Abstract
Medicinal leech therapy or Hirudino therapy have roots back in ancient civilization. It was a prevalent form of therapy in various ailments. The novel Ayurveda text Sushruta Samhita devoted a complete chapter on hirudino therapy. In the early 20th century this therapy had a major setback due to origin and evolution of antibiotics. There was a discontinuity in the flow of knowledge about this therapy. Then, resumed and revived after few recent decades, due to its contribution in reconstructive surgeries. During this period, the research work on various aspects have been conducted. The present paper summarizes the various aspects of medicinal leech therapy both from Ayurveda text and the present knowledge and to enable the fraternity to use the both source for benefits of humankind.
Keywords: Hirudino therapy, Jaloka Avacharana, Medical leech therapy
1. Introduction
In Ayurveda system of medicine Raktamokshana Karma (bloodletting) (RK) is considered as a regimental therapy. It is essential to adopt this procedure in autumn season for purification of body humors, which are otherwise deranged due to seasonal change. RK is also indicated in treatment of Raktaja Roga (diseases caused by or affecting the tissues of blood) [1]. The two types of RK are Pracchana Karma (scrapping or scarification) (PK) and Siravedha Karma (vein puncture) (SK) [2]. In both of these procedures sharp instruments are used and the amount of blood loss is relatively more in SK than the PK, which is a relative localized superficial therapy. There are alternative methods of RK for delicate patients. They are Jaloka Avacharana (medical leech therapy [MLT] or hirudotherapy) (JA), Kshringa Avacharana (wet cupping) and Alabu Avacharana (wet fire cupping). The most delicate method of RK is JA. It can be applied in RK, unless otherwise contraindicated [3]. The importance of JA can be assessed by the fact that the lord Dhanvantri (the god of Ayurveda) was carrying leeches at the time of his origin in the course of Ksheerasagaramantha (churning of Ocean of milk). Acharya Charaka has considered JA as a surgical procedure [4].
MLT was practiced in various ancient civilizations like Mesopotamians, the Greeks, the Mayans, and the Aztecs. The history of MLT is as old as 3500 years and a time line describing the history of leech therapy is summarized in Table 1. There was origin and evolution of antibiotics around 1930 [5], that greatly caused MLT to lose its importance. It was considered a primitive mode of treatment. In later half of 20th century, MLT revived due to its use in reconstruction surgeries. That was the era during which researches on various aspects of MLT were conducted. Various therapeutic indications were revalidated. In recent few decades, new disease entities are emerging, hence researches on MLT also discovered many new indications.
Table 1.
A time line for describing the history of leech therapy.
| Time | Historical Milestones |
|---|---|
| 3500 BC | Egypt, Mesopotamians, the Greeks, the Mayans, and the Aztecs used MLT for various aliments. |
| 1600-1300 BC | Have documented literature in Vedic writings. A mural painting showing the application of leeches has been retrieved inside a tomb in Thebes (Egypt) from the 18th dynasty. |
| 460-370 BC | Hippocrates of Cos, Greek Physician used to balance body humors. |
| 335-280 BC | Herophilos, Greek Physician used to balance body humors. |
| 138-185 BC | Nicander of Colophon (Greece) mentioned leech in the poem Alexipharmacia |
| 129–199 BC | Roman physician Galen described medicinal use |
| 123-50 BC | Themison of Laodicea was first to mentioned leech in Rome |
| 100–600 B.C. | Described in Ayurveda text Sushruta Samhita. |
| 100 BC. | Syrian physicians described medicinal use |
| 80-40 B.C. | In Greece, Themison, a pupil of Asclepiades described medicinal use. |
| 23 to 79 AD | Pliny the Elder in Rome, used MLT in treatment of phlebitis and hemorrhoids'. |
| 129–200 AD | Aelius Galenus, Roman Physician used it to balance body humor. |
| 1510–90 AD | Ambroise Par, recommended MLT where cupping-glasses could not be used, and in sites like on hemorrhoid veins, mouth of the womb, the gums, lips, nose, fingers etc. |
| Mid 1600's | Conrad Gessner of Zurich gave detail description on MLT |
| 1700 | Jerome Negrisoli used MLT in the field of gynaecology |
| 1772–1838 | Francois-Joseph-Victor Broussais, a surgeon in Napoleon's army advocated MLT |
| 1800 | Dealers in Europe started unfair practice to feed blood of unhealthy horses to leeches for financial gains and harmed MLT. |
| 1809 | Vitet authored “Treaty of Medical Leeches” |
| 1817 | Thomas Bell treated an oro antral fistula with facial swelling with MLT. |
| 1829–1836 | Parisian hospitals consumed 5–6 million leeches |
| 1830–1840 | Europe consumed 60 million leeches per year, and Russia consumed 30 million per year. |
| 1832 | St. Bartholomew's Hospital in London consumed 97,300 leeches for MLT |
| 1835 | American government offered a subsidy of 500 dollars for successful breeding of European leech. |
| 1838 | Richard Arnold, a Savannah physician, complained for high cost of MLT. |
| 1839 | Chapin A. Harris used MLT for drainage of gum in tooth abscess. |
| Mid 1800's | French imported about forty million leeches a year and England imported six million leeches a year. |
| 1840 | Benjamin Rush, (USA) advocated Leech therapy in Royal College of Physicians |
| 1850 | Leech breeding business collapsed in Europe due to surplus production. |
| 1884 | John Berry Haycroft, a Birmingham chemist discovered presence of an anticoagulant in leech saliva. |
| 1904 | Jacoby isolated hirudin from leech saliva and named it. |
| 1938 | Leeches removed from French pharmacopoeia |
| 1980 | Leeches used to relieve venous congestion in transplant surgery |
| 1987 | Hirudo medicinalis included in the International Union for Conservation of Nature Invertebrate Red Data Book and Appendix II of the Convention on International Trade in Endangered Species of Wild Fauna and Flora. |
| 1972 | MLT removed from French Social Security system. |
| 1983 | Henderson et al. reported use of MLT in the post-operative treatment of a scalp avulsion case |
| 1985 | Harvard physician Joseph used MLT for reattaching the ear of a five year- old boy. |
| June 28, 2004 | Food and Drug administration (FDA) approved Medicinal leech as a medical device. |
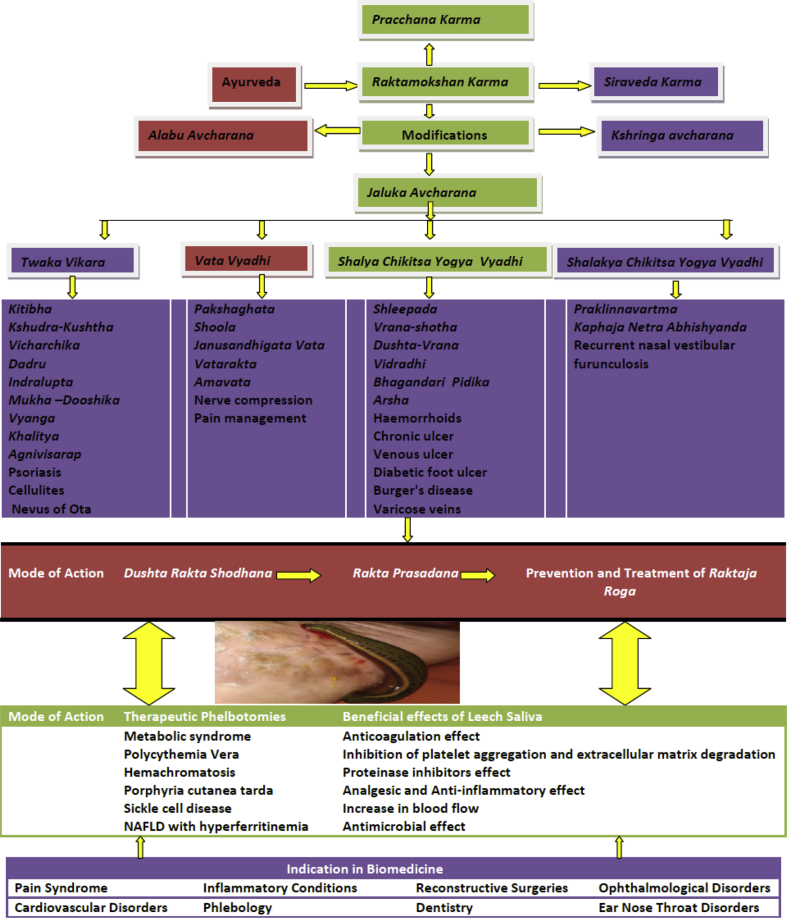
JA has been seen as an important therapeutic modality in various health conditions. A graphical representation of the therapeutic effects of JA on various areas was depicted in Fig. 1. A significant proportion work was conducted on the basis of Ayurveda principles on JA in various skin conditions like Kitibha (∼psoriasis), Kshudra-Kushtha (∼ skin diseases), Vicharchika (∼eczema), Dadru (∼ tinea infections), Indralupta (∼alopecia areata), Mukha -Dooshika or Tarunyapidika (∼acne), Mandal kustha (∼psoriasis), for pigment reduction in nevus of Ota, Vyanga (∼facial melanosis), Khalitya (∼alopecia), Agnivisarap (∼herpes zoster shingles), psoriasis and cellulites. The other diseases, in which the role of JA was explored were Shleepada (∼filariasis), Pakshaghata (∼hemiplegia), Amavata (∼rheumatoid arthritis), Vatarakta (∼metabolic disorders), pain management, Janusandhigata Vata (∼osteoarthritis of knee joints), shoola (∼pain), sciatic nerve compression, Vrana-shotha (∼initial stage of inflammation leading to abscess formation), Dushta-Vrana (∼chronic wound), Vidradhi (∼pyogenic abscess), chronic ulcer, venous ulcer, diabetic foot ulcer, Bhagandari Pidika (∼initial stage of inflammation leading to anorectal sepsis), haemorrhoids, Arsha (thrombosed piles), burger's disease, varicose veins, Praklinnavartma (blepharitis), Kaphaja Netra Abhishyanda (∼mucopurulent conjunctivitis) and recurrent nasal vestibular furunculosis. Research work on JA have been undertaken by various postgraduate Ayurvedic Institutes and the resultant observations were published in Pub Med indexed journals. A list of such research papers were enlisted in Table 2. A Supplementary file is attached providing a list of titles of Doctoral thesis conducted on Ayurvedic principles of JA. It was observed that most of work on JA was focused on limited areas and very few attempts were made beyond. There is a need for an extended study on JA. Hence the present paper is designed to provide a better understanding of JA from Ayurvedic literature and supplement its missing links from present day knowledge with supporting evidences generated from research works done over few decades in the field of MLT.
Fig. 1.
A Graphical representation of the therapeutic effects of JA on various areas.
Table 2.
List of articles indexed in PubMed on Ayurvedic MLT.
| Authors | Publication |
Title |
|---|---|---|
| Year | ||
| Bapat RD, Acharya BS, Juvekar S, Dahanukar SA. | 1998 | Leech therapy for complicated varicose veins. |
| Raval HN, Thakar AB | 2012 | Role of Raktamokshana by Jalaukavcharana and Siravedhana in the management of Vicharchika (Eczema) |
| Bhagat PJ, Raut SY, Lakhapati AM | 2012 | Clinical efficacy of Jalaukawacharana (leech application) in Thrombosed piles. |
| Rai PK, Singh AK, Singh OP, Rai NP, Dwivedi AK | 2011 | Efficacy of leech therapy in the management of osteoarthritis (Sandhivata). |
| Sharma MR, Mehta CS, Shukla DJ, Patel KB, Patel MV, Gupta SN. | 2013 | Multimodal Ayurvedic management for Sandhigatavata (Osteoarthritis of knee joints). |
| Kadu AS, Rajput DS, Deshmukh SG | 2017 | Management of Recurrent Nasal Vestibular Furunculosis by Jalaukāvacaraṇa and Palliative Treatment. |
| Shankar KMP, Rao SD, Umar SN, Gopalakrishnaiah V. | 2014 | A clinical trial for evaluation of leech application in the management of Vicarcika (Eczema). |
| Rastogi S, Chaudhari P. | 2014 | Pigment reduction in nevus of Ota following leech therapy. |
| Sathish HS, Vaghela DB | 2011 | Bloodletting – An Ayurvedic perspective |
An on-line search of five databases including the Pub med, Cochrane Library, Scopus, Ebscohost and Dhara databases was conducted. The classical Ayurveda texts were scrutinized and information pertaining to JA had been compiled meticulously. This classical data along with the various aspects of leeches and MLT of present knowledge from research papers retrieved from databases was summarized and presented to develop a better understanding of the concept of JA and help to fill in the gaps of knowledge due to unavailability of complete ancient Ayurveda text. For this purpose, 130 potential articles were identified, 90 abstracts were screened and 69 full text articles were assessed for eligibility and 38 original articles were included in this review.
2. Jaloka in Ayurveda
In Ayurveda text the Jaloka (leeches) has been classified in two major varieties based on their therapeutic role, the Savisha (unfit for therapeutic purposes) and Nirvisha (fit for therapeutic purposes). These were further sub-classified into six types each. These twelve types of Jaloka were named according to their distinct properties. The Nirvisha Jalokas are Kapila, Pingala, Sankumukhi, Mushika, Pundarikamukhi and Savarika. The other six types of Savisha Jaloka which should be avoided are Krishna, Karbura, Algarda, Indrayudha, Samudrika and Gochandana. Jaloka on the basis of their breeding grounds were also determined as Savisha and Nirvisha. The water body having lots of contaminations were the breeding ground of Savisha Jaloka, whereas the fresh water bodies were the breeding ground of Nirvisha Jaloka. The various toxic symptoms that developed due to therapeutic use or accidental bite of Savisha Jaloka were Svayathu (inflammation), Atimatra Kandu (excessive itching), Murcha (unconsciousness), Jwara (febrile state), Daha (burning sensation), Chardi (vomiting), Mada (confusion) and Sadana (lethargy). The line of treatment in such condition was also prescribed. They were treated as a case of Visha (poisoning), Pitta (disorders due to deranged pitta) and Rakta (disorders due to deranged blood tissue) [6]. The other criteria of being unfit for therapeutic purposes were on the basis of the appearance and activity status of Jaloka. The Jaloka for therapeutic purposes were collected from fresh water ponds using piece of wet leather or fresh meat. The site of fresh water was specifically determined by stating that these sites should have water lilies rooted in the soil beds. The collected Jaloka were preserved in a wide and new earthen pot with clean water. Aquatic plants parts and dried meat powder of mammals living in marshy lands like pig were added to provide feeding of these Jaloka. Water and feed of the pot were replaced on every third day and the pot was replaced on every seventh day [7].
3. Leeches in biomedicine
Globally there are more than 700 leech species out of which the most frequently used species for therapeutic purposes were Hirudo medicinalis, Hirudo verbena, Macrobdella decora, Haementeria officinalis, Hirudinaria manillensis, Hirudotroctina, Hirudo quinquestriata, Hirudo nipponia, Poecilobdella granulose and Hirudinaria javanica [8]. The medicinal leech (H. medicinalis) was certified by Food and drug Administration (FDA) on June 21, 2004 as a medical device. These leeches are slightly flattened, cylindrical and segmented (33–34 segments) annelids belonging to phylum Annelida, class Clitellata and subclass Hirudinea (Lamark, 1818) [9]. Leech is a fresh water animal, live in eutrophic water bodies. The temperature suitable for survival of leeches range between 0 °C to 30 °C, like other water being leeches were also sensitive to rapid changes in temperature. For therapeutic purpose in leech farming, it is recommended by FDA that the animal must be maintained without feeding at a temperature range of 4 °C −13 °C and water volume area per animal should not be less than 0.7 L, with typically 10–15 leeches being held in a large jar. Leeches take up oxygen dissolved in water. All type of contaminants cause stress to the leeches causing secretion of mucous layer over their body [10]. Leeches are hermaphrodite; still there is a need of a partner for reproduction. Reciprocal fertilization leads to reproduction in leeches. Young leeches are produced in three to five weeks from the eggs stored in cocoons. These young leeches feed on the blood of frogs and fishes [11]. At the age of two years these leeches are fully matured to be used for therapeutic purposes. Leeches have a pair of suckers, anterior sucker and posterior sucker. Anterior sucker is oral sucker consisting of the jaw and teeth; it is used for connecting to host for feeding. Through this sucker leeches secretes its salivary secretion which is anesthetic, which makes the host insensitive to its bite. This leech saliva (LS) contains more than 100 bio active substances. These are responsible for various therapeutic benefits like anticoagulant, anti-inflammatory, anesthetic, thrombolytic, vasodilator, and anti-edematous, bacteriostatic and blood- and lymph-circulation enhancing properties. The digestive tracts of a leech consist of three major parts. The first part is the pharynx which is an extension of the oral region and it lies adjacent to the salivary glands. The second part is the crop which is the storage organ for the ingested blood. The watery content of the meal is removed through pairs of bladders thus leaving a high viscous intraluminal fluid in the crop region. The crop region along with the third part of the tract intestinum region is colonized by symbiotic partners such as Aeromonas hydrophila and Pseudomonas hirudinia. These partners assist in the complex digestion of the ingested erythrocytes meals over several weeks. The symbiotic partners have capability of anaerobic metabolism. They digest the complex meals into simplest metabolic end products which assist in nourishment of their own and the host body. The erythrocytes of the blood are digested by two mechanisms, the haemolysis and proteolysis. The hemoglobin of the erythrocytes is disintegrated into globins and haem parts, the globins part is utilized by the leech's metabolism and the haem part is excreted as iron and protoporphyrin. The scar left by the leech bites resembles the mercedes-benz emblem. The posterior sucker is used mainly for leverage purposes. The successive attachment and detachment of these suckers help in movement of leeches. For medicinal purpose leeches breed in certified bio farms are used. These leeches are stored in a sterile container with non-chlorinated water. The water of the containers is routinely changed every day or on alternate day depending on the presence of turbidity in the containers. The number of leeches should not be more than fifty for a container of ten liters capacity. These containers are placed in cold dark placed with temperature not exceeding 4 °C. These containers can be placed in refrigerator also but it should be ensured that the leeches should be maintained at normal room temperature several hours before their use in a therapeutic session. This will help leeches in regaining their activity and motility.
4. JA in Ayurvedic treatment
For JA a thick paste of mustard seed and turmeric was applied on Jaloka. Then Jaloka was suspended in solution of turmeric for a Muhurta (approximately 45 min) till they regained their motility. This Jaloka was applied on roughened desired spot for JA. If the Jaloka was unable to stick on the desired spot, then drop of milk or blood was applied on the affected part or slight incision was made into the lesion. After all efforts, if Jaloka does not attach itself at the desired spot, it was replaced with other fresh Jaloka. On attachment to the affected part from the suckers, Jaloka assumes Aswakhuravata Ananam, Unnabhya Va Skandham (the shape of a horse shoe in the raised and arched position). At this moment Jaloka was covered with a piece of thin and wet linen or with a piece of white cotton and drops of cool water were frequently dropped on the covering part to provide cooling effect. The Jaloka detaches after completing its feed. Then efforts were made to regurgitate the ingested blood [12]. Subsiding of pain and disease were the signs of proper JA. The treatment adopted in this case was application of Shatdhautam Ghritam (prepared by washing of ghee with cold water by 100 times) on the lesion. In case of insufficient bleeding honey was rubbed on the lesion. If there was profuse bleeding then for arresting the blood flow, cold water was sprinkled on the lesion [13].
5. MLT in biomedicine
For using these creatures in MLT, the number required for the purpose should be decided. Although there are no general guidelines for this, but it could be decided by taking into consideration the extent of area and the amount of blood needed to draw from the site. To treat a flap of finger one or two leeches are more than sufficient but larger areas may require six to eight leeches. On an average it is estimated that one leech can draw up to 50 ml of blood during and post MLT session. Thus, this can give a rough idea of the number of leeches employed to draw a desired amount of blood. In MLT, a suitable leech is selected, the rule in this regard is the hungriest (which is generally the smallest) is selected. The creature was rinsed twice with distilled water and placed in a sterile container filled with distilled water to ensure minimization of bacterial growth on the body surface of the leech. This should be done at least 4 h prior to its use in MLT. The site of attachment of patient's body was thoroughly washed with soap and water followed by rinsing with plain water. A barrier of dampen gauze with a hole, which exposes the site of attachment was placed on the site. This was an attempt to limit the leech movements around the desired site. The head part of leech was determined by its movements, the tail part was majorly used as an organ of fixation. The head end of the leech was steered in the hole of the gauze barrier. This facilitates the attachment of the leech to the desired site. If the leech was not able to attach then, as a last alternative a small needle pick on the skin could be done. The tiny blood droplet attracts the leech to attach on the site. If still leech refuses to attach then the leech should be replaced. On attachment the leech draws blood from the lesion till it is fully satisfied, that varies from 30 to 60 min and then drop itself after completing its feed. The used leech was then killed by immersing it in 70 percent alcohol solution for five to 10 min and disposed it off as biohazard material. The site of attachment post MLT is routinely observed and if there was abnormal persistent bleeding, then hemoglobin levels could be assessed as a precautionary measure.
6. Indications of JA in Ayurveda
In Ayurveda JA are indicated in delicate persons like weak patients, female patients, too aged or too young patients suffering from Rakta-Pradoshaj vikaras [diseases originated in Rakta Dhatu (∼blood)]. The Rakta-P. vikaras are Mukhapaka (erosion in oral cavity), Akshiraga (redness in eyes), Puti Nasa (Smelly secretion from nose or foul smell sensation), Asyagandhata (smelling mouth or smelly secretion from mouth), Gulma (inflammatory condition of abdomen), Upkusha (Bleeding gums), Visarpa (inflammatory skin disorders), Raktapitta (hemorrhagic disorders), Prameelaka (fatigue), Vidradhi (abscess), Raktameha (blood discharge with urine), Pradara (vaginal discharge), Vatashonita (gout), Vaivarnya (discoloration of skin), Agnisada (loss of appetite), Pipasa (excessive thirst), Gurugatrata (heaviness in body), Santapa (febrile condition), Atidurbala (excessive weakness), Tikta Amla Udgara (belching with bitter & acidic taste), Klama (unexplained fatigue), Krodha Prachurya (excessive explained anger), Buddhi Sammoha (confusion), Lavan Asyata (unreasonable excessive salty taste perception), Sweda Sharir Durgandhya (excessive sweating with or without foul odor), Mada (unreasonable compulsive behavior disorders), Kampa (tremors like pathological condition), Swara Kshaya (vocal intensity decreased), Tandra (unexplained mental fatigue), Nidra Atiyoga (excessive sleepiness), Tamaas Atidarshana (unexplained frequent blackouts), Kandu (itching), Twaka Vikara like Aru, Kotha, Pidika, Kustha, Charmadala etc (skin disorders) [14]. Specific indications of JA were also provided. It is indicated in Gulma (∼various gastrointestinal diseases) Arsha, Vidradhi, Kustha (various skin diseases) Vatrakta, Galamaya (diseases of throat region), Netra ruka (eye pain, various diseases of eye) Visha (poisoning and other similar condition) etc [15].
Ayurvedic research work conducted in field of JA under various disease conditions were summarized below:
6.1. JA in Vicharchika
A clinical study was carried out on 29 clinically diagnosed cases of Vicharchika. Among them, 14 patients were subjected to JA for four sittings in four consecutive weeks. Number of leeches applied was decided on the basis of the size of lesion (1 cm = 1 leech). The other group of 15 patients was subjected to Siravedha Karma (venesection at the median cubital vein) for two sitting (once in a fortnight). In each sitting on an average 63.75 ml blood was removed depending upon the Anjali Pramana (amount of liquid collected by joining both the palms) of the patient. In this study it was observed that JA had proved more effective than Siravedha Karma in managing the disease [16].
6.2. JA in Indralupta
An interesting case study of a male patient suffering from Indralupta was undertaken. He was subjected to JA twice a week along with daily application of Gunjabeeja (paste of seeds of Abrus precatorius) on bald spot. It was observed that this treatment was effective in regaining the growth of hairs in affected area [17].
6.3. JA in Puyalasa (Acute Dacryocystitis)
A clinical study was conducted on the clinically diagnosed case of Puyalasa (Acute Dacryocystitis) it was observed that JA along with oral drugs proved beneficial in management of the disease [18].
6.4. JA in Shleepada
A pilot study was carried out on 13 diagnosed cases of Shleepada. These cases were subjected to JA for six weeks and most of the patients had significant relief in sign and symptoms [19].
6.5. JA in case of nevus of Ota
A study was conducted on a case of nevus of Ota. She was subjected to JA for five sessions in a span of two months. It was observed that there was substantial reduction in pigmentation [20].
6.6. JA in scalp psoriasis
A single case study was conducted on a patient suffering from scalp psoriasis. The patient was subjected to JA for three settings, with a gap of 2 days in between the sitting. In each sitting four leeches were used. After a period of seven days a significant improvement was noticed [21].
6.7. JA in externo – internal thrombosed hemorrhoids
A study on thirteen patients suffering from externo - internal thrombosed hemorrhoids was conducted. It was observed that JA provided analgesic, thrombolytic, antimicrobial and mucolytic effects on the patients [22].
6.8. JA in periapical abscess
A case study of a female patient suffering from periapical abscess due to dental carries was carried out with JA alone for five sittings and it was observed that JA alone can be used for curing this type of condition [23].
6.9. JA in Sandhigatavata
A multimodal Ayurveda treatment study was carried on fifty patients of Sandhigatavata. Among these 31 patients were subjected to JA once at 11th day in a 45 days regime and if required it was repeated on 15th day also. The other treatment modalities were Snehana, Svedana, Mriduvirechana and Matrabasti along with certain Ayurvedic oral Preparations. In this study substantial relief was observed in the patients [24].
7. Indications of MLT in biomedicine
The MLT was indicated in varieties of diseased conditions. These conditions are elaborated in modern biomedicine by various research works and were described below:
7.1. MLT in pain syndrome
MLT have beneficial effect on regional pain syndrome and reported to have analgesic activity in Osteoarthritis. A randomized controlled trail was conducted on patients of Osteoarthritis of the knee joint using single sitting of eight leeches in MLT and transcutaneous electrical nerve stimulation as comparator. It was observed that MLT showed significant and sustaining effect on pain relief as compared to the other group [25]. Studies have suggested that MLT was beneficial in disorders like osteoarthritis (ankle, hip, shoulder, small joint), sports injuries, iliosacral joint pain, chronic low back pain, cervico brachialgia, cervical spine syndrome and cancer pain [26].
7.2. MLT in inflammatory conditions
MLT have beneficial effect as adjuvant therapy on inflammatory conditions like abscesses, hypersensitivity conditions, rheumatic disease (rheumatoid arthritis, fibromyalgia and myasthenia gravis), gout, arthritis, systemic lupus erythematosus, paronychia, tendinitis, tendovaginitis, sialadenitis and inflammatory diseases of internal organs [27].
7.3. MLT in reconstructive surgeries
MLT has been extensively used in reconstructive surgeries for more than five decades. Specially in some surgeries of small area like glans penis, breast flap (cosmetic breast reduction mammoplasty), digits replants, ears, nasal tips, lips, maxofacial region etc. These sites have least possibility of venous anastomosis. At times this fact creates the condition of venous congestion in free flaps. There were evidences that MLT is beneficial in such cases. It has been seen as the only alternative in cases, where revision surgery cannot be adopted or failed. It has been estimated that the success rate of MLT for flap vascularization ranges from 65 to 85 percent according to cases encountered. The MLT were adopted on cases with the age range of 2–81yrs and the ratio of male to female is 2:1 [28] Average duration needed for the various cases varied approximately between two to 8 h. The average days needed for the various cases approximately ranged between four to ten days. The number of leeches required was dependent on the volume of the flap requiring improved vascularization. While considering use of MLT in such surgeries two important points have to be considered; the first one was continuous monitoring of hematocrit, that should be more than thirty percent in such cases. It had been reported that 50 percent of such cases required transfusion. The second important factor was the prophylaxis against Aeromonas spp. strains infection. For this it was advisable to administer a combination of ciprofloxacin and trimethoprim-sulfametoxazole as prophylactic antibiotic therapy.
7.4. MLT in phlebology and cardiovascular disorders
MLT had proved benefits in disorders of cardiovascular origin like acute, subacute, chronic thrombophlebitis and post-phlebitis syndrome, deep vein thrombosis, arterial hypertension, spider naevi, frostbite, varicose veins, hemorrhoids, hematoma (massive scrotal hematoma) [29] chronic venous insufficiency, priapism [30], ocular circulation disorders, peripheral circulation disorders, acute myocardial infarction and myocardial ischemia. A case study was conducted on a patient suffering from macroglossia caused by hematoma after placement of dental implants. She was subjected to MLT for three sessions daily and it was observed that this aliment could be successfully managed [31].
7.5. MLT in dentistry
MLT had proved beneficial in the field of dentistry. Studies had proved that it was useful in case of oroantral fistula, in drainage of abscess from gums [32] in root canal treatment, oral pemphigus and periodontitis.
7.6. MLT in Ophthalmological and ear nose throat (ENT) disorders
MLT had proved beneficial in ENT disorders like tinnitus, periorbital haematomas, glaucoma, laryngitis acute rhino pharyngitis [33], parotitis, acute and chronic otitis.
7.7. MLT in others arena
MLT had proved beneficial in a varieties of arenas like diseases of dermatological origin, diabetes and complications of diabetes mellitus [34], obesity, gastrointestinal disorders, neurology (epilepsy), gynecology (female sterility and ovarian cysts) [9], herpes zoster, male sterility, prostate diseases and asthma.
8. Contraindications
8.1. Contradiction of JA in Ayurveda
In Ayurveda text there was no direct description of contraindications of JA. But the contraindication of RK can be considered as contraindications of JA. RK was contraindicated in patients with Sarvanga Sotha (individual with generalized edema), Ksheenacha Amla Bhojana Nimitta (individuals emaciated due to intake of sour food articles), Pandu Rogi (Anemic Patient), Arsha Rogi (individual suffering hemorrhoids), Udar Rogi (individual with inflammatory disorders of abdomen organs), Shosha Rogi (individual suffering from disorders causing cachexia), Garbhini (pregnant ladies)and Svayathu (individual suffering from inflammatory disorders) [35]. Certain conditions were also mentioned in Ayurveda text when the RK should not be administered in indicated patients they are – Duradina (days with rainfall), Sheetavata (breezy day or place), Aswina (without administration of proper swedana) and Bhukta Matre (after intake of complete meals or immediately after meals) [36]. In Ayurveda text immediate status of patients were also mentioned when the RK can not administered in indicated patients they were - Mada (delirium), Murcha (unconscious patient), Shrama Artanama (physically exhausted patient), Vata – Vina- Mutra Sangi (patient with holding the urges of flatus, feces & urine), Nidraabhibhota (in sleeping state) and Bheeta (in fearful individual) [37].
8.2. Contraindication of MLT in biomedicine
The various conditions in which MLT is contraindicated are hemorrhagic diathesis, absolute hemophilia, known protein allergies, anticoagulant therapy, leukemia, hypotonia, bone narrow suppression, chronic gastrointestinal disorders, dialysis, cirrhosis, in tendency to keloid scar formation, pregnancy, chemotherapy, radiotherapy, cachexis in infants, serious organic disease and immunosuppressive conditions [25].
9. Complications
9.1. JA in Ayurveda
In Ayurveda text complication of JA was not directly mentioned but complication of RK was mentioned. If RK was applied in described contraindicated states, it caused Shopha (edema), Daha (burning sensation), Raga (redness), Paka (inflammation) and Vedana (pain) [38].
9.2. MLT in biomedicine
The most important complication encountered in MLT were surgical site infection caused due to Aeromonas spp. strains. Studies havereported that this strain was susceptible to fluoroquinolones, sulfamethoxazole or trimethoprim, aminosides, levofloxacin and third-generation cephalosporins. Amoxicillin, clavulanic acid and second-generation cephalosporins had failed to arrest the postoperative complications caused due to these strains [39]. A rare complication was reported after MLT when leech tunneled beneath the flap in a reconstructive surgery. To locate the leech duplex ultrasound was used followed by removal of leech through a minimal access incision [40]. Surrounding flap area with petroleum jelly or occlusive dressings was a measure developed to prevent leeches from moving from the desired site [41]. In few cases local allergic reaction was reported in patients due to some content of LS. At times patients were not willing to adopt this treatment due to presence of blood-sucking ectoparasites as a major aspect of this therapy. The solution for this issue was resolved by adopting psychological precounseling before MLT. Another complication of MLT was prolonged bleeding followed by MLT. In such condition attempts were made to arrest bleeding and as a last resort primary suturing was adopted [42]. Other complications which rarely occurred due to MLT were anaphylaxis, anemia, and mucosal synechiae. Strict contraindication of MLT in patients on aspirin therapy was also reported.
10. Precautions
10.1. JA in Ayurveda
In JA Sthoula Madhya (thick in medial part), Pariklishta (ugly), Prithu (flattened), Manda Vichesta (have reduced activity), Agrahi (non grasping), Alpapayi (least blood sucking), Savisha (poisonous leeches) [43], Asamyaka Vamanata (those leeches in which improper vomiting of ingested blood is been done), Pratantama (tired leeches after blood ingestion) and Nipatanata (those leeches who are immotile after blood sucking or by getting used for long time) Jalokas were avoided [44].
10.2. MLT in biomedicine
Since in the therapy blood, body fluid, open wound and animals are involved there are chances of transfer of infections at various levels like from the organism itself, though their symbiotic partners A. hydrophila and Ppseudomonas hirudinia, from the pre-ingested and regurgitated meals in the fresh wound like sepsis, septic shock, HIV, hepatitis C, Dengue fever, Methicillin-resistant Staphylococcus aureus (MRSA or Super Bug). Therefore, it becomes necessary that certain precautions are to be undertaken in the process to minimize these transmissions. The leeches used in MLT are breed in certified biofarm and maintained in a sterile environment for culture, transportation and storage which reduces the chances of interaction of harmful microbial flora and the annelids. A weekly sampling of water from leech tank is done for culture and antibiotic susceptibility test to determine appropriate prophylactic antibiotic regimen provided prior to the therapy thus developing a shield against infections. The leeches prior to the therapy are rinse and suspended in the sterile water for at least 4 h prior to use, to ensure minimization of infection through body surface of leech. It is ensured that leeches selected for the process are kept on fasting for at least six months prior therapy and most probably the last meal is the sterile bovine blood in the biofarm. The chances of cross transfer of blood borne infection can be reduced by sacrificing the animal after single use or limiting it to a single subject. These measures ensure least chances of microbial infection transmission though leeches [45]. Prior to the therapy the patients is examined thoroughly and particularly for blood born infections and contraindications, then the treatment are appropriately planned. A precaution at the time of therapy is undertaken of maintaining the mammalian range skin temperature on which leech is to be attached and the site should be clean because leeches are repelled by perfumed and greasy skin [46].
11. Probable mode of action
11.1. JA
The probable mode of action of JA as per Ayurveda text suggests that it was due to its capacity of removing Rakta Dhatu along with vitiated Doshas. Although there are three Sharira Doshas but at times Rakta is also considered as fourth Dosha, since the Rakta Dhatu is the prime carrier of vitiate Pitta in whole of the body. This suggests that the vitiated Pitta Dhatu may be the loads of metabolic waste that is carried along with this circulatory fluid. When this Rakta Dhatu is expelled from the body it carries the vitiated Pitta with itself and thus purifying the body by removal and further decreasing its quantum by compensatory production of healthy Rakta Dhatu, caused due to blood loss. It also states that the properly administered RK causes Prasada Manas (normalization of physiology of the Manas or whole body with senses) and it prevents development of Raktaja Rogas like Twaka Dosha (skin disorders), Granthi (abnormal outgrowth) and Shopha (inflammation) [47]. From the above description it can be interpreted that there are certain specific conditions like Polycythemia Vera, malignant tumors, Hepatocellular Carcinoma, acquired cystic kidney disease, hemochromatosis, porphyria cutanea tarda, sickle cell disease and nonalcoholic fatty liver disease (NAFLD) with hyperferritinemia etc. which can be considered Raktaja Roga and are prevented on maintaining a low hematocrit. An important concept of Ayurveda that further glorifies the importance of RK is that, if a disease condition was not been cured by adopting Sheeta (therapies causing decrease in metabolic activities by decreasing core temperature), Ushana (therapies promoting metabolic activities by increasing core temperature), Snigdha (therapies enhancing the metabolic activities by reducing resistance or Vata Shamana), Rukshana (therapies decreasing the metabolic activities by enhancing resistance or Vata Prakopa) treatments then it is a Raktaja Roga and under these circumstances treatment for Raktaja Roga should be adopted and among them prime is RK [48] While describing the symptoms of Suddha Rakta Purusha (individual with purified Rakta dhatu after RK) it is stated that he is Prasanna Varna (have clear complexion, denotes the correction in metabolism of pigments or more precisely of correcting dysmetabolic iron overload syndrome (DIOS) in cases of NAFLD and the metabolic syndrome), Indriya-Indriyaarthnichantama (have proper sensory perception at macro and micro level. The micro level Indriya can be considered the receptors sites for enzymes and hormones etc., since the ferritin and body iron stores at increased levels affects the insulin resistance (IR) and at times causes metabolic abnormalities in metabolic syndrome, thus on reducing their levels through RK will favor the health status in above said conditions), Avyathapakti (correction in metabolism at all levels, this again supports the above said fact), Vegama Sukhanvintam (have normal physiological functions like movements of metabolites or proper progression of metabolic process, defecation, urination etc., natural urges properly removed or completion of metabolic processes as whole and more precisely the catabolic activities) and Pushti Bala Uttpana (have proper nourishment andstrengthened body denotes the correction of anabolic activities of the body) [49]. Specifically for JA, it was mentioned that it was the most suitable for Pitta Dushta Rakta RK and the reason for its clarification was given as this Annelids lives in cold water & have Madhura (anabolism promoting) properties, that pacifies Pitta. Specific indication of JA was in the presence of Grathita or Avagada Rakta Dhatu (thickened or coagulated blood). The above description suggest about the specific properties of Leech that causes removal of Rakta Dhatu, that has its affinity towards the erythrocytes components of the blood, and its capacity of promoting blood loss through anticoagulation effect, inhibition of platelet aggregation and extracellular matrix degradation. It was also described that in ‘Aatyayika Gadata’ (an emergency condition in reference of disease state) and in otherwise contraindications of Siravedha, JA was to be done [50] and it was the most appropriate method of RK in Nripa (delicate individuals), Bala (children), Sthavira (aged), Bhiru (fearful), Durbala (weak), Nari (females) and Sukumara (similar delicate individual) since it was the ‘Parama Sukumara’ (the extreme delicate) way of RK [51]. These descriptions suggest the analgesic, antiinflammatory effects and antimicrobial action of JA that makes the process least troublesome for delicate individuals and conditions. The mode of action of JA was summarized by stating that it draws only impure blood just like the swan can drinks milk and leaves water from a mixture of milk and water [52] This signifies the removal of erythrocytes components of the blood which may be the prime source of Raktaja Roga.
11.2. MLT
The probable mode of action of MLT is dependent on two factors; Primarily the amount of blood that is removed in the therapy by suction action of leech which is approximately 5–15 ml blood and on an average 50–150 ml of blood that oozes up to 10–48 h post MLT session. The cause of oozing of blood was due to LS which are poured in the wound site during the MLT sessions. The second factor that is responsible for the therapeutic action of MLT was the content of LS that are poured in host body. Interestingly leeches do not have a proper salivary gland but there are salivary cells with cell bodies located in pharyngeal region which pours their secretion individually through excretory ducts which have their openings between the teeth lets on the dental ridges of the jaws. The LS contains several bioactive components that attributes to its therapeutic uses in wide range of disease conditions. Both of the therapeutic benefits producing effects were summarized below.
11.2.1. Beneficial effects of therapeutic phlebotomies (TP)
11.2.1.1. Metabolic syndrome (MS)
MS is a group of cardiovascular disease risk factors like visceral obesity, hypertension, dyslipidemia, hyperglycemia, insulin resistance, glucose intolerance and fatty liver disease. A randomized controlled single blinded study was conducted on 64 hypertensive patients among them, thirty-seven percent patients were suffering from type II diabetes mellitus. Thirty-three patients were subjected to TP and thirty-one patients were assigned to controlled group. In the TP group 300 mL’ (mL) of blood was remove at entry level followed by repeated TP ranging between 250 mL to 500 mL of blood depending upon the ferritin level assessed at entry level. After six weeks, it was observed that there was reduction in body iron store, lowering of blood pressure and improvements in markers of cardiovascular risk and glycemic control [53].
11.2.1.2. Polycythemia Vera (PV)
PV is a condition in which there is an increased production of erythrocytes and at times there is an increase in white blood cells and platelets production also. In PV, through TP the blood viscosity is reduced resulting in reduction of risk for thrombotic events like hematomas, solid tumors, arterial or venous thromboembolism, cerebrovascular disease and cardiovascular disease [54].
11.2.1.3. Hemachromatosis
Hemachromatosis is a metabolic condition in which there is excess of iron load in the body. If the cause of this condition is genetic, it is termed as hereditary hemochromatosis. It results in increased, inappropriate absorption of dietary iron leading to liver cirrhosis, hepatocellular carcinoma, pancreatic disease, joint disease, pituitary disease, diabetes and heart disease. There are secondary causes of iron overloads also. This could be due to iron load anemias like thalassemia major, chronic hemolytic anemia, pyruvate sideroblastic anemia, aplastic anemia, pyridoxine-responsive kinase deficiency anemia. An another cause of iron load could be excessive supplementation of iron through long term hemodialysis, iron–dextran injections and red blood cell transfusions. Chronic liver disease can also result in hemachromatosis. In such conditions, TP is a prime treatment. One unit of blood is removed once or twice a week depending upon the tolerability and hemoglobin concentration of the patient's body till there is considerable reduction in iron stores [55].
11.2.1.4. Porphyria cutanea tarda (PCT)
PCT is a metabolic condition in which there are low levels of uroporphyrinogen decarboxylase enzymes responsible for heme (component of hemoglobin) production. It could be due to genetic causes or due to secondary factors like infection with the hepatitis c virus, alcohol abuse, excess iron intake, estrogen excess and exposure to chlorinated cyclic hydrocarbons and agent Orange. In this condition TP (till there is slight anemia and sign of iron deficiency) have proved as an additive therapy by reducing the excessive iron which provides a benefit of limiting heme synthesis [56].
11.2.1.5. Sickle cell disease (SCD)
SCD is a group of genetic diseases having abnormality in production of hemoglobin present in red blood cells. TP have known to lower the blood viscosity, hematocrit and induce iron deficiency resulting in decrease in vaso-occlusive pain episodes and thromboembolic complication. In SCD, TP was administered weekly until a hemoglobin target of 9.5 g per deci liter (gm/dL) has not reached. Then TP was repeated to maintain hemoglobin between 9.5 and 10.5 gm/dL with a monthly monitoring schedule [57].
11.2.1.6. NAFLD with hyperferritinemia
NAFLD is an abnormal lipid-deposition in hepatocytes, it was not caused due to excessive alcohol intake but associated with MS. NAFLD may develop in liver fibrosis, cirrhosis and hepatocellular carcinoma. In NAFLD patients, if there is increase in hepatic iron deposition and elevated serum ferritin levels then it is termed as NAFLD with hyperferritinemia that often leads to hepatocellular carcinoma. In such cases TP (removal of 350 mL of blood every ten to fifteen days) had improved the liver damage after a span of two years. There were improvements in enzymes of liver also [58].
11.2.2. Beneficial effects of LS
11.2.2.1. Anticoagulation effect
One of the important actions of the LS is the anticoagulation effect. The anticoagulant effect is majorly contributed by hirudin protein, gelin, eglins C, factor Xa inhibitor, destabilase complex, new leech protein-1, whitide, and whitmanin 29. The hirudin protein of the LS is known to have thrombin inhibition by binding itself with the thrombin of the vertebrate blood and thus inhibits fibrin production resulting in prevention of coagulation of blood. This compound is functionally similar to heparin. It is identified molecularly, synthesized though recombinant techniques using yeast, bacteria and higher eukaryotes. It used as thrombosis prophylaxis, particularly very useful in patients with hypersensitivity for heparin. The use of hirudin protein is extended in patients with antithrombin III deficiency [59] Gelin and eglins C are similar thrombin inhibitor present in LS. They are anti-inflammatory and known to have effect on inhibiting the activity of α-chymotrypsin, chymase, subtilisin, elastase, and cathepsin G. They have major therapeutic role in diseases associated with inflammation. Eglin is also known to have proteinase inhibitors action [60]. In addition to these above compounds of LS, the factor Xa inhibitor have as pronounced action as an anticoagulant. Destabilase complex is another compound of LS, basically it is an invertebrate lysozyme developed as a resultant of symbiotic relationship between the leech and A. hydrophila bacteria. It possesses both enzymatic and non-enzymatic antibacterial action and it also assist in dissolving blood clots. This property of destabilase complex is useful in thrombophlebitis [61]. There are few newly identified proteins which assist in anticoagulant effect they are new leech protein-1, whitide, and whitmanin - 29.
11.2.2.2. Inhibition of platelet aggregation and extracellular matrix degradation
An important effect of salivary secretion was the inhibition of platelet aggregation, that was attributed by calin, saratin, apyrase, decorsin and collagenase. The factor that was responsible for prolonged bleeding post MLT was the calin compound present in LS. The calin compound suppresses the collagen induced platelet aggregation. It blocks the binding of von willebrand factor to collagen thus results in prevention of adhesion between platelets and collagen. Saratin is a protein which affects reaction between collagen and von willebrand factor and hampers the initial steps of platelets adhesions [62]. Sartin and apyrase hydrolyze adenosine triphosphate and adenosine diphosphate into adenosine monophosphate which does not bind to purinergic receptors, resulting in hampering of platelet aggregation by inhibiting receptor mechanisms. Decorsin is a proteineacous compound which act as an antagonist of platelet glycoproteins and resulting in disturbing the mechanism of platelets aggregation [63]. Collagenase is an enzyme that disintegrates the collagen chain and involved in activation of platelet aggregation. Collagenase along with hyaluronidase is responsible for extracellular matrix degradation, due to their action rapid tissue penetration and spreading of bioactive substances of LS is possible. Hyaluronidase also disturbs the immune function of host by mobilizing the water content from the proteoglycans. These have an additive antimicrobial effect. In addition to the above mentioned compounds, a prostaglandin substance is also present that acts like prostacyclin it prevents the interaction between platelets and collagen and it also activates the adenyl cyclase of the platelet membrane which favors the antiaggregation of platelets [64].
11.2.2.3. Proteinase inhibitors effect
A similar group of compounds like bdellin, eglin C, kallikrein inhibitor and hirustasin are known to have effect like proteinase inhibitors. Bdellin is an enzyme that inhibits activities of trypsin, chymotrypsin, and plasmin and sperm acrosin. It has competitive action with hirudin on blood coagulation. It can be used as plasmin inhibitor to control bleeding. It also have anti-inflammatory role [65]. Kallikrein inhibitor is an inhibitor of the coagulation factors, plasma kallikrein and factor XIIa, which play a role in the intrinsic coagulation process. Hirustasin is serine protease inhibitors and basically it is Hirudo antistasin, it has capacity to bind with tissue kallikrein and it specifically inhibits the blood coagulation factor Xa. Recombinant antistasin (RA) was being used in animal experiments models. The main utility of RA established in animal studies is that it prevents vascular graft thrombosis. It reduces chances of restonsis of atherosclerotic arteries after balloon angioplasty. RA accelerates reperfusion in arterial thrombosis. It influences the mitotic division of cultured aortic smooth muscle cells. Another interesting feature observed for RA was that it has remarkable antimetastatic property [66].
11.2.2.4. Analgesic and anti-inflammatory effect
Some of the components of LS are known to have analgesic and anti inflammatory effects. They are hirustastin, ghilantens, eglin C, leech-derived tryptase inhibitor, complement C1 inhibitor, guamerin and piguamerin, bdellins and bdellastasin. The hirustastin of the LS inactivates kinins which activates the nociceptive nerve cells to induce or enhance pain sensations in host tissues. This property of hirustastin establishes it as a potential analgesic. Ghilantens is a protein component of LS which prolongs the prothrombin time of normal human plasma and it hampers the activity of factor Xa in blood coagulation. In animal experimental models it is known to suppress the metastases processes [60]. Eglin C of the LS binds with the neutrophils and blocks its activity on feeding site and its surrounding tissues. It acts an anti-inflammatory agent and prevents immune response on the host tissues. Leech-derived tryptase inhibitor has serine-type endopeptidase inhibitor activity. It inhibits the activity of tryptase and chymotrypsin of mast cells which are responsible for inflammatory reactions. An additional effect of this tryptase is exhibited on kinin–kallikrein system, chemo taxis, leukocyte activation, vasoactive actions and pain-generating interactions. Recombinant tryptase inhibitor is being explored experimentally for allergic and inflammatory diseases such anaphylaxis, arthritis and asthmas. Thus, it provides benefits of suppression of cell mediated inflammation in certain inflammatory diseases [67]. Complement C1 inhibitor block the pathways of complement system and is an integral part of immune system of host and first line of defense. Hence, it act as an anti – inflammatory in host tissues. Guamerin is a leukocyte elastase inhibitor and it is homologous to hirustasin. Piguamerin is a serine protease inhibitor of plasma kallikrein. It inhibits plasma and tissue kallikrein and trypsin. Bdellins and bdellastasin of LS inhibits trypsin, plasmin and sperm acrosin and known to have anti inflammatory effect on host tissues.
11.2.2.5. Increasing blood flow
The increase in blood flow on feeding site is caused by vasodilatation, endothelial muscle relaxation and by increasing local vascular permeability. This effect is result of activities of carboxypeptidase inhibitor, acetylcholine and histamine like substance present in LS. Carboxypeptidase inhibitor of LS inhibits a metalloproteinase which is responsible for the cleavage of kinin in blood plasma. This increased kinin result in blood flow to the feeding site [32].
11.2.2.6. Antimicrobial effect
Antimicrobial action of LS is not a completely established phenomenon but few compounds of LS know to have anti microbial properties [22] They are destabilase, chloromycetyn, theromacin, theromyzin.
11.2.2.7. Other action
LS contain enzymes that reduce scar tissue and adhesions. Fibrinases and collagenase in saliva reduces the density of scar tissue and it helps to reduce fibroblast formation in keloids and hypertrophic scars.
12. Future of MLT
MLT have huge benefits but to counter the unavailability of medicinal leech and to minimize the chances of secondary infections, chemical and mechanical alternatives may prove a beneficial tool in the future. Recent research had been carried out for developing a continual suction electromechanical device which performs the feeding function like medicinal leech. Trials on suction capacity of instruments have been evaluated by using liquids of different viscosity. Animal trials of such instruments had been carried out. If success is achieved in such attempts then the major hindrances of unavailability of sterile leeches for the MLT procedure can be successfully managed. The various secretions of LS are individually been extracted and synthesized by recombinant techniques. These compounds are been studied on various aspects like molecular structure, cellular and molecular activity, physiological functions and their specific therapeutic actions on various disease conditions. Hopefully this may assist in developing of various specific therapeutic agents for variety of diseases.
13. Conclusion
After reviewing various aspects of JA and MLT it can be concluded that both were similar in most of the aspects. The various indication and contraindication can be clearly understood in present day terminology along with descriptions of Ayurveda text. The various complications can be assessed and the possible measures can be adopted for their prevention. The probable mode of action of MLT not just helps in developing an understanding of the process but also lays a foundation for exploring the various new indications. Thus, it can be stated that the present day knowledge can assist in filling the gaps produced due extinction of parts of ancient literature and with its help an elaborated knowledge of the subject in present day terminology can be achieved that was explained in concise manner in Ayurveda text.
Source(s) of Funding
None
Conflict of interest
None
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2018.09.003.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Pandey Gangasahay., editor. Pt. Kashinath Sastri Vidhyotini Hindi commentarator of Caraka Samhita of Agnivesa- 1st volume, Sutra Sthan Viddhishonitama Adhayay chapter 24 verse 18. Chaukumba Sanskrit Sansthan; Varanasi: 2006. p. 445. [Google Scholar]
- 2.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 25. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 53. [Google Scholar]
- 3.Pt Vidhyasagar P.S., editor. Adhamalla's Dipika and Kashiram's Gudhartha-dipika Commentaries. Sharangdhara Samhita; Uttar Khanda Shonitasravaviddhi Adhayay chapter 12 verse 19-22. Surbharati Prakashana; Varanasi: 2006. pp. 622–623. [Google Scholar]
- 4.Pandey Gangasahay., editor. Pt. Kashinath Sastri Vidhyotini Hindi commentarator of Caraka Samhita of Agnivesa- 1st volume, Sutra Sthan Tris Eshaniya Adhayay chapter 11 verse 55. Chaukumba Sanskrit Sansthan; Varanasi: 2006. p. 239. [Google Scholar]
- 5.Demain Arnold L., Sanchez Sergio. Microbial drug discovery: 80 years of progress. J Antibiot. 2009;62:5–16. doi: 10.1038/ja.2008.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pt Harisadashiva shastri paradakara, editor. Sarvang sundar commentary by Arundatta and Ayurveda rasayan commentary by Hemadri of Astang Hridya of Vagbhata, Sutra Sthan Shastraviddhima Adhayay chapter 26 verse 36–37. Choukhambha Surbharati Prakashan Reprinted; Varanasi: 2011. p. 119. [Google Scholar]
- 7.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita , Sutra Sthan Jalokaavcharniyo Adhayay chapter 13 verse 15-17. Chaukumba Sanskrit Sansthan; Varanasi: 2009. pp. 44–45. [Google Scholar]
- 8.Eldor A., Orevi M., Rigbi M. The role of the leech in medical therapeutics. Blood Rev. 1996;10:201–209. doi: 10.1016/s0268-960x(96)90000-4. [DOI] [PubMed] [Google Scholar]
- 9.Mory R.N., Mindell D., Bloom D.A. The leech and the physician: biology, etymology, and medical practice with Hirudinea medicinalis. World J Surg. 2000;24:878–883. doi: 10.1007/s002680010141. [DOI] [PubMed] [Google Scholar]
- 10.Abdullah S., Dar M Latief, Adil Rashid, Anita Tewari. Hirudotherapy/leech therapy: applications and indications in surgery. Arch Clin Exp Surg. 2012;1(3):172–180. [Google Scholar]
- 11.Eroglu C., Hokelek M., Guneren E., Esen S., Pekbay A., Uysal O.A. Bacterial flora of Hirudo medicinalis and their antibiotic sensitivities in the middle black sea region, Turkey. Ann Plast Surg. 2001;47:70–73. doi: 10.1097/00000637-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita , Sutra Sthan Jalokaavcharniyo Adhayay chapter 13 verse 19-22. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 45. [Google Scholar]
- 13.Kaviraja Atrideva gupta, editor. Vd. Yadunandana Upadhyaya. Vidyotini Hindi commentary of Astang Hridya of Vagbhata, Sutra Sthan Shastraviddhima Adhayay chapter 26 verse 46-47. Choukhambha Prakashan Reprinted; Varanasi: 2008. p. 200. [Google Scholar]
- 14.Pandey Gangasahay., editor. Pt. Kashinath Sastri Vidhyotini Hindi commentarator of Caraka Samhita of Agnivesa- 1st volume, Sutra Sthan Viddhishonitama Adhayay chapter 24 verse 11-16. Chaukumba Sanskrit Sansthan; Varanasi: 2006. pp. 444–445. [Google Scholar]
- 15.PtHarisadashiva shastri paradakara, editor. Sarvang sundar commentary by Arundatta and Ayurveda rasayan commentary by Hemadri of Astang Hridya of Vagbhata, Sutra Sthan Shastraviddhima Adhayay chapter 26 verse 35. Choukhambha Surbharati Prakashan Reprinted; Varanasi: 2011. p. 199. [Google Scholar]
- 16.Raval H.N., Thakar A.B. Role of Raktamokshana by Jalaukavacharana and Siravedha in the management of Vicharchika (eczema) Ayurvedic. 2012;33(1):68–72. doi: 10.4103/0974-8520.100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borakhade Vasundhara R. Varsha S Khot treatment of Indralupta with local Jalaukavacharan and application of Gunja beeja Lepa: a case report. Int J Herbal Med. 2015;3(2):24–25. [Google Scholar]
- 18.Chaudhari Devendra R. To study the efficacy of Jalaukavacharan and shadanga Guggulu in Puyalasa w.s.r. to acute Dacryocystitis. J Ayurveda Integr Med Sci. 2016;4:39–41. [Google Scholar]
- 19.Bhuyan Chatrubhuja, Dudhamal T.S., Gupta S.K. Jalaukavacharan (leech application): Para-surgical approach to shlipada (filariasis): a pilot study indian. J Ancient Med Yoga. 2012;5(3):15–21. [Google Scholar]
- 20.Rastogi S., Chaudhari P. Pigment reduction in nevus of Ota following leech therapy. J Ayurveda Integr Med. 2014;5:125–128. doi: 10.4103/0975-9476.131736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andhey Vijay Pratap, Tambe Abhijit Laxman, Malavade Hrishikesh Chandrakant, Tople Prashant B. Role of Jalaukavacharana (hirudotherapy) in the management of scalp psoriasis- a case study. Int J Ayurveda Pharma Res. 2016;4(3):25–28. [Google Scholar]
- 22.Bhagat P.J., Raut S.Y., Lakhapati A.M. Clinical efficacy of Jalaukawacharana (leech application) in Thrombosed piles. Ayu. 2012;33(2):261–263. doi: 10.4103/0974-8520.105248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sawant D.P., Panzade S.M. Management of periapical abscess with Jalaukavcharana (Leech application) - a single case study. Int J Ayush Care. 2017;1(1):6–9. [Google Scholar]
- 24.Sharma M.R., Mehta C.S., Shukla D.J., Patel K.B., Patel M.V., Gupta S.N. Multimodal ayurvedic management for sandhigatavata (osteoarthritis of knee joints) Ayurvedic. 2013;34(1):49–55. doi: 10.4103/0974-8520.115447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stange R., Moser C., Hopfenmueller W., Mansmann U., Buehring M., Uehleke B. Randomised controlled trial with medical leeches for osteoarthritis of the knee. Compl Ther Med. 2012 Feb-Apr;20(1–2):1–7. doi: 10.1016/j.ctim.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Kalender M.E., Comez G., Sevinc A., Dirier A., Camci C. Leech therapy for symptomatic relief of cancer pain. Pain Med. 2010;11:443–445. doi: 10.1111/j.1526-4637.2010.00800.x. [DOI] [PubMed] [Google Scholar]
- 27.Abdualkader A.M., Ghawi A.M., Alaama M., Awang M., Merzouk A. Leech therapeutic applications. Indian J Pharmaceut Sci. 2013;75(2):127–137. [PMC free article] [PubMed] [Google Scholar]
- 28.Whitaker S., Oboumarzouk O., Rozen W.M., Naderi N., Balasubramanian S.P., Azzopardi E.A. The efficacy of medicinal leeches in plastic and reconstructive surgery: a systematic review of 277 reported clinical cases. Microsurgery. 2012 Mar;32(3):240–250. doi: 10.1002/micr.20971. [DOI] [PubMed] [Google Scholar]
- 29.Goessl C., Steffen-Wilke K., Miller K. Leech therapy for massive scrotal hematoma following percutaneous transluminal angioplasty. J Urol. 1997;158:545. [PubMed] [Google Scholar]
- 30.Asgari S.A., Rostami S., Teimoori M. Leech therapy for treating priapism: case report. Iran J Public Health. 2017;46(7):985–988. [PMC free article] [PubMed] [Google Scholar]
- 31.Ramzan M., Droog W., Visser Sleeswijk S., van Roessel E.W., Meynaar I.A. Leech got your tongue? Haematoma of the tongue treated with medicinal leeches: a case report. Neth J Crit Care. 2010;14(4):268–270. [Google Scholar]
- 32.Jha K., Garg A., Narang R., Das S. Hirudotherapy in medicine and Dentistry. J Clin Diagn Res: JCDR. 2015;9(12):ZE05–ZE07. doi: 10.7860/JCDR/2015/16670.6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Chalain T.M. Exploring the use of the Medicinal Leech: a clinical risk-benefit. J Reconst Microsurg. 1996;12(3):165–172. doi: 10.1055/s-2007-1006471. [DOI] [PubMed] [Google Scholar]
- 34.Cherniack E.P. Bugs as drugs, part two: worms, leeches, scorpions, snails, ticks, centipedes, and spiders. Altern Med Rev. 2011;16:50–58. [PubMed] [Google Scholar]
- 35.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 24. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 53. [Google Scholar]
- 36.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 27. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 53. [Google Scholar]
- 37.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 28. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 53. [Google Scholar]
- 38.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 29. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 53. [Google Scholar]
- 39.Verriere B., Sabatier B., Carbonnelle E., Mainardi J.L., Prognon P., Whitaker I., Lantieri L., Hivelin M. Medicinal leech therapy and Aeromonas spp. infection. Eur J Clin Microbiol Infect Dis. 2016;35(6):1001–1006. doi: 10.1007/s10096-016-2629-5. [DOI] [PubMed] [Google Scholar]
- 40.Martin G., 2nd, Linnell J.D., Yang S.S., Lin J., Camarata P.J., Andrews B.T. Ultrasound localization of a tunneled leech beneath a microvascular scalp reconstruction: a case report. Microsurgery. 2013;33(7):572–574. doi: 10.1002/micr.22163. [DOI] [PubMed] [Google Scholar]
- 41.Chua S., Pitts M., Lemark P. A simple, flexible and readily applicable method of boundary construction to prevent leech migration. Singap Med J. 2015;56(11):644. doi: 10.11622/smedj.2015176. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 42.Zengin S., Yarbil P., Kilic H., Al B. Prolonged bleeding due to a medicinal leech bite: another treatment method, primary suture BMJ. Case Rep. 2012;13:1–4. doi: 10.1136/bcr.02.2012.5759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Jalokaavcharniyo Adhayay chapter 13 verse 18. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 45. [Google Scholar]
- 44.Kaviraja Atrideva gupta, editor. Vd. Yadunandana Upadhyaya. Vidyotini Hindi commentary of Astang Hridya of Vagbhata, Sutra Sthan Shastraviddhima Adhayay chapter 26 verse 39. Choukhambha Prakashan Reprinted; Varanasi: 2008. p. 199. [Google Scholar]
- 45.Wilmer A., Slater K., Yip J., Carr N., Grant J. The role of leech water sampling in choice of prophylactic antibiotics in medical leech therapy. Microsurgery. 2013 May;33(4):301–304. doi: 10.1002/micr.22087. [DOI] [PubMed] [Google Scholar]
- 46.Das B.K. An Overview on Hirudo therapy/leech therapy. Ind Res J Pharm Science. 2014;1(1):33–41. [Google Scholar]
- 47.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita, Sutra Sthan Shonitavarniyama Adhayay chapter 14 verse 33-34. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 55. [Google Scholar]
- 48.Pandey Gangasahay., editor. Pt. Kashinath Sastri Vidhyotini Hindi commentarator of Caraka Samhita of Agnivesa- 1st volume, Sutra Sthan Viddhishonitama Adhayay chapter 24 verse 17- 18. Chaukumba Sanskrit Sansthan; Varanasi: 2006. p. 445. [Google Scholar]
- 49.Pandey Gangasahay., editor. Pt. Kashinath Sastri Vidhyotini Hindi commentarator of Caraka Samhita of Agnivesa- 1st volume, Sutra Sthan Viddhishonitama Adhayay chapter 24 verse 24. Chaukumba Sanskrit Sansthan; Varanasi: 2006. p. 449. [Google Scholar]
- 50.Pt. Harisadashiva shastri paradakara, editor. Sarvang sundar commentary by Arundatta and Ayurveda rasayan commentary by Hemadri of Astang Hridya of Vagbhata, Sutra Sthan Siravydha viddhi Adhayay chapter 27 verse 6–9. Choukhambha Surbharati Prakashan Reprinted; Varanasi: 2011. p. 202. [Google Scholar]
- 51.Vaidya yadavji Trikamji Acharya, editor. Shri Dalhanacharaya Nibandhasamgraha commentarator of Sushruta Samhita , Sutra Sthan Jalokaavcharniyo Adhayay chapter 13 verse 3. Chaukumba Sanskrit Sansthan; Varanasi: 2009. p. 44. [Google Scholar]
- 52.Pt Harisadashiva shastri paradakara, editor. Sarvang sundar commentary by Arundatta and Ayurveda rasayan commentary by Hemadri of Astang Hridya of Vagbhata, Sutra Sthan Shastraviddhima Adhayay chapter 26 verse 41–42. Choukhambha Surbharati Prakashan Reprinted; Varanasi: 2011. p. 200. [Google Scholar]
- 53.Houschyar K.S., Lüdtke R., Dobos G.J., Broecker-Preuss M., Rampp T., Brinkhaus B. Effects of phlebotomy-induced reduction of body iron stores on metabolic syndrome: results from a randomized clinical trial. BMC Med. 2012;10:53. doi: 10.1186/1741-7015-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim K.H., Oh K.Y. Clinical applications of therapeutic phlebotomy. Hematol Res Rev. 2016;7:139–144. doi: 10.2147/JBM.S108479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bacon B.R., Adams P.C., Kowdley K.V., Powell L.W., Tavill A.S. Diagnosis and management of hemochromatosis: 2011 practice guideline by the american association for the study of liver diseases. Hepatology (Baltimore, Md) 2011;54(1):328–343. doi: 10.1002/hep.24330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singal A.K., Kormos-Hallberg C., Lee C., Sadagoparamanujam V.M., Graddy J.J., Freeman D.H. Low-dose hydroxychloroquine is as effective as phlebotomy in treatment of patients with porphyria cutanea tarda. Clin Gastroenterol Hepatol. 2012;10(12):1402–1409. doi: 10.1016/j.cgh.2012.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Markham M.J., Lottenberg R., Zumberg M. Role of phlebotomy in the management of hemoglobin SC disease: case report and review of the literature. Am J Hematol. 2003;73(2):121–125. doi: 10.1002/ajh.10328. [DOI] [PubMed] [Google Scholar]
- 58.Valenti L., Fracanzani A.L., Dongiovanni P., Rovida S., Rametta R., Fatta E. A randomized trial of iron depletion in patients with nonalcoholic fatty liver disease and hyperferritinemia. World J Gastroenterol. 2014;20(11):3002–3010. doi: 10.3748/wjg.v20.i11.3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zaidi S.M., Jameel S.S., Zaman F., Jilani S., Sultana A., Khan S.A. A systematic overview of the medicinal importance of sanguivorous leeches. Altern Med Rev. 2011;16:59–65. [PubMed] [Google Scholar]
- 60.Sig A.K., Guney M., Uskudar Guclu A., Ozmen E. Medicinal leech therapy—an overall perspective. Integr Med Res. 2017;6(4):337–343. doi: 10.1016/j.imr.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Min G.S., Sarkar I.N., Siddall M.E. Salivary transcriptome of the North American medicinal leech, Macrobdella decora. J Parasitol. 2010;96:1211–1221. doi: 10.1645/GE-2496.1. [DOI] [PubMed] [Google Scholar]
- 62.Munro R., Powell Jones C., Sawyer Roy. Calin – a platelet adhesion inhibitor from the saliva of the medicinal leech. Blood Coagul Fibrinol – Int J Haemostasis Thromb. 1991;2:179–184. doi: 10.1097/00001721-199102000-00027. [DOI] [PubMed] [Google Scholar]
- 63.Seymour J.L., Henzel W.J., Nevins B., Stults J.T., Lazarus R.A. Decorsin. A potent glycoprotein IIb-IIIa antagonist and platelet aggregation inhibitor from the leech Macrobdella decora. J Biol Chem. 1990;265 [PubMed] [Google Scholar]
- 64.Salzet M. Anticoagulants and inhibitors of platelet aggregation derived from leeches. FEBS Lett. 2001;492:187–192. doi: 10.1016/s0014-5793(01)02212-8. [DOI] [PubMed] [Google Scholar]
- 65.Kvist S., Min G.-S., Siddall M.E. Diversity and selective pressures of anticoagulants in three medicinal leeches (Hirudinida: Hirudinidae, Macrobdellidae) Ecolo Evolut. 2013;3(4):918–933. doi: 10.1002/ece3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nutt E.M., Jain D., Lenny A.B., Schaffer L., Siegl P.K., Dunwiddie C.T. Purification and characterization of recombinant antistasin: a leech-derived inhibitor of coagulation Factor Xa. Arch Biochem Biophys. 1991;285:37-44. doi: 10.1016/0003-9861(91)90325-d. [DOI] [PubMed] [Google Scholar]
- 67.Pantoja-Uceda D., Arolas J.L., Aviles F.X., Santoro J., Ventura S., Sommerhoff C.P. Deciphering the structural basis that Guides the oxidative folding of leech-derived tryptase inhibitor. J Biol Chem. 2009;284(51):35612–35620. doi: 10.1074/jbc.M109.061077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.