Abstract
Objective
Out-of-Hospital Cardiac Arrest (OHCA) is a global public health problem. There is inadequate data on OHCA in India. The Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR) was planned to understand OHCA in a regional setting in India.
Methods
WACAR is a prospective one-year observational cohort study of OHCA in the Warangal area, Telangana, India. The study included 814 subjects of OHCA of presumed cardiac etiology brought to the Mahatma Gandhi Memorial Hospital during January 1, 2018, and December 31, 2018. The data collected included; standard Utstein variables with additional data on clinical characteristics (modified Utstein template).
Results
The majority of OHCA subjects were male with a median age of 60 years, and mostly occurring in residential locations within 1 h of onset of symptoms. Individuals with knowledge of CVD risk factors were more likely to report symptoms before OHCA. Data on resuscitation characteristics were inadequate.
Conclusions
The WACAR study provides baseline data regarding OHCA in a regional setting in India. The study demonstrated barriers involving data collection, patient knowledge of CVD risk factors and disease, and access to healthcare, which; impacted the data registry.
Keywords: Out-of-hospital cardiac arrest, Utstein template, CVD Risk factors, Cardiopulmonary resuscitation, Survival outcomes
1. Introduction
Cardiovascular disease (CVD) is a global public health problem with significant morbidity and mortality.1 The most concerning manifestation of CVD is Out-of-Hospital Cardiac Arrest.2,3 Global variations in reporting and documentation of OHCA pose a challenge in evaluating the exact burden of OHCA.4 Globally, it is estimated that on average, less than 10% of all patients with OHCA survive.5 An OHCA registry is an initial step in the collection of data on cardiac arrest. It helps to understand barriers in patient knowledge, regional healthcare-delivery issues, and information on measures, such as the links in the Chain of Survival that can improve survival rates from OHCA.6 The various currently available global registries on OHCA-the Cardiac Arrest Registry to Enhance Survival, the Pan-Asian Resuscitation Outcomes Study, European Registry of Cardiac Arrest and others have contributed significantly to the epidemiology of OHCA.7 These registries, and known literature have shown that the factors impacting OHCA are variable based on the setting and health care resources.8 Individual medical literacy, community and bystander involvement, the timing of cardiopulmonary resuscitation, EMS characteristics, and hospital services affect the OHCA outcomes.9,10 With the increasing impact of CVD in developing countries (low and middle-income countries - LMIC), it is imperative to have registries on OHCA. While several of the registries are developed based on the Utstein template, there is limited data on OHCA from India.11,12,13 A recent study on media reports of OHCA gave a glimpse of OHCA in India.14 With this background, the Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR) was planned to serve as one of the initial registries from India.
The Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR) was conducted to provide data on OHCA in a regional setting in India. In addition to standard Utstein variables, data collection on clinical information surrounding OHCA is also aimed at evaluating the relationship between knowledge about CVD, risk factors and their burden, and its impact on OHCA. Additionally, the registry could possibly provide insight into the barriers to the timely interventions.
2. Methods
2.1. Study design and setting
The WACAR is a prospective one-year observational study of OHCA in the Warangal area in the State of Telangana, India. OHCA cases were obtained from a regional Government Hospital, Mahatma Gandhi Memorial Hospital, which is a secondary care District Headquarters Hospital serving the medical needs of a population of about 2,000,000 individuals a year in a low resource setting.
2.2. Participants
The study population included all those above 18 years brought to the hospital with history of non-traumatic OHCA of presumed cardiac origin from January 1, 2018–December 31, 2018. A total of 814 individuals were included in the study for data analysis. The geographical area was chosen as a representative of India's communities with similar awareness and access to healthcare seen in most parts of India.
2.3. Data collection and variables
The Utstein checklist for standardized reporting of OHCA was followed in the study.15 The data form is based on the ILCOR consensus statement and other registries (CARES, PAROS).16,17 A Modified Utstein template was used with additional variables added to the original template. The data collection form includes information on demographics, patient characteristics, risk factors, history of heart disease, comorbidities, prior symptoms, resuscitation characteristics, event timing, utilization of Emergency Medical Services (EMS), and outcomes.
Study data were obtained from a review of hospital records. Medical staff involved in the care of OHCA were given data collection forms that were filled out in the emergency room setting. Information not obtained during the initial emergency room evaluation was acquired from bystanders (including victim's relatives) through telephone interviews. A few OHCA individuals had neither address nor phone number available to collect information.
Individual age was categorized into premature age and advanced or characteristic age for CVD to delineate differences associated with premature CVD risk. Age cutoffs for premature CVD risk were: under 55 years for Males and under 65 years for females.18 For the second age-category, 55 years and higher for males and 65 years and higher for females were used. Traditional CVD risk factors evaluated were: hypertension (HTN), hyperlipidemia, diabetes mellitus (DM), tobacco use, and family history of CVD. Risk factors were weighted similarly with 1 point assigned to risk factors, with higher points assigned for more risk factor burden. Symptom duration was classified as less than 1 h versus greater than 1 h before the onset of OHCA. Symptoms were evaluated, and individuals were categorized by those who had symptoms preceding the OHCA event versus those without known symptoms.
2.4. Ethical consideration
Permission for the study was taken from the hospital authorities and Institutional Ethics Committee (Approval number – KIEC/KMC/NCT/NIS/2018/CAR01). The study was registered in clinicaltrials.gov (N.C.T. number - NCT03791359).
2.5. Statistical analysis
Data are recorded in a structured database using MS Excel. Statistical analysis is done with 1) MedCalc Statistical Software version 19.3.1 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020) and 2) Epi Info™ 7.2.3.1 of the Centers for Disease Control and Prevention (C.D.C.), U.S.A.
Quantitative variables are summarized as mean ± S.D. and 95% C.I (confidence interval) of mean or median and 95% C.I of median depending upon normal or non- normal distribution. Qualitative variables are summarized as frequency, percentage, proportion, and 95% CI (confidence interval) of percentage.
The relationship between two or more qualitative variables is tested using the Fischer exact test or Chi-square test. An odds ratio (OR) and 95% C.I of OR is calculated to quantify the strength of the association between two variables. A p value less than 0.05 is taken as significant and exact p-values are reported.
3. Results
3.1. Etiology of OHCA
A total of 1106 subjects of OHCA were brought to M.G.M. hospital during January 2018 and December 2018. After exclusion of subjects due to trauma, hanging and burns, the sample of non-traumatic OHCA was sized down to 926. The study sample included 814 subjects with presumed cardiac etiology, the most common cause of OHCA (Table 1).
Table 1.
Etiology of Out of Hospital Cardiac Arrest. Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR).
| Presumed cardiac arrest etiology | Number | Percentage |
|---|---|---|
| Presumed cardiac | 814 | 87.90% |
| Poisoning | 52 | 5.62% |
| Respiratory | 15 | 1.62% |
| Electrocution | 10 | 1.07% |
| Snakebite | 10 | 1.07% |
| Others | 25 | 2.72% |
| Total | 926 | 100.00% |
3.2. Demographics and clinical characteristics of the study population
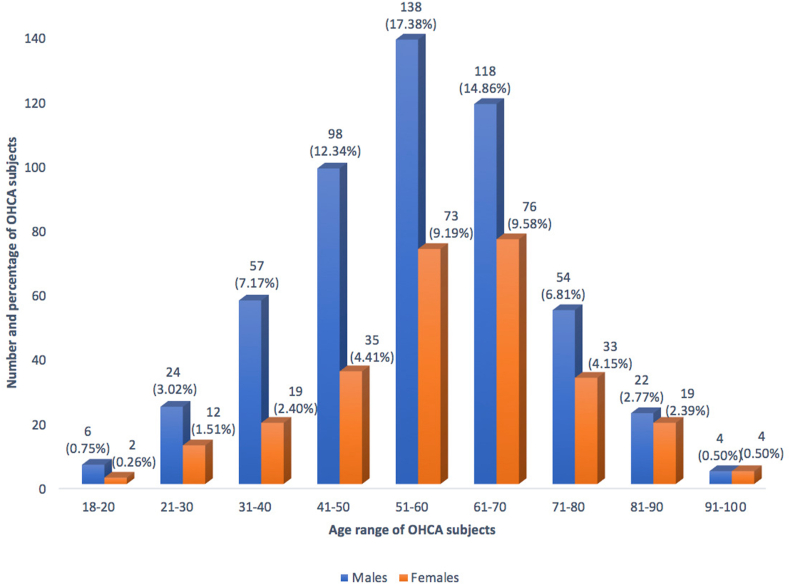
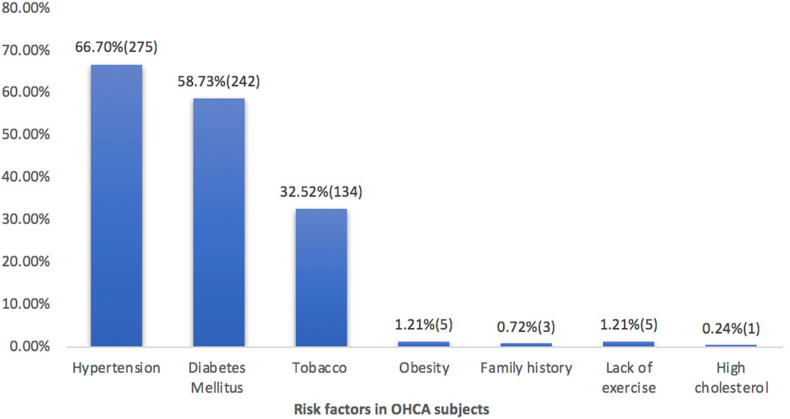
Preponderance of male subjects noted in the WACAR study. The median age for the population was 60 years. (range 18–100 years). Majority of OHCA occurred at residential locations and during day time. (Table 2, Fig. 1). Predominant proportion of OHCA patients belong to the advanced age group n = 448, 56.42%) in comparison to proportion of the premature age group (n = 346, 43.58%). Clinical characteristics are represented in Table 3. Analysis is done based on the available data for each variable. A significant number of subjects had at least one cardiovascular risk factor. Hypertension, diabetes mellitus and tobacco use were the common risk factors noted. (Fig. 2). Ischaemic heart disease and heart failure were the most common CVD reported (Table 3). Chest pain and shortness of breath are the common prodromal symptoms noted in this study.
Table 2.
Demographic characteristics of subjects of Out of Hospital Cardiac Arrest - Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR).
| Characteristic | Group | Frequency | Percent | 95% C.I (Wilson) | |
|---|---|---|---|---|---|
| 1. Gender (n = 814) | Male | 538 | 66.09% | 62.8%–69.3% | |
| Female | 276 | 33.91% | 30.7%–37.2% | ||
| 2. Age group (n = 794)* | 18–20 | 8 | 1.01% | 0.5%–2.0% | |
| 21–30 | 36 | 4.53% | 3.3%–6.2% | ||
| 31–40 | 76 | 9.57% | 7.7%–11.8% | ||
| 41–50 | 133 | 16.75% | 14.3%–19.5% | ||
| 51–60 | 211 | 26.57% | 23.6%–29.7% | ||
| 61–70 | 194 | 24.44% | 21.6%–27.5% | ||
| 71–80 | 87 | 10.96% | 9.0%–13.3% | ||
| 81–90 | 41 | 5.16% | 3.8%–6.9% | ||
| 91–100 | 8 | 1.01% | 0.5%–2.0% | ||
| 3. Location of OHCA (n = 760)** | Residence | 719 | 94.61% | 92.8%–96.0% | |
| Public place (Healthcare facility – 11; Street/Highway – 24; workplace – 2; Commercial building – 1; Hospital (MGMH) premises – 1; Office – 1 School −1) | 41 | 5.39% | 4.0%–7.2% | ||
| 4. Time of OHCA (n = 806)*** | Day: 56.09% | Morning | 207 | 25.69% | 22.8%–28.8% |
| Afternoon | 245 | 30.39% | 27.3%–33.7% | ||
| NIGHT: 43.91% | Evening | 218 | 27.05% | 24.1%–30.3% | |
| Early hours of morning | 136 | 16.87% | 14.5%–19.6% | ||
OHCA, Out -of Hospital Cardiac Arrest; M G M H, Mahatma Gandhi Memorial Hospital.
Missing data: * In 20 patients, the information on age was not available. - ** In 54 cases the data on location of OHCA was not mentioned. - *** In 8 patients the time of OHCA was not available.
Fig. 1.
Age distribution in subjects of Out-of-Hospital Cardiac Arrest-Males versus Females—Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR).
Table 3.
Clinical characteristics of subjects of OHCA - WACAR.
| Characteristic | Group | Frequency | Percent | 95% C.I (Wilson) | |
|---|---|---|---|---|---|
| 1. Risk factors (n = 589) | Yes | 414 | 70.29% | 66.48% | 73.84% |
| No | 175 | 29.71% | 26.16% | 33.52% | |
| 2. Number of Risk factors (n = 412)∗ | One risk factor | 201 | 48.79% | 43.99% | 53.60% |
| Two risk factors | 170 | 41.26% | 36.61% | 46.07% | |
| Three risk factors | 40 | 9.71% | 7.21% | 12.95% | |
| Four risk factors | 1 | 0.24% | 0.04% | 1.36% | |
| 3. Any past history of Heart Disease (n = 547) | Yes | 138 | 25.23% | 21.77% | 29.03% |
| No | 409 | 74.77% | 70.97% | 78.32% | |
| 4. If yes, Condition (n = 106)∗∗ | IHD and Heart Failure- Ischemic | 81 | 76.41% | 67.50% | 83.48% |
| Heart failure and Non-Ischemic Heart Failure | 18 | 16.98% | 11.02% | 25.25% | |
| Other | 7 | 6.61% | 3.24% | 13.01% | |
| ∗∗ | 32 | ||||
| 5. Any other comorbid illness (n = 375) | Yes | 174 | 46.40% | 41.41% | 51.46% |
| No | 199 | 53.06% | 48.01% | 58.06% | |
| Unknown | 2 | 0.54% | 0.15% | 1.92% | |
| 6. Comorbid illness (n = 173) | Cancer | 14 | 8.09% | 4.88% | 13.12% |
| Respiratory disease | 49 | 28.27% | 22.14% | 35.45% | |
| Renal disease | 35 | 20.17% | 14.92% | 26.83% | |
| Thyroid disease | 7 | 4.16% | 1.97% | 8.12% | |
| Stroke | 30 | 17.29% | 12.43% | 23.68% | |
| Liver disease | 9 | 5.26% | 2.76% | 9.59% | |
| Others | 29 | 16.76% | 11.93% | 23.04% | |
| 7. Preceding symptoms present (n = 764) | Yes | 460 | 60.21% | 56.7% | 63.6% |
| No | 304 | 39.79% | 36.38% | 43.30% | |
| 8. Duration of Symptoms (n = 352)∗∗∗ | <1hr | 282 | 80.11% | 75.63% | 83.95% |
| 1–24 h s | 51 | 14.49% | 11.19% | 18.55% | |
| >24 h s | 19 | 5.40% | 3.48% | 8.28% | |
| 9. Did victim Tell about the symptoms? (n = 252) ∗∗∗∗ | Yes | 218 | 86.51% | 81.74% | 90.18% |
| No | 34 | 13.49% | 9.82% | 18.26% | |
| 10. Any physician contacted? (n = 159) ∗∗∗∗∗ | Yes | 38 | 24.00% | 17.94% | 31.09% |
| No | 121 | 76.00% | 68.91% | 82.06% | |
Missing data: ∗ In 2(0.48%) patients definitive information on risk factors was not available. - ∗∗In 32(23.18%) there is no data on nature and type of heart disease. - ∗∗∗ In 108(23.47%) duration of onset of preceding symptoms in pts was not available. - ∗∗∗∗In 208(45.20%) There was no data on “did victim tell about the symptoms?” - ∗∗∗∗∗ In 301(65.43%) There was missing data on whether any physician was contacted.
OHCA,Out-of-Hospital Cardiac Arrest WACAR, Warangal Area Out-of-Hospital Cardiac Arrest Registry IHD, Ischaemic Heart Disease.
Fig. 2.
Risk factors in subjects of Out-of-Hospital Cardiac Arrest-Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR).
3.3. Resuscitation characteristics
OHCA was witnessed in a significant number of subjects. A relative was the first responder in the majority of subjects. Inadequate data was reported on resuscitation characteristics like the performance of CPR and the utilization of EMS(Table 4). A call to EMS was made in 281 subjects, but it was available in only 190 subjects. All other subjects were reported to have utilized private modes of transport. Documentation of cardiac rhythm was available only for one subject. Though performance of CPR was reported in 139 subjects, no survivors of OHCA were reported in this study.
Table 4.
Resuscitation characteristics of subjects of OHCA-Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR).
| Characteristic | Group | Frequency | Percent | 95% C.I (Wilson) | |
|---|---|---|---|---|---|
|
Yes | 523 | 90.79% | 88.16% | 92.9% |
| No | 53 | 9.21% | 7.10% | 11.84% | |
| 2. First responder witness (n = 540) | Relative | 533 | 98.70% | 97.35% | 99.37% |
| Friend | 3 | 0.56% | 0.20% | 1.62% | |
| Stranger | 1 | 0.18% | 0.03% | 1.04% | |
| Other | 3 | 0.56% | 0.20% | 1.62% | |
| 3. EMS called (n = 567) | Yes | 281 | 49.55% | 45.46% | 53.66% |
| No | 286 | 50.45% | 46.34% | 54.54% | |
| 4. Type of EMS called (n = 258) ∗ | Ambulance 108 | 221 | 85.70% | 80.86% | 89.58% |
| Ambulance- | 37 | 14.30% | 10.59% | 19.14% | |
| 5. CPR initiated (n = 500) | Yes | 139 | 27.80% | 24.05% | 31.88% |
| No | 361 | 72.20% | 68.12% | 75.95% | |
| 6. If Yes, type of CPR initiated (n = 103)∗∗ | CPR with compressions and breaths | 7 | 6.80% | 3.33% | 13.37% |
| Hands only CPR | 95 | 92.23% | 85.42% | 96.01% | |
| Hands only CPR, use of defibrillator. | 1 | 0.97% | 0.17% | 5.30% | |
| 7. CPR initiated by (n = 126)∗∗∗ | EMS person | 42 | 33.33% | 25.70% | 41.95% |
| Trained in CPR | 43 | 34.13% | 26.43% | 42.76% | |
| Family LP | 31 | 24.60% | 17.91% | 32.80% | |
| stranger LP | 10 | 7.94% | 4.37% | 13.99% | |
| 8. Time interval between OHCA and initiation of CPR (n = 87)∗∗∗∗ | <5 min | 7 | 8.04%% | 3.95% | 15.69% |
| 5–20 min | 64 | 73.56% | 63.44% | 81.69% | |
| >20 min | 16 | 18.40% | 11.65% | 27.80% | |
| 9. EMS ambulance available (n = 190) | Yes | 108 in 153 and other ambulance in 37 | 108 responded in 69.2% and other ambulance responded in 100.00% | – | – |
| – | – | – | – | – | |
| 10. Time of arrival of EMS (n = 124)∗∗∗∗∗ | |||||
| 5 min | 4 | 03.23% | 1.30% | 8.00% | |
| 10 min | 24 | 19.35% | 13.37% | 27.19% | |
| 15 min | 55 | 44.35% | 35.91% | 53.14% | |
| 20 min | 23 | 18.55% | 12.69% | 26.30% | |
| 30 min | 12 | 09.70% | 5.62% | 16.15% | |
| 40 min | 3 | 02.41% | 0.83% | 6.87% | |
| 60 min | 3 | 02.41% | 0.83% | 6.87% | |
| 11. AED/Defibrillator used (n = 44) | Yes | 17 | 38.63% | 25.72% | 53.38% |
| No | 27 | 61.36% | 46.62% | 75.25% |
Missing data: ∗ In 23(8.18%) cases there is no data on the type of EMS called. - ∗∗ In 36(25.89%) there is missing data of which type of CPR was performed - ∗∗∗ In 13(9.35%) there is no data regarding who initiated the CPR - ∗∗∗∗ In 52(37.41%) the time between OHCA and start of CPR was not available. - ∗∗∗∗∗ In 66(34.7%) The time of arrival of EMS was not available.
OHCA,Out-of-Hospital Cardiac Arrest; EMS, Emergency Medical Services; CPR,Cardiopulmonary Resuscitation; AED, Automated External Defibrillator; LP, Lay Person.
3.4. Associations between characteristics of subjects of OHCA
We studied the associations between variables or defined characteristics of subjects of OHCA. The study noted predominance of males in the advanced age group (71.65%) compared to females (28.35%), p value < 0.0001. Gender differences were not observed in the prevalence of risk factors in OHCA subjects. (Males, 72.56% vs. Females, 66.19%). A higher proportion of males and females in advanced age Group (75.9%, 78.6%) had risk factors compared to those in the premature age group respectively (66.9%,55.9% respectively, p = 0.0003). The study results point to a lack of association between gender and heart disease and also gender wise age group and CVD (Females with CVD 24.24% and males with CVD 24.79%). OHCA subjects in advanced age group (63.26%) are two times more likely to have CAD risk factors compared to those in the premature CVD age group (36.74%) p < 0.0001. Majority of those with risk factors, 84.68% reported symptoms preceding OHCA compared to those without risk factors, 65.58%, p < 0.0001. 84.8% of those with CVD had risk factors, while 15.2% of those with CVD had no risk factors. This suggests that OHCA subjects with risk factors have a greater chance of heart disease (p value < 0.0003). Significant proportion of patients with history of heart disease belong to advanced age group (69.34%), compared to premature age group (30.66%) p = 0.0094. Females (66.28%) are more likely to have symptoms preceding cardiac arrest Compared to males (57.06%) p < 0.0156). While 63.1% in the advanced age group reported symptoms preceding OHCA, 59.38% of those in premature age group had symptoms. There is no association between the proportion of subjects in the age group versus symptoms preceding OHCA and duration of symptoms before cardiac arrest versus the victim reporting symptoms to the attendants. 15.2% of OHCA subjects with symptoms less than 1 h did not inform attendants about symptoms.75.76% of those with preceding symptoms more than 1 h prior had known risk factors compared to 76.87% of those with preceding symptoms of less than 1 h. This suggests no correlation between risk factors and duration of symptoms preceding OHCA. In 27.5% (n = 224) of the total 814 subjects, there was difficulty in completing the entire data due to lack of contact phone number and follow-up responses.
4. Discussion
This is the first registry on OHCA in a regional setting in India incorporating standard Utstein data elements including clinical characteristics (Modified Utstein template). The WACAR study provides a snapshot of epidemiology of OHCA in India. This registry is an initial attempt to understand the issues regarding CVD in India in relation to OHCA. This study was designed to understand the barriers in OHCA registry from the healthcare systems perspective and the impact of patient's CVD knowledge on OHCA. To the best of our knowledge, the mutual relationship between patient's knowledge of CVD and OHCA in the current setting has not been addressed before in the available literature.
A comparative review of the Utstein data elements in the WACAR study in relation to other international registries provides a framework for emergency systems in India to measure and improve resuscitation care. Data of gender, age and location are similar to other OHCA registries.19,20,21
Gender differences in epidemiology and resuscitation outcomes after OHCA are well known.22 Female subjects of OHCA belong to the older age group, experience arrest in private locations, have fewer initial shockable rhythms, are less likely to receive evidence-based interventions and have worse outcomes. This is partly explained by biological sex and gender-based influences.23 The PAROS study showed that women in reproductive age group had better outcomes compared to menopausal women.24
Efforts to improve survival from OHCA in residential areas should include training family members in CPR and reducing ambulance response times.25 The present study has relatively higher occurrences of OHCA in residential areas compared to other registries. A recent study in India has given elaborate information on public locations of OHCA in India which highlights the need to identify high risk areas of OHCA and initiate public health measures in this direction.14Implementation of Public access defibrillation programs is known to improve survival from OHCA.26 The increased occurrence of OHCA during day time is noted in this study. Temporal variability in incidence and survival after OHCA is well known. This is explained by the variability in biological processes and the links in the Chain of survival.27, 28
The WACAR study demonstrated the predominance of classical risk factors for CAD—HTN, DM, tobacco use which are known to increase the risk for OHCA which is already known from the Reykjavik study.29,30 Smoking as a modifiable risk factor has the strongest association with OHCA in men, increasing the risk by 70% IHD and heart failure as common causes of cardiac-related OHCA have been documented in previous studies.31,32 Increasing age and comorbid conditions negatively impact outcomes after OHCA.
The importance of collecting detailed data on clinical characteristics of OHCA in the Indian scenario is emphasised in the context of increasing burden of CVDs in India.33. With the UN Goal of Reducing Premature Mortality from NCDs by 25% by 2025 fast approaching, focusing on screening for risk factors, implementation of National programs on NCD, population-based screening for CVD and evidence-based treatment of CVD are the need of the hour.
The reporting of chest pain and shortness of breath as dominant symptoms is consistent with other studies.,34 Early notice of prodromal symptoms would lead to early activation of EMS, Early access to healthcare and prevent OHCA and also improve outcomes.35 Increasing delay in activating EMS before the onset of OHCA is associated with reduced survival. Individuals with prior knowledge of CVD are more likely to report symptoms before OHCA and seek early Emergency Cardiovascular care. It is also known that subjects of OHCA seek healthcare and present symptoms during the week prior to an OHCA. Data in the registry indicates that knowledge of CVD and risk factors contribute to behavioural changes to seek early healthcare. This could encourage the family members to call EMS urgently and transport patients to hospitals faster. Public health initiatives like educating lay public on aspects of CVD are expected to reduce patient delays to access health care from the onset of symptoms. Various factors such as witnessed OHCA, immediate High-quality CPR and early defibrillation impact the survival outcomes from OHCA.36
The weak data on resuscitation variables in the study points to the need to increase awareness on cardiac arrest and Hands-only CPR. It is known that Utstein survival (the rate of survival among, persons whose arrests are witnessed by a bystander and who had an initial shockable rhythm) is a better measurement tool for determining the effective of Community CPR training. National health initiatives to enhance public awareness of OHCA and lay rescuer CPR training involving partnerships between national societies are on the anvil.37 A recent study by Srinivas et al highlighted the vital role of Indian media in raising public awareness of cardiac arrest and CPR.14 The weak links in the Chain of Survival provide an opportunity to improve survival outcomes from OHCA.38,39
The vital information from such registries needs to be utilised in initiating region-specific cardiac care projects throughout India (such as Heart Rescue India project in Bengaluru, Karnataka) to enhance outcomes.40 A community-centred public health approach involving the application of the framework of the Haddon Matrix for sudden cardiac arrest is in need. This involves surveillance-high-quality data collection, identification of risk of SCA, protective factors, evidence-based interventions and implementation -population level education and enforcement aiming at improvement of outcomes from OHCA.41 Implementation of the Utstein formula pairing medical science with educational efficiency and local implementation along with a systems approach is proven to improve survival from OHCA.3
4.1. Limitations
The limiting factors in the study include the lack of a centralized data collection and OHCA registry system, difficulties in accessing relevant information from all area hospitals, and possible inaccuracy in the total number of OHCA cases reported from this study's geographic area in one year. All these contribute to selection or reporting bias. Difficulties in data collection are also due to lack of access to records from EMS ambulance systems (Public or Private).42 OHCA is not a reportable event in India. Lack of verifiable data from death certificates, gaps in information from the hospital records and unreliability of information provided by the first responders and family contribute to information bias. Recalling the details of the OHCA by first responders could be a recall-bias.
5. Conclusions
The results of WACAR highlight that OHCA of cardiac etiology is a significant public health problem in India. WACAR also gives insight into the epidemiology of OHCA in India to some extent and the difficulties in data collection. Initial high-quality data collection, designing and implementation of regional programs tailored to the specific needs of a community are necessary. Public health campaign strategies to raise awareness of CVD and Sudden Cardiac Arrest, Bystander CPR training and Public Access Defibrillators and timely Tertiary Cardiac Care are needed to improve outcomes. The EMS system, public or private, needs to be adequately strengthened with the necessary life-saving equipment and ongoing training of EMS personnel. It is hoped that this preliminary study will generate enough interest for more prospective comprehensive OHCA Registries with the Governmental support.
Key messages.
-
∗
What is already known about this subject?
There is limited data on OHCA in India. Until now, there is no Registry on OHCA in India based on Utstein template.
-
∗
What does this study add to existing knowledge?
The WACAR study provides a snapshot of the epidemiology of OHCA in a regional setting in India. In addition, the study provides data on CVD and risk factors in subjects of OHCA.
-
∗
What is the likely impact?
This study highlights the need for an Indian OHCA National Registry to improve outcomes.
Mendeley dataset: Research data linked to this article: http://dx.doi.org/10.17632/cwc9v4p56s.1.
Funding
There is no funding for the WACAR study.
Conflicts of interest
All authors have none to declare.
Acknowledgments
Our sincere thanks to the following for their help during the study.
1. Dr B Srinivas Rao,Superintendent, M.G.M Hospital.
2. Medical staff in the Casualty/ED. MGM Hospital, Warangal, Telangana, India.
3. Deepak Kumar Bandari, PrashanthiBalerao, Mahesh Adimulam, Jillila Sushma Jemimah, Beeram. Manoj Prabhakar Reddy, Vankudoth Sandeep from Vaagdevi Institute of Pharmaceutical Sciences,Warangal, Telangana,India.
4. Mruudhula Devi Pandi, SaikumarMedi,fromJayamukhi College of Pharmacy,Warangal,Telangana, India and.
5. Mr Vineet from Kakatiya Medical College, Warangal, Telangana, India.
6. Relatives and attendants of subjects of OHCA in the WACAR study.
References
- 1.Benjamin E.J., Muntner P., Alonso A. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Morentin B., Audicana C. Population-based study of out-of-hospital sudden cardiovascular death: incidence and causes of death in middle-aged adults. Rev Esp Cardiol. 2011;64(1):28–34. doi: 10.1016/j.recesp.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Myat A., Song K.J., Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391:970–979. doi: 10.1016/S0140-6736(18)30472-0. [DOI] [PubMed] [Google Scholar]
- 4.Schulz M., Steinmetz J. 2018. Global Differences in Out-Of-Hospital Cardiac Arrest Reporting; pp. 1–19. [online] Jems.com. [Google Scholar]
- 5.Editorial Out-of-hospital cardiac arrest: a unique medical emergency. Lancet. 2018;391:911. doi: 10.1016/S0140-6736(18)30552-X. [DOI] [PubMed] [Google Scholar]
- 6.Wu W.Y. Out-of-hospital cardiac arrest: the importance of a registry. Hong Kong Med J. 2019;25(3):176–177. doi: 10.12809/hkmj197990. [DOI] [PubMed] [Google Scholar]
- 7.McNally B. The importance of cardiac arrest registries. Scand J Trauma Resus. 2014;22(Suppl 1):A3. [Google Scholar]
- 8.Robert Graham, McCoy Margaret A., Andrea M.S. Strategies to Improve Cardiac Arrest Survival: A Time to Act. 2015. Understanding the public health burden of cardiac arrest: the need for national surveillance; pp. 49–87. [Google Scholar]
- 9.Morgan D.P., Muscatello D., Hayen A. Human factors influencing out-of-hospital cardiac arrest survival. Emerg Med Australasia (EMA) 2019;31(4):600–604. doi: 10.1111/1742-6723.13222. [DOI] [PubMed] [Google Scholar]
- 10.Navab E., Esmaeili M., Poorkhorshidi N. Predictors of out of hospital cardiac arrest outcomes in pre-hospital settings; a retrospective cross-sectional study. Arch. Acad. Emerg. Med. 2019;7(1):e36. [PMC free article] [PubMed] [Google Scholar]
- 11.Krishna C.K., Showkat H.I., Taktani M. Out of hospital cardiac arrest resuscitation outcome in North India CARO study. World J Emerg Med. 2017;8(No 3):200–205. doi: 10.5847/wjem.j.1920-8642.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grewal C.S., Singh B., Bansal R. Outcome in survivors of out of hospital cardiac arrest in a tertiary care center of north India: a prospective observational study. J Pract Cardiovasc Sci. 2018;4:193–197. [Google Scholar]
- 13.Ramaka S., Machavarapu M., Chodavarapu P. A study of adult out of hospital cardiac arrests in an Indian population. Global Heart. 2016;11(2):e82–e83. [Google Scholar]
- 14.Ramaka S., Murthy V.S., Nanda N.C. An observational study of out-of-hospital cardiac arrests reported in Indian print media. J Indian collcardiol. 2019;9:223–229. [Google Scholar]
- 15.Perkins G.D., Jacobs I.G., Nadkarni V.M. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 16.Cardiac Arrest Registry to Enhance Survival (CARES) 2018. Data Dictionary; pp. 1–61.https://mycares.net/sitepages/uploads/2018/Data%20Dictionary%20(2018).pdf Retrieved from. [Google Scholar]
- 17.Ong M.E.H., Shin S Do, Tanaka H. Pan-asian resuscitation outcomes study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18(8):890–897. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 18.Iyengar S.S., Gupta R., Ravi S. Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry. Indian Heart J. 2017;69(2):211–216. doi: 10.1016/j.ihj.2016.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mcnally B., Mehta M. Cardiac arrest registry to enhance survival (CARES) My Cares. 2011;60(8):1–19. https://mycares.net/downloads/CARES Summary Document 9.10.07.pdf Retrieved from. [PubMed] [Google Scholar]
- 20.Gräsner J.T., Lefering R., Koster R.W. EuReCa ONE—27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Ong M.E.H., Shin SDo, De Souza N.N.A. Outcomes for out-of-hospital cardiac arrests across 7 countries in asia: the Pan asian resuscitation outcomes study (PAROS) Resuscitation. 2015;(96):100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 22.Karlsson V., Dankiewicz J., Nielsen N. Association of gender to outcome after out-of-hospital cardiac arrest - areport from the international cardiac arrest registry. Crit Care. 2015;19:182. doi: 10.1186/s13054-015-0904-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jarman A.F., Mumma B.E., Perman S.M. When the female heart stops: sex and gender differences in out-of-hospital cardiac arrest epidemiology and resuscitation. Clin Therapeut. 2019;41(6):1013–1019. doi: 10.1016/j.clinthera.2019.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng Y.Y., Wah W., Liu N. Associations between gender and cardiac arrest outcomes in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation. 2016;102:116–121. doi: 10.1016/j.resuscitation.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Shaun Goh E., Liang B., Fook-Chong S. Effect of location of out-of-hospital cardiac arrest on survival outcomes. Ann Acad Med Singapore. 2013;42:437–444. [PubMed] [Google Scholar]
- 26.Hansen S.M., Hansen C.M., FolkeF Bystander defibrillation for out-of-hospital cardiac arrest in Public vs Residential Locations. JAMA Cardiol. 2017;2(5):507–514. doi: 10.1001/jamacardio.2017.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bagai A., McNally B.F., Al-Khatib S.M. Temporal differences in out-of-hospital cardiac arrest incidence and survival. Circlation. 2013;128(24):2595–2602. doi: 10.1161/CIRCULATIONAHA.113.004164. [DOI] [PubMed] [Google Scholar]
- 28.Wallace S.K., Abella B.S., Shofer F.S. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation. 2013;127(15):1591–1596. doi: 10.1161/CIRCULATIONAHA.113.002058. [DOI] [PubMed] [Google Scholar]
- 29.Thorgeirsson G., Thorgeirsson G., Sigvaldason H. Risk factors for out-of-hospital cardiac arrest: the Reykjavik Study. Eur Heart J. 2005;26:1499–1505. doi: 10.1093/eurheartj/ehi179. [DOI] [PubMed] [Google Scholar]
- 30.Voruganti D.C., Chennamadhavuni A., GarjeR Association between diabetes mellitus and poor patient outcomes after out-of-hospital cardiac arrest: a systematic review and meta-analysis. Sci Rep. 2018;8(1):1–8. doi: 10.1038/s41598-018-36288-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geri G., Passouant O., Dumas F. Etiological diagnoses of out-of-hospital cardiac arrest survivors admitted to the intensive care unit: insights from a French registry. Resuscitation. 2017;117:66–72. doi: 10.1016/j.resuscitation.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Gorgels A.P.M., Gijsbers C., De Vreede-Swagemakers J. Out-of-hospital cardiac arrest - the relevance of heart failure. The Maastricht Circulatory Arrest Registry. Eur Heart J. 2003;24:1204–1209. doi: 10.1016/s0195-668x(03)00191-x. [DOI] [PubMed] [Google Scholar]
- 33.Prabhakaran D., Jeemon P., Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133:1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 34.Nehme Z., Bernard S., Andrew E. Warning symptoms preceding out-of-hospital cardiac arrest: do patient delays matter? Resuscitation. 2018;123:65–70. doi: 10.1016/j.resuscitation.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 35.Höglund H., Jansson J.H., Forslund A.S. Prodromal symptoms and health care consumption prior to out-of-hospital cardiac arrest in patients without previously known ischaemic heart disease. Resuscitation. 2014;85(7):864–868. doi: 10.1016/j.resuscitation.2014.03.300. [DOI] [PubMed] [Google Scholar]
- 36.Ong M.E.H., Perkins G.D., Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet. 2018 Mar 10;391(10124):980–988. doi: 10.1016/S0140-6736(18)30316-7. [DOI] [PubMed] [Google Scholar]
- 37.Kapoor M.C., Ahmed S.M., Garg R. Indian resuscitation council cardiopulmonary resuscitation guidelines: the way ahead! Indian J Anaesth. 2018;62(11):924–925. doi: 10.4103/ija.IJA_646_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sasson C., Rogers M.A.M., Dahl J. Predictors of survival from out-of-hospital cardiac arrest a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 39.McCarthy J.J., Carr B., SassonC Out-of-Hospital cardiac arrest resuscitation systems of care: a scientific statement from the American heart association. Circulation. 2018;137(21):e645–e660. doi: 10.1161/CIR.0000000000000557. [DOI] [PubMed] [Google Scholar]
- 40.Ramesh A., LaBresh K.A., Begeman R. Implementing a STEMI system of care in urban Bangalore: rationale and Study Design for heart rescue India. Contemp Clin Trials. 2018;10:105–110. doi: 10.1016/j.conctc.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van de Voorde P., Monsieurs K.G., Perkins G.D. Looking over the wall: using a Haddon Matrix to guide public policy making on the problem of sudden cardiac arrest. Resuscitation. 2014;85(5):602–605. doi: 10.1016/j.resuscitation.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 42.National Health Systems Resource Centre, MOHFW, Government of India, https//www.nhsrcindia.org Emergency Medical Service (EMS) In India: A Concept Paper National Health Systems Resource Centre (NHSRC) Technical Support Institution with National Rural Health Mission (NRHM) Ministry of Health & Family Welfare, Government of India New Delhi – 11006. 1-17. Accessed September 16, 2020.