Abstract
Background
The institution-wide response of the University of California San Diego Health system to the 2019 novel coronavirus disease (COVID-19) pandemic was founded on rapid development of in-house testing capacity, optimization of personal protective equipment usage, expansion of intensive care unit capacity, development of analytic dashboards for monitoring of institutional status, and implementation of an operating room (OR) triage plan that postponed nonessential/elective procedures. We analyzed the impact of this triage plan on the only academic neurosurgery center in San Diego County, California, USA.
Methods
We conducted a de-identified retrospective review of all operative cases and procedures performed by the Department of Neurosurgery from November 24, 2019, through July 6, 2020, a 226-day period. Statistical analysis involved 2-sample z tests assessing daily case totals over the 113-day periods before and after implementation of the OR triage plan on March 16, 2020.
Results
The neurosurgical service performed 1429 surgical and interventional radiologic procedures over the study period. There was no statistically significant difference in mean number of daily total cases in the pre–versus post–OR triage plan periods (6.9 vs. 5.8 mean daily cases; 1-tail P = 0.050, 2-tail P = 0.101), a trend reflected by nearly every category of neurosurgical cases.
Conclusions
During the COVID-19 pandemic, the University of California San Diego Department of Neurosurgery maintained an operative volume that was only modestly diminished and continued to meet the essential neurosurgical needs of a large population. Lessons from our experience can guide other departments as they triage neurosurgical cases to meet community needs.
Key words: COVID-19, Elective, Essential, Operative volume
Abbreviations and Acronyms: COVID-19, 2019 novel coronavirus disease; ICU, Intensive care unit; IR, Interventional radiology; OR, Operating room; PCR, Polymerase chain reaction; PPE, Personal protective equipment; UC, University of California
Introduction
Severe acute respiratory syndrome coronavirus 2, the novel coronavirus strain that causes 2019 novel coronavirus disease (COVID-19), has a broad range of clinical manifestations, with some patients remaining asymptomatic carriers or experiencing only mild upper respiratory symptoms, while others progress to severe respiratory distress and failure necessitating intubation and intensive care unit (ICU) care.1, 2, 3, 4 Cerebrovascular complications, including acute ischemic hemorrhage, thromboembolic events, and subarachnoid hemorrhage, have been associated with COVID-19 infection.5 , 6
Owing to the severity and multisystem effects of this viral infection, there have been marked global shifts in medical practice. The neurosurgical community has transitioned toward reduction of nonessential surgery for the purpose of ensuring ICU availability for patients with COVID-19.7 As the only major academic medical center in San Diego County, California, USA, University of California (UC) San Diego Health is uniquely equipped to serve the public health needs of a diverse population of >3.3 million residents of the fifth largest county in the United States.8 UC San Diego Health operates multiple hospitals, including Jacobs Medical Center in La Jolla, UC San Diego Medical Center in Hillcrest, San Diego, and Sulpizio Cardiovascular Center in La Jolla, comprising 808 hospital beds and 112 ICU beds. UC San Diego Health is also distinguished as 1 of only 2 adult Level I trauma centers and the only regional burn center in San Diego County.9 As such, UC San Diego Health has played a key role in fulfilling public health needs in San Diego County during the COVID-19 pandemic.
The importance of documenting the effects of pandemic responses and resulting changes in surgical and clinical practice in both neurosurgery and other surgical specialties has been emphasized by several groups.7 , 10, 11, 12, 13, 14, 15, 16, 17 In this article, we further discuss shifts in practice at our high-volume academic institution, the only institution of its kind in a highly populous region. We review the methods applied within our health system that have allowed UC San Diego Health to manage this new public health crisis and quantitatively analyze the impact of COVID-19–era institutional policy on the operative volume of the UC San Diego Health Department of Neurosurgery. We posit that our experience will be of interest to the readership and may guide other departments through the process of prioritizing a comprehensive and efficacious institutional response to a global pandemic while maintaining the capacity to serve the essential and urgent neurosurgical needs of the broader community.
Materials and Methods
Review of COVID-19 Statistics in San Diego County
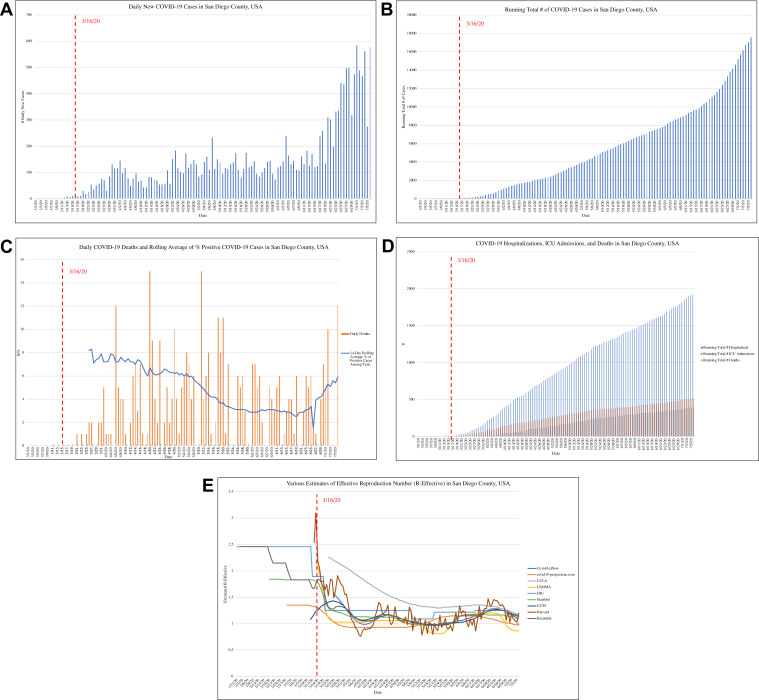
In March 2020, the Epidemiology and Immunization Services Branch of the San Diego County Health and Human Services Agency first implemented a county-wide daily dashboard reporting daily COVID-19 case counts, testing statistics, hospitalizations, and deaths.18 These data are publicly available online and updated daily.18 We reviewed these data and summarized the salient figures over the time period pertinent to our review in Figure 1 , including daily new COVID-19 cases, daily COVID-19 deaths, 14-day rolling average of percent positive tests, and running totals for COVID-19 cases, hospitalizations, ICU admissions, and deaths (Figure 1A–D). Various estimates of the effective reproductive number for COVID-19 in San Diego County, as published via the California COVID Assessment Tool by the California Department of Public Health, are displayed in Figure 1E.19
Figure 1.
2019 Novel coronavirus disease (COVID-19) statistics in San Diego County, California, USA, across the total study period, obtained from the county-wide daily dashboard established and maintained by the Epidemiology and Immunization Services Branch of the San Diego County Health and Human Services Agency.18 (A) Daily new COVID-19 cases in San Diego County. (B) Running total number of confirmed COVID-19 cases in San Diego County. (C) Daily COVID-19 deaths and rolling average of percentage positive COVID-19 cases in San Diego County. (D) Running total number of COVID-19–related hospitalizations, intensive care unit admissions, and deaths in San Diego County. (E) Estimates of effective reproductive number of COVID-19 in San Diego County by various institutions, as compiled by the California Department of Public Health.19 ICU, intensive care unit; UCLA, University of California Los Angeles; LEMMA, Local Epidemic Modeling for Management & Action; JHU, Johns Hopkins University; UCSF, University of California San Francisco.[CN1] (A–D, Data from the public County of San Diego Coronavirus Disease 2019 [COVID-19] Dashboard, maintained by the Epidemiology and Immunization Services Branch of the San Diego County Health and Human Services Agency. E, Data from the public open-source California COVID Assessment Tool, maintained by the California Department of Public Health.)
Review of Institutional Policy Changes in Response to COVID-19
We reviewed the institutional response of UC San Diego Health to the COVID-19 pandemic. The use of widespread in-house testing capacity was crucial to the institution's ability to maximize the safety of both patients and staff. UC San Diego Health became the first health institution in San Diego County as well as one of the first health institutions nationally to incrementally implement large-scale in-house COVID-19 polymerase chain reaction (PCR) and serologic testing. This rapid development of substantial in-house testing was achieved by the UC San Diego Center for Advanced Laboratory Medicine in collaboration with 5 in vitro diagnostics manufacturers (GenMark Diagnostics [Carlsbad, California, USA], Thermo Fisher Scientific [San Diego, California, USA], Roche Diagnostics [Santa Clara, California, USA], Abbott Diagnostics [Santa Clara, California, USA], and Luminex Corporation [Hayward, California, USA]). As of early April 2020, 700 in-house nucleic acid tests were being performed daily. This capacity has since grown with UC San Diego Health now able to perform in-house up to 1000 standard COVID-19 PCR tests, 100 rapid response COVID-19 PCR tests, and 1000 serologic tests for COVID-19 antibodies daily.
The in-house rapid response PCR has seen widespread use both in the emergency department and on the surgical floor at UC San Diego Health. These rapid tests can provide results within 1 hour of specimen collection and have been implemented as an initial screen for urgent/emergent patients to guide the use of personal protective equipment (PPE) during patient care and aerosolizing procedures. However, while highly specific for COVID-19, these rapid response PCR tests have demonstrated lower sensitivity than standard PCR, which has a turnaround time of 12–24 hours. While appropriate for patients with acute stroke and trauma requiring emergent interventions with a highly limited preintervention window for screening before aerosolizing procedures, the in-house rapid PCR tests alone do not provide sufficient screening sensitivity in nonemergent settings. At UC San Diego Health, it has become standard of care to ensure that all patients with a negative rapid response PCR receive a follow-up standard COVID-19 PCR to ensure adequate screening sensitivity.
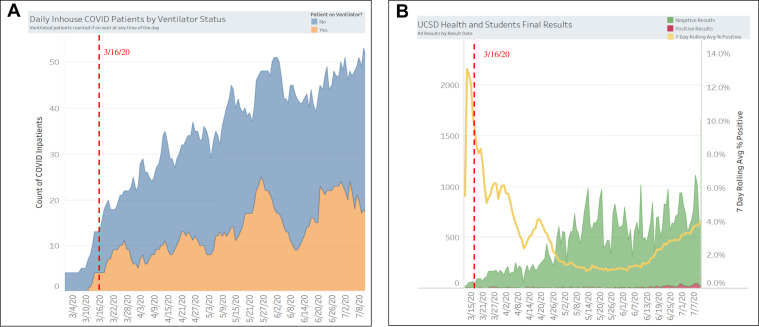
Beyond working to rapidly increase in-house testing capacity, UC San Diego Health further implemented institutional policies to expand ICU capacity and ensure adequate supplies of PPE. Outside the operating room (OR), a 4-phase staffing plan was developed to expand ICU capacity via incremental recruitment of physicians; dedicated traveling “SWAT teams” of surgeons to place central and arterial lines and physician ultrasound teams were among several modular physician units that were created to expand capacity to treat COVID-19–positive patients requiring intensive care. ICU capacity was further increased by the identification of all hospital beds with access to all oxygen, which was crucial to expanding capacity to care for patients with moderate-to-severe COVID-19 not yet requiring mechanical ventilation. PPE supply lines were secured with suppliers on an institutional level. A daily dashboard was created and distributed to all staff to provide quantitative and current data regarding ICU capacity, PPE supply, COVID-19 patient census, and institution-wide PCR and serologic test results.20 The total census and ventilator status of inpatients with COVID-19 at UC San Diego Health over the period of our review as well as pertinent PCR testing statistics among UC San Diego Health employees and students are summarized in Figure 2 . To maintain our support of satellite hospitals while minimizing the movement of infected patients, care teams were sent to highly impacted satellite hospitals to provide on-site support, while transfers of patients from such locales were minimized.
Figure 2.
2019 Novel coronavirus disease (COVID-19) statistics at University of California San Diego Health, including inpatient census, ventilator status, and testing statistics among staff and students, obtained from the daily dashboard that was implemented as a part of the institution-wide response to the COVID-19 pandemic. (A) COVID-19 inpatient census and ventilator status at University of California San Diego Health during the study period. (B) COVID-19 testing statistics, including 7-day rolling average percentage of positive tests, among University of San Diego Health employees and students during the study period. UCSD, University of San Diego.
(Reproduced from UC San Diego Health daily dashboards with permission of Dr. Christopher A. Longhurst, M.D.)
An OR triage plan was implemented on March 16, 2020, as part of an overall UC San Diego Health initiative to decrease nonessential inpatient hospitalizations and/or surgeries to maximize provider and ICU bed availability. To this end, nonurgent/nonemergent surgeries were globally postponed throughout the 3 main hospitals comprising the core of the UC San Diego Health system, while essential surgeries continued as needed. During this period, all potential surgical cases required approval by the corresponding department chair before being added to the OR schedule. In the Department of Neurosurgery, criteria for essential neurosurgical cases included both life-threatening conditions and the possibility of a progressive or permanent neurological deficit. Consideration was also given to the risk profile of individual cases, particularly cases involving aerosolizing procedures. Furthermore, the potential impact of specific cases on ICU capacity was factored into department chair–level decisions regarding which OR cases should proceed. Such decisions were guided by daily dashboards that reflected ongoing trends in COVID-19 hospitalizations, ICU capacity, ventilator availability, and hospital staff sick leave. In this manner, the scheduling of neurosurgical OR cases remained highly adaptive and responsive to changes in bed capacity and staff availability, thereby maintaining surge readiness. When possible, all surgical patients were screened for COVID-19 before their surgeries, with rapid response PCRs used for emergent stroke and trauma patients for whom the standard PCR test was unlikely to provide a result before incision time. For urgent and emergent cases, such screening was used to inform appropriate PPE use by all OR staff involved, thereby optimizing PPE use and supply while maximizing provider safety.
Retrospective Review of Neurosurgical Cases Before and After OR Triage Plan
We conducted a de-identified retrospective review of all operative cases and procedures performed by UC San Diego Health Department of Neurosurgery faculty from November 24, 2019, through July 6, 2020. This period included the 113 days before and the 113 days after implementation of the UC San Diego Health COVID-19 OR triage plan on March 16, 2020.
All UC San Diego Health neurosurgical operative cases and procedures conducted during the 113-day periods before and after implementation of the COVID-19 OR triage plan were reviewed and categorized according to type of case. Operative case data were pooled from the OR schedules of the 2 UC San Diego Health System hospitals at which the Department of Neurosurgery operates, the Jacobs Medical Center in La Jolla and the UC San Diego Medical Center in Hillcrest, San Diego. Pooling of operative data from these 2 primary hospitals was deemed appropriate given that the ready availability of patient transfers between the sites essentially combines the overall bed and ICU capacities of the 2 hospitals, with changes in case volume therefore reflecting changes in the combined neurosurgical operative capacity of the 2 hospitals. The categorizations employed are displayed in Table 1 . The category other interventional radiology (IR) refers to nonendovascular neurosurgical procedures performed in the IR suite by UC San Diego Health Department of Neurosurgery faculty, including epidural steroid injections, computed tomography myelograms, and IR-guided lumbar punctures. The category miscellaneous includes any cases not clearly referable to the other categories, such as follow-up cranioplasty and abdominal wound washouts.
Table 1.
Tabulated Case Totals and Z-Statistics Over Entire Study Period
| Case Category | Total 226-Day Period | Before 3/16/20 | 3/16/20 and Beyond | z | P, 1-Tail | P, 2-Tail |
|---|---|---|---|---|---|---|
| All | 1429 (100.0%); 6.3/day | 776 (100.0%); 6.9/day | 653 (100.0%); 5.8/day | 1.642 | 0.050 | 0.101 |
| Endovascular and diagnostic vascular | 382 (26.7%); 1.7/day | 203 (26.2%); 1.8/day∗ | 179 (27.4%); 1.6/day∗ | 0.982 | 0.163 | 0.326 |
| Nontraumatic spine (general and tumor) | 268 (18.8%); 1.2/day | 126 (16.2%); 1.1/day∗ | 142 (21.7%); 1.3/day∗ | −0.743 | 0.229 | 0.457 |
| Other IR (ESI, etc.) | 245 (17.1%); 1.1/day | 150 (19.3%); 1.3/day† | 95 (14.5%); 0.8/day† | 2.085 | 0.019 | 0.037 |
| Cranial tumor | 172 (12.0%); 0.8/day | 95 (12.2%); 0.8/day† | 77 (11.8%); 0.7/day† | 1.143 | 0.126 | 0.253 |
| Functional and peripheral/cranial nerve | 126 (8.8%); 0.6/day | 70 (9.0%); 0.6/day† | 56 (8.6%); 0.5/day† | 0.960 | 0.169 | 0.337 |
| Miscellaneous | 78 (5.5%); 0.3/day | 48 (6.2%); 0.4/day† | 30 (4.6%); 0.3/day† | 1.936 | 0.026 | 0.053 |
| Shunt (VPS and LP) | 60 (4.2%); 0.3/day | 35 (4.5%); 0.3/day† | 25 (3.8%); 0.2/day† | 1.268 | 0.102 | 0.205 |
| Trauma (cranial, spine) and Level I cases | 49 (3.4%); 0.2/day | 25 (3.2%); 0.2/day∗ | 24 (3.7%); 0.2/day∗ | 0.138 | 0.445 | 0.891 |
| Open vascular | 26 (1.8%); 0.1/day | 10 (1.3%); 0.1/day∗ | 16 (2.5%); 0.1/day∗ | −1.075 | 0.141 | 0.282 |
| EEA and transsphenoidal | 23 (1.6%); 0.1/day | 14 (1.8%); 0.1/day† | 9 (1.4%); 0.1/day† | 1.048 | 0.147 | 0.295 |
Tabulated University of California San Diego neurosurgical cases are reported as number of cases (%); mean number/day. Cases over the total 226-day period of the retrospective study as well as during the 113-day periods before and after implementation of the 2019 novel coronavirus disease (COVID-19) operating room triage plan are included. Two-sample z tests were performed to compare the daily number of cases before and after implementation of the plan in each category.
IR, interventional radiology; ESI, epidural steroid injection; VPS, ventriculoperitoneal shunt; LP, lumboperitoneal (shunt); EEA, endoscopic endonasal approach.
Increase in percentage of the total after implementation of the operating room triage plan.
Decrease in percentage of the total after implementation of the operating room triage plan.
Statistical Analysis of Neurosurgical Case Data
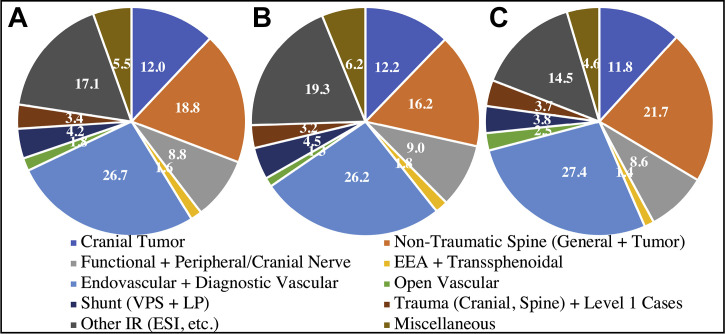
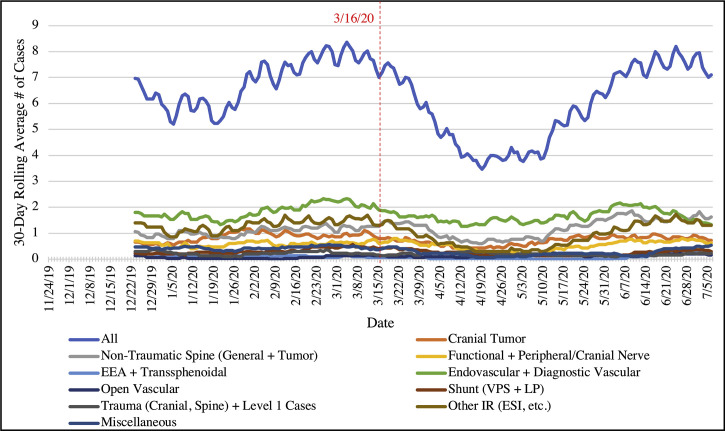
Overall case tallies and percentages of total by case type in the pre–and post–OR triage plan implementation periods were compared. The breakdown of all neurosurgical surgeries and procedures by case type was analyzed graphically (over the entire 226-day period of the study in Figure 3A ; over the 113-day pre–and post–OR triage plan implementation periods in Figure 3B and C). All case data were appropriately de-identified to protect patient privacy, and no protected health information was included. Mean numbers of cases per day by case type were also computed. The variances in the numbers of cases per day were computed in the pre–and post–OR triage plan implementation periods, and 2-sample z tests (α = 0.05) were performed. These results are summarized in Table 1. The 30-day rolling averages of daily cases (overall and subdivided by case type) are displayed in Figure 4 .
Figure 3.
Breakdown of University of California San Diego neurosurgical operative cases and procedures by type across the total study period and pre–and post–operating room (OR) triage plan implementation. (A) Case breakdown over the total 226-day period of the retrospective study. (B) Case breakdown over the 113 days before implementation of the University of California San Diego 2019 novel coronavirus disease (COVID-19) OR triage plan on March 16, 2020. (C) Case breakdown over the 113 days after implementation of the OR triage plan. VPS, ventriculoperitoneal shunt; LP, lumboperitoneal (shunt); IR, interventional radiology; ESI, epidural steroid injection; EEA, endoscopic endonasal approach.
Figure 4.
Rolling 30-day averages of daily University of California San Diego neurosurgical operative cases and procedures, total and by type, over the total 226-day period of the study. Implementation of the 2019 novel coronavirus disease (COVID-19) operating room triage plan on March 16, 2020, is delineated in red. EEA, endoscopic endonasal approach; VPS, ventriculoperitoneal shunt; LP, lumboperitoneal (shunt); IR, interventional radiology; ESI, epidural steroid injection.
Results
Impact of COVID-19 on San Diego County Over Entire Study Period
The first confirmed case of COVID-19 in San Diego County was reported on March 7, 2020 (Figure 1A).18 By the end of the study period on July 6, 2020, there were 17,578 confirmed cases of COVID-19 in San Diego County (Figure 1B), with a maximum of 584 new cases daily and a maximum of 15 deaths daily attributable to COVID-19 (Figure 1A and C).18 The 14-day rolling average of the percentage of positive tests throughout the county reached a maximum of 8.3% on March 27, 2020, only 11 days after implementation of the OR triage plan at UC San Diego Health (Figure 1C).18 By the conclusion of the study period, the county had experienced 1923 hospitalizations, 517 ICU admissions, and 399 deaths (approximately 0.01% of the county population) attributable to COVID-19 (Figure 1D).18 As displayed in Figure 1E, estimates of the effective reproductive number of COVID-19 in San Diego County by different institutions varied considerably, but the majority remained >1 for the majority of the post–OR triage plan period.19
UC San Diego Health COVID-19 Inpatient Census and Testing Over Entire Study Period
A review of the UC San Diego Health daily COVID-19 dashboards demonstrates a steadily increasing census of COVID-19–infected inpatients from early March 2020 through the remainder of the study period, with a peak of >50 COVID-19 admissions in the post–OR triage plan period (Figure 2A). This was accompanied by a concomitant increase in COVID-19–related ICU admissions, with a maximum of 25 patients with COVID-19 on ventilators at any given time (Figure 2A). COVID-19 testing data from tests conducted among UC San Diego Health staff and students revealed a peak positivity rate of >12% immediately before implementation of the OR triage plan on March 16, 2020 (Figure 2B). This rate steadily declined to a minimum of <2% by mid-May to late May 2020 (Figure 2B). These data were collected in a de-identified fashion from among all tested UC San Diego Health employees and students, and as such, data specific to UC San Diego Health surgical staff and the Department of Neurosurgery specifically are not available from official dashboards.
Breakdown of Neurosurgical Cases Over Entire 226-Day Study Period
Over the entire 226-day period of the retrospective study, 1429 surgical and IR procedures were performed by UC San Diego Health Department of Neurosurgery faculty (Table 1). This represented a mean of 6.3 total cases per day over the entire period. Endovascular procedures, including diagnostic cerebral angiography, accounted for the largest proportion of these cases (26.7% of the total) (Figure 3A) and an overall mean of 1.7 cases per day. This was followed by atraumatic operative spinal cases, including spinal tumor (18.8% of the total; mean of 1.2 cases per day) (Figure 3A). Cases involving an endoscopic endonasal approach or transsphenoidal approach accounted for the smallest percentage of the total, at 1.6% overall (mean of 0.1 case per day) (Figure 3A).
Breakdown of Neurosurgical Cases Before and After OR Triage Plan Implementation
Over the 113 days before implementation of the UC San Diego Health COVID-19 OR triage plan on March 16, 2020, 776 surgical and IR procedures were performed (Table 1). This represented a mean of 6.9 total cases per day over the pre–OR triage plan period. This decreased slightly to a total of 653 cases over the 113 days after implementation of the OR triage plan and a daily mean of 5.8 total cases per day. The transition to the OR triage plan led to a small relative increase in the proportion of endovascular/diagnostic vascular (from 26.2% to 27.4%), atraumatic spine (from 16.2% to 21.7%), trauma/Level I (from 3.2% to 3.7%), and open vascular (from 1.3% to 2.5%) cases in the post–OR triage plan period (Figure 3B and C). This transition also led to a small relative decrease in the proportion of cranial tumor (from 12.2% to 11.8%), functional and peripheral/cranial nerve (from 9.0% to 8.6%), shunt (from 4.5% to 3.8%), endoscopic endonasal approach/transsphenoidal (from 1.8% to 1.4%), other IR (from 19.3% to 14.5%), and miscellaneous (from 6.2% to 4.6%) cases in the post–OR triage plan period (Figure 3B and C).
Statistical Comparison of Daily Cases Before and After OR Triage Plan Implementation
Two-sample z tests were performed to compare the daily number of cases before and after implementation of the COVID-19 OR triage plan in each case category. The z statistics and 1- and 2-tail P values are displayed in Table 1. There was no statistically significant difference in the mean number of daily total cases in the pre–versus post–OR triage plan periods (6.9 vs. 5.8 mean daily cases; 1-tail P = 0.050, 2-tail P = 0.101). With statistical significance defined as P < 0.05, this lack of a statistically significant difference in the mean number of daily cases in the pre–versus post–OR triage plan periods was reflected in the P values of every single category of neurosurgical cases and procedures, with the exceptions of the other IR and miscellaneous categories. The other IR category of cases—comprising nonendovascular cases performed in the IR suite by UC San Diego Health Department of Neurosurgery faculty, such as epidural steroid injections and IR-guided lumbar punctures—did exhibit a statistically significant decrease in mean daily cases from the pre–to post–OR triage plan periods (from 1.3 to 0.8 mean daily cases; 1-tail P = 0.019, 2-tail P = 0.037). The miscellaneous category of cases exhibited a decrease in mean daily cases from the pre–to post–OR triage plan periods (from 0.4 to 0.3 mean daily cases) that was statistically significant by the 1-tail P value (0.026), but not by the corresponding 2-tail P value (0.053). The only category of cases to exhibit an increase in the mean daily number of cases after implementation of the OR triage plan was the atraumatic spine category (1.1 vs. 1.3 mean daily cases), though this increase was not statistically significant.
The 30-Day Rolling Averages of Daily Cases
Figure 4 displays the rolling 30-day averages of daily neurosurgical operative cases and procedures performed at UC San Diego Health over the entire 226-day period of the study. The implementation on March 16, 2020, of the COVID-19 OR triage plan prioritizing essential surgeries and procedures is marked by a dotted line in this figure. The maximum number of daily atraumatic spine cases computed from the 30-day rolling average increased from a maximum of 1.4/day to 1.9/day after implementation of the OR triage plan. The minimum number of daily other IR cases decreased from a minimum of 0.9/day to 0.3/day after implementation of the OR triage plan. Other than these 2 instances, none of the subdivided categories of neurosurgical cases displayed a change in rolling 30-day daily minimum/maximum number of cases greater than ±0.2 cases/day after implementation of the OR triage plan.
Discussion
The COVID-19 pandemic has mandated many changes in health care systems worldwide to enable health care practitioners to continue to provide services while maximizing staff and patient safety.11, 12, 13, 14, 15, 16, 17 , 21 Surgical services in particular have needed to adapt to navigate the safety hazards posed by the COVID-19 pandemic while continuing to meet the undiminished surgical needs of the populations they serve.11, 12, 13, 14, 15, 16, 17 Multiple academic studies have attempted to outline appropriate and effective safety procedures to be implemented by surgical services during these unprecedented times.7 , 10, 11, 12, 13, 14, 15, 16, 17 However, the impact of the pandemic on academic neurosurgical practices in the United States has not yet been fully explored, and we propose that a quantitative analysis of this impact on a large academic center over the course of many months will offer novel and beneficial insights.
UC San Diego Health is unique in that it serves as the only academic health institution in a large county that is also notable for its diversity, with 34.1% of residents identifying as Hispanic or Latino, 12.6% identifying as Asian, 5.5% identifying as Black or African American, and 1.3% identifying as American Indian and Alaskan Native as of July 1, 2019.8 San Diego County experienced a substantial surge in COVID-19 cases during the period of this study, with a county maximum of 584 daily new cases, a maximum 14-day rolling average of 8.3% positive tests in late March, and estimates of the effective reproductive number of COVID-19 in San Diego County that remained >1 for the majority of the post–OR triage plan period, indicating increasing spread of the virus for the majority of the study period.18 , 19
In March 2020, the UC San Diego Health system launched a comprehensive program to respond to the many needs and challenges encountered as a result of the COVID-19 pandemic. Adequate testing capacity was the first key threshold required for UC San Diego Health to maintain sufficient high-quality hospital function. UC San Diego Health implemented a policy of testing all inpatients and all surgery patients for COVID-19 as well as both asymptomatic and symptomatic employee screening. With results able to be generated in <60 minutes, the in-house rapid response PCR test for COVID-19 served as a mainstay of screening primarily for emergent stroke and trauma patients. It has become standard of care at UC San Diego Health to employ the more sensitive standard PCR, which requires only 12–24 hours to obtain a result owing to remaining entirely in-house, for the screening of nonemergent patients as an adjunct to increase sensitivity for patients who formerly underwent rapid screening. The substantial in-house testing capacity of UC San Diego Health continues to inform PPE use in a manner that optimizes PPE supply while simultaneously maximizing provider safety.
Various other measures, including daily symptomatic screening of all patients, staff, and visitors as well as guidelines for isolating COVID-19–positive patients for treatment in dedicated hospital units, have proven highly effective at enabling UC San Diego Health to maintain high-quality, high-volume patient care. Revised guidelines concerning conservation of PPE, together with institutionally secured PPE supplies from vendors and mandated use of N95 respirators and eye protection during encounters with acute/emergent patients with unknown COVID-19 status and during potentially aerosolizing procedures, have further promoted the health and safety of staff during the pandemic. Daily screening, contact tracing, and analytics dashboards further facilitate accurate tracking of the institutional impact of the pandemic.20 The efficacy of these measures in ensuring the safety of UC San Diego Health staff is evidenced by our low rate of positive COVID-19 tests among staff and students during the majority of the study period (Figure 2B).
Another key element of the UC San Diego Health response to COVID-19 was implementation of an OR triage plan on March 16, 2020, in an effort to decrease nonessential inpatient hospitalizations and nonessential surgery to maximize provider and ICU bed availability. Starting on that date, nonurgent/nonemergent surgeries were globally postponed throughout the UC San Diego Health system, while essential surgeries continued as needed. All surgical cases required the authorization of the department chair for essential status, with criteria including life-threatening conditions and a high risk of a progressive or permanent neurological deficit. Such decisions were responsive to daily dashboards that reflected ongoing trends in COVID-19 hospitalizations, ICU capacity, ventilator availability, and hospital staff sick leave. Indeed, during the period of the study, UC San Diego Health demonstrated a peak of >50 COVID-19 admissions in the post–OR triage plan period but never surpassed total bed or ICU capacity. Such findings strongly suggest that surge capacity and readiness were maintained for the duration of the study period, despite increasing spread of COVID-19 on a county-wide level during this period.19 These changes were implemented alongside institutional isolation and cohort protocols for COVID-19–positive patients.11 , 13 , 14
UC San Diego Health Department of Neurosurgery faculty performed 1429 neurosurgical operative and IR procedures over the entire 226-day period of the retrospective study, 776 (54.3%) of which were performed in the 113 days before implementation of the COVID-19 OR triage plan. This represents a markedly high neurosurgical operative volume that, per our analysis of daily case totals, was only modestly diminished in the 113 days after implementation of the OR triage plan. Moreover, the plurality of endovascular and atraumatic spine cases that was evident before this transition did not diminish in any significant manner. The small relative increase in the proportion of endovascular/diagnostic vascular (from 26.2% to 27.4%) and atraumatic spine (from 16.2% to 21.7%) cases in the post–OR triage plan period was likely due to multiple factors. The continued high volume of oncologic, endovascular, and atraumatic spinal operative neurosurgical cases that we observed even during the period of the OR triage plan was likely partly referable to the criteria used by the department chair for determining essential case status, which prioritized pathologies with a high risk of a permanent or progressive neurological deficit or substantial threat to life. Moreover, many endovascular/diagnostic vascular and atraumatic spine cases that were deemed essential by these criteria were unlikely to require postoperative ICU admission and therefore could feasibly proceed without significantly impacting ICU surge capacity during the pandemic. Such decisions were guided by daily dashboards that reflected ongoing trends in COVID-19 hospitalizations, ICU capacity, PPE and ventilator availability, and hospital staff sick leave. These data enabled anticipation of the potential impact of potential OR cases on surge readiness and guided decisions regarding whether nonemergent cases could proceed. In this manner, the scheduling of neurosurgical OR cases remained highly adaptive and responsive to changes in bed capacity and staff availability.
The overall distribution of neurosurgical cases by type remained relatively constant, as depicted in Figure 3. We show that the institution-wide shift in focus from elective to essential surgical cases at UC San Diego Health only moderately diminished the operative volume and did not significantly alter the case distribution of its traditionally high-volume neurosurgical service. This trend is likely multifactorial in origin, but may relate to the fact that the majority of neurosurgical procedures are either lifesaving or vital for preserving neurological function and therefore remain essential even during an institutional curtailment of elective procedures. Our findings suggest that despite the limitations imposed by COVID-19, UC San Diego Health has continued to serve the acute and urgent neurosurgical needs of one of the most populated counties in the United States in an undiminished fashion. The institution-wide screening, testing, isolation/cohorting, and PPE policies enacted by UC San Diego Health have been vital to the ongoing efforts of the Department of Neurosurgery to maintain operative volume after implementation of the OR triage plan and continue to meet the essential and urgent needs of a highly populated county, while maintaining the health and safety of staff members.
Our statistical analysis further revealed that the lack of a statistically significant difference in the mean number of daily cases in the pre–versus post–OR triage plan periods was maintained by every single category of neurosurgical cases and procedures, with the exceptions of other IR and miscellaneous categories. The procedures falling into these two categories, such as IR-guided lumbar punctures and epidural steroid injections, were typically nonacute/nonurgent procedures. As such, the decrease in the daily totals of such cases after implementation of the OR triage plan can be readily explained by nonessential status. The core operative neurosurgical cranial and spine daily caseloads remained statistically undiminished after the switch from elective to essential surgeries at UC San Diego Health. This underscores the essential nature of the majority of operative neurosurgical procedures and the large county-wide need for diverse acute/urgent neurosurgical interventions that remained undiminished by the COVID-19 pandemic.
The 30-day rolling averages of daily case numbers over the entire 226-day period of the retrospective study are displayed in Figure 4. While a marked dip in daily case totals is qualitatively observed immediately after implementation of the OR triage plan on March 16, 2020, we show that this decline was both small in magnitude (from a 30-day rolling average minimum of 5.2 cases/day before vs. 3.5 cases/day after implementation of the OR triage plan) and temporary. In fact, the rolling 30-day average daily number of cases exceeded the pre–OR triage plan minimum of 5.2 cases/day after approximately 2 months by May 19, 2020. The corresponding dips in cases/day observed in the rolling 30-day averages for the individual case categories were comparatively small. This demonstrates that the operative volume of the UC San Diego Health Department of Neurosurgery was only modestly diminished while meeting the community needs of focusing on essential cases to minimize inpatient hospitalizations and ICU stays for noncritical cases.
We acknowledge that different hospitals, cities, and countries differ in terms of patient population, testing ability, bed capacity, staffing, and other resources, and as such, exact replication of the UC San Diego Health COVID-19 policies is not fully possible at other health care centers. For instance, preoperative testing of all patients for COVID-19 and rapid in-house testing of emergent patients is simply not possible in all health systems and regions. Our experience, however, highlights several key principles that may be universally applied to any health care system and may serve as a roadmap that other institutions can follow. Regardless of resource availability, the key components of our pandemic response—including implementation of a cohesive and institution-wide plan, emphasis on essential rather than elective OR cases, and monitoring of various metrics of hospital capacity to enable adequate surge planning—may be enacted to some degree in any health care setting. Large academic centers such as UC San Diego Health have benefited from the ability to rapidly scale up in-house COVID-19 testing capabilities, and it must be acknowledged that accurate and rapid testing of patients and staff for COVID-19 is not yet universally available. Though testing capacity may vary considerably with circumstances, however, these other key principles are otherwise broadly applicable and are likely to improve institutional ability to continue to meet the surgical needs of a given population, regardless of setting.
Conclusions
This article serves as a record of how the UC San Diego Health neurosurgical service has continued to meet the essential and urgent needs of the fifth most populous county in the United States.9 During such unprecedented times, the UC San Diego Health Department of Neurosurgery maintained an operative volume that was only modestly diminished owing to implementation of a comprehensive OR triage plan, as evidenced by only a very moderate difference in the mean number of daily total cases in the pre–versus post–OR triage plan periods (6.9 vs. 5.8 mean daily cases). Crucial among the measures enacted were the development of widespread in-house testing capacity and the prioritization of essential and emergent OR cases and postponement of nonessential/elective procedures to preserve the availability of both providers and ICU beds. Our hope is that lessons from our experience can guide other departments as they triage essential neurosurgical cases to meet the demands of their diverse communities. Though resources inevitably vary among institutions, cities, and countries, many of these principles—particularly those pertaining to implementation of an institution-wide response and monitoring of key metrics—are broadly applicable regardless of resource availability.
CRediT authorship contribution statement
Arvin R. Wali: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing. Bryan E. Ryba: Investigation, Formal analysis, Writing - original draft, Writing - review & editing. Keiko Kang: Investigation, Writing - original draft. David R. Santiago-Dieppa: Resources, Writing - review & editing. Jeffrey Steinberg: Resources, Writing - review & editing. Luis Daniel Diaz-Aguilar: Resources, Writing - review & editing. Lauren E. Stone: Resources, Writing - review & editing. Michael G. Brandel: Resources, Writing - review & editing. Christopher A. Longhurst: Data curation, Writing - review & editing. William Taylor: Supervision, Project administration, Writing - review & editing. Alexander A. Khalessi: Supervision, Project administration, Writing - review & editing.
Acknowledgments
We acknowledge the physicians, nurses, hospital staff, and scientists working tirelessly to serve our community and keep us safe during this pandemic.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Arvin R. Wali and Bryan E. Ryba are co–first authors.
References
- 1.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma R., Agarwal M., Gupta M., Somendra S., Saxena S.K. In: Coronavirus Disease 2019 (COVID-19): Epidemiology, Pathogenesis, Diagnosis, and Therapeutics. Saxena S.K., editor. Springer; Singapore: 2020. Clinical characteristics and differential clinical diagnosis of novel coronavirus disease 2019 (COVID-19) pp. 55–70. [Google Scholar]
- 3.Lewnard J.A., Liu V.X., Jackson M.L., et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. doi: 10.1136/bmj.m1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatraju P.K., Ghassemieh B.J., Nichols M., et al. COVID-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varatharaj A., Thomas N., Ellul M.A., et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7:875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ellul M.A., Benjamin L., Singh B., et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: Adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020;87:E173–E177. doi: 10.1093/neuros/nyaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Census Bureau QuickFacts: San Diego County, California. https://www.census.gov/quickfacts/fact/table/sandiegocountycalifornia,CA/PST045219 Available at:
- 9.San Diego County Health & Human Services Agency Demographics. https://www.sandiegocounty.gov/hhsa/statistics_demographics.html#:∼:text=Contact%20Us-,Demographics,and%20will%20be%20increasingly%20so Available at:
- 10.Khalafallah A.M., Jimenez A.E., Lee R.P., et al. Impact of COVID-19 on an academic neurosurgery department: the Johns Hopkins experience. World Neurosurg. 2020;139:e877–e884. doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coccolini F., Perrone G., Chiarugi M., et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15:25. doi: 10.1186/s13017-020-00307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Couloigner V., Schmerber S., Nicollas R., et al. COVID-19 and ENT surgery. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137:161–166. doi: 10.1016/j.anorl.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Simone B., Chouillard E., Di Saverio S., et al. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flemming S., Hankir M., Ernestus R.I., et al. Surgery in times of COVID-19-recommendations for hospital and patient management. Langenbecks Arch Surg. 2020;405:359–364. doi: 10.1007/s00423-020-01888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pai E., Chopra S., Mandloi D., Upadhyay A.K., Prem A., Pandey D. Continuing surgical care in cancer patients during the nationwide lockdown in the COVID-19 pandemic—perioperative outcomes from a tertiary care cancer center in India. https://doi.org/10.1002/jso.26134 [e-pub ahead of print]. J Surg Oncol. [DOI] [PMC free article] [PubMed]
- 16.Steward J.E., Kitley W.R., Schmidt C.M., Sundaram C.P. Urologic surgery and COVID-19: how the pandemic is changing the way we operate. J Endourol. 2020;34:541–549. doi: 10.1089/end.2020.0342. [DOI] [PubMed] [Google Scholar]
- 17.Wexner S.D., Cortes-Guiral D., Gilshtein H., Kent I., Reymond M.A. COVID-19: impact on colorectal surgery. Colorectal Dis. 2020;22:635–640. doi: 10.1111/codi.15112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.County of San Diego - Coronavirus Disease 2019 (COVID-19) Dashboard. https://www.arcgis.com/apps/opsdashboard/index.html#/96feda77f12f46638b984fcb1d17bd24 Available at:
- 19.California COVID Assessment Tool Modeling COVID-19 to Inform State and Local Response. https://calcat.covid19.ca.gov/cacovidmodels/ Available at:
- 20.Reeves J.J., Hollandsworth H.M., Torriani F.J., et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27:853–859. doi: 10.1093/jamia/ocaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopez S., Decastro G., Van Ogtrop K.M., et al. “Palliative pandemic plan,” triage and symptoms algorithm as a strategy to decrease providers’ exposure, while trying to increase teams availability and guidance for goals of care (GOC) and symptoms control. Am J Hosp Palliat Care. 2020;37:980–984. doi: 10.1177/1049909120942494. [DOI] [PMC free article] [PubMed] [Google Scholar]