Abstract
Policy Points.
One of the most important possibilities of value‐based payment is its potential to spur innovation in upstream prevention, such as attention to social needs that lead to poor health. Screening patients for social risks such as housing instability and food insecurity represents an early step physician practices can take to address social needs.
At present, adoption of social risk screening by physician practices is linked with having high innovation capacity and focusing on low‐income populations, but not exposure to value‐based payment.
Expanding social risk screening by physician practices may require standardization and technical assistance for practices that have less innovative capacity.
Context
One of the most important possibilities of value‐based payment is its potential to spur innovation in upstream prevention, such as attention to social needs that lead to poor health. However, there is uncertainty about the conditions under which value‐based payment will encourage health care providers to innovate to address upstream social risks.
Methods
We used the 2017‐2018 National Survey of Healthcare Organizations and Systems (NSHOS), a nationally representative survey of physician practices (n = 2,178), to ascertain (1) the number of social risks for which practices systematically screen patients; (2) the extent of practices’ participation in value‐based payment models; and (3) measures of practices’ capacity for innovation. We used multivariate regression models to examine predictors of social risk screening.
Findings
On average, physician practices systematically screened for 2.4 out of 7 (34%) social risks assessed by the survey. In the fully adjusted model, implementing social risk screening was not associated with the practices’ overall exposure to value‐based payment. Being in the top quartile on any of three innovation capacity scales, however, was associated with screening for 0.95 to 1.00 additional social risk (p < 0.001 for all three results) relative to the bottom quartile. In subanalysis examining specific payment models, participating in a Medicaid accountable care organization was associated with screening for 0.37 more social risks (p = 0.015). Expecting more exposure to accountable care in the future was associated with greater social risk screening, but the effect size was small compared with practices’ capacity for innovation.
Conclusions
Our results indicate that implementation of social risk screening—an initial step in enhancing awareness of social needs in health care—is not associated with overall exposure to value‐based payment for physician practices. Expanding social risk screening by physician practices may require standardized approaches and implementation assistance to reduce the level of innovative capacity required.
Keywords: social determinants of health, social risk screening, primary care, implementation science
Emerging evidence suggests that helping patients resolve social needs such as unstable housing, food insecurity, and lack of income can improve health and thereby reduce unnecessary health care use and spending. 1 , 2 , 3 Health care providers operating under value‐based payment models such as capitated insurance designs, accountable care organizations (ACOs), and pay‐for‐performance programs, therefore, could have a business case for identifying patients’ social risks and offering support to help patients address social needs. 4 However, there is uncertainty about the conditions under which value‐based payment incentives will actually lead health care providers to innovate with upstream approaches focused on social needs of vulnerable populations. 5 , 6 A recent evidence synthesis found a lack of research to determine which if any accountable care models were encouraging attention to social needs, 7 though two studies have reported unadjusted associations between social needs programs and ACO participation. 8 , 9 Upstream approaches stretch the traditional boundaries of health care, requiring new types of expertise and new work patterns for health care organizations. Further research is needed to understand how value‐based payment models and organizational capacity for innovation jointly influence adoption of upstream approaches.
To help patients with upstream social needs, health care providers must first become aware of social risks faced by their patients. 7 Although models for assisting patients with social needs in health care settings remain nascent, a 2019 consensus report by the National Academy of Medicine stated that “identifying social needs is a critical first step to the integration of these needs into health care.” 7 Screening patients for social risks is core to pilot initiatives such as the federal Accountable Health Communities model, in which participating health care providers use a standardized tool to screen Medicare and Medicaid patients for risks related to housing, food, transportation, utilities, and safety. 10
Additional efforts to document social risks in health care settings have proliferated in recent years. 11 , 12 Large‐scale empirical evidence on implementation of social risk screening remains limited, 7 but the recent National Survey of Healthcare Organizations and Systems (NSHOS) indicated that across the United States, less than one‐quarter of either physician practices or hospitals systematically screen patients for common social risks. 8 Descriptive results from this recent survey published by members of our team showed that physician practices participating in value‐based payment models such as ACOs and bundled payments were more likely to screen for social risks. 8 It is unclear, however, if these value‐based models facilitate social care integration, or if underlying organizational capacities facilitate both value‐based payment and social risk screening.
Dissemination of Health Care Delivery Innovations
Prominent conceptual models of innovation in health care recognize that some organizations are better at identifying and implementing care delivery innovations than other organizations, regardless of external incentives that may be created by value‐based payment. Organization‐level capacity to implement innovations—also called absorptive capacity 13 —often depends on having an organizational culture that encourages innovation, as well as specific infrastructure and skills needed to deploy the innovation in question. As an emergent intervention, social risk screening implementation may be especially sensitive to whether a particular physician practice has an organizational culture of innovation. Because social risk screening involves complex processes with many potential points of failure, 14 implementation is also likely to depend on physician practices having certain prerequisite infrastructure and skills. Such prerequisites could include information technology to administer screening and having established processes for adapting care delivery systems within the practice.
In considering dissemination of social risk screening, it is also important to recognize that patients with unmet social needs are unevenly distributed across physician practices. Practices where low‐income patients make up a substantial share of the patient population, such as Federally Qualified Health Centers (FQHCs), would likely see more advantages to introducing systematic approaches to social risk screening.
The recent availability of national data on social risk screening by physician practices presents an opportunity to investigate how value‐based payment encourages social risk screening across practices with varying capacities for innovation and levels of patient need. Value‐based payment models continue to spread. One of the most important possibilities of value‐based payment is its potential to spur innovation in upstream prevention, correcting a market failure that has historically focused innovators on curative as opposed to preventive interventions. Innovation in a system as complex as health care delivery depends on many factors, however, making it important to deepen our understanding of the interrelation of value‐based payment and organizational capacities that underlie innovation.
In this study, we used detailed data on US primary care physician practices to examine how exposure to value‐based payment models and practice capacity for innovation were associated with the extent to which physician practices screen for social risks. Our results can help inform practitioners and policymakers interested in the interaction between value‐based payment and adoption of new models of prevention by health care providers.
Methods
Sample and Data Collection
We used the 2017‐2018 National Survey of Healthcare Organizations and Systems to obtain data on screening for social risks, exposure to value‐based payment reform, and organizational capacity for innovation. NSHOS is a nationally representative survey of physician practice sites that include three or more adult primary care physicians. 15 The survey was completed by a practice leader on behalf of the practice. NSHOS used the OneKey database, produced by IQVIA, to identify physician practices and draw a representative national sample. A total of 2,333 of 4,976 physician practices completed the NSHOS survey (response rate 46.9%). After we removed 155 responses from practices that were identified as ineligible or missing variables needed for our analysis, survey responses from 2,178 practices were available for analysis.
Dependent Variable
The NSHOS survey asked practices to report whether they had systems in place to screen for seven social risks: food insecurity, housing instability, utility needs, interpersonal violence, transportation needs, inability to pay medical bills, and unused Medicaid eligibility. We calculated the number of social risks screened by each practice.
Independent Variables
Exposure to Value‐Based Payment Models
We calculated current exposure as number of value‐based payment initiatives the practice reported on the NSHOS (range 0‐7). Options included bundled or episode‐based payment, improvement programs such as the Comprehensive Primary Care initiative or patient‐centered medical homes, pay for performance, capitated contracts, Medicare ACOs, Medicaid ACOs, and commercial ACOs. As a measure of expectations for future exposure, we used a single‐item measure of the proportion of patients the respondent anticipated being covered by accountable care models in five years (responses dichotomized to None/Some and Most/All).
Practice Capacity for Innovation
We used NSHOS survey responses to generate four measures of practice capacity for innovation: (1) innovation culture (5‐item scale), (2) barriers to adopting care delivery innovations (6‐item scale), (3) advanced data system capacity (7‐item scale), and (4) whether the practice had a system in place to keep up with evidence (single item). Details of scales are provided in the online Appendix.
Focus of Practice on Low‐Income Patient Population
To ascertain underlying social risk of practices’ patient population we used NSHOS survey items indicating whether the practice was an FQHC or “FQHC look‐alike” and the share of the practice's revenue from Medicaid, categorized as none, low (<30%), or high (30% or higher). We chose 30% as the threshold for high share of practice revenue from Medicaid as this cutoff has been used in prior studies that examine relationships between Medicaid revenue and adoption of care processes by physician practices. 16
Covariates
Additional NSHOS survey items were obtained to measure other practice characteristics shown in prior work to influence adoption of different types of care delivery innovations, including practice ownership, practice size, and geographic region. 17
Analysis
We began by generating descriptive statistics and examining unadjusted associations between dependent variables and independent variables. To facilitate interpretation, we converted scores on all scale‐based independent variables to quartiles. Next, we used multivariable linear regression analysis to model associations among the number of social risks screened by a practice, exposure to value‐based payment, and practices’ capacity for innovation, adjusting for covariates. We used a successive‐model‐building approach, beginning with a model including only the covariates, then adding measures of value‐based payment exposure, and finally adding the measures of practices’ capacity for innovation. We conducted two subanalyses to test the robustness of our findings to alternative specification of the dependent and independent variables. First, instead of operationalizing value‐payment exposure as a continuous scale, we included dichotomous variables for each of the value‐based payments together in a single model. Second, rather than modeling the dependent variable as the total number of social risks screened, we used logistic regression analyses to model the odds of screening for each of the 7 social risks separately.
All models were weighted to reflect the national population of physician practices that have 3 or more primary care physicians. Weights adjust for the stratified sampling design of the NSHOS survey as well as practice characteristics associated with survey nonresponse. Stata 14 was used for all analyses.
Results
On average, physician practices reported systematically screening for 2.4 out of 7 (34%) social risks assessed by the survey. About 13% of practices screened for all 7 risks, while 23% of practices screened for none. In terms of key exposures, about 89% of practices reported participating in any type of value‐based payment model. Pay for performance was the most commonly reported, with 65% of practices participating. Looking to the future, 43% of practices anticipated most or all revenue to come from accountable care in five years. Of practices in our sample, 14% were FQHCs and 22% derive a high share (>30%) of practice revenue from Medicaid. Nearly half of practices were owned by a hospital or health system. See additional characteristics in Table 1.
Table 1.
Characteristics of 2,178 Physician Practices in Sample
| Unweighted | |||
|---|---|---|---|
| Freq/Mean | %/SD | ||
| Mean number social risks screened by practice | 2.4 | 34.0 | |
| Practice is FQHC/look‐alike | 314 | 14.3 | |
| Medicaid revenue | None | 288 | 13.2 |
| Low Medicaid (<30%) | 1,423 | 65.0 | |
| High Medicaid (≥30%) | 479 | 21.9 | |
| Value‐based payment reform exposure scale * | 42.6 | 27.6 | |
| Payment reforms | Bundled payments | 584 | 26.7 |
| Improvement programs | 1,227 | 56.0 | |
| Pay for performance | 1,426 | 65.1 | |
| Capitated contracts | 1,001 | 45.7 | |
| Medicare ACO | 1,100 | 50.2 | |
| Medicaid ACO | 750 | 34.3 | |
| Commercial ACO | 961 | 43.9 | |
| Anticipated accountable care in 5 years | None/Some | 1,260 | 57.5 |
| Most/All | 930 | 42.5 | |
| Innovation culture scale * | 53.0 | 21.4 | |
| Innovation barriers scale * | 55.1 | 29.5 | |
| Advanced data systems scale * | 54.5 | 21.5 | |
| System for evidence | 981 | 44.8 | |
| Practice ownership | Hospital or system | 1,158 | 52.9 |
| Larger physician group | 267 | 12.2 | |
| Independent | 612 | 28.0 | |
| Other | 153 | 7.0 | |
| Practice size | 0‐3 physicians | 539 | 24.6 |
| 4‐7 physicians | 845 | 38.6 | |
| 8‐12 physicians | 331 | 15.1 | |
| 13‐19 physicians | 167 | 7.6 | |
| 20+ physicians | 308 | 14.1 | |
| Region (census) | West | 548 | 25.0 |
| Midwest | 631 | 28.8 | |
| Northeast | 433 | 19.8 | |
| South | 578 | 26.4 | |
Abbreviations: ACO, accountable care organization; FQHC, Federally Qualified Health Center; SD, standard deviation.
Scale variables marked with an asterisk (*) are composite scales calculated from multiple survey items. In all cases, scale scores can range from 0 to 100.
In analyses adjusted only for basic practice characteristics (ownership, size, and region) and underlying social risk of the patient population (FQHC status and Medicaid revenue), practices in the highest quartile of value‐based payment participation screened for an additional 0.47 social risks (p = 0.017) compared with practices in the lowest quartile of value‐based payment participation. Practices expecting most or all of their patients to be covered by accountable care models in the future screened for 0.46 more social risks (p = 0.001) than practices expecting some or none of their patients to be covered by such contracts. These results are shown in Table 2.
Table 2.
Association Between Social Needs Screening and Practices’ Focus on Low‐Income Populations, Exposure to Value‐Based Payment, and Capacity for Innovation (Weighted)
| Model 1: Adjusted for Value‐Based Payment Exposure Only | Model 2: Also Adjusted for Practice Capacity for Innovation | ||
|---|---|---|---|
| Unadjusted (Bivariate) Associations | Coefficient | Coefficient | |
| FQHC status | |||
| Not FQHC | Ref | Ref | Ref |
| FQHC | 1.66*** | 1.28*** | 1.08*** |
| Medicaid revenue | |||
| None | Ref | Ref | Ref |
| Low | 1.05*** | 0.93*** | 0.87*** |
| High | 1.72*** | 1.27*** | 1.10*** |
| Payment reform index | |||
| Quartile 1 | Ref | Ref | Ref |
| Quartile 2 | 0.05 | −0.07 | −0.09 |
| Quartile 3 | 0.34 | 0.25 | 0.12 |
| Quartile 4 | 0.71*** | 0.47* | 0.16 |
| Anticipated accountable care in 5 years | |||
| None or Some | Ref | Ref | Ref |
| Most or All | 0.57*** | 0.46*** | 0.40** |
| Innovation culture | |||
| Quartile 1 | Ref | Ref | |
| Quartile 2 | 0.67*** | 0.42* | |
| Quartile 3 | 1.15*** | 0.64*** | |
| Quartile 4 | 1.82*** | 1.00*** | |
| Innovation barriers | |||
| Quartile 1 | Ref | Ref | |
| Quartile 2 | −0.56** | −0.3 | |
| Quartile 3 | −1.04*** | −0.69*** | |
| Quartile 4 | −1.83*** | −0.98*** | |
| System for evidence | |||
| No | Ref | Ref | |
| Yes | 0.93*** | 0.47** | |
| Advanced data systems | |||
| Quartile 1 | Ref | Ref | |
| Quartile 2 | 0.38* | 0.18 | |
| Quartile 3 | 0.65** | 0.34* | |
| Quartile 4 | 1.58*** | 0.95*** | |
| Observations | 2,178 | 2,178 | 2,178 |
Abbreviation: FQHC, Federally Qualified Health Center.
* p < 0.05, ** p < 0.01, *** p < 0.001.
The dependent variable in all models is the number of social risks systematically screened by the practice. The number of social risks can range from 0 to 7, representing the total number of risks screened from food insecurity, housing instability, utility needs, interpersonal violence, transportation needs, need for financial assistance with medical bills, and Medicaid eligibility. Other variables included in the adjusted model (but not shown here) were practice ownership, practice size, and geographic region.
The association between current participation in value‐based payment models and social risk screening was no longer significant after adding measures of practice capacity for innovation. The fully adjusted model revealed that all four of our measures of practice capacity for innovation were associated with social risk screening (results in Table 2 and Figure 1). Being in the top quartile on the three innovation capacity scales was associated with screening for 0.95 to 1.00 additional social risk (p < 0.001 for all three results) relative to the bottom quartile. Having a system in place to keep up with evidence was associated with screening for 0.47 additional social risks (p = 0.001). Although practices’ current participation in value‐based payment was not associated with social risk screening in the adjusted models, expectations about future payment were. Practices expecting most or all of their patients would be covered by contracts with total cost of care accountability in five years screened for 0.40 more social risks (p = 0.002) than practices expecting some or none of their patients to be covered by such contracts.
Figure 1.
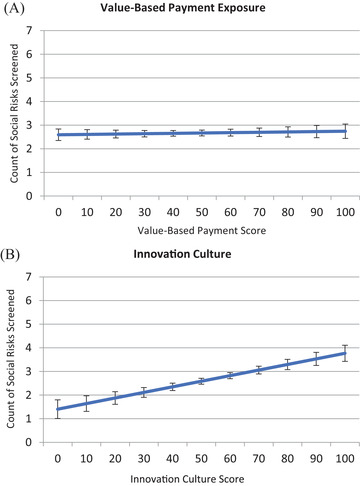
Margin Plots Depicting Adjusted Association of Value‐Based Payment Exposure and Innovation Culture With Social Risk Screening [Color figure can be viewed at wileyonlinelibrary.com]
These panels, based on the multivariable analyses presented in Table 2, show adjusted relationships between the number of social needs screened by a physician practice and select variables of interest. Panel A illustrates the nonsignificant relationship between greater exposure to value‐based payment models and social risk screening. Panel B illustrates the significant, positive association between practice scores on the innovation culture scale and social risk screening. Social risk screening also showed a significant, positive relationship with our other three measures of practice capacity for innovation as well, namely, scales measuring barriers to care delivery innovation and advanced health data system capacity, and the single‐item measure of having a system in place to keep up with evidence.
We examined individual payment models in subanalyses in order to see whether our scale of exposure to value‐based payment might have obscured differences among specific payment models. Participating in a Medicaid ACO was associated with screening for 0.37 more social risks (p = 0.015). No other payment models were associated with increased screening, although participating in a Medicare ACO was associated with screening for fewer social risks (Figure 2 and Table A2 in the online Appendix). In our subanalyses that examined screening for each of the 7 social risks in separate logistic regression models—rather than the total number of risks included in social screening—current participation in value‐based payment models was not associated with increased screening for any of the individual social risks (Table A3 in the online Appendix). Anticipating most or all revenue from accountable care in the future was associated with greater odds of screening for food insecurity, housing instability, utility needs, and interpersonal violence. With just a few exceptions, almost all measures of higher practice capacity for innovation were associated with greater likelihood of screening for each individual social risk.
Figure 2.
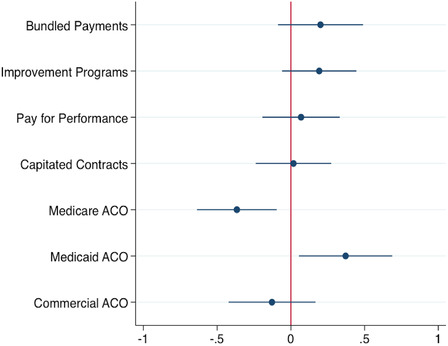
Adjusted Association of Participation in Specific Value‐Based Payment Models With Number of Social Risks Screened [Color figure can be viewed at wileyonlinelibrary.com]
Abbreviation: ACO, accountable care organization.
This figure depicts associations between individual payment reforms and number of social risks screened. Dots represent the estimated coefficient for each payment reform, with lines representing 95% confidence intervals. Only the coefficients for participation in individual payment reforms are shown here, but the fully adjusted and weighted regression model included practice ownership, size, region, Federally Qualified Health Center status, Medicaid revenue, anticipated accountable care in five years, and scales for innovation culture, innovation barriers, having a system for evidence, and advanced data system capacity.
Discussion
Health care stakeholders—including academics and health policy thought leaders—have expressed optimism that the spread of value‐based payment models will encourage providers to consider approaches to improve health outcomes through attention to social dimensions of health. 4 , 18 Our results indicate that implementation of social risk screening—an initial step in enhancing awareness of social needs—is not associated with overall exposure to value‐based payment for physician practices. Instead, social risk screening is being implemented by practices with high capacity for innovation and in practices serving patient populations likely to face social risks, regardless of payment incentives. We do find that expectations about future exposure to accountable care may play a role in practice decisions to implement social risk screening, but the magnitude of this association is considerably lower than the association with innovative capacity. Examining the role of specific payment reforms in subanalyses supported the interpretation that practice capacity for innovation, rather than payment incentives, is the primary driver of social risk screening. The only value‐based payment mechanism associated with increased screening was participation in a Medicaid ACO. That association may stem from some state Medicaid programs’ explicit requirements 19 as opposed to cost‐of‐care incentives. Participation in a Medicare ACO was associated with reduced social risk screening.
The lack of association with value‐based payment exposure at this stage—and dependence on organizational innovation capacity—has important implications for efforts to leverage social care to improve health. First, physician practices currently participating in more value‐based payment programs are not more likely to screen for social risks once capacity for innovation is considered. In other words, incentives in today's value‐based payment models do not generally appear sufficient to encourage practices to initiate the screening activities that are typically a first step toward addressing health‐related social needs.
Second, standardized approaches and implementation assistance may be needed to lower the bar on innovative capacity required to introduce social risk screening at the practice level. Experiences in Oregon, which introduced Medicaid flexibility to spend on social determinants of health in 2012, suggest that too much flexibility around initiatives to address social needs can be paralyzing. In the face of uncertainty about what types of social services were considered health‐related, some coordinated care organizations did not fully use the new spending flexibility, leading the state to introduce more specific definitions of health‐related services in 2017. 20
Third, individual physician practices may not be in a position to independently adopt social risk screening given the association between screening and advanced electronic health records and data systems. Affiliation with larger health systems may be important to help practices access emerging electronic health record–based tools for social risk screening.
Fourth, physician practices seeking to optimize performance under value‐based payment may be waiting for further evidence to decide whether screening patients for social risks and intervening to support social needs represents a strategy for success under these payment models. The most recent intervention studies on this topic have shown mixed results depending on the intervention and targeting strategies. 3 , 21 , 22 , 23 Larger managed care organizations and integrated health systems have the scale and analytic capacity to pilot and evaluate the impact of social needs assistance strategies internally, but individual physician practices rarely do. Thus, accumulation of further published evidence regarding impacts of interventions to address social needs is likely to be particularly important to inform adoption decisions among physician practices.
Limitations
Our results should be interpreted in light of study limitations. First, our analysis represents cross‐sectional associations and therefore cannot be used to infer causality. However, we adjust for many potential confounding variables and believe that our results make a valuable contribution in an area where evidence is lacking. Second, survey nonresponse could influence generalizability of our findings, although we were able to mitigate this impact by using nonresponse weights. Third, reliance of the NSHOS on a single survey respondent to represent each practice could introduce misclassification bias, particularly for measures of innovation capacity, which rely on some personal judgment. Such challenges to reliability would likely bias results toward the null, however, suggesting that the highly significant associations involving these measures in our analyses are more likely to underestimate the relationship between innovation capacity and implementation of social risk screening.
Future Directions
In considering the design of future value‐based payment incentives, it is also important to address the potential for divergent impacts on practices where low‐income patients are concentrated versus practices serving a broader range of income groups. Investing in systems for social risk screening could benefit FQHCs and other practices primarily serving lower‐income patients, and our results do show that such practices are implementing more social risk screening. At the same time, practices not primarily serving low‐income patients may decline to invest in developing these types of supports, leading to greater differentiation in the ability of practices to identify and respond to health‐related social needs.
In summary, our results add to the small but growing evidence base characterizing the adoption of social care strategies in the US health care system. These findings build on earlier results documenting a relatively low prevalence of social risk screening among US physician practices and explore how value‐based payment and practice capacity for innovation appear to influence patterns of adoption. Monitoring organizational efforts to address patients’ social needs can shed light on how value‐based payment reforms influence adoption. This may also elevate other tools, such as support for practice innovation, that are necessary to improve health care for patients with unmet social needs.
Funding/Support: This work was supported in part by the Agency for Healthcare Research and Quality's (AHRQ's) Comparative Health System Performance Initiative under Grant # 1U19HS024075, which studies how health care delivery systems promote evidence‐based practices and patient‐centered outcomes research in delivering care. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of AHRQ.
Acknowledgments: We thank Hector Rodriguez and Stephen Shortell for support in study development and data acquisition for this research.
The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from IQVIA information services: OneKey subscription information services 2010‐2017, IQVIA Incorporated, all rights reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IQVIA Incorporated or any of its affiliated or subsidiary entities. AMA is the source for the raw physician data; statistics, tables, or tabulations were prepared by the authors using AMA Masterfile data.
Supporting information
Online Technical Appendix
References
- 1. Shier G, Ginsburg M, Howell J, Volland P, Golden R. Strong social support services, such as transportation and help for caregivers, can lead to lower health care use and costs. Health Aff (Millwood). 2013;32(3):544‐551. 10.1377/hlthaff.2012.0170. [DOI] [PubMed] [Google Scholar]
- 2. Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719‐729. 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 3. Schickedanz A, Sharp A, Hu YR, et al. Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi‐experimental study J Gen Intern Med. 2019;34(11):2382‐2389. Published online June 21, 2019. 10.1007/s11606-019-05123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bachrach D, Pfister H, Wallis K, Lipson M. Addressing Patients’ Social Needs: An Emerging Business Case for Provider Investment. New York, NY: The Commonwealth Fund; 2014. [Google Scholar]
- 5. Joynt Maddox KE. Financial incentives and vulnerable populations—will alternative payment models help or hurt? N Engl J Med. 2018;378(11):977‐979. 10.1056/NEJMp1715455. [DOI] [PubMed] [Google Scholar]
- 6. Lewis VA, Larson BK, McClurg AB, Boswell RG, Fisher ES. The promise and peril of accountable care for vulnerable populations: a framework for overcoming obstacles. Health Aff (Millwood). 2012;31(8):1777‐1785. 10.1377/hlthaff.2012.0490. [DOI] [PubMed] [Google Scholar]
- 7. National Academies of Sciences, Engineering, and Medicine . Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation's Health. Washington, DC: The National Academies Press; 2019. 10.17226/25467. [DOI] [PubMed] [Google Scholar]
- 8. Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw Open. 2019;2(9):e1911514‐e1911514. 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Horwitz LI, Chang C, Arcilla HN, Knickman JR. Quantifying health systems’ investment in social determinants of health, by sector, 2017–19. Health Aff (Millwood). 2020;39(2):192‐198. 10.1377/hlthaff.2019.01246. [DOI] [PubMed] [Google Scholar]
- 10. Billioux A, Verlander K, Anthony S, Alley D. Standardized Screening for Health‐Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. Washington, DC: National Academy of Medicine; 2017. https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf. Accessed July 29, 2020. [Google Scholar]
- 11. Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39(1):19 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Buitron de la Vega P, Losi S, Sprague Martinez L, et al. Implementing an EHR‐based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57:S133 10.1097/MLR.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 13. Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q. 1990;35(1):128‐152. 10.2307/2393553. [DOI] [Google Scholar]
- 14. LaForge K, Gold R, Cottrell E, et al. How 6 organizations developed tools and processes for social determinants of health screening in primary care: an overview. J Ambul Care Manage. 2018;41(1):2‐14. 10.1097/JAC.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. About NSHOS . Comparative Health System Performance website. https://sites.dartmouth.edu/coe/nshos/. Accessed October 18, 2019.
- 16. Rodriguez HP, McClellan SR, Bibi S, Casalino LP, Ramsay PP, Shortell SM. Increased use of care management processes and expanded health information technology functions by practice ownership and Medicaid revenue. Med Care Res Rev. 2016;73(3):308‐328. 10.1177/1077558715613233. [DOI] [PubMed] [Google Scholar]
- 17. Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289(4):434‐441. 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 18. Shortell SM. Bridging the divide between health and health care. JAMA. 2013;309(11):1121‐1122. 10.1001/jama.2013.887. [DOI] [PubMed] [Google Scholar]
- 19. Addressing social determinants of health through Medicaid accountable care organizations . Center for Health Care Strategies website. https://www.chcs.org/addressing-social-determinants-health-medicaid-accountable-care-organizations/. Published April 18, 2018. Accessed October 21, 2019.
- 20. Kushner J, McConnell KJ. Addressing social determinants of health through Medicaid: lessons from Oregon. J Health Polit Policy Law. 2019;44(6):919‐935. 10.1215/03616878-7785823. [DOI] [PubMed] [Google Scholar]
- 21. Berkowitz SA, Terranova J, Hill C, et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018;37(4):535‐542. 10.1377/hlthaff.2017.0999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kangovi S, Mitra N, Grande D, Long JA, Asch DA. Evidence‐based community health worker program addresses unmet social needs and generates positive return on investment. Health Aff (Millwood). 2020;39(2):207‐213. 10.1377/hlthaff.2019.00981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Finkelstein A, Zhou A, Taubman S, Doyle J. Health care hotspotting—a randomized, controlled trial. N Engl J Med. 2020;382(2):152‐162. 10.1056/NEJMsa1906848. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Technical Appendix


