. 12 Brief educational interventions for physicians have been shown to decrease opioid prescription after surgery. 13 Although one study showed that effective pain management inside the ED was associated with increased patient satisfaction, 14 another study of 2 EDs showed that giving opioid or non‐opioid pain medications in the ED was not independently associated with Press Ganey ED satisfaction scores. 15 Interestingly, other non‐ED studies have shown that patient satisfaction does not correlate with clinical outcomes. 16
Because of the increasingly recognized harms associated with routine opioid use, there have been attempts to create ED protocols that use alternatives to opioids (ALTO) as first‐line pain medications for those conditions where alternatives are effective. The first ED ALTO program was developed and implemented at St. Joseph's Regional Medical Center in Paterson, NJ, in 2016 and reduced ED opioid use by 38%. 17 , 18 Similar ALTO pathways were published in the Colorado American College of Emergency Physicians (COACEP) 2017 Opioid Prescribing and Treatment Guidelines and piloted by the Colorado Hospital Association (CHA). Predicated on these the efforts in New Jersey and Colorado and recognizing the opportunity to decrease harm, in 2018 Congress passed the ALTO in the Emergency Department Act, which “requires the Department of Health and Human Services to carry out a 3‐year demonstration program awarding grants to hospitals and EDs to develop, implement, enhance, or study alternative pain management protocols and treatments that promote limited use of opioids in EDs.” 19
The Bottom Line
The use of an alternative to opioids protocol and brief educational intervention significantly reduced opioid use in emergency departments without affecting patient‐reported pain and satisfaction surveys.
1.3. Goals of this investigation
The St. Joseph's ALTO and CHA models use a multidisciplinary approach to implementing ALTO, including developing electronic order “bundles” that made ordering non‐narcotic pain medications easier as well as educating pharmacists, nurses, nurse practitioners, physician assistants, and physicians on the data supporting use of ALTO medications. The primary purpose of this study is to determine effectiveness in reducing opioid use in 10 Colorado EDs by implementing educational and systemic interventions as outlined in the COACEP 2017 Opioid Prescribing and Treatment Guidelines. Secondary objectives include determining whether patient self‐reported pain control and satisfaction differed before and after the intervention, as measured by Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores.
2. METHODS
2.1. Study design and setting
This was a preintervention and postintervention study design comparing in‐ED opioid and non‐opioid use as well as HCAHPS responses about satisfaction and pain control. Data collection took place for the 6 months before the intervention and for the same 6 months of the following year to reduce seasonal variability.
2.2. Selection of participants
A CHA ad hoc committee solicited EDs to participate. Of 20 applicants, 10 EDs were chosen to present a diversity of clinical practice environments and patient populations (see Table 1). Reasons for excluding hospitals included lack of support from senior executives, lack of responsiveness to the committee, and an unwillingness to share data.
TABLE 1.
Characteristics of participating facilities
| ED | Licensed hospital beds | CMS urban/rural designation | CMS hospital type | No. ED visits a | Trauma designation |
|---|---|---|---|---|---|
| 1 | 408 | Urban | Acute care | 59,972 | Level I b |
| 2 | 39 | Rural | Acute care | 7921 | Level IV b |
| 3 | N/A | Urban | N/A‐freestanding ED | 11,821 | None b |
| 4 | N/A | Urban | N/A‐freestanding ED | 24,005 | None b |
| 5 | 15 | Rural | Critical access | 1023 | Level IV |
| 6 | 284 | Urban | Acute care | 33,986 | Level II |
| 7 | 174 | Urban | Acute care | 31,535 | Level II b |
| 8 | 178 | Urban | Acute care | 33,943 | Level I |
| 9 | 225 | Urban | Acute care | 52,735 | Level III c |
| 10 | 24 | Rural | Critical access | 6743 | Level IV c |
CMS, Centers for Medicare and Medicaid Services; ED, emergency department; N/A, not applicable.
Total number of ED visits for preintervention and postintervention time periods.
Missing 1 month of preintervention Hospital Consumer Assessment of Healthcare Providers and Systems data.
No Hospital Consumer Assessment of Healthcare Providers and Systems data available.
2.3. Interventions
The intervention took place from December 1, 2016, until May 31, 2017, and consisted of providing participating EDs with an ALTO checklist explaining roles, timelines, and educational interventions and creating an electronic ALTO order set. 20 The CHA required participating EDs to provide a “clinical champion” to assure the adoption of practices and fulfillment of deadlines for participation, and roles were delineated for the ED medical director, ED physician or physician assistant or nurse practitioner, ED nurse, pharmacy director, quality improvement champion, communications and marketing director, IT champion, and data support.
The following 2 educational interventions were provided by CHA to each participating hospital: (1) 1 half day of in‐person, peer‐to‐peer, non‐mandatory training was provided by CHA to each participating hospital's ED physicians, physician assistants, nurse practitioners, nurses, and pharmacists; and (2) online webinars tailored to each of the 3 peer groups were made freely accessible but were non‐mandatory. 21
Each hospital was required to create a new electronic order pathway for non‐opioid pain medication administration in the ED in accordance with the COACEP 2017 Opioid Prescribing and Treatment Guidelines. 22 All participating EDs had electronic medical records that required electronic ordering of medications given in the ED, none of which had a standard order set for non‐opioid pain medication prior to the intervention. Each ED's pharmacy department determined how best to implement the guidelines, and no medications or specific dosages were required for participation.
2.4. Measurements
There was a standard data collection process where each of the participating hospitals submitted 3 specific reports on a monthly basis. One contained de‐identified medication administration per patient, another contained the total number of ED visits, and the last contained HCAHPS scores for the 2 questions of interest. Data were collected for 6 months preintervention from June 1, 2016, to November 30, 2016, and for the same 6 months in the year after the intervention, from June 1, 2017, to November 30, 2017. Data were provided from electronic health record data extracts according to specifications provided by the CHA. Details of the data extracts are available from the authors upon request. A local clinical data expert was engaged from each participating site. One site abstracted pharmacy records by hand because of insufficient reporting capability from their electronic health record. Data were validated by local clinical informatics personnel and were again reviewed by the CHA data team. HCAHPS scores were collected by a third party and reported to the hospital. They were subsequently obtained from the appropriate local administrator. Use of pain pathways was identified using CHA's claims database from a list of International Classification of Diseases Tenth Revision codes that are available upon request. Patient diagnosis and demographics were obtained from claims data. Data were shared under individual data use agreements between CHA and each member hospital or health system.
2.5. Outcomes
Medications described as “ALTOs” are non‐opioid medications used for the purpose of analgesia and identified in the COACEP 2017 Opioid Prescribing and Treatment Guidelines. 22
Each administration of a drug of interest (see Figure 1) was considered to be a pharmacologic pain intervention. Opioid pain medications were converted to morphine equivalent units (MEUs). 23 Only medications administered in the ED were included in the analysis. Every instance and dosage of opioid and non‐opioid analgesic administration in the ED were recorded; data from patients who received both opioid and non‐opioid analgesics in the same visit was included. If a medication dose contained both an opioid and a non‐opioid, such as with acetaminophen/oxycodone, it was counted as an opioid.
FIGURE 1.
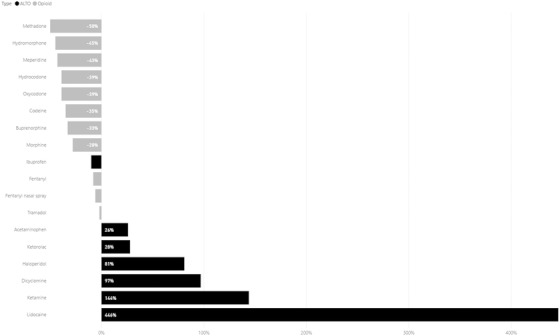
Percent change in measured medication administrations from baseline
Additional secondary outcomes included scores on 2 ED patient satisfaction questions from the HCAHPS survey, which is required for all acute care hospitals in the United States by the Centers for Medicare and Medicaid Services. Hospitals reported results from patients discharged from the ED during the baseline and intervention periods regarding a question about how well pain was controlled (1 = never, 2 = sometimes, 3 = usually, 4 = always) and a question about the likelihood of recommending this ED (1 = no, 2 = probably no, 3 = probably yes, 4 = definitely yes). 24
Encounter‐level data elements included date of service, principal visit diagnosis, age, and sex. It is important to note that HCAHPS scores were for all ED patients during the time period and not just those who received opioids or ALTO for pain.
2.6. Analysis
Alteryx version 2018.4 was used for all data analysis and statistics. A paired Wilcoxon signed rank test was conducted on the preintervention and postintervention data to determine P values. Preintervention and postintervention measurement periods were 1 year apart but occurred during the same 6‐month range.
Each hospital agreed to participate in the intervention as part of a quality improvement initiative led by CHA. A data‐sharing agreement with CHA enabled sharing and publication of de‐identified data. For data extraction and publication purposes, institutional review boards at Swedish Hospital and the University of Colorado approved the study.
3. RESULTS
The 10 participating EDs are described in Table 1. The EDs included 6 acute care hospital EDs, 2 critical access hospital EDs, and 2 freestanding EDs affiliated with hospital systems. Three EDs were affiliated with rural hospitals and 7 with urban hospitals. The EDs ranged in volume from 4164 to 59,753 annual visits (median 26,297). All 10 EDs completed the intervention and retrospective data sharing. During the course of the 6‐month postintervention period, the 10 EDs saw a total of 130,700 unique patient visits. This volume was comparable to the preintervention 6‐month period in the prior year (n = 131,765). Of the total preintervention and postintervention unique patient visits, 47.2% received one of the drugs of interest, an ALTO or opioid, while in the ED.
In aggregate, the EDs decreased opioid usage (MEUs per 1000 ED visits) by 37.4% (95% confidence interval [CI], 33.6%–76.2%; P < 0.0001) between 2017 and the comparable 6‐month period in 2016. This represented 35,000 fewer opioid administrations during 2017 versus 2016. Furthermore, reductions in opioid use in MEUs per visit demonstrated an overall trend of decreased opioid usage as the pilot progressed (Figure 2). Individual ED results ranged from 31% to 46% reductions in opioids administered during our study period (Figure 1). It was also noted that total analgesic medication administrations decreased by 4.5%.
FIGURE 2.
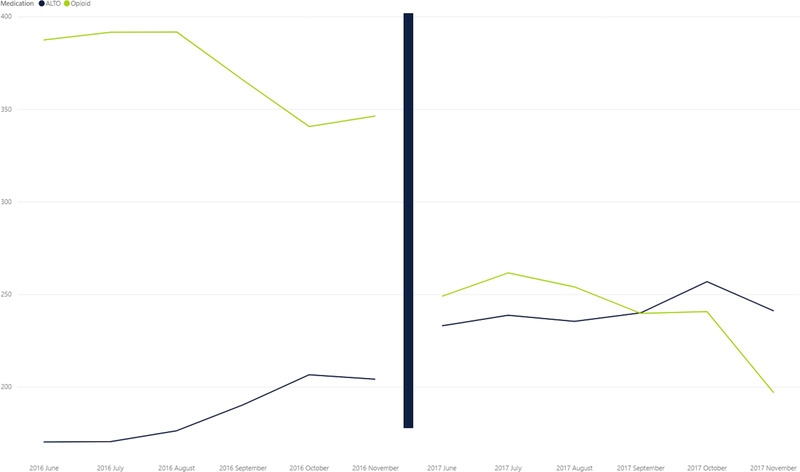
ALTOs vs Opioid use over time, by month
The COACEP 2017 Opioid Prescribing and Treatment Guidelines call for ALTOs to be used as first‐line agents for nearly all painful conditions and for opioids to be used as second line or rescue drugs for pain management. After implementation of the COACEP protocols, ALTO use became more common for treated pain visits than opioid use within the first month of the pilot. In fact, there was a 28.1% reduction in total number of ED pain visits treated with opioids per 1000 ED visits (P < 0.0001; incidence rate ratio, 0.719; 95% CI, 0.707–0.730), whereas there was a 16.4% increase in total number of ED visits treated with ALTOs per 1000 ED visits (P < 0.0001; incidence rate ratio, 1.164; 95% CI, 1.145–1.184).
Guideline‐supported changes in prescribing were seen across nearly every medication tracked (Figure 1). EDs reduced administrations of all opioid medications, except for tramadol, which was unchanged. In contrast, EDs increased administration of each measured ALTO medication, except for ibuprofen, which decreased (−13.4%; P < 0.0001). Increases were particularly dramatic in the administration of intravenous lidocaine (+493%; P < 0.0001) and ketamine (+144%; P < 0.0001).
Regarding condition‐specific pathways described in the COACEP 2017 Opioid Prescribing and Treatment Guidelines, there was significant progress in emergency clinician adoption of this guidance between 2016 and 2017. In 2016, opioids were the predominant medication used to treat low back pain/lumbago (58.0%), kidney stones (59.7%), and unspecified abdominal pain (64.0%); after the interventions, ALTOs matched or surpassed opioids in treating these painful conditions (42.0%, 40.3%, and 36.0% used ALTOs, respectively; P values < 0.0001). In the case of headaches/migraine where ALTOs were used more than opioids prior to the pilot, there was still a large decrease in opioid usage (39.2% pre vs 20.2% post; P < 0.0001). Finally, for severe pain such as extremity fractures and pain associated with malignant neoplasms, opioid administration did not significantly decrease (extremity fractures 75.3% vs 72.1%, P = 0.867; malignant neoplasms 89.4% vs 80.5%, P = 0.174), although ALTOs were used more frequently for these indications than in 2016 (Table 2).
TABLE 2.
Comparison of opioid usage per pain pathway
| Pain pathway | Baseline (%) | Postintervention (%) |
|---|---|---|
| Extremity fractures | 75.3 | 71.1 |
| Headaches/migraine* | 39.2 | 20.2 |
| Kidney stones* | 59.7 | 40.3 |
| Low back/lumbago pain* | 58.0 | 42.0 |
| Malignant neoplasms | 89.4 | 80.5 |
| Unspecified abdominal pain* | 64.0 | 36.0 |
* P < 0.05.
One hospital did not have HCAHPS scores, and 4 of the remaining 9 were missing 1 month of postintervention scores and changed their HCAHPS questions for the last 2 months of the postintervention timeline. HCAHPS data from these 4 hospitals, after the patient satisfaction scores were changed, was excluded from analysis (Table 1). Hence, there was complete HCAHPS data for 5 sites, incomplete data for 4 sites, and no data from 1 site. When the data were aggregated and analyzed, there was a small but statistically significant increase in HCAHPS scores for pain control between the baseline (mean, 3.62; SD, 0.80) and project period (mean, 3.66; SD, 0.79); P = 0.002. There was also no significant difference in HCAHPS scores for recommending the ED between the baseline (mean, 3.74; SD, 0.70) and project period (mean 3.74; SD, 0.72); P = 0.637.
4. LIMITATIONS
The limitations of this study include the retrospective data‐collecting approach. All administrations of a medication that was an opioid or on the ALTO medication list was presumed to be given for pain; because of the complexity of the medical charting, this assumption ignored other reasons for giving these medications, such as giving haloperidol for a psychiatric illness or ibuprofen for fever control or lidocaine for a heart arrhythmia. Lastly, the HCAHPS data provided were incomplete because of administrative changes within one of our participating hospital systems.
5. DISCUSSION
The observed reductions in MEUs per 1000 ED visits of 37.4% was significant and substantial across all participating EDs, ranging from 31% to 46% after implementation of ALTO protocols. Despite these reductions in opioid use and increase in ALTO use, there were no differences in HCAHPS satisfaction scores before and after the intervention, and there was a small but statistically significant improvement in patient assessment of how well their pain was controlled in the ED. These findings across 10 EDs seem to suggest that implementing ALTO guidelines is feasible and effective.
The degree of reduction in opioid use observed was 37.4% and is in line with previous research showing reductions of 38%. 18 Showing such a large impact with minimal external investment in the systems demonstrates the effectiveness and potential scalability of implementing ALTO protocols. With such a large number of patients presenting to EDs in pain, ALTO protocols offer a substantial opportunity to reduce patient opioid exposure. Future research is warranted to investigate the role of ALTO protocols on reducing rates of opioid prescribing at the time of discharge from the ED.
The results of our study must be interpreted in the context of a changing landscape of clinician and patient beliefs about opioids and pain treatment in the wake of the opioid crisis. Opioid use by clinicians was already decreasing in 2016 a total of 14% from June 2016 to November 2016 of our preintervention period. As there are no control EDs, it is possible that some of the reduction in opioid use in the ED we documented was the result of an existing trend toward reducing use of opioids (ie, secular trend). Nonetheless, the magnitude and uniformity across medications, diagnoses, and EDs suggest a marked effect of the intervention.
Furthermore, although the HCAHPS data set is incomplete, we can state that in the EDs providing HCAHPS scores, the results were promising with no change in patients’ recommending a hospital and small but significant improvements in the perception of pain control. Our study adds to the scientific literature showing no relation between opioid usage and patient satisfaction. 25 , 26 There are other potential balancing measures, such as ED length of stay and opioid‐related adverse events, that were not measured in this pilot and are potential targets for future study. Likewise, although the use of opioids while patients were treated in the ED was studied, discharge prescriptions were not monitored, and it is unknown whether implementation of ALTO protocols decreased opioid prescriptions from the ED.
There is great potential to replicate this intervention across the country as part of a comprehensive response to the opioid epidemic. 27 Doing so would help decrease opioid use on a large scale in little time and would provide a model for reducing unnecessary opioid use in other medical settings.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Donald Stader, Heidi Wald, Diane Rossi MacKay, Alexandra Mannerings, and Robert Valuck conceived of the retrospective study of the impact of implementation of the Alternative to Opioids Guidelines issued by the Colorado American College of Emergency Medicine. Donald Stader and Diane Rossi MacKay primarily oversaw the implementation of the guidelines. Diane Rossi MacKay and Alexandra Mannerings obtained research funding. Heidi Wald, Diane Rossi MacKay, Alexandra Mannerings, and Dominick Kuljis performed data collection and analysis. Mark F. Brady and Donald Stader drafted the manuscript, and all authors contributed substantially to its revision. Donald Stader takes responsibility for the paper as a whole.
Biography
Donald Stader, MD, is an emergency physician at Swedish Medical Center in Englewood, CO; is the Senior Pain Management & Opioid Policy Physician Advisor with the Colorado Hospital Association; and is President of Stader Opioid Consultants LLC.
Stader D, Wald H, MacKay DR, et al. Alternatives to opioid protocols in Colorado emergency departments reduce opioid use without changing reported pain. JACEP Open. 2020;1:1493–1499. 10.1002/emp2.12263
Funding and support: The analyses upon which this report is based were performed under Contract Number HHSM‐500‐2016‐00067C, titled “Hospital Improvement and Innovation Network (HIIN),”and sponsored by the Centers for Medicare & Medicaid Services, Department of Health and Human Services.
Supervising Editor: Karl A. Sporer, MD.
REFERENCES
- 1. Baker DW. History of the joint commission's pain standards: lessons for today's prescription opioid epidemic. JAMA. 2017;317(11):1117‐1118. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . 2018 Annual Surveillance Report of Drug‐Related Risks and Outcomes—United States. Surveillance Special Report. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2018. https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf. Accessed November 1, 2019. [Google Scholar]
- 3. Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1‐2):95‐100. [DOI] [PubMed] [Google Scholar]
- 4. Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23(1):37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016;315(15):1624‐1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long‐term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mazer‐Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med. 2014;21(3):236‐243. [DOI] [PubMed] [Google Scholar]
- 8. Cantrill SV, Brown MD, Carlisle RJ, et al. Clinical policy: critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60(4):499‐525. [DOI] [PubMed] [Google Scholar]
- 9. Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2017 emergency department summary tables. National Center for Health Statistics. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf.
- 10. Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165‐169. [DOI] [PubMed] [Google Scholar]
- 11. Tanabe P, Buschmann M. A prospective study of ED pain management practices and the patient's perspective. J Emerg Nurs. 1999;25(3):171‐177. [DOI] [PubMed] [Google Scholar]
- 12. Platts‐Mills TF, Hunold KM, Bortsov AV, et al. More educated emergency department patients are less likely to receive opioids for acute pain. Pain. 2012;153(5):967‐973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018;267(3):468‐472. [DOI] [PubMed] [Google Scholar]
- 14. Bhakta HC, Marco CA. Pain management: association with patient satisfaction among emergency department patients. J Emerg Med. 2014;46(4):456‐464. [DOI] [PubMed] [Google Scholar]
- 15. Schwartz TM, Tai M, Babu KM, Merchant RC. Evaluating the relationship between opioid analgesics and patient satisfaction among emergency department patients. Ann Emerg Med. 2013;62(4):S126‐S127. [Google Scholar]
- 16. Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172(5):405‐411. [DOI] [PubMed] [Google Scholar]
- 17. Hoffman J. An E.R. kicks the habit of opioids for pain New York Times. June 14, 2014:D1. [Google Scholar]
- 18.Rosenberg, M. Alternatives to Opiates (ALTO) program. https://www.aha.org/system/files/content/16/16behavhealthcaseex-stjosephs.pdf. Published 2016. Accessed November 1, 2019.
- 19. Alternatives to Opioids (ALTO) in the Emergency Department Act, S. 2516, 115th Cong. (2018).
- 20. Colorado Hospital Association . Using Alternatives to Opioids (ALTOs) in hospital emergency departments: pre‐launch checklist. https://cha.com/wp-content/uploads/2018/01/CHA-Opioid-Checklist.pdf. Published 2018. Accessed November 1, 2019.
- 21. Colorado Hospital Association . Clinician training materials. https://cha.com/clinician-training-materials/. Published 2018. Accessed November 1, 2019.
- 22. Stader DE , ed. Colorado American College of Emergency Physicians 2017 Opioid Prescribing & Treatment Guidelines. Colorado American College of Emergency Physicians; 2017:12‐16. https://coacep.org/docs/COACEP_Opioid_Guidelines-Final.pdf. Accessed November 1, 2019.
- 23. Centers for Medicare and Medicaid Services . Opioid morphine equivalent conversion factors; 2015. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-March-2015.pdf. Accessed November 1, 2019.
- 24. Health Services Advisory Group . Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey. https://www.hcahpsonline.org/globalassets/hcahps/survey-instruments/mail/jan-1-2018-and-forward-discharges/click-here-to-view-or-download-the-updated-english-survey-materials..pdf. Published 2018. Accessed November 1, 2019.
- 25. Sharp AL, Shen E, Wu YL, et al. Satisfaction with care after reducing opioids for chronic pain. Am J Manag Care. 2018;24(6):e196‐e199. [PubMed] [Google Scholar]
- 26. Hallway A, Vu J, Lee J, et al. Patient Satisfaction and Pain Control Using an Opioid‐Sparing Postoperative Pathway. J Am Coll Surg. 2019;229(3):316‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Murray M, Stone A, Pearson V, Treisman G. Clinical solutions to chronic pain and the opiate epidemic. Prev Med. 2019;118:171‐175. [DOI] [PubMed] [Google Scholar]


