Abstract
Objective
To identify the CT findings associated with treatment failure after antibiotic therapy for acute appendicitis.
Materials and Methods
Altogether, 198 patients who received antibiotic therapy for appendicitis were identified by searching the hospital's surgery database. Selection criteria for antibiotic therapy were uncomplicated appendicitis with an appendiceal diameter equal to or less than 11 mm. The 86 patients included in the study were divided into a treatment success group and a treatment failure group. Treatment failure was defined as a resistance to antibiotic therapy or recurrent appendicitis during a 1-year follow-up period. Two radiologists independently evaluated the following CT findings: appendix–location, involved extent, maximal diameter, thickness, wall enhancement, focal wall defect, periappendiceal fat infiltration, and so on. For the quantitative analysis, two readers independently measured the CT values at the least attenuated wall of the appendix by drawing a round region of interest on the enhanced CT (HUpost) and non-enhanced CT (HUpre). The degree of appendiceal wall enhancement (HUsub) was calculated as the subtracted value between HUpost and HUpre. A logistic regression analysis was used to identify the CT findings associated with treatment failure.
Results
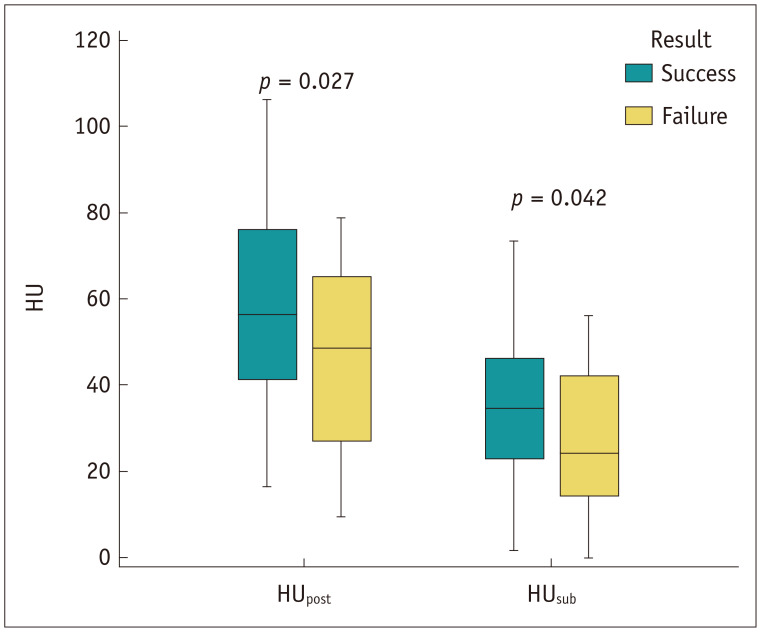
Sixty-four of 86 (74.4%) patients were successfully treated with antibiotic therapy, with treatment failure occurring in the remaining 22 (25.5%). The treatment failure group showed a higher frequency of hypoenhancement of the appendiceal wall than the success group (31.8% vs. 7.8%; p = 0.005). Upon quantitative analysis, both HUpost (46.7 ± 21.3 HU vs. 58.9 ± 22.0 HU; p = 0.027) and HUsub (26.9 ± 17.3 HU vs. 35.4 ± 16.6 HU; p = 0.042) values were significantly lower in the treatment failure group than in the success group.
Conclusion
Hypoenhancement of the appendiceal wall was significantly associated with treatment failure after antibiotic therapy for acute appendicitis.
Keywords: Appendicitis; Tomography, X-ray computed; Antibiotic; Therapy; Treatment failure
INTRODUCTION
Appendectomy has been established as the standard treatment for acute appendicitis, which is the most common cause of right lower quadrant pain in emergency departments (1). Although the advent of laparoscopic appendectomy has significantly decreased postoperative complications, surgery-related morbidity and mortality cannot be completely avoided (2,3). Recently, many clinical trials and meta-analyses have reported evidence supporting the safety and effectiveness of antibiotic therapy as an alternative to appendectomy for acute appendicitis (4,5,6,7,8,9,10,11). Antibiotic therapy for appendicitis has been reported to have a lower risk of complications, less pain, reduced costs, and lower hospital stay lengths than surgical therapy (4,6,12).
However, the success rates of antibiotic therapy have varied widely across clinical trials, and the reported 1-year treatment failure rates, ranging from 19.3% to 40.0%, have been a concern, which leads many surgeons and patients to avoid antibiotic therapy (4,5,6,7,8,13). The unsatisfactory success rates in the previous clinical trials may be associated with the criteria used to select patients for enrollment. Previously, trials enrolled patients with acute appendicitis diagnosed only by clinical examination, without excluding complicated cases of appendicitis that were based on radiological evaluations (4,5,6). Since then, recent trials have excluded patients with complicated appendicitis that present with any of the following CT findings: abscess, phlegmon, extraluminal gas, extraluminal appendicolith, or when a tumor is suspected. These exclusion criteria have been focused on obvious acute appendicitis perforations on CT scans, and do not take microperforations or nonperforated infarctions into account (7,8).
We hypothesized that an appropriate selection of patients for antibiotic therapy, based on a more detailed analysis of CT imaging features, would be helpful in lowering the failure rate and increasing the success rate of antibiotic therapy in patients with acute appendicitis. Therefore, the purpose of this retrospective study was to compare the CT findings between the treatment success and failure groups after antibiotic therapy, in patients with acute appendicitis, and identify the CT findings associated with treatment failure as possible exclusion criteria.
MATERIALS AND METHODS
Patient Population
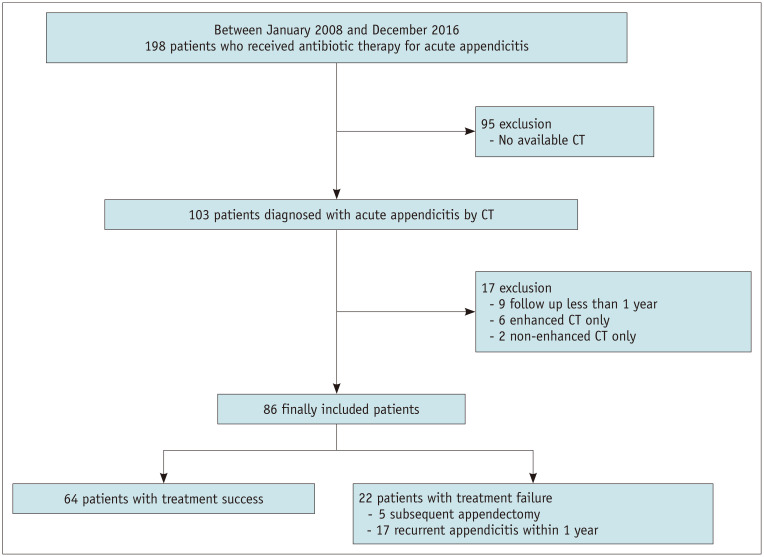
This retrospective study was approved by an ethical committee and a waiver of the requirement for informed consent was obtained. Between January 2008 and December 2016, 198 patients who received antibiotic therapy for acute appendicitis were identified by searching the surgery database. Of these patients, 83 and 68 patients, a total of 151 patients, participated in two clinical trials investigating the clinical outcome of antibiotic therapy for uncomplicated appendicitis performed by our surgery department, respectively (14,15). The remaining 47 patients were elderly or patients with comorbidities including heart disease, neurologic diseases such as dementia or Parkinson's disease, chronic obstructive pulmonary disease, diabetes mellitus, and renal disease. According to the protocol of our surgery department, only patients with uncomplicated appendicitis and an appendiceal diameter equal or less than 11 mm were considered for antibiotic therapy (14,15). Uncomplicated appendicitis was defined as cases with no signs of complications such as extraluminal air, extraluminal appendicoliths, abscesses, or phlegmon. Appendiceal diameter was measured as the maximum outer diameter excluding luminal fluid of the appendix. Of these 198 patients, 112 were excluded for the following reasons: 95 had no CT available; 9 were followed up for less than 1 year; 6 underwent enhanced CT scanning only; 2 underwent non-enhanced CT scanning only. Therefore, 86 patients were included in the present study (Fig. 1). They consisted of 41 male patients (mean age ± standard deviation [SD], 41.5 ± 18.5 years [range, 16–87 years]) and 45 female patients (mean age ± SD , 42.7 ± 17.3 years [range, 17–86 years]), of whom 64 patients were successfully treated with antibiotic therapy and did not have a recurrence during the 1-year follow up (success group). The remaining 22 patients showed treatment failure (failure group).
Fig. 1. Flow diagram of the study population.
Medical Records
The medical records of the patients were reviewed by one investigator. Data on patient age, sex, laboratory findings including white blood cell (WBC) count and C-reactive protein (CRP) levels, body temperature on the day of admission, duration of symptoms, and clinical outcomes, were obtained from the hospital medical records. Altogether, 86 patients received antibiotic therapy consisting of intravenous administration of second-generation cephalosporin and metronidazole for 48 hours, with a 24-hour fasting period. After the initial period, clinical symptom progression and laboratory parameter deterioration (i.e., increased WBC and/or CRP levels on admission day 3) were considered to indicate a resistance to the therapy, and an appendectomy was subsequently performed. Patients who exhibited an improvement of clinical symptoms and laboratory parameters were discharged with additional oral antibiotic therapy for 2 days. Treatment success was defined as symptom improvement and no recurrence during the 1-year follow-up period. Treatment failure was defined as a resistance to antibiotic therapy or recurrent appendicitis during the 1-year follow-up period. Recurrent appendicitis was defined as the presence of repeated symptoms and disease confirmed by CT scanning or ultrasonography. The patients included in the study were divided into a treatment success group (success group) and a treatment failure group (failure group).
Multi-Detector CT Imaging Acquisition
All CT examinations were performed using one of three multi-detector CT scanners: a 64-detector CT (Brilliance 64, Philips Healthcare), and two 128-detector CT (SOMATOM Definition Edge and SOMATOM Definition Flash, Siemens Healthineers). CT parameters were as follows: detector configuration, 64 × 0.625 mm and 128 × 0.625 mm, respectively; tube current, 140–200 mAs; tube voltage, 100 or 120 kVp; slice thickness, 5 mm; reconstruction interval, 5 mm; gantry rotation time, 0.5 seconds. Non-enhanced and enhanced CT images were obtained from the dome of the diaphragm to the symphysis pubis in all 86 patients. Both transverse and coronal reconstruction images were acquired.
CT Image Analyses
All transverse and coronal reconstruction images were retrospectively reviewed on a picture archiving and communication system (PACS) workstation (M6, INFINITT Healthcare) independently by two radiologists (with 15 and 7 years of clinical experience in abdominal imaging, respectively). All continuous data are represented as the mean values from both readers. In cases of disagreement between the two readers regarding the categorical data, they reviewed the data again until a consensus was reached. They were aware of the diagnosis of acute appendicitis but blinded to the initial CT report, clinical and laboratory data, and patient outcomes.
Visual Assessment of CT Images
The following CT findings were evaluated: location of the appendix (peritoneal or retroperitoneal); involved extent of appendicitis (focal [≤ 50%] or diffuse [> 50%]); maximal diameter of the appendix; maximal thickness of the appendiceal wall; appendiceal wall enhancement; periappendiceal fat infiltration; focal wall defect; appendicolith; intraluminal air; periappendiceal fluid; adjacent small bowel ileus; lymphadenopathy; cecal wall thickening; and terminal ileal wall thickening.
The maximal diameter of the appendix was measured from the outer-to-outer border diameter of the appendix in the short axis. The maximal thickness of the appendiceal wall was measured at the greatest wall thickness of the inflamed appendix. Appendiceal wall enhancements were categorized into two groups: iso- or hyperenhancement; and hypoenhancement, compared to the enhancement of the adjacent small bowels. Periappendiceal fat infiltration was categorized into two groups: none or perceptible fat stranding; and confined to or beyond the mesoappendix. A focal wall defect of the appendix was defined as a focal interruption or discontinuity in the enhancement of the appendiceal wall. An appendicolith was defined as a well-defined round or oval radiodense structure within the appendix. Intraluminal appendiceal air referred to air densities within the lumen of the appendix. Periappendiceal fluid was defined as poorly defined extraluminal fluid, without encapsulation, with a depth > 1 cm. Adjacent small bowel ileus referred to the fluid-filled dilatation of the small bowel adjacent to the appendix. Lymphadenopathy was defined as multiple clustered lymph nodes in the right lower quadrant area.
Quantification of Appendiceal Wall Enhancements
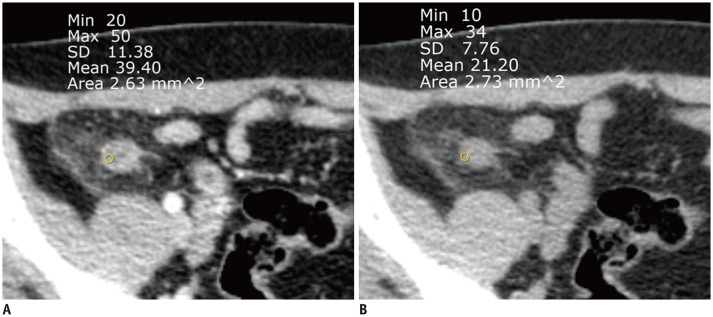
For the quantitative analysis of appendiceal wall enhancements, two readers independently measured the Hounsfield unit (HU) values of the appendiceal walls in both the enhanced and non-enhanced CT scans. During the visual assessment of the enhanced CT images, they checked the least attenuated site of the appendiceal wall, including the focal hypoenhancements or focal defects in the appendiceal walls. After full magnification of the CT images, a round region of interest (ROI) was placed at the least attenuated site within the appendix walls, which was done using the PACS workstation. First, mean CT HU values were measured on the enhanced CTs (HUpost), and then other mean CT HU values were measured at the corresponding areas of the non-enhanced CTs (HUpre) (Fig. 2). The degree of appendiceal wall enhancement (HUsub) for each patient was calculated as the subtraction of the mean CT HU values between the enhanced and non-enhanced CT (i.e., HUsub = HUpost - HUpre).
Fig. 2. Quantitative measurement of the appendiceal wall enhancement.
A 32-year-old woman with acute appendicitis was treated with antibiotic therapy, and recurrent appendicitis occurred after 93 days (failure group).
A. A mean CT HU value (39 HU) was obtained by drawing a round ROI within the appendiceal wall that showed the least enhancement on the contrast-enhanced CT, which is indicated by HUpost. B. A corresponding round ROI was placed on the non-enhanced CT. The mean HU value (21 HU) was measured in the same fashion, which is indicated by HUpre. Therefore, the degree of the appendiceal wall enhancement (HUsub = 18) was calculated by subtracting HUpost and HUpre. HUpost = mean HU values at the least enhanced part of the appendiceal wall on contrast-enhanced images, HUpre = mean HU values at the corresponding part of appendiceal wall on non-enhanced images, HUsub = subtracted value of the mean HU values at the least enhanced part of the appendiceal wall between contrast-enhanced CTs (HUpost) and non-enhanced CTs (HUpre) (i.e., HUsub = HUpost - HUpre). HU = Hounsfield unit, ROI = region of interest, SD = standard deviation
Statistical Analyses
All statistical analyses were performed using SPSS version 24.0 (IBM Corp.) and MedCalc 18.11.6 (MedCalc Software); p < 0.05 was considered to be statistically significant. Pearson's chi-squared test or Fisher's exact test was used for categorical data, as appropriate. The independent t test or Mann-Whitney U tests were used, as appropriate, for continuous data with normal or non-normal distributions. A univariate logistic regression analysis was used to identify the CT findings associated with the treatment failure after antibiotic therapy. Results are expressed as odds ratio (OR) with corresponding 95% confidence intervals (CIs) and p values. For the quantitative analysis of the appendiceal wall enhancements, the independent t test was used to compare the CT HU values between the two groups. Interobserver agreement was assessed by intraclass correlation coefficients (ICCs) for continuous data, or by Cohen's kappa (κ) for categorical data. An ICC/κ value > 0.80 was regarded as excellent agreement, ICC/κ of around 0.61–0.80 as substantial agreement, ICC/κ of 0.41–0.60 as moderate agreement, ICC/κ of 0.21–0.40 as fair agreement, and ICC/κ < 0.20 as poor agreement (16,17).
RESULTS
There were no significant differences between the two groups in terms of patient characteristics (Table 1). Among the 22 patients in the failure group, five patients did not respond to antibiotic therapy within 1 month and underwent a subsequent appendectomy. They were confirmed to have acute perforated appendicitis (n = 1) and acute suppurative appendicitis (n = 4) by pathologic reports. The remaining 17 patients experienced recurrent symptoms and they were diagnosed with recurrent appendicitis by radiological evaluation, such as CT (n = 12) or ultrasound (n = 5), within the 1-year follow up. In total, 15 of 17 patients underwent an appendectomy and the remaining 2 patients did not undergo an operation, and were instead managed with repeated antibiotic therapy (Supplementary Table 1).
Table 1. Clinical and Laboratory Characteristics between Treatment Success and Failure Groups.
| Characteristics | Treatment Group | P | |
|---|---|---|---|
| Success (n = 64) | Failure (n = 22) | ||
| Age (years) | 43.1 ± 19.1 | 39.1 ± 13.1 | 0.621 |
| Sex, n (%) | 0.218 | ||
| Male | 33 (51.6) | 8 (36.4) | - |
| Female | 31 (48.4) | 14 (63.6) | - |
| WBC on admission (x 1000/L) | 11.16 ± 4.03 | 13.00 ± 3.22 | 0.057 |
| CRP on admission (mg/L) | 38.11 ± 48.17 | 28.17 ± 41.37 | 0.469 |
| Body temperature (°C) | 37.21 ± 0.68 | 37.39 ± 0.67 | 0.283 |
| Symptom duration (days) | 2.3 ± 2.3 | 1.7 ± 0.7 | 0.728 |
Data presented as mean ± standard deviation unless otherwise indicated. CRP = C-reactive protein, WBC = white blood cell
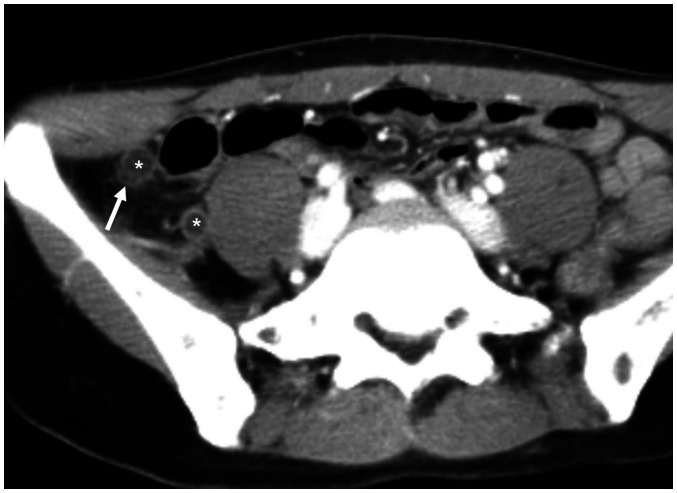
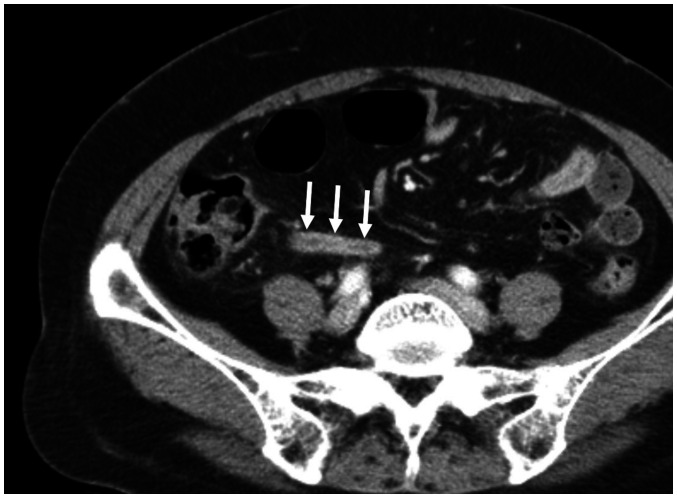
The CT findings from the treatment success and failure groups were analyzed (Table 2). The failure group showed a higher frequency of hypoenhancement in their appendiceal walls than the success group (31.8% vs. 7.8%, respectively; p = 0.005) (Fig. 3), while the success group showed a higher frequency of iso- or hyperenhancement in their appendiceal walls (Fig. 4). According to the results of the univariate logistic regression analysis, an appendiceal wall hypoenhancement (OR 5.507 [95% CI 1.531–19.805]; p = 0.009) was significantly associated with treatment failure. The maximal diameter of appendix was larger in the failure group than in the success group (9.99 ± 1.67 mm vs. 9.18 ± 1.81 mm, respectively); the difference, however, was not statistically significant (p = 0.070). The maximal thickness of the appendiceal wall was not significantly different between the two groups. The appendix was frequently located in patients' peritoneal space, and diffuse involvement of appendicitis was more frequent than focal involvement in both groups. Other CT findings including periappendiceal fat infiltration, focal wall defects, appendicoliths, intraluminal air, periappendiceal fluid, adjacent small bowel ileus, cecal thickening, terminal ileal thickening, and lymphadenopathy were not significantly different between the treatment success and failure groups. We observed substantial to excellent interobserver agreements with ICC values of 0.623–0.927 for the CT findings, except for focal wall defects and periappendiceal fluid (Supplementary Table 2).
Table 2. Comparison of CT Findings between the Success and Failure Groups.
| CT Findings | Success Group (n = 64) | Failure Group (n = 22) | P | Univariate Regression | ||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | ||||
| Location | 0.711 | |||||
| Peritoneal | 57 (89.1) | 19 (86.4) | 0.778 | 0.183–3.312 | 0.734 | |
| Retroperitoneal | 7 (10.9) | 3 (13.6) | Reference | |||
| Involved extent | 1.000 | |||||
| Focal | 5 (7.8) | 1 (4.5) | Reference | |||
| Diffuse | 59 (92.2) | 21 (95.5) | 1.780 | 0.196–16.126 | 0.608 | |
| Maximal diameter of appendix (mm) | 9.18 ± 1.81 | 9.99 ± 1.67 | 0.070 | 1.290 | 0.975–1.714 | 0.075 |
| Maximal thickness of appendiceal wall (mm) | 2.62 ± 0.86 | 2.68 ± 1.03 | 0.808 | 1.070 | 0.624–1.837 | 0.805 |
| Appendiceal wall enhancement | 0.005* | |||||
| Iso- or hyperenhancement | 59 (92.2) | 15 (68.2) | Reference | |||
| Hypoenhancement | 5 (7.8) | 7 (31.8) | 5.507 | 1.531–19.805 | 0.009* | |
| Periappendiceal fat infiltration | 0.228 | |||||
| No or only perceptible stranding | 44 (68.8) | 12 (54.5) | Reference | |||
| Confined to or beyond mesoappendix | 22 (31.3) | 10 (45.5) | 1.833 | 0.680–4.943 | 0.231 | |
| Focal wall defect | 12 (18.8) | 8 (36.4) | 0.092 | 2.476 | 0.848–7.231 | 0.097 |
| Appendicolith | 10 (15.6) | 7 (31.8) | 0.100 | 2.520 | 0.820–7.743 | 0.107 |
| Intraluminal air | 13 (20.3) | 4 (18.2) | 1.000 | 0.872 | 0.252–3.021 | 0.829 |
| Periappendiceal fluid | 2 (3.1) | 1 (4.5) | 1.000 | 1.476 | 0.127–17.123 | 0.755 |
| Adjacent small bowel ileus | 20 (31.3) | 7 (31.8) | 0.960 | 1.027 | 0.362–2.908 | 0.960 |
| Cecal wall thickening | 10 (15.6) | 3 (13.6) | 1.000 | 0.853 | 0.212–3.430 | 0.822 |
| Terminal ileal wall thickening | 8 (12.5) | 3 (13.6) | 1.000 | 1.105 | 0.266–4.597 | 0.891 |
| Lymphadenopathy | 18 (28.1) | 8 (36.4) | 0.468 | 1.460 | 0.524–4.072 | 0.469 |
Data presented as number (percentage) unless otherwise indicated. *p < 0.05 (significant). CI = confidence interval, OR = odds ratio
Fig. 3. A 46-year-old woman in the failure group.
The contrast-enhanced axial CT shows diffuse dilatation of the appendix (*) with a maximal diameter of 10.3 mm, focal hypoenhancement of the appendiceal wall (arrow), and mild peritoneal fat infiltration. The patient was treated with antibiotic therapy and the patient's condition improved, but recurrent appendicitis developed after 198 days.
Fig. 4. A 61-year-old woman in the success group.
The contrast-enhanced axial CT shows mild dilatation of the appendix, with a maximal diameter of 8.3 mm, hyperenhancement of the appendiceal wall (arrows), and no periappendiceal fat stranding. She was successfully treated with antibiotic therapy and no recurrence occurred.
The quantitative analysis of appendiceal wall enhancements revealed that the failure group showed significantly lower HU values for the appendiceal wall on enhanced CT scans (HUpost) than the success group (46.7 ± 21.3 HU vs. 58.9 ± 22.0 HU, respectively; p = 0.027). The degree of appendiceal wall enhancement (HUsub) was also significantly lower in the treatment failure group than in the success group (26.9 ± 17.3 HU vs. 35.4 ± 16.6 HU, respectively; p = 0.042) (Fig. 5). Interobserver agreement was excellent, with ICC values of 0.943 (0.913–0.963) for HUpost and 0.904 (0.853–0.938) for HUsub.
Fig. 5. Box-and-whisker plots of comparisons of the HUpost and HUsub values between the success and failure groups.
HUpost values were significantly lower in the failure group than in the success group (46.7 ± 21.3 HU vs. 58.9 ± 22.0 HU, respectively; p = 0.027). The degrees of the appendiceal wall enhancements (HUsub) were also significantly lower in the failure group than in the success group (26.9 ± 17.3 HU vs. 35.4 ± 16.6 HU, respectively; p = 0.042).
DISCUSSION
Our study identified the CT finding associated with treatment failure after antibiotic therapy for patients with acute appendicitis without obvious perforations. Compared to the success group, the failure group had a higher frequency of hypoenhancement of the appendiceal wall, which was a significant factor associated with treatment failure. This was determined by a univariate logistic regression analysis. The quantitative assessment of the appendiceal wall enhancements revealed that both HUpost and HUsub values were lower in the failure group than in the success group.
Recent clinical trials that provided antibiotic therapy for patients with uncomplicated appendicitis excluded patients with complicated appendicitis, which was confirmed based on CT results. They defined CT findings of complicated appendicitis as cases presenting with extraluminal gas, periappendiceal fluid, disseminated intraperitoneal fluid, appendicoliths, perforations, and abscesses (7,8). These CT findings have been observed in patients with perforated appendicitis, and were similar to the exclusion criteria used for our patient selection, which determined their suitability for antibiotic therapy. Previous clinical trials as well as the present study demonstrated a high failure rate, ranging from 25.0% to 36.7%, which could, in part, be due to a failure to detect complicated appendicitis on CT scans (7,8,18). In the literature, complicated appendicitis has been defined as appendicitis intractable to conservative management due to perforation or gangrenous change of appendicitis (18,19). However, only perforated appendicitis has been considered as complicated appendicitis, which was an important exclusion criterion in previous clinical trials. Patients with nonperforated gangrenous appendicitis or necrotic appendicitis were included and managed with antibiotic therapy for appendicitis, which may be a reason for the high failure rate.
To our knowledge, few studies have directly compared detailed the CT findings between treatment success and failure groups in patients who underwent antibiotic therapy for acute uncomplicated appendicitis. Our results demonstrated that hypoenhancement of the appendiceal wall was associated with treatment failure after antibiotic therapy for acute nonperforated appendicitis, and increased the likelihood of developing complications in the near future. A reduced or absent enhancement of the bowel wall on contrast-enhanced CT scans has been the most specific CT finding for the diagnosis of bowel ischemia (20). In the same context, hypoenhancement of the appendiceal wall, compared with the adjacent small bowel, implies ischemia or gangrenous changes in the appendix. Although many studies have differentiated perforated appendicitis from nonperforated appendicitis (18,21,22,23), not much is known about how to detect nonperforated gangrenous appendicitis or necrotic appendicitis (24,25,26). The reported CT findings of gangrenous appendicitis included focal or diffuse loss of mural perfusion, thinning of the appendiceal wall, intraluminal gas, and intraluminal appendicoliths (24,25,26). The hypoenhancements seen in the appendiceal walls in our results are findings similar to the diffuse loss of mural perfusion that represents gangrenous appendicitis, which is a type of complicated appendicitis that is resistant to antibiotic therapy (7). Therefore, we believe that the inclusion of this CT finding as an exclusion criterion for antibiotic therapy may help to decrease treatment failure rates.
Quantification of the appendiceal wall enhancements was performed with reference to a previous study that measured small bowel wall enhancements using the maximal attenuation of ROI for the diagnosis of intestinal ischemia (20). Our results demonstrated that the failure group had lower HUpost and HUsub values than the success group. This result was concordant with the higher frequency of hypoenhancements of the appendiceal walls in the failure group.
Among 10 informative CT features for complicated appendicitis identified in a recent meta-analysis (18), 4 CT findings, including extraluminal appendicoliths, extraluminal air, abscesses, and ascites, are usually observed in advanced perforated appendicitis, and not in early perforated or nonperforated gangrenous appendicitis. We speculate that the remaining six CT findings, which were analyzed in our study, may be associated with nonperforated gangrenous appendicitis. However, there were no clinical differences between the success and failure groups in all six CT findings, including appendiceal wall enhancement defects, periappendiceal fat stranding, ileus, periappendiceal fluid collection, intraluminal air, and intraluminal appendicoliths.
The present study had several limitations; the first was its retrospective design. We retrospectively evaluated the CT images knowing that all the patients were diagnosed with appendicitis, which may have artificially elevated the diagnostic performance of the CT analyses, although we did not know which patients were successfully treated and which failed treatment. Second, our study included a small sample size and thus, we were unable to perform comparisons between the distinctive CT findings from the early treatment failure group after they received antibiotic therapy and the recurrent appendicitis group within 1 year. Considering that uncomplicated and complicated appendicitis may be two discrete entities with different pathophysiologies, the early failure group that did not show symptom improvements and the recurrent appendicitis group (after initial symptom improvements) may have different CT features. Therefore, further investigations will be needed to compare the CT findings between the two groups. Third, there were limitations in the quantification of the appendiceal wall attenuations on the CTs. Although we used an objective tool to evaluate the appendiceal wall enhancements, we subjectively chose only certain portions of the appendix, and not the entire appendix. Although the CT HU values used cannot reflect the full attenuation of the appendix walls, we believe that the values represented the presence or absence of focal ischemia in the appendix. These values allow this by measuring the parts of the appendix walls that show the lowest attenuations, based on visual assessments.
In conclusion, hypoenhancement of the appendiceal wall is associated with treatment failure after antibiotic therapy for acute nonperforated appendicitis. Adding this CT finding as an exclusion criterion may help to lower the failure rates after antibiotic therapy of patients with acute appendicitis. Further investigations evaluating the utility of CT parameters associated with treatment failure are warranted.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Supplementary Materials
The Data Supplement is available with this article at https://doi.org/10.3348/kjr.2019.0823.
Clinical Outcomes in Treatement Failure Group
Interobserver Agreement for CT Findings
References
- 1.Sartelli M, Viale P, Catena F, Ansaloni L, Moore E, Malangoni M, et al. 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2013;8:3. doi: 10.1186/1749-7922-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brügger L, Rosella L, Candinas D, Güller U. Improving outcomes after laparoscopic appendectomy: a population-based, 12-year trend analysis of 7446 patients. Ann Surg. 2011;253:309–313. doi: 10.1097/SLA.0b013e3181fc9d53. [DOI] [PubMed] [Google Scholar]
- 3.Kouhia ST, Heiskanen JT, Huttunen R, Ahtola HI, Kiviniemi VV, Hakala T. Long-term follow-up of a randomized clinical trial of open versus laparoscopic appendicectomy. Br J Surg. 2010;97:1395–1400. doi: 10.1002/bjs.7114. [DOI] [PubMed] [Google Scholar]
- 4.Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166–169. doi: 10.1002/bjs.1800820207. [DOI] [PubMed] [Google Scholar]
- 5.Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, et al. Appendectomy versus antibiotic treatment in acute appendicitis. A prospective multicenter randomized controlled trial. World J Surg. 2006;30:1033–1037. doi: 10.1007/s00268-005-0304-6. [DOI] [PubMed] [Google Scholar]
- 6.Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96:473–481. doi: 10.1002/bjs.6482. [DOI] [PubMed] [Google Scholar]
- 7.Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377:1573–1579. doi: 10.1016/S0140-6736(11)60410-8. [DOI] [PubMed] [Google Scholar]
- 8.Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313:2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 9.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147:818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156. doi: 10.1136/bmj.e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103:656–667. doi: 10.1002/bjs.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allievi N, Harbi A, Ceresoli M, Montori G, Poiasina E, Coccolini F, et al. Acute appendicitis: still a surgical disease? results from a propensity score-based outcome analysis of conservative versus surgical management from a prospective database. World J Surg. 2017;41:2697–2705. doi: 10.1007/s00268-017-4094-4. [DOI] [PubMed] [Google Scholar]
- 13.Hanson AL, Crosby RD, Basson MD. Patient preferences for surgery or antibiotics for the treatment of acute appendicitis. JAMA Surg. 2018;153:471–478. doi: 10.1001/jamasurg.2017.5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park HC, Kim MJ, Lee BH. The outcome of antibiotic therapy for uncomplicated appendicitis with diameters ≤ 10 mm. Int J Surg. 2014;12:897–900. doi: 10.1016/j.ijsu.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Park HC, Kim MJ, Lee BH. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg. 2017;104:1785–1790. doi: 10.1002/bjs.10660. [DOI] [PubMed] [Google Scholar]
- 16.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 17.Avanesov M, Wiese NJ, Karul M, Guerreiro H, Keller S, Busch P, et al. Diagnostic prediction of complicated appendicitis by combined clinical and radiological appendicitis severity index (APSI) Eur Radiol. 2018;28:3601–3610. doi: 10.1007/s00330-018-5339-9. [DOI] [PubMed] [Google Scholar]
- 18.Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology. 2018;287:104–115. doi: 10.1148/radiol.2017171260. [DOI] [PubMed] [Google Scholar]
- 19.Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 20.Jang KM, Min K, Kim MJ, Koh SH, Jeon EY, Kim IG, et al. Diagnostic performance of CT in the detection of intestinal ischemia associated with small-bowel obstruction using maximal attenuation of region of interest. AJR Am J Roentgenol. 2010;194:957–963. doi: 10.2214/AJR.09.2702. [DOI] [PubMed] [Google Scholar]
- 21.Horrow MM, White DS, Horrow JC. Differentiation of perforated from nonperforated appendicitis at CT. Radiology. 2003;227:46–51. doi: 10.1148/radiol.2272020223. [DOI] [PubMed] [Google Scholar]
- 22.Bixby SD, Lucey BC, Soto JA, Theysohn JM, Ozonoff A, Varghese JC. Perforated versus nonperforated acute appendicitis: accuracy of multidetector CT detection. Radiology. 2006;241:780–786. doi: 10.1148/radiol.2413051896. [DOI] [PubMed] [Google Scholar]
- 23.Tsuboi M, Takase K, Kaneda I, Ishibashi T, Yamada T, Kitami M, et al. Perforated and nonperforated appendicitis: defect in enhancing appendiceal wall--depiction with multi-detector row CT. Radiology. 2008;246:142–147. doi: 10.1148/radiol.2461051760. [DOI] [PubMed] [Google Scholar]
- 24.Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C. CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings. AJR Am J Roentgenol. 2005;185:406–417. doi: 10.2214/ajr.185.2.01850406. [DOI] [PubMed] [Google Scholar]
- 25.Antonopoulos P, Konstantinidis F, Dalamarinis K, Petroulakis A, Konstantinidou E, Karanikas I, et al. Acute gangrenous appendicitis-diagnosis by spiral CT. Ann Gastroenterol. 2006;19:72–76. [Google Scholar]
- 26.Elbanna KY, Mohammed MF, Chahal T, Khosa F, Ali IT, Berger FH, et al. Dual-energy CT in differentiating nonperforated gangrenous appendicitis from uncomplicated appendicitis. AJR Am J Roentgenol. 2018;211:776–782. doi: 10.2214/AJR.17.19274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Clinical Outcomes in Treatement Failure Group
Interobserver Agreement for CT Findings