Abstract
Purpose:
Clinical trials are necessary to test HIV-prevention strategies among adolescent girls and young women in sub-Saharan Africa. Psychosocial risk factors that increase girls’ and young women’s vulnerability for HIV may also impact their experiences in clinical trials. A better understanding of psychosocial risks among girls and young women enrolled in HIV-prevention research is needed. This analysis explores depression and sexual trauma among adolescent girls and young women enrolled in a mock microbicide trial in Tanzania.
Methods:
We collected cross-sectional data from 135 HIV-negative adolescent girls and young women between 15–21 in Dar es Salaam, Tanzania enrolled in a mock microbicide trial. Depression, sexual behavior, and sexual trauma were measured. Sexual trauma and demographic variables were entered into a multivariate binomial logistic regression model predicting depression.
Findings:
Overall, 27% of participants had moderate-to-severe depression. The most commonly endorsed items were anhedonia (lack of interest/pleasure) and low mood, which were reported by 78% of participants. Thoughts of suicide or self-harm were endorsed by 17% of participants. Coerced/forced first sex was reported by 42% of participants. Participants reporting coerced/forced first sex had 3.16 times the likelihood of moderate-to-severe depression.
Conclusions:
Depression and coerced/forced sex were common among participants in an HIV-prevention mock clinical trial in Tanzania. When enrolling adolescent girls and young women in HIV-prevention trials in sub-Saharan Africa, our research suggests the need for a trauma-informed approach, referrals for trauma and depression, and interventions that address the impact of depression and trauma on HIV prevention, clinical trial adherence, and clinical outcomes.
Keywords: mental health, depression, HIV, sexual trauma, clinical trials, Tanzania
Clinical trials to test biomedical HIV-prevention methods among adolescent girls and young women in sub-Saharan Africa are urgently needed (Hosek & Pettifor, 2019; Phillips & Mbizvo, 2016). Approximately 3.6% of 14- to-24-year-old girls across East and Southern Africa are infected with HIV (Brown et al., 2018). Rates of HIV are disproportionately high among adolescent girls and young women. HIV disparities are driven by multiple interacting psychosocial risks experienced by women and girls, such as high rates of sexual trauma and poor mental health, which are associated with HIV-infection and sexual risk behavior (Page & Hall, 2009; Pence et al., 2012; Spies, Konkiewitz, & Seedat, 2018; UNAID, 2014). Conducting clinical trials with young women and girls, a vulnerable population that encounters frequent psychosocial challenges, may present logistical and ethical barriers. For example, in addition to issues of parental consent and confidentiality, researchers must ensure adolescents understand experimental assignment and the benefits and harms of an intervention (Hosek & Zimet, 2010; Pack et al., 2019; Singh et al., 2006). Despite potential difficulties conducting research with adolescents, studies with adolescents are necessary to combat HIV among those most affected by the virus (Nelson, Lewis, Struble, & Wood, 2010; Pomfret, Karim, & Benatar, 2010).
To implement feasible, acceptable, and ethical clinical trials, researchers must investigate mental health and factors such as sexual trauma that could impact recruitment, retention, consent, adherence to intervention procedures, and clinical outcomes. However, little is known about depression or correlates between depression and sexual trauma among girls and young women in HIV-prevention trials in sub-Saharan Africa. For this reason, the present analysis focuses on depression and sexual trauma among girls and young women enrolled in a mock vaginal and oral microbicide trial in Tanzania.
Depression is a global problem that may impact girls and young women in HIV research. Globally, unipolar depressive disorders are the leading cause of disability among girls and women 10-to-24 years old (Gore et al., 2011). Prevalence estimates of clinical depression among adolescents in sub-Saharan Africa range from 36% to 37% (Closson et al., 2016; Neese, Pittman, & Hunemorder, 2013; Kuringe et al., 2019). Symptoms such as suicidal ideation and self-harm may require immediate referrals in clinical trials and are sometimes used as exclusion criteria in psychotherapy research (Fisher, Pearson, Kim, & Reynolds, 2002; Ronconi, Shiner, & Watts, 2014; Stirman, DeRubeis, Crits-Christoph, & Brody, 2003). However, evidence from research on antidepressants suggests excluding individuals with suicidal ideation or severe depression leads to a discrepancy between clinical trial samples and what is actually seen in clinical practice (Zimmerman, Chelminski, & Posternak, 2005). The potential impact of using mental health symptoms as exclusion criteria for HIV research warrants further investigation. Across populations, depression has been linked to poor HIV care engagement, poor healthcare utilization, and poor HIV medication adherence (Byakika-Tusiime et al., 2009; Ramirez-Avila et al., 2012). Treating depression leads to improvements in antiretroviral medication adherence (Sin & DiMatteo, 2014). This research highlights the possibility that depression may impact clinical trial participation and may be important to address. Lastly, depression is associated with increased sexual risk behaviors and poor clinical outcomes, which makes it an essential factor to consider when examining outcomes of HIV-prevention clinical trials (Ickovics JR, Hamburger ME, Vlahov D, & et al, 2001; Khan et al., 2009).
Forced and coerced sex are common among adolescent girls in sub-Saharan Africa, and trauma may impact HIV-related clinical trials (Closson et al., 2016; Lalor, 2004). Trauma has been linked to depression, poor adherence to HIV care, poor healthcare utilization, poor clinical health outcomes, increased sexual risk behavior, and worse health-related functioning (Closson et al., 2016; Kalichman & Simbayi, 2004; Mugavero et al., 2009; Pence et al., 2012; Raja et al., 2015; Siyahhan Julnes et al., 2016; Suliman et al., 2009). Although growing research shows the importance of gender issues and intimate partner violence on the implementation of pre-exposure prophylaxis and microbicides among women (Doggett et al., 2015), less is known about how past sexual trauma can impact participants when woman-controlled biomedical strategies, such as vaginal microbicides, are used in clinical trials. For these reasons, trauma may be relevant to clinical trial participation.
Objectives
Despite the potential for depression and sexual trauma to impact clinical trials, less is known about the prevalence of these issues or the interrelationship between these factors among HIV-negative adolescent girls and young women in sub-Saharan Africa who would agree to take part in a biomedical HIV-prevention trial. The present analysis of cross-sectional data fills this gap by exploring depression symptoms and the relationship between depression and sexual trauma among girls and young women enrolled in a mock microbicide trial in Tanzania.
Method
Participants
We collected self-report, cross-sectional baseline data from adolescent girls (15–17 years old) and young women (18–21 years old) in Dar es Salaam, Tanzania who were enrolled in a mock microbicide trial. Methods for the mock trial have been previously described (Baumgartner et al., 2015; Tolley et al., 2014). Enrollment criteria included reporting sexual activity in the last three months, not being currently pregnant, and being HIV-negative. Convenience sampling was used with the aim of recruiting participants who would be likely to take part in a real microbicide trial. Recruitment occurred in a range of settings, including youth-focused clinics, schools, other organizations, and public areas where adolescents are known to frequent. Word of mouth and written study brochures were used.
Protection of Human Subjects
Ethical approval was granted by the National Institute for Medical Research (NIMR) and Muhimbili University of Health and Allied Sciences (MUHAS) in Tanzania and FHI 360’s Protection of Human Subjects Committee. Participants who were 15 years old provided written assent with parental consent, and participants older than 15 years old provided written informed consent to take part in the study.
Mental health professionals were available to address suicidality and depression and follow-up with participants as needed.
Procedure
From 2011–2013, we collected quantitative data via interview in Swahili at the Infectious Disease Clinic (IDC) in Dar es Salaam, Tanzania, which provided adolescent-friendly health services. All data collection was completed by Swahili-speaking female research assistants with at least a bachelor’s degree. Because the parent study was focused on ethical and legal issues working with adolescents, all staff were trained in the special conduct of research with adolescents (Baumgartner et al., 2015; Tolley et al., 2014). Research was conducted in a private location either at the clinic or in the participant’s home, if requested. Interviews took approximately one hour.
Measures
The measures in the present analysis were part of a larger battery of items exploring psychosocial factors among adolescent girls and young women enrolled in a mock microbicide HIV-prevention trial. Per the World Health Organization’s recommended translation and adaptation process, the local study team conducted forward and back translations of the psychosocial scales to finalize the survey in Swahili, and scales were pre-tested with adolescent girls (World Health Organization, n.d.).
Depression.
Depression was measured using the Patient Health Questionnaire – 9, a brief, self-administered measure of depression severity (Kroenke, Spitzer, & Williams, 2001). The PHQ-9 has been previously used in East Africa and among adolescents in Tanzania and high-income settings and has shown good reliability and validity (Dow et al., 2016; Gelaye et al., 2013; Monahan et al., 2009; Richardson et al., 2010). In the PHQ-9, participants were asked how often they had been bothered by a series of problems over the last two weeks. Responses could range from 0 = not at all to 3 = nearly every day. Symptoms included (1) little interest or pleasure in doing things; (2) feeling down, depressed or hopeless; (3) trouble falling asleep or staying asleep, or sleeping too much; (4) feeling tired or having little energy; (5) poor appetite or overeating; (6) feeling bad about yourself - or that you are a failure or have let yourself or your family down; (7) trouble concentrating on things, such as reading the newspaper or watching television; (8) moving or speaking so slowly that other people could have noticed, or the opposite - being so fidgety or restless that you have been moving around a lot more than usual; and (9) thoughts that you would be better off dead, or of hurting yourself in some way. A final question asked about the difficulty of functioning due to these problems, with responses ranging from “not difficult at all” to “extremely difficult.” A summary score was computed for the nine symptoms of depression, with a score of 1–4 indicating minimal depression, 5–9 indicating mild depression, 10–14 indicating moderate depression, 15–19 indicating moderately severe depression, and 20–27 indicating severe depression (Kroenke et al., 2001). A dichotomous variable was computed for whether a participant had none-to-mild depression (0–9) or moderate-to-severe depression (10–27). The cut-off of 10 or more has been shown to be the most optimal for accurately diagnosing clinical depression among adults in East Africa and Nigeria, although research with adolescents in high-income settings has provided conflicting findings on whether a cut-off of 8 or 11 provides a better balance of sensitivity and specificity (Adewuya, Ola, & Afolabi, 2006; Gelaye et al., 2013; Richardson et al., 2010).
Demographics.
Participants were asked about their religion, age, highest level of schooling completed, education and employment status, and whether one or both biological parents are still alive.
Sexual behaviors and sexual trauma.
Participants were asked to report on their marriage status, whether they have ever been pregnant, whether they have ever been diagnosed or had the self-reported symptoms of a reproductive tract infection, whether they have ever used contraceptives, the age of their first and current sexual partner(s), and age of sexual debut. Variables were computed to examine if their current or first partners were five or more years older than the participant. Participants were asked how willing they were to have sex for the first time, with the options of willing/wanted, persuaded/coerced, or physically forced/raped. They were also asked this question for the last time they had sex. For analysis, the category of persuaded/coerced was collapsed with physically forced/raped, to create a dichotomous variable of either 1) willing/wanted or 2) coerced/forced.
Statistical Analyses
We completed all statistical analyses using SPSS 25. We examined frequencies and distributions for overall depression severity and responses to individual questions on the PHQ-9. We computed Chronbach’s alpha for the PHQ-9 total score. We conducted separate univariate binomial logistic regressions for all predictor variables, with depression severity included as a dichotomous outcome, where scores of 0–9 indicated none-to-mild depression and scores of 10–27 indicated moderate-to-severe depression. Key demographic variables and those variables that were significant in the univariate models at p < .05 were included in a final multivariate model, with all predictors entered into the binomial logistic regression model simultaneously using the standard selection method. Because first sex coerced/forced was a significant predictor of depression severity, we conducted chi-square tests, Fisher’s exact tests, and univariate ANOVAs to explore demographic characteristics of participants who reported coerced/forced first sex compared to participants whose first sex was willing/wanted. P-values were set to .05, and 95% confidence intervals are reported throughout. Missing data was minimal and was handled using listwise deletion, which excludes cases with missing data.
Results
The final sample included 135 adolescent girls and young women. Demographic information can be found in Table 1.
Table 1.
Demographic Characteristics
| Variable | M (SD) |
|---|---|
| Age | 18.38 (1.634) |
| Religion | % (n) |
| Muslim | 53.3 (72) |
| Catholic | 35.6 (48) |
| Protestant | 8.9 (12) |
| Education | |
| Some Primary | 5.2 (7) |
| Completed Primary | 37 (50) |
| Some Secondary School | 57 (77) |
| Secondary or Post-Secondary School | 7 (1) |
| Employment | |
| Not Attending School & Unemployed | 52.6 (71) |
| Student | 19.3 (26) |
| Paid Employment | 28.1 (38) |
| Had prior Pregnancy | 33.3 (45) |
| Married | 4.4 (6) |
| Last Sexual Encounter Coerced/Forced | 7.4 (10) |
| First Sexual Encounter Coerced/Forced | 42.2 (57) |
M = Mean, SD = Standard Deviation
Frequency and distribution outcomes for depression severity and responses to individual symptoms of depression are reported in Table 2. Overall, 27% of participants met the criteria for moderate-to-severe depression with a score of 10 or above on the PHQ-9. The mean PHQ-9 score of 7.87 falls into the “mild depression” range.
Table 2.
Endorsement of Depression Symptoms and Depression Severity among Adolescents Ages 15–21 Participating in a Mock Clinical Trial in Dar es Salaam, Tanzania
| Variable | Descriptive Statistics |
|---|---|
| Depression Severity | % (n) |
| None/Minimal (0–4) | 17.77 (24) |
| Mild (5–9) | 54.81 (74) |
| Moderate (10–14) | 22.22 (30) |
| Moderately Severe (15–19) | 4.44 (6) |
| Severe (20–27) | 74 (1) |
| Mean PHQ-9 Total Score | 7.87 (SD = 4.06; range = 0–24, α = .64) |
| Little interest or pleasure | M = 1.20 (SD = .98) |
| Not at all (0) | 22.22 (30) |
| Several days (1) | 55.55 (75) |
| More than half the days (2) | 4.44 (6) |
| Nearly every day (3) | 17.77 (24) |
| Feeling down, depressed or hopeless | M = 1.02 (SD = .74) |
| Not at all (0) | 21.48 (29) |
| Several days (1) | 60.74 (82) |
| More than half the days (2) | 11.85 (16) |
| Nearly every day (3) | 5.18 (7) |
| Trouble sleeping or sleeping too much | M = 1.06 (SD = .93) |
| Not at all (0) | 28.88 (39) |
| Several days (1) | 49.62 (67) |
| More than half the days (2) | 9.62 (13) |
| Nearly every day (3) | 11.85 (16) |
| Feeling tired or having little energy | M = 1.08 (SD = .85) |
| Not at all (0) | 22.96 (31) |
| Several days (1) | 54.07 (73) |
| More than half the days (2) | 14.07 (19) |
| Nearly every day (3) | 8.82 (12) |
| Poor appetite or overeating | M = .94 (SD = .86) |
| Not at all (0) | 30.37 (41) |
| Several days (1) | 52.59 (71) |
| More than half the days (2) | 6.66 (9) |
| Nearly every day (3) | 8.88 (12) |
| Feeling bad about yourself | M = .67 (SD = .72) |
| Not at all (0) | 43.70 (59) |
| Several days (1) | 48.14 (65) |
| More than half the days (2) | 5.18 (7) |
| Nearly every day (3) | 2.96 (4) |
| Trouble concentrating | M = .61 (SD = .89) |
| Not at all (0) | 59.25 (80) |
| Several days (1) | 27.40 (37) |
| More than half the days (2) | 6.66 (9) |
| Nearly every day (3) | 6.66 (9) |
| Moving too slowly or a lot | M = .64 (SD = .89) |
| Not at all (0) | 56.29 (76) |
| Several days (1) | 32.59 (44) |
| More than half the days (2) | 2.96 (4) |
| Nearly every day (3) | 8.14 (11) |
| Thoughts you might be better off dead, or of hurting yourself | M = .24 (SD = .63) |
| Not at all (0) | 82.96 (112) |
| Several days (1) | 11.85 (16) |
| More than half the days (2) | 2.22 (3) |
| Nearly every day (3) | 2.96 (4) |
| Difficulties Doing Activities Due to Problems | |
| Not difficult at all | 60 (81) |
| Somewhat difficult | 33.33 (45) |
| Very difficult | 2.22 (3) |
| Extremely difficult | 2.22 (3) |
M = Mean, SD = Standard Deviation
The most commonly endorsed items were “little interest or pleasure in doing things” and “feeling down, depressed, or hopeless.” For each of these items, 78% of participants responded at least “several days” or more. The least commonly endorsed item was “thoughts you might be better off dead, or of hurting yourself,” which was endorsed by 17% of participants. Of the 98 participants with no/minimal or mild depression, 8% (n = 8) endorsed suicidality or thoughts of self-harm several days, and 2% (n = 2) reported suicidality or thoughts of self-harm more than half of the days. Figure 1 shows mean scores on each of the nine PHQ-9 items.
Figure 1. Mean Score on Individual PHQ-9 Items.
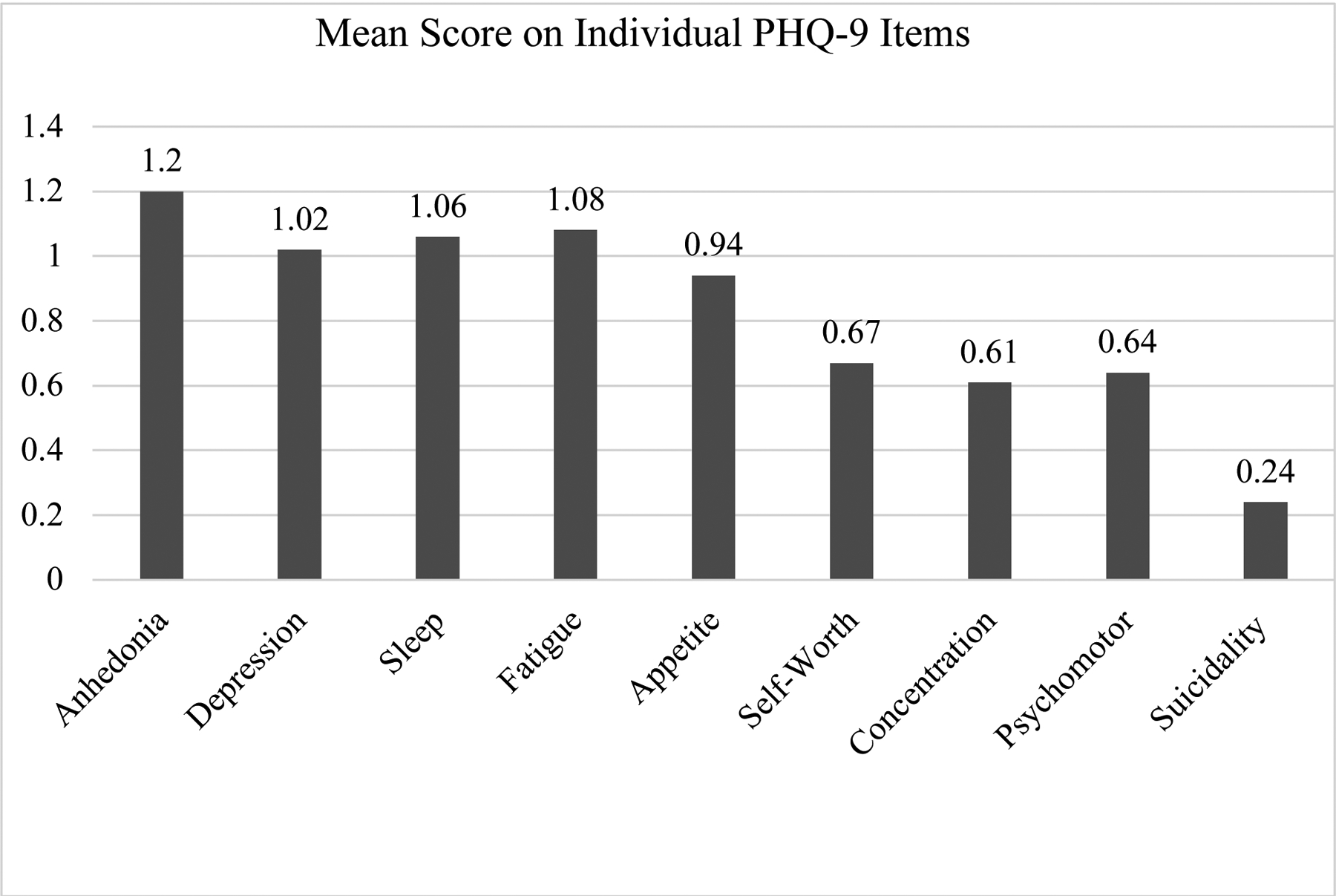
Mean scores on items 1–9 of the Patient Health Questionnaire – 9, a measure of depression symptoms. Scores for individual items could range from 0–3.
Results from the series of univariate binomial logistic regression models can be found in Table 3. Of the predictive variables, only first sex coerced/forced was a statistically significant predictor of depression, with participants having a coerced/forced first sexual experience being 3.09 times more likely to have moderate-to-severe depression, X2 (1, N = 135) = 8.26, p = .004). Highest year of school completed trended on significance (p = .083), with higher years of school predicting smaller likelihood of moderate-to-severe depression.
Table 3.
Bivariate Logistic Regression Models Predicting Moderate-to-Severe Depression
| Variable(s) | % (n) within variable category | OR | 95% CI | P | |
|---|---|---|---|---|---|
| None-Mild Depression | Moderate-Severe Depression | ||||
| Age | M = 18.31 | M = 18.57 | 1.10 | .87, 1.40 | .406 |
| Highest year school | M = 8.98 | M = 8.30 | .85 | .70, 1.02 | .083 |
| Student status | 2.39 | .76, 7.48 | .135 | ||
| Current Student | 85 (22) | 15 (4) | |||
| Non-Student | 70 (76) | 30 (33) | |||
| Age at first sex | M = 15.96 | M = 15.84 | .95 | .76, 1.21 | .695 |
| Age of current/last partner | 1.03 | .45, 2.35 | .951 | ||
| < 5 years older | 73 (51) | 27 (19) | |||
| 5+ years older | 72 (34) | 28 (13) | |||
| Marriage Status | 2.79 | .54, 14.51 | .222 | ||
| Never Married | 74 (95) | 26 (34) | |||
| Currently? Married | 50 (3) | 50 (3) | |||
| Pregnancy History | 1.12 | .50, 2.48 | .785 | ||
| Never Pregnant | 73 (66) | 27 (24) | |||
| Ever//current? Pregnant | 71 (32) | 29 (13) | |||
| Contraceptive Use History | .57 | .24, 1.40 | .224 | ||
| Never Used | 63 (17) | 37 (10) | |||
| Ever Used | 75 (80) | 25 (27) | |||
| RTI History | 2.06 | .82, 5.17 | .126 | ||
| No RTI history | 76 (74) | 25 (24) | |||
| Had RTI | 60 (15) | 40 (10) | |||
| Orphan Status | 1.31 | .61, 2.83 | .489 | ||
| Both parents alive | 75 (62) | 25 (21) | |||
| 1 or both parents died | 69 (36) | 31 (16) | |||
| Age of First Sex Partner | 2.02 | .59, 6.68 | .260 | ||
| < 5 years older | 74 (82) | 26 (29) | |||
| 5+ years older | 58 (7) | 42 (5) | |||
| Relationship Status | 1.86 | .49, 7.00 | .360 | ||
| Has Partner | 74 (92) | 26 (33) | |||
| Single | 60 (6) | 40 (4) | |||
| Last Sex Forced | 2.91 | .79, 10.70 | .109 | ||
| Willing/wanted | 74 (93) | 26 (32) | |||
| Coerced/forced | 50 (5) | 50 (5) | |||
| First Sex Forced* | 3.09 | 1.41, 6.77 | .005* | ||
| Willing/wanted | 82 (64) | 18(14) | |||
| Coerced/forced | 60 (34) | 40 (23) | |||
Percents are rounded to the nearest whole value,
= P < .05
The four-predictor model including age, highest year in school, relationship status, and first sex forced significantly predicted whether an individual had moderate-to-severe depression, X2 (4, N = 135) = 12.611, p = .013). Partial regression coefficents, standard errors, the Wald test, odds ratios, and confidence intervals are presented in Table 4. Nagelkerke pseudo R2 suggests the model accounts for about 13% of the variance in depression. With a classification cutoff value of .500, 72.6% of cases were correctly predicted, although rates varied by outcome, with 93.9% of individuals in the none-to-mild group predicted correctly and 16.2% of individuals in the moderate-to-severe group predicted correctly. When controlling for other variables in the model, first sex coerced/forced predicted depression, with participants reporting a coerced/forced first sexual experience having 3.16 times the likelihood of moderate-to-severe depression compared to participants whose first sex was willing/wanted. All else held constant, highest year of school completed trended toward significant association with depression; for a year increase in the highest year of school completed, participants had .82 times the likelihood of moderate-to-severe depression, indicating greater number of years in school may relate to lower likelihood of depression.
Table 4.
Final Multivariate Logistic Regression Model Predicting Moderate-to-Severe Depression
| Variable (n) | B | SE B | Wald | P | Adjusted OR | 95% CI |
|---|---|---|---|---|---|---|
| Age | .13 | .13 | 1.02 | .313 | 1.14 | .89, 1.46 |
| Highest Year School | −.20 | .10 | 3.68 | .055 | .82 | .67, 1.00 |
| Relationship Status | .02 | .71 | .00 | .975 | 1.02 | .25, 4.12 |
| First Sex Coerced/Forced | 1.15 | .42 | 7.63 | .006 | 3.16 | 1.40, 7.15 |
The dependent variable was depression categorization, with moderate-to-severe depression as the target category and none-to-mild depression as the reference category; girls without a regular partner were the focus of the Relationship Status variable; girls whose first sex was coerced/forced were the focus of the First Sex Forced variable.
Nagelkerke R2 = .13.
Overall, 42% of participants reported a coerced/forced first sexual experience. Those participants whose first sex was coerced/forced were not significantly different in age (p = .636), highest education level completed (p = .919), age at first sex (p = .503), or employment/student status (p = .517) compared to those whose first sex was willing/wanted. Eighty-six percent (86%) of participants whose first sex was coerced/forced were married or had a regular partner, whereas 97% of participants whose first sex was willing/wanted were married or had a regular partner, which shows a statistically significantly relationship between current relationship status and whether first sex was coerced/forced (Fisher’s Exact Test, Two-Sided = .018). Fourteen percent (14%) of participants whose first sex was coerced/forced reported that their last sexual experience was coerced/forced, compared to 2.6% of participants whose first sex was willing/wanted, which was statistically significant (Fisher’s Exact Test, Two-Sided = .018).
Conclusions for Practice
Secondary analyses were conducted on baseline data from a mock vaginal and oral microbicide trial among HIV-negative, non-pregnant, and sexually active adolescent girls and young women in Tanzania to examine depression symptoms and the relationships between depression and sexual trauma. Findings suggested concerning rates of moderate-to-severe depression (27%), thoughts of suicide and self-harm (17%), and forced/coerced first sexual experiences (42%). In both a univariate model and a multivariate model controlling for demographic variables, depression severity was predicted by first sex forced/coerced, with participants whose first sexual experience was forced being over 3 times more likely to have moderate-to-severe depression. A multivariate model including first sex forced/coerced and other demographic variables accounted for approximately 13% of the variance in depression severity.
Not every participant who reported thoughts of suicide or self-harm met the criteria for moderate-to-severe depression. Suicidality and completed suicide without major depression has been found in other studies and highlights the multiple causes of suicidal ideation (Rhodes & Bethell, 2008). In prior research, PHQ item 9, which asks about suicidality and self-harm, was a strong predictor of suicide attempts (Simon et al., 2013). For this reason, particular attention should be paid to responses on item 9 of the PHQ-9 when considering risk for suicide or self-harm. This consideration may be important to researchers who are choosing between the PHQ-2 and the PHQ-9. The PHQ-2 only includes the first two questions of the PHQ-9, which pertain to anhedonia and low mood. When we examined responses on just the first two items of the PHQ-9 using a cutoff score of 3 for “further screening recommended,” 28% of our sample would have met the criteria, which is only 1 point more than the 27% who had moderate-to-severe depression using all nine items of the PHQ-9 (Monahan et al., 2009). However, the risk for suicide among 10 participants would be missed when using just these two items. For this reason, researchers should carefully consider whether to add a separate question on suicidality when using the PHQ-2.
Our findings provide suggestions for researchers hoping to enroll HIV-negative adolescent girls and young women in clinical trials in sub-Saharan Africa. First, researchers should be aware of the significant rate of depression and sexual trauma in this group, be ready to provide referrals for care, and have an action plan for handling suicidality or cases where there is risk of imminent harm that follows local confidentiality laws, reporting requirements, and professional ethics codes while protecting the rights and well-being of participants. Ideally, same-day psychosocial counseling should be provided to high-risk individuals. The World Health Organization’s mhGAP Intervention Guide 2.0 for mental health disorders in non-specialized health settings provides assessment and management guides for depression and suicide that could be used as screening, referral, and treatment planning tools by both mental health professionals and non-specialists in clinic settings (World Health Organization, 2016).
When including participants who have experienced sexual trauma, a trauma-informed approach should be taken, particularly when research involves the vaginal delivery of microbicides or gynecological exams (Stadler, Delany-Moretlwe, Palanee, & Rees, 2014). Prior research on this sample showed high rates of familial violence, which also should be taken into consideration (Baumgartner et al., 2015). There is evidence for the effectiveness of trauma-informed HIV-related interventions both globally and in sub-Saharan Africa (Sales, Swartzendruber, & Phillips, 2016). However, there is a need for interventions that focus specifically on trauma and the use of intravaginal medications.
Although researchers may want to exclude individuals with depression, sexual trauma, or suicidal ideation from HIV-prevention trials, researchers should think about the implications for generalizability if they exclude these individuals, as the present study indicates this criteria would exclude a considerable percentage of potential participants.
Further research is needed on the impact of depression, sexual trauma, and the intersection of these two issues on clinical trial participation, understanding of consent, and adherence to biomedical interventions. Interventions that have a dual component to treat mental health issues in tandem with biomedical HIV prevention methods may be warranted.
Limitations
The present analysis was cross-sectional, so causality cannot be inferred, and it is possible that important confounding variables were not included in the model. However, forced/coerced first sex occurred in the past, whereas scores on the PHQ-9 referred to symptoms over the past 2 weeks, so forced/coerced first sex preceded current symptomology.
Our study was designed to focus on the unique population of girls and young women who would take part in a microbicide trial. As such, our findings are not generalizable to the entire population of girls and young women in Tanzania. Although our study included more Muslim participants than would be expected according to country-level demographics, we expect that our sample was more reflective of the demographic characteristics of Dar es Saalam (Anthony, 2002; Stark, 2018).
One limitation of the present analysis is that it was a secondary analysis, so although an a priori power analysis was conducted for the original mock trial outcomes, the sample size for the present analysis was pre-determined based on available data.
Internal reliability for the PHQ-9 was moderate, which was lower than previous studies (Monahan et al., 2009). We do not know whether the low reliability was due to cultural differences in the presentation of depression symptoms or another reason, although the measure was translated, back-translated, and pre-tested to ensure the items were understandable and relevant with adolescent girls and young women. One study from the United States did show that reliability could vary by ethnicity (Huang, Chung, Kroenke, Delucchi, & Spitzer, 2006). Future research that employs cognitive interviewing with the PHQ-9, factor analyses with larger samples, or repeated longitudinal administration of the PHQ-9 could be useful to understand the reliability of this measure among adolescent girls and young women in Tanzania (Drennan, 2003). Nevertheless, our finding that 27% of participants had moderate-to-severe depression is in line with previous research, which provides evidence for the validity of this measure (Closson et al., 2016).
Conclusions
This study provided evidence of high rates of depression among adolescent girls and young women enrolled in HIV-prevention research, which was associated with having a coerced/forced first sexual experience. By carefully considering the impact of depression and sexual trauma on girls and young women, we can more readily develop adolescent-friendly HIV-prevention clinical trials.
Significance.
Depression symptoms were common among girls and young women ages 15–21 enrolled in HIV-prevention research in Tanzania. Participants reporting coerced/forced first sex were more likely to experience moderate-to-severe depression. Both depression and sexual trauma are important to consider when enrolling adolescent girls and young women in HIV-prevention trials.
References
- Adewuya AO, Ola BA, & Afolabi OO (2006). Validity of the patient health questionnaire (PHQ-9) as a screening tool for depression amongst Nigerian university students. Journal of Affective Disorders, 96(1–2), 89–93. 10.1016/j.jad.2006.05.021 [DOI] [PubMed] [Google Scholar]
- Anthony DH (2002). Islam in Dar es Salaam, Tanzania. Studies in Contemporary Islam, 4(2), 21–40. [Google Scholar]
- Baumgartner JN, Kaaya S, Karungula H, Kaale A, Headley J, & Tolley E (2015). Domestic violence among adolescents in HIV prevention research in Tanzania: Participant experiences and measurement issues. Maternal and Child Health Journal, 19(1), 33–39. 10.1007/s10995-014-1492-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K, Williams DB, Kinchen S, Saito S, Radin E, Patel H, … Voetsch AC (2018). Status of HIV epidemic control among adolescent girls and young women aged 15–24 years—Seven african countries, 2015–2017. MMWR. Morbidity and Mortality Weekly Report, 67(1), 29–32. 10.15585/mmwr.mm6701a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byakika-Tusiime J, Crane J, Oyugi JH, Ragland K, Kawuma A, Musoke P, & Bangsberg DR (2009). Longitudinal antiretroviral adherence in HIV+ Ugandan parents and their children initiating HAART in the MCTC-plus family treatment model: Role of depression in declining adherence over time. AIDS and Behavior, 13(S1), 82–91. 10.1007/s10461-009-9546-x [DOI] [PubMed] [Google Scholar]
- Closson K, Dietrich JJ, Nkala B, Musuku A, Cui Z, Chia J, … Kaida A (2016). Prevalence, type, and correlates of trauma exposure among adolescent men and women in Soweto, South Africa: Implications for HIV prevention. BMC Public Health, 16(1). 10.1186/s12889-016-3832-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doggett EG, Lanham M, Wilcher R, Gafos M, Karim QA, & Heise L (2015). Optimizing HIV prevention for women: A review of evidence from microbicide studies and considerations for gender-sensitive microbicide introduction. Journal of the International AIDS Society, 18(1), 20536 10.7448/IAS.18.1.20536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dow DE, Turner EL, Shayo AM, Mmbaga B, Cunningham CK, & O’Donnell K (2016). Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care, 28(7), 825–833. 10.1080/09540121.2016.1139043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drennan J (2003). Cognitive interviewing: Verbal data in the design and pretesting of questionnaires. Journal of Advanced Nursing, 42(1), 57–63. 10.1046/j.1365-2648.2003.02579.x [DOI] [PubMed] [Google Scholar]
- Fisher CB, Pearson JL, Kim S, & Reynolds CF (2002). Ethical issues in including suicidal individuals in clinical research. IRB: Ethics & Human Research, 24(5), 9–14. [PubMed] [Google Scholar]
- Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, … Andrew Zhou X-H (2013). Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Research, 210(2), 653–661. 10.1016/j.psychres.2013.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, … Mathers CD (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. The Lancet, 377(9783), 2093–2102. 10.1016/S0140-6736(11)60512-6 [DOI] [PubMed] [Google Scholar]
- Hosek SG, & Zimet GD (2010). Behavioral considerations for engaging youth in HIV clinical research. JAIDS Journal of Acquired Immune Deficiency Syndromes, 54, S25–S30. 10.1097/QAI.0b013e3181e15c22 [DOI] [PubMed] [Google Scholar]
- Hosek S, & Pettifor A (2019). HIV prevention interventions for adolescents. Current HIV/AIDS Reports, 16(1), 120–128. 10.1007/s11904-019-00431-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang FY, Chung H, Kroenke K, Delucchi KL, & Spitzer RL (2006). Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. Journal of General Internal Medicine, 21(6), 547–552. 10.1111/j.1525-1497.2006.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics JR, Hamburger ME, Vlahov D, & et al. (2001). Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: Longitudinal analysis from the HIV epidemiology research study. JAMA, 285(11), 1466–1474. 10.1001/jama.285.11.1466 [DOI] [PubMed] [Google Scholar]
- Kalichman SC, & Simbayi LC (2004). Sexual assault history and risks for sexually transmitted infections among women in an African township in Cape Town, South Africa. AIDS Care, 16(6), 681–689. 10.1080/09540120410331269530 [DOI] [PubMed] [Google Scholar]
- Khan MR, Kaufman JS, Pence BW, Gaynes BN, Adimora AA, Weir SS, & Miller WC (2009). Depression, sexually transmitted infection, and sexual risk behavior among young adults in the United States. Archives of Pediatrics & Adolescent Medicine, 163(7), 644–652. 10.1001/archpediatrics.2009.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuringe E, Materu J, Nyato D, Majani E, Ngeni F, Shao A, Mjungu D, Mtenga B, Nnko S, Kipingili T, Mongi A, Nyanda P, Changalucha J, & Wambura M (2019). Prevalence and correlates of depression and anxiety symptoms among out-of-school adolescent girls and young women in Tanzania: A cross-sectional study. PLOS ONE, 14(8), e0221053 10.1371/journal.pone.0221053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalor K (2004). Child sexual abuse in sub-Saharan Africa: A literature review. Child Abuse & Neglect, 28(4), 439–460. 10.1016/j.chiabu.2003.07.005 [DOI] [PubMed] [Google Scholar]
- Monahan PO, Shacham E, Reece M, Kroenke K, Ong’or WO, Omollo O, … Ojwang C (2009). Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in Western Kenya. Journal of General Internal Medicine, 24(2), 189–197. 10.1007/s11606-008-0846-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero MJ, Raper JL, Reif S, Whetten K, Leserman J, Thielman NM, & Pence BW (2009). Overload: Impact of incident stressful events on antiretroviral medication adherence and virologic failure in a longitudinal, multisite human immunodeficiency virus cohort study. Psychosomatic Medicine, 71(9), 920–926. 10.1097/PSY.0b013e3181bfe8d2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neese AL, Pittman LD, & Hunemorder R (2013). Depressive symptoms and somatic complaints among Zambian adolescents: Associations with stress and coping. Journal of Research on Adolescence, 23(1), 118–127. 10.1111/j.1532-7795.2012.00834.x [DOI] [Google Scholar]
- Nelson RM, Lewis LL, Struble K, & Wood SF (2010). Ethical and regulatory considerations for the inclusion of adolescents in HIV biomedical prevention research. JAIDS Journal of Acquired Immune Deficiency Syndromes, 54, S18–S24. 10.1097/QAI.0b013e3181e2012e [DOI] [PubMed] [Google Scholar]
- Pack AP, Sastry J, Tolley EE, Kaaya S, Headley J, Kaale A, & Baumgartner JN (2019). Stakeholder acceptability of adolescent participation in clinical trials for biomedical HIV prevention products: Considerations from Tanzania and India. AIDS Care, 31(7), 857–863. 10.1080/09540121.2018.1563285 [DOI] [PubMed] [Google Scholar]
- Page RM, & Hall CP (2009). Psychosocial distress and alcohol use as factors in adolescent sexual behavior among sub-Saharan African adolescents. Journal of School Health, 79(8), 369–379. 10.1111/j.1746-1561.2009.00423.x [DOI] [PubMed] [Google Scholar]
- Pence BW, Mugavero MJ, Carter TJ, Leserman J, Thielman NM, Raper JL, … Whetten K (2012). Childhood trauma and health outcomes in HIV-infected patients: An exploration of causal pathways. Journal of Acquired Immune Deficiency Syndromes (1999), 59(4), 409–416. 10.1097/QAI.0b013e31824150bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips SJ, & Mbizvo MT (2016). Empowering adolescent girls in Sub-Saharan Africa to prevent unintended pregnancy and HIV: A critical research gap. International Journal of Gynecology & Obstetrics, 132(1), 1–3. 10.1016/j.ijgo.2015.10.005 [DOI] [PubMed] [Google Scholar]
- Pomfret S, Karim QA, & Benatar SR (2010). Inclusion of adolescent women in microbicide trials: A public health imperative! Public Health Ethics, 3(1), 39–50. 10.1093/phe/php013 [DOI] [Google Scholar]
- Raja S, Holland C, Bois SND, McKirnan D, Allgood KL, & Glick N (2015). History of traumatic events in HIV-positive individuals: Risk behavior implications in an urban clinic setting. Journal of HIV/AIDS & Social Services, 14(1), 110–128. 10.1080/15381501.2014.999182 [DOI] [Google Scholar]
- Ramirez-Avila L, Regan S, Giddy J, Chetty S, Ross D, Katz JN, … Bassett IV (2012). Depressive symptoms and their impact on health-seeking behaviors in newly-diagnosed HIV-infected patients in Durban, South Africa. AIDS and Behavior, 16(8), 2226–2235. 10.1007/s10461-012-0160-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes AE, & Bethell J (2008). Suicidal ideators without major depression—Whom are we not reaching? The Canadian Journal of Psychiatry, 53(2), 125–130. 10.1177/070674370805300209 [DOI] [PubMed] [Google Scholar]
- Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, … Katon W (2010). Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatrics, 126(6), 1117–1123. 10.1542/peds.2010-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronconi JM, Shiner B, & Watts BV (2014). Inclusion and exclusion criteria in randomized controlled trials of psychotherapy for PTSD. Journal of Psychiatric Practice, 20(1), 25–37. 10.1097/01.pra.0000442936.23457.5b [DOI] [PubMed] [Google Scholar]
- Sales JM, Swartzendruber A, & Phillips AL (2016). Trauma-informed HIV prevention and treatment. Current HIV/AIDS Reports, 13(6), 374–382. 10.1007/s11904-016-0337-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, & Ludman EJ (2013). Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatric Services, 64(12), 1195–1202. 10.1176/appi.ps.201200587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, & DiMatteo MR (2014). Depression treatment enhances adherence to antiretroviral therapy: A meta-analysis. Annals of Behavioral Medicine, 47(3), 259–269. 10.1007/s12160-013-9559-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh JA, Abdool Karim SS, Abdool Karim Q, Mlisana K, Williamson C, Gray C, … Gray A (2006). Enrolling adolescents in research on HIV and other sensitive issues: Lessons from South Africa. PLoS Medicine, 3(7), e180 10.1371/journal.pmed.0030180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siyahhan Julnes P, Auh S, Krakora R, Withers K, Nora D, Matthews L, … Kapetanovic S (2016). The association between post-traumatic stress disorder and markers of inflammation and immune activation in HIV-infected individuals with controlled viremia. Psychosomatics, 57(4), 423–430. 10.1016/j.psym.2016.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies G, Konkiewitz EC, & Seedat S (2018). Incidence and persistence of depression among women living with and without HIV in South Africa: A longitudinal study. AIDS and Behavior, 22(10), 3155–3165. 10.1007/s10461-018-2072-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadler J, Delany-Moretlwe S, Palanee T, & Rees H (2014). Hidden harms: Women’s narratives of intimate partner violence in a microbicide trial, South Africa. Social Science & Medicine, 110, 49–55. 10.1016/j.socscimed.2014.03.021 [DOI] [PubMed] [Google Scholar]
- Stark L (2018). Early marriage and cultural constructions of adulthood in two slums in Dar es Salaam. Culture, Health & Sexuality, 20(8), 888–901. 10.1080/13691058.2017.1390162 [DOI] [PubMed] [Google Scholar]
- Stirman SW, DeRubeis RJ, Crits-Christoph P, & Brody PE (2003). Are samples in randomized controlled trials of psychotherapy representative of community outpatients? A New methodology and initial findings. Journal of Consulting and Clinical Psychology, 71(6), 963–972. 10.1037/0022-006X.71.6.963 [DOI] [PubMed] [Google Scholar]
- Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, & Seedat S (2009). Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry, 50(2), 121–127. 10.1016/j.comppsych.2008.06.006 [DOI] [PubMed] [Google Scholar]
- Tolley EE, Kaaya S, Kaale A, Minja A, Bangapi D, Kalungura H, … Baumgartner JN (2014). Comparing patterns of sexual risk among adolescent and young women in a mixed-method study in Tanzania: Implications for adolescent participation in HIV prevention trials. Journal of the International AIDS Society, 17(3(Suppl 2)). 10.7448/IAS.17.3.19149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAID. (2014). GAP Report 2014: People left behind: Adolescent girls and young women. Retrieved from http://www.unaids.org/sites/default/files/media/images/gap_report_popn_02_girlsyoungwomen_2014july-sept.pdf [Google Scholar]
- World Health Organization. (2016). mhGAP Intervention Guide—Version 2.0 Retrieved from https://www.who.int/publications-detail/mhgap-intervention-guide---version-2.0 [Google Scholar]
- World Health Organization. (n.d.). Process of translation and adaptation of instruments. Retrieved from https://www.who.int/substance_abuse/research_tools/translation/en/ [Google Scholar]
- Zimmerman M, Chelminski I, & Posternak MA (2005). Generalizability of antidepressant efficacy trials: Differences between depressed psychiatric outpatients who would or would not qualify for an efficacy trial. American Journal of Psychiatry, 162(7), 1370–1372. 10.1176/appi.ajp.162.7.1370 [DOI] [PubMed] [Google Scholar]


