Abstract
Background
This study compares the experiences of African American (AA) families who authorized organ donation with those who refused.
Methods
Large administrative datasets were obtained from 9 partnering Organ Procurement Organizations (OPO). Initial analyses used these data to assess authorization among African American families (N=1,651). Subsequent analyses were performed using a subsample of interview data of AA family decision makers (N=276). Initial bivariate analyses tested differences in study variables by authorization status (donor/nondonor). Two separate multilevel logistic regressions examined associations between independent variables and family authorization.
Results
Analyses of the administrative datasets found that refusal was more likely when the patient was older, female, a DCD case, and not referred in a timely manner; refusal was less likely when families initiated donation conversations. Interview data revealed that families who refused donation were less likely to respond favorably to initial donation requests and reported less satisfaction with the overall approach, amount of time with OPO staff, and how questions were handled. Refusing families were also more likely to feel pressured, had less comprehensive donation discussions, and rated the OPO requesters’ communication skills lower. No significant differences in organ donation attitudes were found between families who authorized donation and those refusing to donate.
Conclusions
The study suggests that AA families making decisions about organ donation would benefit from culturally-appropriate discussions.
Keywords: Organ donation, Decision making, African American, Communication, Disparities
INTRODUCTION
Although the rate of deceased organ donation among African Americans (AA) has nearly doubled over the last three decades – from 8.8% in 1988 to 15.1% in 2019 [1], the authorization rate among AA families remains significantly lower than that found among Caucasians (54.9% vs. 77.0%) [2]. Recent studies have revealed a consistent picture of AAs’ continued reluctance to donate their own or a family member’s organs upon death [3,4]. Data from a 2019 national poll on organ donation (N=10,000) found 84.5% of AAs in support of organ donation, as compared to 86.4% for Hispanics, 88.2% Asians, and 92.9% for Caucasians [5]. The same poll also found lower rates of donor designation (37.9%) and willingness to register as posthumous organ donors (65.3%) among AAs. AAs were also among the least likely to indicate a desire to have their organs donated after death, to donate deceased family members’ organs, or to have communicated their donation wishes to family and friends.
Callender and colleagues’ seminal studies on AA organ donation identified fear of premature death, lack of awareness of the transplantation process, perceived and actual racism, religious beliefs and misperceptions, and mistrust of the healthcare system as barriers to organ donation by AAs [6,7]. To counter these factors and encourage more widespread acceptance of organ donation among AAs, public educational programs were initiated under the national Minority Organ Tissue Transplant Education Program (MOTTEP) [8]. Certainly, MOTTEP has yielded some positive results by increasing awareness and understanding of the need for donation [9,10].
Yet general mistrust of the healthcare and donation systems, including a perception that AAs are less likely to receive a transplant, persists [11,12]. There is also evidence of implicit bias, i.e., the extra-conscious beliefs or attitudes toward individuals by virtue of some “irrelevant characteristic” [13], that permeate discussions of organ donation with AA families about the opportunity for donation while in hospital [14]. Past studies comparing the experiences of AA and Caucasian families who have made decisions about donating a family member’s organs found that donor-eligible AA patients were less likely to be referred to an Organ Procurement Organization (OPO) by hospital staff [14], and that when referred, AA families report less complete discussions about the possibility of organ donation and are often not told of the need for transplantable organs within the AA community [14]. Cultural competence is another factor impacting AA donation rates. Cultural competence, or the ability to provide high-quality care to families of all cultural backgrounds, impacts perceptions of and satisfaction with care [15]. It also upholds patients’ cultural identities, which facilitates the development of trust and provides a safe space to ask questions and express concerns [15]. At least one study has shown family authorization rates for organ donation are higher for AAs when the OPO staff discussing donation are also AA, but the majority of OPO staff continue to be Caucasian [16].
Despite the continued hesitancy to donate, a substantial proportion (reports range from 29% - 39%) of AAs are willing to donate and ultimately authorize donation at the bedside [17–19]. While numerous studies have compared donation outcomes across racial/ethnic categories [14,20,21], the analysis presented here advances our understanding of the facilitators and impediments to organ donation among AAs by exploring within-group differences in organ donation knowledge, attitudes, and behaviors. Our goal is to identify substantive and modifiable factors that could create an environment in which authorization of donation among AA families is optimized. This study compares a comprehensive set of factors – demographic, attitudinal, and behavioral – to differentiate AA family decision makers who made decisions to donate deceased family members’ organs with those who refused to authorize donation.
MATERIALS AND METHODS
Overview
From January 2009 to March 2012, as part of a larger study [22], we collaborated with nine OPOs representing five regions of the U.S., (i.e., Northeast (n=2), Midwest (n=2), South (n=3), Southwest (n=1), and Mid-Atlantic (n=1)), to identify a sample of potential donor-eligible patients and recruit their family decision makers to the study. A family decision maker (FDM) is defined as the individual tasked by the family to make a decision about donor authorization, typically the next-of-kin. Each month, OPOs provided administrative data about deceased patients (e.g., age, race), FDMs (i.e., name, contact information), and donation decisions (authorized/refused). To ensure that the research team contacted all individuals who were potentially eligible to participate, OPO staff also completed brief, online surveys with the FDMs’ contact information following every organ donation discussion. Two months after an adult patient’s death, or three months if the patient was younger than 18 years of age, potential participants were mailed recruitment packets with an invitation to participate, consent forms, and an opt-out postcard. If individuals did not opt out within two weeks of mailing recruitment materials, the research team contacted FDMs by telephone. Cases included both patients who died from neurological trauma (brain death) and those who were eligible for donation after cardiac death (DCD) due to devastating and irreversible brain injury and being near death but not meeting formal brain death criteria.
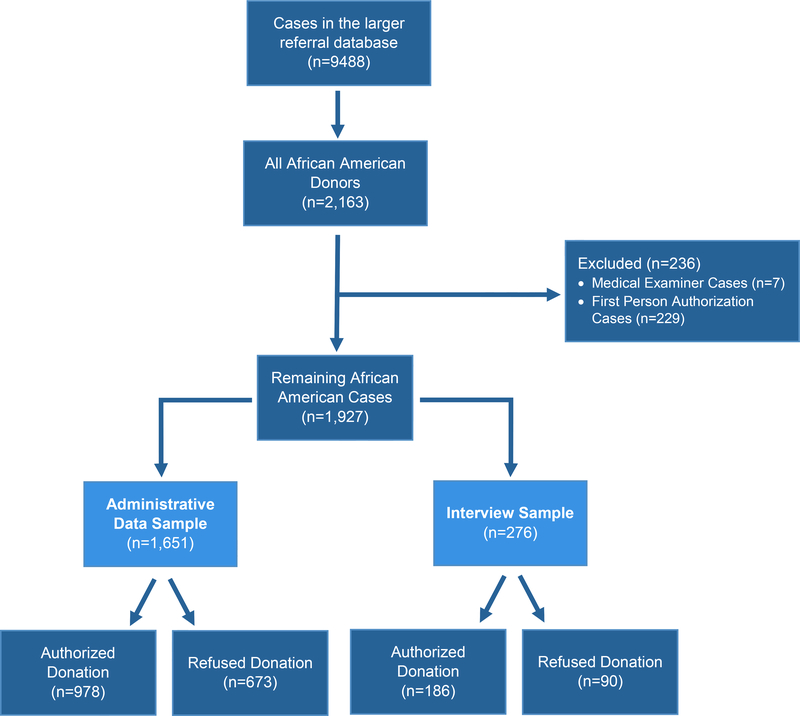
This report drew from two related data sets: 1) a large administrative data set combining data obtained from the participating OPOs of all potential cases during the data collection period, and 2) a smaller subsample of cases in which data were obtained via telephone interviews with FDMs. Of the 9,488 cases in the larger referral database (DCD = 20.25%), 2,163 included an AA potential donor (DCD = 10.1%). Because we were interested in cases in which families made a donation decision, we excluded first person authorization cases (n=229; 10.6%), which since 2006 are legally binding [23], and cases involving medical examiners (n=7; .03%). Of the remaining 1,927 cases, 1,651 are in the administrative sample (DCD = 11.68%) and 276 in the interview subsample (DCD = 9.4%; see Figure 1).
Figure 1.
Flow chart of case accrual
Of the AA patient cases in the administrative-only sample, 978 FDMs (59.2%) authorized donation, and 673 (40.8%) refused donation. Of the AA cases in the interview sample, 186 FDMs (67.4%) authorized donation and 90 (32.6%) refused. We conducted two separate analyses given the discrepancy in the authorization rates in the two samples and the availability of more detailed information in the interview sample.
OPO Administrative Data
The data collected from the nine OPOs’ administrative databases included authorization outcome (authorized/refused), patient age and sex, DCD (yes/no), family initiation of donation conversation (yes/no), and timely referral (yes/no). The referral of a patient is deemed timely if it occurs as soon as possible after imminent death criteria has been reached [24]. Because the exact timeframe for referral after identifying imminent death varies by OPO, we used each participating OPO’s operational definition. The main outcome variable was the final donation decision (authorized/refused), which was cross-verified for cases with an FDM interview.
FDM Interview Data
FDMs were contacted about study participation 2–3 months after the patient’s death (3 months for pediatric cases). Potential participants were mailed a recruitment packet containing a letter describing the study and a pre-paid opt-out postcard. Those who did not return the postcard within two weeks were contacted by telephone and invited to participate. This validated recruitment and interview protocol has been described in detail elsewhere [22,25,26]. All participants provided informed consent, and the study was approved by the Institutional Review Board at Virginia Commonwealth University (#HM11773).
The semi-structured interviews collected FDM sociodemographic data (e.g. age, marital status, gender, race, etc.) and organ donation attitudes and knowledge. FDMs were asked about their experiences during the patient’s hospitalization, such as the care the patient received, the donation process experience and details about that discussion, and reasons for the donation decision. The specific measures are described below.
Organ Donation Attitudes
Attitudes toward organ donation were assessed using the Attitudes Toward Organ Donation Scale [27,28]. The well-validated, 17-item scale assesses attitudes along five-point Likert-type scales of agreement (1=Strongly disagree; 5=Strongly agree) [22,25]. Individual items were summed to compute a global attitude score ranging from 17 to 85.
Quality of OPO Requesters’ Communication
A shortened version of Burgoon and Hale’s Relational Communication Scale (RCS)[29] was used to capture respondents’ perceptions of requesters’ relational communication skills. The RCS consists of 12 items rated using seven-point Likert scales (1=strongly disagree; 7=strongly agree). Items were summed with higher scores (range 12–84) reflecting more positive assessments. In addition, FDMs were asked to provide a single-item global rating of the quality of the requester’s communication using a five-point response scale (1=poor; 5=excellent); higher scores reflect more positive impressions of the exchange.
FDMs rated their satisfaction with 3 major domains of communication: 1) the amount of time spent discussing donation with the OPO staff requester, 2) the requester’s handling of questions, and 3) assessment of the overall organ donation request process. Each question was rated on a 7-point scale (1=not at all; 7=very satisfied). Respondents were also asked to rate whether they felt pressured or harassed at the hospital about organ donation (1=not at all pressured; 7=very pressured), were surprised at the request (yes/no), and their initial reactions to the request for organ donation (1=favorable; 2=mixed/undecided; 3=unfavorable).
Twenty-four theoretically-based relational communication skills were identified a priori [22,25,26] and their frequency of use during the request was assessed by FDMs using a 5-point Likert scale (1=never; 5=always). Skills included acknowledging FDMs’ concerns, providing offers of service, and checking in to assure the FDMs’ understanding. A total score was computed using the sum (range: 24–120) of the individual items with higher values reflecting greater use of the skills. In addition, based on previous research that identified specific topics important to FDM decision-making [26,30], we asked families whether a series of 17 donation-related topics were discussed (yes/no). The total number of topics discussed was computed by summing affirmative responses (see Online Resource).
Healthcare Provider (HCP) Interaction
FDMs were asked whether they spoke with hospital staff or healthcare providers (HCPs) about organ donation (no=0; yes=1) and to rate the level of care and concern exhibited by HCPs who were most important to providing care using a 7-point Likert scale (1=in no way caring or concerned; 7=very caring and concerned).
Analytic Plan
Administrative and interview data were linked to create a single dataset for these analyses. For the characteristics common to both the OPO administrative-only and the FDM interview groups (patient race, patient age, DCD, timely referral, family initiated), the samples are compared using the chi-square test for categorical variables and t-test for continuous variables. Descriptive statistics are reported for all variables from both sources. We conducted bivariate assessments for AA FDMs who authorized donation compared to those who refused. Multivariable logistic regression analyses were performed on each dataset to examine the association of the independent variables with refusal to authorize donation. The model controlled for nesting of FDMs within OPO requesters as well as requesters within OPOs. All statistical analyses were performed using SAS 9.4 [31].
RESULTS
OPO Administrative Data
A slight majority of patients were male (n=895; 53.8%) with an average age of 45.3 years (sd=19.1). The majority of patients were deemed dead by neurological criteria (n=1,458; 88.3%). In addition, 33.1% of patient referrals were not indicated as timely by the OPO (n=551). Notably, only 2.2% (n=36) of families initiated donation discussions. Refusal was more likely when the patient was older, female, a DCD case, and the referral was not timely (see Table 1). Refusal was less likely when the family initiated the donation conversation.
Table 1.
Descriptive Statistics for OPO Administrative Data by Authorization Decision
| Refused N = 978 (59.2%) M (sd) |
Authorized N = 673 (40.8%) M (sd) |
F (p-value) | |
|---|---|---|---|
| Patient age (years) | 48.2 (18.5) | 43.1 (19.5) | 6.63 (.0001) |
| N (%) | N (%) | χ2 (p-value) | |
| Patient Female | 479 (48.9) | 288 (42.8) | 6.2 (.01) |
| DCD (yes) | 129 (13.2) | 64 (9.5) | 5.3 (.02) |
| Timely Referral (no) | 355 (36.3) | 196 (29.1) | 9.3 (.02) |
| Family Initiated (yes) | 6 (0.06) | 30 (4.4) | 27.6 (.0001) |
The multilevel logistic regression included all the independent variables and affirmed the bivariate findings as significantly associated with FDM authorization: refusal was significantly more likely when the patient was older (OR=1.01, 95% CL 1.01–1.02; p< .05), female (OR=1.3, 95% CL 1.1–1.5; p< .01), a DCD case (OR=1.6, 95% CL 1.2–2.2; p< .01), and the referral was not timely (OR=0.71, 95% CL .57–.87; p< .01). Refusal was less likely when the family initiated the donation conversation (OR=0.19, 95% CL .08–.41; p< .001); however, as noted above, the number of cases in which the family initiated the donation discussion was very small.
FDM Interview Sample Characteristics
Compared with FDMs from the administrative-only sample, interview participants had a higher authorization rate (χ2 (1) = 50.6; p< .0001) and were more likely to have experienced a timely referral (73.2 vs. 66.8%; χ2 (1) = 4.3; p< .04). No other statistically significant differences were observed between the two samples (data not shown).
Comparing FDMs in the interview sample who authorized and those who did not, both groups were approximately 45 years old, and the majority were female (almost 70%). A plurality of FDMs in the interview sample were married/cohabitating, had approximately 14 years of education, and almost half reported an annual household income below $30,000 (see Table 2). However, more cases with FDMs refusing donation involved potential DCD donors (n=14; 15.6%) compared to the cases that authorized (n=12; 6.45%), although these numbers are very small. AA FDMs who authorized donation did not differ from refusing FDMs on patient age, patient sex, timely referral, or whether the family initiated the donation conversation.
Table 2.
Sociodemographic characteristics of Interviewed FDM and Patient
| Characteristic | Refused n = 90 (32.6%) M (sd) |
Authorized n = 186 (67.4%) M (sd) |
t-test (p-value) |
|---|---|---|---|
| Age (years) | 45.4 (15.2) | 45.2 (15.1) | .30 (.70) |
| Education (years) | 13.8 (2.2) | 13.6 (2.5) | .50 (.46) |
| n (%) | n (%) | χ2 (p-value) | |
| Female | 64 (71.1) | 140 (75.3) | .54 (.46) |
| Marital status | 4.5 (.10) | ||
| Never Married/Single | 33 (36.7) | 46 (24.7) | |
| Married/Cohabit | 45 (50.0) | 105 (56.4) | |
| Divorced/Separated | 35 (18.8) | 12 (13.3) | |
| Household Income | .13 (.90) | ||
| <$30,000 | 43 (47.8) | 93 (50.0) | |
| $30,000–70,000 | 30 (33.3) | 60 (32.3) | |
| >$70,000 | 17 (18.9) | 33 (17.7) | |
| M (sd) | M (sd) | ||
| Patient Age (years) | 42.9 (18.3) | 43.7 (19.0) | 0.12 (.73) |
| FDM assessment of how caring and concerned the primary hospital HCP was | 5.8 (1.6) | 6.3 (1.3) | 2.18 (.03)* |
| n (%) | n (%) | χ2 (p-value) | |
| Patient Female | 41 (45.6) | 77 (41.8) | .34 (.56) |
| DCD case (yes) | 14 (15.6) | 12 (6.4) | 5.9 (.01)** |
| Timely referral (no) | 13 (14.4) | 21 (11.35) | 0.63 (.73) |
| Family initiated (yes) | 2 (2.2) | 5 (2.7) | 0.05 (.81) |
| FDM spoke with hospital staff about organ donation (yes) | 32 (35.6) | 96 (51.6) | 6.3 (.01)** |
Organ Donation Attitudes
Composite organ donation attitude scores were similar for FDMs who authorized (M=55.0, sd=8.1) and those who refused donation (M=54.0, sd=7.8). Notably, refusing FDM were less likely to agree with the statement, ‘organ donation helps families grieve’ (n=32; 35.6%) than were FDM who authorized donation (n=119; 63.9%; p<.0001).
Communication Quality, Skills, and Topics Discussed
Consistent with previously published research [22,32,33], communication variables were significantly associated with the donation decision. Nearly all communication-related items were rated less favorably by non-donor families compared to their counterparts who authorized donation (see Table 3). Refusing FDMs had fewer positive perceptions of OPO requesters’ communication skills and lower composite RCS scores than FDMs who donated (M=62.3 vs 75.5; p<.0001). The global rating of the quality of requesters’ communication during the donation discussion was also significantly lower (p<.0001) among refusing FDMs (M =3.38 vs. 4.45 for authorizing FDM), as were ratings of satisfaction with the amount of time spent speaking with the OPO requester (M=5.32 vs. 6.49; p<.0001), requesters’ handling of questions (M=5.68 vs. 6.69; p<.0001), and satisfaction with the overall organ donation request process (M=4.62 vs 6.5; p<.0001).
Table 3.
Ratings of Communication Skills and Experiences
| Refused M (sd) | Authorized M (sd) | t-test (p-value) | |
|---|---|---|---|
| Relational Communication Scale | 62.3 (15.1) | 75.5 (8.24) | 88.3 (.0001) |
| Overall communication quality with OPO requester. | 3.38 (1.43) | 4.45 (0.82) | 62.4 (.0001) |
| Satisfaction with time spent discussing donation | 5.32 (2.1) | 6.49 (0.91) | 41.3 (.0001) |
| Satisfaction with how OPO requester handled your questions | 5.68 (1.87) | 6.69 (0.70) | 42.2 (.0001) |
| Satisfaction with request process | 4.62 (2.37) | 6.5 (1.1) | 78.3 (.0001) |
| Felt pressured or harassed at the hospital about organ donation | 3.1 (2.4) | 1.75 (1.7) | 28.6 (.0001) |
| Requester Effective Communication Skills | 95.6 (15.4) | 105.8 (9.3) | 2.8 (.0001) |
| Number of Donation Related Topics Discussed | 5.5 (4.1) | 11.5 (3.8) | 142.6 (.0001) |
| N (%) | N (%) | χ2 (p-value) | |
| Surprise at request for donation (Yes) | 46 (51.1) | 83 (44.6) | 1.02 (.31) |
| Initial reaction to organ donation (Favorable) | 17 (17.8) | 108 (58.1) | 39.8 (.0001) |
Additionally, refusing families felt more pressured or harassed about the donation decision than those who authorized donation (M= 3.1 vs, 1.75; p<.0001) and were less likely to have a favorable reaction to the initial request for organ donation (17.8% vs. 58.1%; p<.0001). Non-donor families rated their requester’s use of effective communication skills lower than did families who donated (M=95.6 vs. 105.8; p<.0001) and reported discussing fewer donation-related topics with requesters (5.5 vs. 11.5; p< .001).
Regarding interactions with HCPs, refusing FDMs were less likely to report speaking with HCPs about donation (35.6% vs. 51.2%; p<.01). They also rated the care and concern of the primary HCP significantly lower (M=5.8) than those who authorized donation (M=6.3; p<.05).
The logistic regression analysis confirmed that non-donor FDMs rated their requesters’ relational communication skills lower (OR=.94), were not favorable to the initial request for donation (OR=.19), and discussed fewer donation-specific topics (OR=.76) with requesters. No other variables were significantly related to the authorization decision for this sample of AA FDMs (see Table 4).
Table 4.
Logistic Regression Examining Decision to Decline Authorization
| Variable | Odds Ratio (95% CL) |
|---|---|
| Donation helps families grieve | 0.89 (.70–1.1) |
| Relational Communication (RCS) | 0.95 (.90–.98)* |
| Quality of Communication | 1.3 (.72–2.2) |
| Satisfaction with time spent | 0.93 (.68–1.3) |
| Satisfaction with how requester answered questions | 0.96 (.52–1.5) |
| Satisfaction with request process | 0.75 (.53–1.1) |
| Initial reaction | 0.17 (.08–.43)*** |
| Pressured or harassed | 0.92 (.73–1.2) |
| Requester communication skills | 1.0 (.96–1.1) |
| Topics discussed | 0.76 (.69–.83)*** |
| FDM assessment of how caring and concerned the primary hospital HCP was | 0.96 (.74–1.2) |
| FDM spoke with hospital staff about organ donation | .80 (.38–1.7) |
Note: CL = Confidence Limit.
= p< .05
= p< .0001
DISCUSSION
These results emphasize the critical need for culturally-appropriate communication skills to be deployed with AA families throughout the organ donation conversation. The amount of time spent talking about organ donation and a sensitivity to assuring that FDMs feel neither pressured nor harassed are easily modifiable aspects of the discussion. Refusing FDMs in the interview sample reported greater dissatisfaction with the amount of time spent discussing donation. FDMs who declined the donation opportunity were more likely to report feeling pressured about organ donation and although the multilevel logistic regression found no significant interaction between these two variables, they appear to contribute to the overall decision not to authorize donation.
A major difference found between interviewed AA families who authorized donation and those who did not was that the former was more likely to report higher satisfaction with the overall quality of their communications about donation with the OPO requester. This included the OPO requester using higher levels of relational and effective communication skills such as listening carefully to the FDMs, taking their concerns seriously, being responsive to these concerns, giving FDMs enough time to discuss important issues, checking in with and summarizing their understanding about donation, encouraging FDMs to continue talking, responding to strong emotion with sensitivity and empathy, and offering additional services or assistance. This is consistent with prior studies showing a positive relationship between high quality communication skills and donation behaviors in other populations [3,32,34].
This study found little difference in attitudes toward organ donation between AA FDMs who authorized donation and those who refused. This interesting finding is in contrast to differences found between donors and nondonors in samples that are mostly white. AAs have been reported to not donate due to mistrust in the health system. However, in this study, the specific issue of mistrust in the donation system, as indicated by worry that doctors would not do as much to save their lives if their desire to donate was known [34], was not found. This may be indication of the successes achieved by disseminating public education about organ donation to AAs by groups through programs like MOTTEP.
This study underscores the body of work that has demonstrated the critical roles of the content of the donation discussion and how messages are delivered. These two factors can mean the difference between AA family authorization or refusal [22,32]. Compared to non-donor families, authorizing AA FDMs reported discussing more than double the number of donation related topics with OPO requesters, including the opportunity to help someone in need, the patienťs eligibility to donate, the need for organs, the timeframes for the donation decision and donation process, the ability to choose the organs for donation, and the treatment of the donor patienťs body during organ recovery. Both the content and the number of topics discussed has repeatedly emerged as predictive of donation behavior in large interview studies of FDMs [22,32]. In particular, two topics most frequently discussed with authorizing FDMs and not with non-donor families were costs associated with organ donation and the distribution of donated organs. These two topics have reliably predicted organ donation behavior among AAs in other studies and speak to differentials in healthcare coverage and trust in the healthcare system by AAs compared to white Americans [14,32]. Culturally-appropriate communication is crucial, including explicitly addressing the concerns that AAs have consistently expressed about the equity of the healthcare system and medical debt. These must be incorporated in requesters’ presentation of the option of donation to all AA families.
Prior research has suggested that one of the most powerful predictors of organ donation behavior is the FDM’s initial response to the request [32]. Among FDMs with an initially favorable response, donation rates have been reported as high as 85.1% [35]. It has also been reported that when hospital and OPO staff anticipate a favorable response to a request for organ donation, they are more likely to engage in lengthier and more detailed discussions with the FDMs. However, hospital and OPO staff have been shown to misclassify initial reactions to donation among AA FDMs at a higher rate than Caucasians (23.5 vs. 8.6%) [14]. Failure to present the donation option effectively or to deny FDMs the option of donation altogether, increases the likelihood of decisional regret. Indeed, 32% of AA FDMs who chose not to donate indicated they would not make the same decision again compared to only 3.8% of those who did donate. Moreover, many FDMs indicated they would have welcomed more information and continued dialogue about the organ donation option. This is consistent with Morais, et al. [36], who found many families who previously refused donation later came to advocate donation after learning more about it.
Although much of this study focuses on requesters’ communication and skills, initial receptivity to organ donation may reflect the family’s experience with the hospital healthcare team prior to the donation request. Refusing FDMs rated the care and concern of the patient’s primary HCP lower than authorizing FDMs. These results reveal the association between the donation decision and the coordination between HCPs and OPO staff. In this study, AA FDMs who refused donation were less likely to speak with HCPs about donation-related topics even though they play a vital role in helping families make informed decisions about donation. This research team’s past study with 2,358 HCPs in 77 US hospitals found that the majority of HCPs continue to view OPO staff as outsiders rather than part of the healthcare team [37]. A multidisciplinary request protocol involving both HCPs and OPO staff in family donation conversations has proven effective in increasing rates of organ donation [38–40]. Future interventions should develop and test techniques for practical HCP-OPO collaboration during donation opportunities.
While this study provides insight into a large, nationwide sample of AAs who made organ donation decisions for potential donors, it has some limitations. First, interviewees were asked to recall emotional events that had occurred months previously, creating potential bias from errors in memory. Second, interview participants had a significantly higher rate of authorization compared to those not interviewed, suggesting possible selection bias, limiting generalizability. However, the bias is more likely to reflect even more pronounced dissatisfaction with communication suggesting that the results would have been strengthened if these individuals had participated in the study. Finally, although we drew our nine OPOs from a geographic spectrum, these OPOs may not be wholly representative of all 58 OPOs that operate within the US. However, these methods are similar to most of the large studies conducted and reported in the literature over many years with these populations. The consistency of findings across these studies provides confidence in the validity of these results.
CONCLUSION
This study draws from a large national sample to examine the differences between AA families who authorize and refuse organ donation at the bedside. The most important element that differentiated the decisions of the families was the communication process and skills exhibited by OPO requesters and not attitudes about donation. Families who met with more skilled communicators were more likely to donate than those who had a more attenuated and less rich communication experience about organ donation. Furthermore, interactions with HCPs can affect a family’s decision. These results indicate that the reasons behind many AA families’ decisions to refuse donation are not, as some believe, immutable because of negative pre-existing attitudes toward organ donation but are responsive to careful and sensitive communication and support.
Several considerations are recommended to correct the current disparities in AA donation. Although no studies have ever identified any personality characteristics associated with success as a donation professional, the ability to engage with, actively listen to and empathize with families is critical. Some of these skills can be taught and, most importantly, should be criteria for evaluating their OPO staff performance. Communication-enhancing skills training is essential to success. Finally, donor professionals need to become culturally- and linguistically proficient. Although training for all donor professionals is important, we also need greater diversity in the OPO workforce.
Supplementary Material
Acknowledgments
This research was funded by grants #R01DK081118 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and #R39OT10581 from the Division of Transplantation, Health Resources & Services Administration, U.S. Department of Health and Human Services (HRSA).
Abbreviations
- AA
African American
- DCD
Donation after Cardiac Death
- FDM
Family Decision Maker
- HCP
Healthcare Provider
- MOTTEP
Minority Organ Tissue Transplant Education Program
- OPO
Organ Procurement Organization
- RCS
Relational Communication Scale
Footnotes
Conflicts of interest/Competing interests: The authors declare no conflicts of interest.
Clinical Trial Notation: NCT02138227
DECLARATIONS
Availability of data and material: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability: Not applicable
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- 1.Organ Procurement and Transplantation Network (OPTN). Data - OPTN.
- 2.Goldberg DS, Halpern SD, Reese PP. Deceased Organ Donation Consent Rates Among Racial and Ethnic Minorities and Older Potential Donors*. Crit Care Med. NIH Public Access; 2013;41:496–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siminoff L, Mercer MB, Graham G, Burant C. The Reasons Families Donate Organs for Transplantation: Implications for Policy and Practice. J Trauma Inj Infect Crit Care. 2007/04/12. 2007;62:969–78. [DOI] [PubMed] [Google Scholar]
- 4.Sehgal NKR, Scallan C, Sullivan C, Cedeño M, Pencak J, Kirkland J, et al. The Relationship Between Verified Organ Donor Designation and Patient Demographic and Medical Characteristics. Am J Transplant. NIH Public Access; 2016;16:1294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.HHS Hrsa. National Survey of Organ Donation Attitudes and Practices, 2019: Report of Findings. 2019.
- 6.Callender CO. Organ donation in blacks: a community approach. Transplant Proc. 1987;19:1551–4. [PubMed] [Google Scholar]
- 7.Callender CO, Bayton JA, Yeager C, Clark JE. Attitudes among blacks toward donating kidneys for transplantation: a pilot project. J Natl Med Assoc. National Medical Association; 1982;74:807–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Callender CO, Miles P V. Minority Organ Donation: The Power of an Educated Community. J Am Coll Surg. 2010;210:708–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callender CO, Hall MB, Branch D. An assessment of the effectiveness of the Mottep model for increasing donation rates and preventing the need for transplantation--adult findings: program years 1998 and 1999. Semin Nephrol. 2001;21:419–28. [DOI] [PubMed] [Google Scholar]
- 10.Callender CO, Miles P V, Hall MB. National MOTTEP: educating to prevent the need for transplantation. Minority Organ Tissue Transplant Education Program. Ethn Dis. 2002;12:S134–7 [PubMed] [Google Scholar]
- 11.Morgan SE, Miller JK, Arasaratnam LA. Similarities and Differences Between African Americans’ and European Americans’ Attitudes, Knowledge, and Willingness to Communicate About Organ Donation1. J Appl Soc Psychol. 2003;33:693–715. [Google Scholar]
- 12.Terrell F, Moseley KL, Mosley KL, Terrell AS, Nickerson KJ. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. J Natl Med Assoc. American Psychological Association; 2004;96:53–60. [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzgerald C, Hurst S. Implicit bias in healthcare professionals: A systematic review. BMC Med Ethics. BioMed Central Ltd.; 2017;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siminoff LA, Lawrence RH, Arnold RM. Comparison of black and white families’ experiences and perceptions regarding organ donation requests. Crit Care Med. 2003/01/25. 2003;31:146–51. [DOI] [PubMed] [Google Scholar]
- 15.Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int. J. Nurs. Stud. Elsevier Ltd; 2019. [DOI] [PubMed] [Google Scholar]
- 16.Bodenheimer HC, Okun JM, Tajik W, Obadia J, Icitovic N, Friedmann P, et al. The impact of race on organ donation authorization discussed in the context of liver transplantation. Trans Am Clin Climatol Assoc. 2012;123:64–77; discussion 77–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Donate Life America. Always In Action - 2018 Annual Report. Richmond, VA; 2018. [Google Scholar]
- 18.Korda H, Wagstaff DA, McCleary KJ. How African Americans Express Their Intentions to Be Organ Donors. Prog Transplant. SAGE PublicationsSage CA: Los Angeles, CA; 2007;17:275–80. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services (DHHS). Organ Donation Statistics.
- 20.Thornton JD, Wong KA, Cardenas V, Curtis JR, Spigner C, Allen MD. Ethnic and Gender Differences in Willingness among High School Students to Donate Organs. J Adolesc Heal. 2006;39:266–74. [DOI] [PubMed] [Google Scholar]
- 21.Edwards TM, Essman C, Daryl Thornton J, Cleveland M. Assessing Racial and Ethnic Differences in Medical Student Knowledge, Attitudes and Behaviors Regarding Organ Donation. 2007. [PMC free article] [PubMed]
- 22.Siminoff LA, Traino HM, Genderson MW. Communicating Effectively About Organ Donation. Transplant Direct. Wolters Kluwer Health; 2015;1:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verheijde JL, Rady MY, McGregor JL. The United States Revised Uniform Anatomical Gift Act (2006): New challenges to balancing patient rights and physician responsibilities. Philos. Ethics, Humanit. Med. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ehrle R. Timely referral of potential organ donors. Prog Transplant. 2008/04/24. 2008;18:17–21. [DOI] [PubMed] [Google Scholar]
- 25.Siminoff LA, Alolod GP, Wilson-Genderson M, Yuen EYN, Traino HM. A Comparison of Request Process and Outcomes in Donation After Cardiac Death and Donation After Brain Death: Results From a National Study. Am J Transplant. NIH Public Access; 2017;17:1278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Traino HM, Molisani AJ, Siminoff LA. Regional Differences in Communication Process and Outcomes of Requests for Solid Organ Donation. Am J Transplant. NIH Public Access; 2017;17:1620–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pelletier M. The organ donor family members’ perception of stressful situations during the organ donation experience. J Adv Nurs. 1992/01/01. 1992;17:90–7. [DOI] [PubMed] [Google Scholar]
- 28.Pelletier ML. The needs of family members of organ and tissue donors. Heart Lung. 1993;22:151–7. [PubMed] [Google Scholar]
- 29.Burgoon JK, Hale JL. Validation and measurement of the fundamental themes of relational communication. Commun Monogr. Taylor & Francis Group; 1987;54:19–41. [Google Scholar]
- 30.Siminoff LA, Molisani AJ, Traino HM. A Comparison of the Request Process and Outcomes in Adult and Pediatric Organ Donation. Pediatrics. American Academy of Pediatrics; 2015;136:e108–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.SAS. SAS 9.4. Cary, NC: SAS Institute, Inc.; 2017. [Google Scholar]
- 32.Siminoff LA. Factors Influencing Families’ Consent for Donation of Solid Organs for Transplantation. JAMA. American Medical Association; 2001;286:71. [DOI] [PubMed] [Google Scholar]
- 33.Siminoff LA, Traino HM, Gordon N. Determinants of Family Consent to Tissue Donation. J Trauma Inj Infect Crit Care. 2010;69:956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siminoff LA, Burant CJ, Ibrahim SA. Racial Disparities in Preferences and Perceptions Regarding Organ Donation. J Gen Intern Med. 2006/08/22. 2006;21:060721075157037–??? [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siminoff LA, Arnold RM, Hewlett J. The process of organ donation and its effect on consent. Clin Transplant. John Wiley & Sons, Ltd (10.1111); 2001;15:39–47. [DOI] [PubMed] [Google Scholar]
- 36.Morais M, da Silva RCMA, Duca WJ, Rol JL, de Felicio HCC, Arroyo PC, et al. Families Who Previously Refused Organ Donation Would Agree to Donate in a New Situation: A Cross-sectional Study. Transplant Proc. Elsevier; 2012;44:2268–71. [DOI] [PubMed] [Google Scholar]
- 37.Traino HM, Alolod GP, Shafer T, Siminoff LA. Interim Results of a National Test of the Rapid Assessment of Hospital Procurement Barriers in Donation (RAPiD). Am J Transplant. 2012;12:3094–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bocci MG, D’Alò C, Barelli R, Inguscio S, Prestifilippo A, Di Paolo S, et al. Taking Care of Relationships in the Intensive Care Unit: Positive Impact on Family Consent for Organ Donation. Transplant Proc. Elsevier; 2016;48:3245–50. [DOI] [PubMed] [Google Scholar]
- 39.Potter JE, Perry L, Elliott RM, Aneman A, Brieva JL, Cavazzoni E, et al. Communication with Families Regarding Organ and Tissue Donation after Death in Intensive Care (COMFORT): a multicentre before-and-after study. Crit Care Resusc. 2018;20:268–76. [PubMed] [Google Scholar]
- 40.Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ. BMJ Publishing Group; 2009;338:b991–b991. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.