Abstract
Objective
Symptomatic knee osteoarthritis (OA) and meniscal tear are often treated with weight-bearing exercises and without ordering advanced imaging (e.g. MRI). This may lead to missed diagnoses of subchondral insufficiency fracture of the knee (SIFK). Failure to diagnose SIFK has treatment implications, as patients with SIFK are typically managed with a period of reduced weight-bearing. The primary objective of this study is to determine the prevalence of undiagnosed SIFK among persons treated non-operatively for knee pain and suspected meniscal tear(s).
Methods
The randomized controlled trial, TeMPO (Treatment of Meniscal Problems and Osteoarthritis), enrolls subjects whose clinicians suspect concomitant meniscal tear and knee OA. TeMPO participants undergo MRI ordered by the study to confirm meniscal tear. All study-ordered MRIs revealing a fracture were reviewed by two study radiologists who noted features of the fracture and joint. We report prevalence of SIFK and clinical and imaging features on these subjects with 95% confidence intervals.
Results
Ten of the 340 study-ordered MRIs had SIFK, resulting in an estimated prevalence of 2.94% (95% CI: 1.15%, 4.71%). Eight of the ten participants with SIFK had fractures located medially. The femur was involved in five of these participants, tibia in four, and both in one. Five of the ten participants did not have meniscal tears.
Conclusions
This is the only reported estimate of undiagnosed SIFK in adults with knee pain, to our knowledge. Approximately 3% of patients managed with weight-bearing exercise for suspected meniscal tear may have SIFK, a diagnosis typically treated with reduced weight-bearing approaches.
Keywords: Subchondral insufficiency fracture, Knee, Non-surgical management, Magnetic resonance imaging, Osteoarthritis
1. Introduction
Many middle age adults experience disabling knee pain that could have a variety of origins. One of the most frequent sources of disabling knee pain in persons over 50 years of age is symptomatic knee osteoarthritis (OA), which affects approximately 14 million adults in the United States [1]. Plain radiographs are typically used as the initial imaging evaluation to investigate sources of knee pain in middle-aged and older persons with knee pain. While advanced imaging (e.g. magnetic resonance imaging [MRI]) better demonstrates lesions of the meniscus, synovium, ligaments and other structures compared to radiographs, it is seldom ordered for the initial management of persons with knee pain and suspected symptomatic knee OA in the clinical setting [2].
Some problems associated with pain in middle aged and older persons, including subchondral insufficiency fracture of the knee (SIFK), call for a different approach to management than is typically used with OA and many other sources of knee pain. Patients with SIFK present with weight-bearing pain due to the overloading of the subchondral bone of the femoral condyle or tibia. These patients often have concomitant meniscal or chondral injuries [3]. This fracture may progress to the point of collapse at the subchondral bone plate or spontaneous osteonecrosis of the knee [3,4]. One salient feature of SIFK is that this condition often cannot be detected by plain radiographs. While the treatment for SIFK is not widely agreed upon, physicians often treat patients with these fractures differently than patients with knee OA in the absence of SIFK. Specifically, weight-bearing exercises are recommended for knee OA while treatment recommendations for SIFK often involve a period of reduced weight-bearing in order to permit fracture healing [5]. Because the treatment of knee OA is generally undertaken without obtaining MRIs, cases of SIFK can be missed and treated inappropriately.
There have been no studies, to our knowledge, that have examined the prevalence of SIFK in persons with knee pain who are presumed to have meniscal tear(s) with or without symptomatic knee OA. Such studies would require investigators to obtain MRI scans in subjects with knee pain who would not ordinarily receive MRI. In our current randomized controlled trial of nonoperative treatment of symptomatic knee OA and meniscal tear(s), the trial protocol requires all potentially eligible subjects to undergo MRI to confirm the presence of meniscal tear(s). These MRIs permitted us to identify unsuspected SIFK in patients treated nonoperatively who would not otherwise have undergone MRI as part of routine clinical management. Thus, the purpose of this study was to determine the prevalence of unsuspected SIFK among persons managed nonoperatively for knee pain and presumed meniscal tear.
2. Methods
Setting: Treatment of Meniscal Problems and Osteoarthritis (TeMPO) is an ongoing multicenter, randomized controlled trial examining non-surgical interventions in persons with meniscal tears and knee osteoarthritis [6]. The two largest recruiting sites are academic orthopedic practices in Boston, MA, and Buffalo, NY. The data coordinating center is located in Boston, MA.
Sample: Subjects between 45 and 85 years of age with knee pain, no prior meniscal surgery on the index knee, Kellgren-Lawrence (KL) radiographic grade 0–3, and whom the enrolling physician believes to have symptomatic meniscal tear are potentially eligible for the study. To confirm a subject's eligibility, MRI is used to determine whether a meniscal tear is present. MRIs can be ordered two ways: (1) The subject's clinician can order the MRI for clinical purposes; (2) The study team can order the MRI to confirm eligibility if the clinician is comfortable treating the patient nonoperatively without MRI. These study-ordered MRIs would not be performed initially if the patient were not participating in the TeMPO Trial. Subjects undergoing study-ordered MRIs formed the sample for this analysis.
MRI Reading: Study-ordered MRIs were read by fellowship-trained musculoskeletal radiologists at each site. The radiologists dictate formal readings, which were uploaded to the electronic medical record. Research personnel at the Boston and Buffalo sites reviewed the radiologists’ formal readings on study-ordered MRIs and identified all MRIs in which the radiologist noted the presence of fracture. The MRIs with fractures in Buffalo were deidentified, downloaded onto a compact disk, and mailed to the Boston center. Using the grading system of Sayyid et al. to categorize each subject as having SIFK (grade 2–4 from Sayyid et al.) or not (grade 1) [7], two fellowship-trained musculoskeletal radiologists (SES and NS, with 20 and 10 years of experience, respectively) jointly reviewed all MRIs that mentioned fracture on the formal report. The imaging protocol for the study-ordered MRIs at each center included multiplanar T2 and proton density sequences with and without fat suppression and an isotropic proton density acquisition of the knee. They reached consensus on determination of each imaging feature of the review. The diagnosis of SIFK was assigned to patients who had a fracture line sub-adjacent to the articular cartilage with surrounding edema. The radiologists excluded fractures that were not subchondral in location. The data form included location of the fracture (femoral vs. tibial, medial vs. lateral), bone marrow edema distribution within the epiphysis (<25% of the transverse width of the epiphysis, 25–50%, >50–75%, or >75%), presence of a meniscal tear (none, medial, lateral or both), cartilage degenerative changes (none, partial, or full thickness), and presence of discrete subchondral cysts and other bone marrow lesions in any medial or lateral compartment of the femur or tibia (no, yes) beyond the bone edema generally seen with these fractures.
Other Patient Features: We obtained demographic characteristics (age, sex, race, body mass index) from subjects' baseline questionnaires and the five-item Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score as assessed during in-person or over the phone screening of the subjects for the TeMPO Trial. The subjects’ KL grade was assigned by their clinician based on radiographs that were taken either on the day of their clinic visit or within the month preceding the visit.
Analysis: We used descriptive statistics to portray subject demographics, MRI characteristics, and WOMAC pain scores. We estimated the prevalence of undiagnosed SIFK as the number of cases of SIFK divided by the number of study-ordered MRIs reviewed and multiplied by 100 to obtain a percentage. We calculated a 95% confidence interval (CI) around prevalence in Microsoft Excel (Version 1808) using the normal approximation of binomial distribution. For context, we provide the percent sex, race, and KL grade, and mean age and WOMAC pain of participants who were randomized in the TeMPO Trial.
3. Results
Throughout the first 22 months of study enrollment, 340 TeMPO study-ordered MRIs were completed at the Boston and Buffalo centers. Of these MRIs, 14 were initially suspected to have SIFK based on mention of fracture in the formal readings. These scans were reviewed in detail by the study radiologists in Boston. Four of 14 MRIs were excluded: two did not have a fracture, and two had fractures that were not subchondral. Ten of 340 study MRIs were confirmed to have SIFK, resulting in an estimated prevalence of undiagnosed SIFK of 2.94% (95% CI: 1.15%, 4.71%) in the population of persons with knee pain and suspected meniscal tear. Self-reported characteristics of the 10 subjects with SIFK are presented in Table 1. The median age was 61 years old (range 52–79), and 6 out of 10 subjects (60%, 95% CI: 29.6%, 90.4%) were female. Four out of 10 subjects were KL grade 3 based on radiographs, one subject was KL 2, four were KL 1, and one subject was KL 0. The median baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score was 48 (range 25–65) on a 100-point scale with 100 being the worst. Of the 462 participants randomized in the TeMPO Trial during this time period, 56% were female, 88% were white, 41% were KL 3, the mean age was 59 years, and the mean WOMAC pain score was 47.
Table 1.
Subject and MRI characteristics (n = 10).
| Subject Characteristics | |
|
Characteristic |
Value |
| Age, median (range) [yrs] | 61 (52–79) |
| Sex [number of subjects] | |
| Female | 6 |
| Male | 4 |
| Race [number of subjects] | |
| White | 7 |
| Black | 1 |
| Asian | 1 |
| Unknown | 1 |
| Kellgren-Lawrence (KL) Grade | |
| KL 0 | 1 |
| KL 1 | 4 |
| KL 2 | 1 |
| KL 3 | 4 |
| Body mass index, median (range) [kg/m2] | 30 (18–38) |
| WOMACa pain, median (range) [100 point scale, 100-worst] |
48 (25–65) |
| MRI Characteristics | |
|
Characteristic |
Number of Subjects |
| Compartment of fracture | |
| Medial | 8 |
| Lateral | 2 |
| Bone fractured | |
| Femoral | 5 |
| Tibial | 4 |
| Femoral and tibial | 1 |
| Length of fracture | |
| <10 mm | 4 |
| 10–20 mm | 5 |
| >20 mm | 1 |
| Bone marrow edemab | |
| <25% | 0 |
| 25–50% | 5 |
| 50–75% | 1 |
| >75% | 4 |
| Meniscal tear | |
| No tear | 5 |
| Medial | 2 |
| Lateral | 0 |
| Both | 3 |
| Cartilage degenerative changes | |
| None | 2 |
| Partial thickness only | 5 |
| Partial and full thickness | 3 |
| Bone marrow lesions and cysts | |
| Yes | 2 |
| No | 8 |
Western Ontario and McMaster Universities Osteoarthritis Index.
The greatest amount of bone marrow edema was recorded for the subject with femoral and tibial fractures.
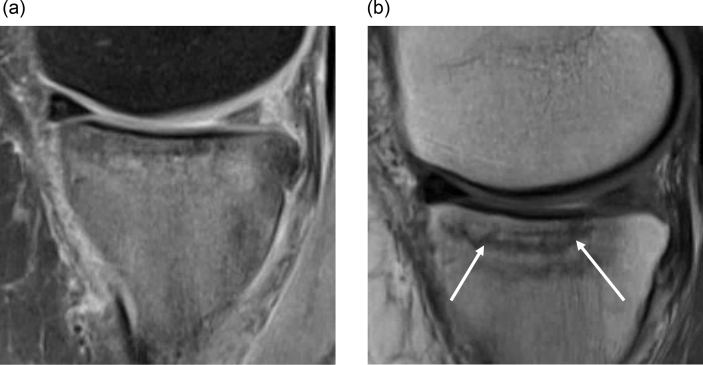
Fracture characteristics and other features found on MRI are presented in Table 1. Eight of the ten participants had fractures located medially (80%, 95% CI: 55.2%, 100.0%), and five of the ten (50%, 95% CI: 19.0%, 81.0%) had fractures located only in the weight-bearing portion of the femur. Additionally, one of the ten participants had both tibial and femoral fractures. Five of the ten participants (50%, 95% CI: 19.0%, 81.0%) had confirmed meniscal tear—either medial, lateral, or in both locations. The two participants who presented with bone marrow lesions also had bone marrow cysts, and all other subjects had neither bone marrow lesions nor cysts. The medial meniscal tear and subchondral insufficiency fracture line of one subject are presented in magnetic resonance images in Fig. 1.
Fig. 1.
Sagittal proton-density magnetic resonance images of one subject's knee with a subchondral insufficiency fracture. (a) Fat-suppressed image demonstrates extensive bone marrow edema in the medial tibial plateau and a posterior horn medial meniscal tear. (b) Image demonstrates linear subchondral insufficiency fracture line in the tibial plateau (white arrows).
4. Discussion
Individuals with knee pain and suspected knee OA are generally managed nonoperatively with weight-bearing exercises without advanced imaging, though such patients are at risk for additional or alternative sources of knee pain that are not seen on plain radiographs. The TeMPO Trial protocol requires MRI for eligibility and thus presented an opportunity to examine the prevalence of unsuspected SIFK in persons with presumed knee OA and meniscal tear whose clinicians have chosen to manage them without MRI. We estimated the prevalence of SIFK to be 2.94% (10 of 340 subjects; 95% CI: 1.15%, 4.71%) in patients managed nonoperatively for knee pain and presumed meniscal tear(s).
The prevalence of SIFK in persons with knee pain and suspected meniscal tears and specific guidelines for the treatment of SIFK are largely unaddressed in the literature. Treatment recommendations in UpToDate®, a point-of-care medical resource, include reduced weight-bearing to protect the fracture site as a part of conservative management for persons with stress fractures [5]. Other literature has focused on the important role of MRI in the diagnosis of SIFK, which is seldom visible on initial radiographs [8,9]. Identification of these fractures is important because recommended initial treatment for knee OA and/or meniscal tear is a weight-bearing home exercise or physical therapy program [10,11], which may be detrimental in patients with SIFK. Clinical features such as the presence of acute pain, may also play a role in distinguishing SIFK from OA and meniscal tear, though more research is needed on making this distinction. Subchondral insufficiency fractures have also resulted as possible adverse events from the administration of intra-articular corticosteroid injections and intravenous tanezumab [12,13]. Additionally, various randomized trials of subcutaneous tanezumab have included subchondral insufficiency fractures as an exclusion criteria, reflecting the concern that SIFK may potentially be a complication of tanezumab [14,15]. The cost of MRI must be considered in formulating clinical policy aimed at identifying these cases of SIFK. Our findings raise questions about the potential role of MRIs in working up patients with knee pain and suspected OA who fail to improve or worsen with weight-bearing exercises.
This is the only reported estimate of SIFK in adults with knee pain to our knowledge. Our study has important limitations, including the small number of cases of SIFK, precluding analysis of factors associated with SIFK. Additionally, it is possible that the fracture did not contribute to the subject's knee pain in some of these cases, raising the question of whether weight-bearing would indeed have been detrimental. Some patients with SIFK may present acutely, prompting immediate evaluation and MRI; such patients would not be included in our analysis as their MRIs would have been ordered by their physicians and not the TeMPO study, limiting the generalizability of the study. We required a visible fracture line on MRI in order to determine that a subject had SIFK. This criterion made the case definition more specific, but we acknowledge that bone marrow edema alone may suggest SIFK in some cases, making our estimate of SIFK prevalence conservative. Not all of the 10 subjects with SIFK have imaging evidence of OA on radiographs and MRI, limiting the applicability of our findings to the entire knee OA population. Osteoporosis may be a risk factor for SIFK, which we were unable to evaluate for these patients given the nature of the study and lack of bone densitometry measurements. Finally, the study was performed in two referral centers and in a clinical trial population, potentially limiting generalizability.
In conclusion, we found the prevalence of SIFK to be 2.94% in patients treated nonoperatively for knee pain and presumed meniscal tear. Further research is needed to identify factors associated with SIFK, permitting a rational strategy of ordering MRI in those at risk. There is also a need to define appropriate weight-bearing status and treatment for patients with SIFK. These data may raise clinicians’ suspicion of SIFK in persons with knee pain and suspected meniscal tear with or without OA managed presumptively with weight-bearing exercise and without advanced imaging.
Author contributions
Jamie L. Huizinga: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, Visualization, Project administration.
Nehal Shah: Conceptualization, Methodology, Validation, Investigation, Writing – review & editing, Visualization.
Stacy E. Smith: Conceptualization, Methodology, Validation, Investigation, Writing – review & editing, Visualization.
Anthony Notino: Conceptualization, Methodology, Validation, Investigation, Writing – review & editing, Visualization.
Melissa A. Kluczynski: Investigation, Data curation, Writing – review & editing, Supervision, Project administration.
Kelly Jordan: Investigation, Data curation, Writing – review & editing, Project administration.
Leslie J. Bisson: Conceptualization, Investigation, Resources, Writing – review & editing.
Antonia F. Chen: Conceptualization, Investigation, Writing – review & editing.
Faith Selzer: Formal analysis, Investigation, Resources, Writing – review & editing, Supervision, Project administration, Funding acquisition.
Elena Losina: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing – review & editing, Supervision, Funding acquisition.
Jeffrey N. Katz: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing – review & editing, Supervision, Funding acquisition.
Role of funding source
This manuscript is supported by research grant NIH/NIAMS U01AR071658.
Declaration of competing interest
Drs. Katz and Losina have research grants with Flexion and Samumed. Dr. Losina has a grant with Pfizer and performs consulting work for Velocity, and Regeneron. Dr. Chen has personal fees from SLACK publishing, Stryker, bOne, Pfizer, Avanos, Irrisept, Convatec, 3M, Recro, Heraeus, DePuy-Ethicon, GLG, and UpToDate. Dr. Chen is on the advisory board of Hyalex, is an associate editor of The Journal of Bone and Joint Surgery, and has equity with Sonoran Biosciences, Graftworx, and Joint Purification Systems.
Acknowledgments
The authors would like to thank TeMPO study participants and the Orthopedics Department at Brigham and Women's Hospital and the SUNY Buffalo Medical Center. We also acknowledge our funding source, the National Institutes of Health/NIAMS grant U01AR071658.
Contributor Information
Jamie L. Huizinga, Email: jamie.huizinga@gmail.com.
Nehal Shah, Email: nshah5@bwh.harvard.edu.
Stacy E. Smith, Email: ssmith@bwh.harvard.edu.
Anthony Notino, Email: anthonynotino@aol.com.
Melissa A. Kluczynski, Email: mk67@buffalo.edu.
Kelly Jordan, Email: kassayk@buffalo.edu.
Leslie J. Bisson, Email: ljbisson@buffalo.edu.
Antonia F. Chen, Email: afchen@bwh.harvard.edu.
Faith Selzer, Email: fselzer@bwh.harvard.edu.
Elena Losina, Email: elosina@bwh.harvard.edu.
Jeffrey N. Katz, Email: jnkatz@bwh.harvard.edu.
References
- 1.Deshpande B.R., Katz J.N., Solomon D.H., Yelin E.H., Hunter D.J., Messier S.P., et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res. 2016;68:1743–1750. doi: 10.1002/acr.22897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guermazi A., Eckstein F., Hellio Le Graverand-Gastineau M.P., Conaghan P.G., Burstein D., Keen H., et al. Osteoarthritis: current role of imaging. Med. Clin. 2009;93:101–126. doi: 10.1016/j.mcna.2008.08.003. xi. [DOI] [PubMed] [Google Scholar]
- 3.Pathria M.N., Chung C.B., Resnick D.L. Acute and stress-related injuries of bone and cartilage: pertinent anatomy, basic biomechanics, and imaging perspective. Radiology. 2016;280:21–38. doi: 10.1148/radiol.16142305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamamoto T., Bullough P.G. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J. Bone Joint Surg. Am. 2000;82:858–866. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 5.deWeber, K. Overview of Stress Fractures. Post, TW, ed. UpToDate, Waltham, MA: UpToDate Inc. https://www.uptodate.com/(Accessed August 25, 2020.).
- 6.Sullivan J.K., Irrgang J.J., Losina E., Safran-Norton C., Collins J., Shrestha S., et al. The TeMPO trial (treatment of meniscal tears in osteoarthritis): rationale and design features for a four arm randomized controlled clinical trial. BMC Muscoskel. Disord. 2018;19:429. doi: 10.1186/s12891-018-2327-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayyid S., Younan Y., Sharma G., Singer A., Morrison W., Zoga A., et al. Subchondral insufficiency fracture of the knee: grading, risk factors, and outcome. Skeletal Radiol. 2019;48:1961–1974. doi: 10.1007/s00256-019-03245-6. [DOI] [PubMed] [Google Scholar]
- 8.Lee S., Saifuddin A. Magnetic resonance imaging of subchondral insufficiency fractures of the lower limb. Skeletal Radiol. 2019;48:1011–1021. doi: 10.1007/s00256-019-3160-4. [DOI] [PubMed] [Google Scholar]
- 9.Jose J., Pasquotti G., Smith M.K., Gupta A., Lesniak B.P., Kaplan L.D. Subchondral insufficiency fractures of the knee: review of imaging findings. Acta Radiol. 2015;56:714–719. doi: 10.1177/0284185114535132. [DOI] [PubMed] [Google Scholar]
- 10.Safran-Norton C.E., Sullivan J.K., Irrgang J.J., Kerman H.M., Bennell K.L., Calabrese G., et al. A consensus-based process identifying physical therapy and exercise treatments for patients with degenerative meniscal tears and knee OA: the TeMPO physical therapy interventions and home exercise program. BMC Muscoskel. Disord. 2019;20:514. doi: 10.1186/s12891-019-2872-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stensrud S., Roos E.M., Risberg M.A. A 12-week exercise therapy program in middle-aged patients with degenerative meniscus tears: a case series with 1-year follow-up. J. Orthop. Sports Phys. Ther. 2012;42:919–931. doi: 10.2519/jospt.2012.4165. [DOI] [PubMed] [Google Scholar]
- 12.Kompel A.J., Roemer F.W., Murakami A.M., Diaz L.E., Crema M.D., Guermazi A. Intra-articular corticosteroid injections in the hip and knee: perhaps not as safe as we thought? Radiology. 2019;293:656–663. doi: 10.1148/radiol.2019190341. [DOI] [PubMed] [Google Scholar]
- 13.Hochberg M.C., Tive L.A., Abramson S.B., Vignon E., Verburg K.M., West C.R., et al. When is osteonecrosis not osteonecrosis?: adjudication of reported serious adverse Joint events in the tanezumab clinical development program. Arthritis Rheum. 2016;68:382–391. doi: 10.1002/art.39492. [DOI] [PubMed] [Google Scholar]
- 14.Schnitzer T.J., Easton R., Pang S., Levinson D.J., Pixton G., Viktrup L., et al. Effect of tanezumab on Joint pain, physical function, and patient global assessment of osteoarthritis among patients with osteoarthritis of the hip or knee: a randomized clinical trial. Jama. 2019;322:37–48. doi: 10.1001/jama.2019.8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berenbaum F., Blanco F.J., Guermazi A., Miki K., Yamabe T., Viktrup L., et al. Subcutaneous tanezumab for osteoarthritis of the hip or knee: efficacy and safety results from a 24-week randomised phase III study with a 24-week follow-up period. Ann. Rheum. Dis. 2020;79:800–810. doi: 10.1136/annrheumdis-2019-216296. [DOI] [PMC free article] [PubMed] [Google Scholar]