Abstract
Background:
In 2012, select Veterans Health Administration (VHA) facilities implemented a homeless-tailored medical home model (called H-PACT) to improve care processes and outcomes for homeless Veterans.
Objective.
To determine whether H-PACT offers a better patient experience than standard VHA primary care.
Research Design:
We used multivariable logistic regressions to estimate differences in the probability of reporting positive primary care experiences on a national survey.
Subjects:
Homeless-experienced survey respondents enrolled in H-PACT (n=251) or standard primary care in facilities with HPACT available (n=1,527) and facilities without H-PACT (n=10,079).
Measures:
Patient experiences in eight domains from the Consumer Assessment of Healthcare Provider and Systems surveys. Domain scores were categorized as positive versus non-positive.
Results:
H-PACT patients were less likely than standard primary care patients to be female, have four-year college degrees, or to have served in recent military conflicts; they received more primary care visits and social services. H-PACT patients were more likely than standard primary care patients in the same facilities to report positive experiences with access (adjusted risk difference[RD]=17.4), communication (RD=13.9), office staff (RD=13.1), provider ratings (RD=11.0), and comprehensiveness (RD=9.3). Standard primary care patients in facilities with H-PACT available were more likely than those from facilities without H-PACT to report positive experiences with communication (RD=4.7) and self-management support (RD=4.6).
Conclusions:
Patient-centered medical homes designed to address the social determinants of health offer a better care experience for homeless patients, compared to standard primary care approaches. The lessons learned from H-PACT can be applied throughout VHA and to other healthcare settings.
Keywords: homelessness, patient experience, primary care, Veterans
Healthcare systems value patient experiences with care as a marker of quality1,2 because patients who report positive experiences are more likely to use primary care services, follow provider recommendations, continue medications as prescribed, and rate their health favorably.3-5 Positive healthcare encounters may be particularly important for persons with homeless experiences (henceforth “homeless”) because these patients have suboptimal health behaviors, difficulty accessing care, and poor outcomes due to these factors.6-11 Healthcare systems lack information to guide efforts to improve the experiences of homeless patients.
More than 37,000 Veterans are homeless on a given night.12 The Veterans Health Administration (VHA) has led primary care redesign efforts to optimize the healthcare experience of all Veterans, including those who are homeless.13 In 2010, VHA facilities implemented a patient-centered medical home (PCMH) model of care that reorganized providers and staff into interdisciplinary primary care teams. With a goal of improving care efficiency, these teams are responsible for delivering comprehensive, well-coordinated, patient-centered care for their empaneled patients.14,15 In addition to this national PCMH model, 63 VHA facilities since 2012 have developed Homeless Patient Aligned Care Teams (H-PACTs) – a PCMH model tailored to the unique needs of homeless Veterans.16
Similar to Health Care for the Homeless (HCH) programs in federally qualified health centers, the H-PACT model is designed to enhance access to care, address the social determinants of health, and facilitate housing placement for persons who are homeless or at risk for homelessness.17 H-PACT is highly contextualized, in that the staffing, services, and features are unique to each facility.18 While variations exist, an H-PACT typically differs from other primary care teams in several regards. For example, H-PACTs focus explicitly on the mission to reduce homelessness, provide access accommodations, train providers in homeless healthcare delivery, and coordinate primary care with mental health, addiction, and social services.18-20 This tailored PCMH model has evidence of benefit, in that some homeless patients enrolled in H-PACT have increases in primary care visits21 and greater reductions in acute services use than homeless patients managed by other primary care teams in the same facilities.17,22 Patient experiences within H-PACT are, however, unknown.
Prior investigations into homeless patient experiences of care in HCH settings were based on small numbers of sites, and/or lacked comparison primary care settings dedicated to homeless patients.6,23 In VHA, two studies of patient experiences in tailored and non-tailored primary care settings produced divergent results.17,24 A first study, conducted prior to the H-PACT initiative, found that homeless patients reported superior healthcare experiences in settings with greater tailoring of services towards homeless patient needs.24 A second study, conducted in two VHA sites that offered H-PACT among their services, found no differences in the experiences of homeless patients enrolled in H-PACT versus other primary care teams at those sites.17 A potential reason for the discrepant findings is that the latter study17 focused on 266 Veterans who consented to enter a prospective study, and such volunteers may have been prone to regard care favorably.
To answer the question of whether H-PACT offers a better patient experience than standard VHA primary care on a broader scale, this study analyzes national data from VHA’s validated survey of healthcare experiences to compare the experiences of homeless patients in H-PACT to those of homeless patients receiving standard primary care in the same facilities, and standard primary care in facilities without any H-PACT. We hypothesized that homeless patients enrolled in H-PACT would be more likely to report positive healthcare experiences than homeless patients receiving standard primary care.
Methods
Design
We conducted a retrospective cohort study of primary care experiences in a large sample of patients with homeless experiences who received primary care in urban VHA facilities.
Data Sources and Study Sample
We accessed data from the fiscal year (FY) 2014-2015 Patient Centered Medical Home Survey of Healthcare Experiences of Patients (PCMH-SHEP), a validated ongoing survey of VHA primary care experiences conducted by the VHA Office of Reporting, Analytics, Performance, Improvement and Deployment.25 Veterans are eligible for the PCMH-SHEP if they received VHA outpatient services in the past month, had a primary care visit with the lead provider of their assigned primary care team lead in past 10 months, and did not participate in the prior year’s survey. Each month, a stratified, random sample of eligible Veterans are mailed a letter explaining the survey goals, followed by the survey the second week, and a thank-you/reminder postcard the third week.
This study includes eligible Veterans with recent administrative evidence of homelessness. We linked records from the 2014-2015 PCMH-SHEP with sociodemographic and clinical characteristics drawn from VHA administrative records in the year prior to the survey. Veterans were coded as “homeless” if they had one inpatient or outpatient visit where lack of housing, unstable housing, or other housing circumstances were documented (ICD-9 codes V60.0, V60.1, V60.89, V60.9), or they received VHA homeless services.26 This definition aligns with the H-PACT goal of managing care for persons at-risk of homelessness, and could include patients with a domicile at the time of the survey. We excluded data from participants not meeting the study classification of H-PACT enrollment (see below), and those with missing data on study variables. All study procedures were approved by institutional review boards at the University of Utah, VA Salt Lake City Health Care System, and VA Pittsburgh Healthcare System.
Facilities with H-PACT
As described elsewhere,27 we identified VHA facilities that had an H-PACT functioning the entire 12 months prior to the first PCMH-SHEP administration (as early as FY 2013) and through FY 2015. Because all facilities with H-PACT in FY 2013-2015 were located in U.S. urban areas, we chose urban VHA facilities with no known H-PACT for comparisons. To identify urban sites, facility geocoded attributes were extracted from VHA Site Tacking (VAST) records.28 We selected facilities classified in VAST as urban (versus rural, highly rural, or insular), based on rural-urban commuting area (RUCA) definitions.
Enrollment in H-PACT versus Other Primary Care Teams
Regardless of housing circumstances, Veterans seeking VHA primary care services are assigned to a primary care team based on provider workload, appointment availability, and service needs. In facilities with H-PACT available, referrals occur through homeless outreach, Veteran word-of-mouth, and close relationships between H-PACT and other medical service lines. While specific enrollment criteria vary by site, H-PACT providers seek to enroll high-risk, high-need patients who are unwilling or unable to access traditional primary care services.20
We used VHA administrative records of primary care team assignment to determine enrollment in H-PACT versus other primary care teams in the year prior to the PCMH-SHEP. A one-year window was selected because the PCMH-SHEP asks patients to report on experiences with their assigned primary care team in the past 12 months. We coded patients as “enrolled in H-PACT” if they were assigned to an H-PACT for the full year prior to PCMH-SHEP, and “standard primary care” if they were not assigned to H-PACT at any time in the prior year. We excluded patients assigned to H-PACT for only part of the year to isolate patient experiences within H-PACT versus other VHA primary care teams. To avoid misclassification, we excluded data from a small number of patients (n=69) with H-PACT enrollment data who primarily received care at VHA facilities without any H-PACT.
Primary Care Experiences
We examined patient-reported experiences with primary care in eight domains.25 We grouped PCMH-SHEP items into domains of access, communication, and office staff helpfulness/courtesy based on the Consumer Assessment of Healthcare Provider and Systems (CAHPS) Clinician and Group Survey 3.0,29 and domains of comprehensiveness, shared decision-making, and self-management support based on the CAHPS PCMH Supplement 2.0.30,31 The access domain assesses how often patients received timely appointments, care, and information. The communication domain assesses how well providers communicated with patients. The office staff domain assesses staff helpfulness, courtesy, and respect. Comprehensiveness assesses whether providers pay attention to mental or emotional health. Shared decision-making assesses whether providers discussed medication decisions with patients. Self-management support assesses whether providers supported patients in taking care of their own health. One item assesses care coordination (“In the last twelve months, how often did the provider seem informed and up-to-date about the care you got from specialists?”) and one assesses patients’ overall rating of providers.
For domains with multiple items, composite scores were calculated as the average of applicable, non-missing items for that domain. The domain scores were highly skewed, with a majority of homeless Veterans reporting positive experiences. Therefore, we categorized experiences in each domain as negative, moderate, or positive using approaches published in prior studies.32,33 Specifically, we reviewed the distribution of responses and selected plausible cut-points for negative and positive experiences that ensured at least 10% of respondents in each category (Supplemental Digital Content 1). This process also minimized the potential impact of extreme response tendencies, which have been found among racial/ethnic minority and lower education groups.34,35
Covariates
We controlled for patient characteristics typically associated with patient experiences with care.6,32,36-38 From the PCMH-SHEP, we controlled for race/ethnicity, education, general health and mental health ratings (categorized as fair/poor vs. excellent/very good/good), and number of past year visits to the assigned primary care team. From administrative data, we selected prior year age, sex, marital status, and urban versus rural geographic residence. In 10% of cases, we used urban/rural residence recorded in 2017 because data were missing in the year preceding the PCMH-SHEP. We used the Gagne Comorbidity Index, a weighted index of chronic conditions predictive of one-year mortality, as a measure of medical morbidity.39 We controlled for psychiatric disorder diagnoses, defined as one inpatient or two outpatient visits with mental health or substance abuse ICD-9 diagnoses in the prior year.40 Types of psychiatric disorders (e.g., mood, anxiety, etc.) were based on the Healthcare Cost and Utilization Project’s Clinical Classification Software for Mental Health and Substance Abuse,41 modified in the current study to include post-traumatic stress disorder. To account for exposures to other VHA social services, we controlled for whether or not patients received: healthcare for homeless Veteran services, U.S. Housing and Urban Development – Veterans Affairs Supportive Housing (HUD-VASH) vouchers, grant and per diem services, community work therapy, justice-related services, or domiciliary care for homeless Veterans.
Statistical Analyses
Analyses were conducted using Stata version 15.0. We applied PCMH-SHEP survey design and post-stratification weights to account for varying proportions of patients sampled across VHA settings and differential response by age and sex. Standard errors were estimated using a Taylor series approximation that accounted for the stratified sampling design.
We used cross-tabulations and design-adjusted chi-square tests to compare the distribution of patient characteristics and PCMH-SHEP responses (categorized as negative, moderate, or positive) for groups differing in H-PACT enrollment. Because only a small percentage of participants enrolled in H-PACT reported negative care experiences (4-13% in any single domain), we combined the negative and moderate response categories in subsequent analyses.
We used multivariable logistic regressions to estimate group differences in reporting positive (versus moderate/negative) experiences with care, controlling for sociodemographic and clinical characteristics. We converted model estimates to predicted probabilities (0-100 percentage scale) and risk differences to aid interpretation.
We conducted a sensitivity analysis to determine if study results would change when accounting for unmeasured variations in site and H-PACT implementation. Specifically, we limited analyses to VHA facilities with H-PACT among their services, and added site-specific dummy variables to the multivariable logistic regression models.
Results
Of 63 facilities with a known H-PACT, 25 were open throughout FY 2013-2015; 485 facilities in urban areas had no H-PACT (Figure 1). From the study facilities, 57,517 homeless patients were eligible for the PCMH-SHEP, and 13,344 (23%) responded to the survey. The response rates were similar for homeless Veterans enrolled in H-PACT (23%), compared to homeless Veterans receiving standard primary care in VHA facilities with an H-PACT available (22%) and in facilities without H-PACT (24%). Homeless survey respondents were more likely than non-respondents to be male (91% vs 87%) and age 65 or older (29% vs 15%); they were less likely to have served in the Gulf War and more recent conflicts (16% vs 36%), to have psychiatric disorder diagnoses (64% vs 72%), and less likely to have used VHA homeless services in the year prior to PCMH-SHEP (80% vs 85%).
Figure.
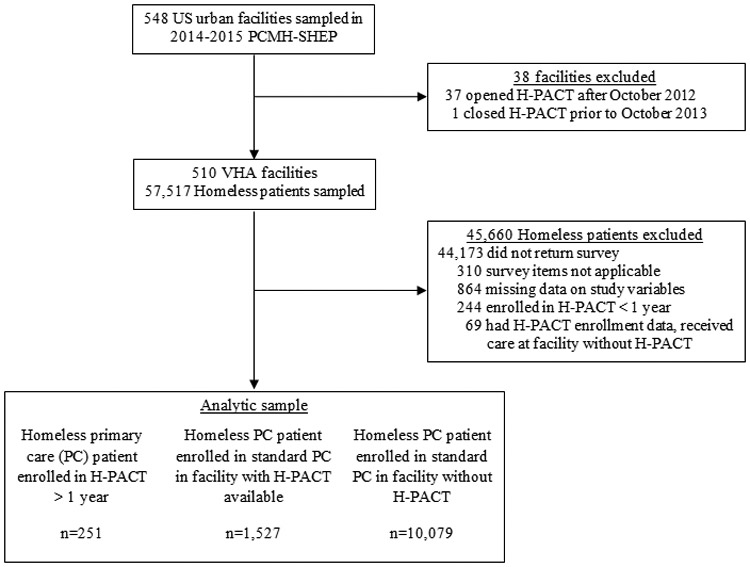
Inclusion and exclusion criteria applied to create an analytic sample of homeless patients who received care at Veterans Healthcare Administration (VHA) facilities with or without an Homeless Patient Aligned Care Team (H-PACT) among their services, and who completed the 2014-2015 Patient Centered Medical Home Survey of Healthcare Experiences of Patients (PCMH-SHEP). Exclusion criteria were applied sequentially.
Among survey respondents, 864 (7%) were excluded due to missing data on study variables of interest (i.e., education, health rating, mental health rating, race/ethnicity, marital status, urban versus rural residence; < 3% missing on any single variable). Respondents with missing data did not differ statistically from respondents with complete data on any of the study variables (all p’s > 0.05). The final sample included 251 patients enrolled in H-PACT for one year, 1,527 receiving standard primary care in facilities with H-PACT available, and 10,079 receiving standard primary care in facilities without H-PACT.
Differences in Sociodemographic and Clinical Characteristics among H-PACT Enrollment Groups
H-PACT patients were less likely than homeless patients receiving standard primary care to be female or non-Hispanic white, to have served in the recent military conflicts, to rate their general health as fair or poor, or to have post-traumatic stress disorder diagnoses (Table 1). H-PACT patients received more primary care visits and were more likely to receive social services, such as health care for homeless Veterans, HUD-VASH vouchers, or grant and per diem services.
Table 1.
Sociodemographic and Clinical Characteristics of Homeless Primary Care Patients in the Veterans Health Administration, by H-PACT Enrollment Groups.
| Facility with H-PACT | ||||||||
|---|---|---|---|---|---|---|---|---|
| Enrolled in H-PACT (n=251)a |
Enrolled in standard PC (n=1,527) |
Standard PC in facility without H-PACT (n=10,079) |
||||||
| Characteristic | %b | SE | % | SE | % | SE | X2 | p-value |
| Female sex | 3.3 | 1.4 | 14.5 | 1.5 | 11.5 | 0.5 | 6.99 | <.001 |
| Age | 2.03 | .08 | ||||||
| 18-44 | 17.6 | 4.1 | 20.0 | 1.9 | 22.7 | 0.9 | ||
| 45-54 | 23.3 | 3.7 | 24.4 | 1.5 | 25.7 | 0.7 | ||
| 55-64 | 48.6 | 4.2 | 38.5 | 1.6 | 35.4 | 0.7 | ||
| 65+ | 10.4 | 2.1 | 17.0 | 1.0 | 16.7 | 0.4 | ||
| Race/ethnicity | 28.86 | <.001 | ||||||
| Non-Hispanic white | 27.3 | 3.6 | 31.9 | 1.6 | 48.9 | 0.8 | ||
| Non-Hispanic black | 57.7 | 4.1 | 51.7 | 1.8 | 36.5 | 0.8 | ||
| Other | 15.1 | 2.8 | 16.4 | 1.4 | 14.6 | 0.6 | ||
| Education | 1.47 | .18 | ||||||
| < 12 years education | 9.3 | 2.5 | 5.9 | 0.7 | 5.7 | 0.3 | ||
| High school equivalent | 34.2 | 3.8 | 30.1 | 1.6 | 32.4 | 0.7 | ||
| Some college | 49.1 | 4.3 | 49.8 | 1.8 | 48.7 | 0.8 | ||
| 4 year college degree | 7.4 | 1.9 | 14.1 | 1.2 | 13.2 | 0.5 | ||
| Marital status | 8.41 | <.001 | ||||||
| Married | 12.6 | 3.2 | 17.9 | 1.4 | 22.5 | 0.6 | ||
| Previously married | 44.9 | 4.2 | 48.2 | 1.8 | 50.9 | 0.8 | ||
| Never married | 42.5 | 4.2 | 33.9 | 1.7 | 26.6 | 0.7 | ||
| Rural residence | 2.1 | 1.0 | 5.0 | 0.7 | 15.6 | 0.5 | 60.67 | <.001 |
| Service era(s) | ||||||||
| Pre-Vietnam | 0.2 | 0.2 | 4.7 | 0.5 | 4.4 | 0.2 | 7.43 | .002 |
| Vietnam | 40.5 | 4.0 | 36.2 | 1.5 | 33.0 | 0.6 | 3.53 | .03 |
| Post-Vietnam | 38.8 | 4.1 | 30.7 | 1.6 | 30.1 | 0.7 | 2.18 | .11 |
| Gulf war or more recent | 19.8 | 4.2 | 26.9 | 1.9 | 31.8 | 0.9 | 5.24 | .006 |
| General health fair/poor | 36.9 | 4.0 | 47.0 | 1.8 | 49.9 | 0.8 | 4.93 | .01 |
| Mental health fair/poor | 45.9 | 4.3 | 53.3 | 1.7 | 53.3 | 0.7 | 1.25 | .29 |
| Gagne comorbidity (mean, sd) | 1.25 | 0.13 | 1.10 | 0.05 | 1.13 | 0.02 | 0.58 | .56 |
| Psychiatric Diagnoses | ||||||||
| Mood disorder | 41.3 | 4.2 | 48.8 | 1.8 | 48.6 | 0.8 | 1.23 | .29 |
| Post-traumatic stress disorder | 12.0 | 2.5 | 25.2 | 1.6 | 25.5 | 0.8 | 5.5 | .005 |
| Other anxiety disorders | 20.3 | 3.5 | 17.0 | 1.4 | 19.1 | 0.6 | 1.07 | .34 |
| Psychotic disorder | 13.2 | 3.0 | 10.6 | 1.1 | 8.1 | 0.5 | 4.14 | .02 |
| Alcohol use disorder | 32.8 | 3.9 | 26.2 | 1.5 | 26.6 | 0.7 | 1.21 | .29 |
| Drug use disorder | 27.8 | 3.6 | 25.2 | 1.5 | 25.2 | 0.7 | 0.22 | .80 |
| VHA primary care visits | 10.92 | <.001 | ||||||
| 1 or 2 | 26.7 | 3.8 | 37.8 | 1.7 | 45.9 | 0.8 | ||
| 3 or 4 | 38.5 | 4.2 | 36.6 | 1.8 | 34.5 | 0.8 | ||
| 5 or more | 34.8 | 4.1 | 25.6 | 1.5 | 19.6 | 0.6 | ||
| Other VHA services | ||||||||
| Healthcare for homeless Veterans | 66.6 | 3.9 | 54.8 | 1.7 | 54.1 | 0.8 | 3.71 | .03 |
| HUD-VASH | 62.2 | 4.3 | 48.0 | 1.8 | 39.7 | 0.8 | 20.41 | <.001 |
| Grant and per diem | 26.1 | 3.5 | 17.7 | 1.4 | 12.9 | 0.6 | 14.21 | <.001 |
| Community employment services | 0.6 | 0.4 | 0.3 | 0.1 | 0.8 | 0.1 | 2.69 | .07 |
| Justice related programs | 5.8 | 2.1 | 4.2 | 0.8 | 6.7 | 0.4 | 3.50 | .03 |
| Domiciliary | 1.7 | 0.7 | 1.6 | 0.5 | 2.1 | 0.2 | 0.66 | .48 |
Abbreviations: Homeless = at least 1 past year diagnosis related to homelessness or receipt of VHA homeless services; H-PACT = Homeless Patient Aligned Care Team; HUD-VASH = U.S. Department of Housing and Urban Development-Veterans Affairs supported housing voucher; PC = primary care.
n = number of respondents to the Patient-Centered Medical Home Survey of Healthcare Experiences of Patients (PCMH-SHEP), administered nationally to Veterans Health Administration (VHA) primary care patients.
All estimates use PCMH-SHEP survey weights. % = Survey weighted percent. SE = standard errors account for clustering by design strata (VHA facility, survey month). The table p-values are from survey weighted tests of differences. X2 tested for group differences in binary or categorical sociodemographic characteristics. ANOVA tested for group differences in Gagne comorbidity index.
Primary Care Experiences across H-PACT Enrollment Groups
H-PACT patients reported more positive healthcare experiences than homeless patients receiving standard primary care in facilities with or without H-PACT available (Table 2; all p’s < .001). Specifically, 54%-75% of H-PACT patients reported positive experiences in any single domain, compared to 35%-58% of standard primary care patients. Only 4%-12% of H-PACT patients reported negative experiences in any single domain.
Table 2.
Percent of VHA Homeless Primary Care Patients who Reported Positive, Moderate, and Negative Primary Care Experiences, by H-PACT Enrollment Groups
| Facility with H-PACT | ||||||||
|---|---|---|---|---|---|---|---|---|
| Enrolled in H-PACT (n=251) |
Enrolled in standard PC (n=1,527) |
Standard PC in facility without H-PACT (n=10,079) |
||||||
| Domain | % | SE | % | SE | % | SE | X2 | p-value |
| Access | 4.41 | .002 | ||||||
| Positive | 55.7 | 4.5 | 35.0 | 1.8 | 34.7 | 0.8 | ||
| Moderate | 37.9 | 4.3 | 51.4 | 1.9 | 51.1 | 0.8 | ||
| Negative | 6.4 | 2.7 | 13.6 | 1.5 | 14.3 | 0.6 | ||
| Communication | ||||||||
| Positive | 75.1 | 3.9 | 58.2 | 1.8 | 52.0 | 0.8 | 7.93 | <.001 |
| Moderate | 19.2 | 3.4 | 25.6 | 1.5 | 27.9 | 0.7 | ||
| Negative | 5.7 | 2.4 | 16.2 | 1.5 | 20.1 | 0.6 | ||
| Office staff helpfulness/courtesy | 2.93 | .02 | ||||||
| Positive | 66.8 | 4.2 | 50.8 | 1.8 | 53.8 | 0.8 | ||
| Moderate | 20.9 | 3.6 | 33.1 | 1.7 | 29.7 | 0.7 | ||
| Negative | 12.3 | 3.1 | 16.1 | 1.3 | 16.5 | 0.7 | ||
| Provider rating | 8.01 | <.001 | ||||||
| Positive | 65.1 | 4.2 | 50.4 | 1.8 | 43.3 | 0.8 | ||
| Moderate | 29.8 | 3.9 | 35.5 | 1.7 | 39.4 | 0.8 | ||
| Negative | 5.1 | 2.4 | 14.1 | 1.4 | 17.3 | 0.6 | ||
| Comprehensiveness | 3.28 | .01 | ||||||
| Positive | 65.6 | 4.0 | 54.0 | 1.8 | 52.0 | 0.8 | ||
| Moderate | 24.4 | 3.7 | 28.9 | 1.7 | 28.6 | 0.7 | ||
| Negative | 10.0 | 2.2 | 17.0 | 1.3 | 19.5 | 0.6 | ||
| Coordination | 3.07 | .02 | ||||||
| Positive | 67.9 | 5.3 | 56.9 | 2.1 | 52.2 | 0.9 | ||
| Moderate | 28.3 | 4.9 | 34.0 | 2.0 | 35.0 | 0.9 | ||
| Negative | 3.7 | 3.2 | 9.1 | 1.4 | 12.9 | 0.7 | ||
| Self-management support | 7.40 | <.001 | ||||||
| Positive | 64.8 | 4.2 | 52.8 | 1.8 | 46.3 | 0.8 | ||
| Moderate | 22.1 | 3.7 | 21.2 | 1.4 | 23.8 | 0.7 | ||
| Negative | 13.0 | 3.0 | 25.5 | 1.6 | 29.9 | 0.7 | ||
| Shared decision-making | 6.53 | <.001 | ||||||
| Positive | 53.6 | 5.2 | 41.5 | 2.1 | 36.9 | 0.9 | ||
| Moderate | 39.6 | 5.1 | 47.1 | 2.1 | 44.7 | 1.0 | ||
| Negative | 6.8 | 3.2 | 11.5 | 1.3 | 18.4 | 0.8 | ||
Abbreviations: H-PACT = Homeless Patient Aligned Care Team; PC = primary care; VHA = Veterans Health Administration.
Domains were drawn from the 2014-2015 Patient-Centered Medical Home Survey of Healthcare Experiences of Patients (PCMH-SHEP). Positive experiences include optimal experiences (e.g., provider “Always” listens); while the negative experience include suboptimal experiences (e.g., provider “Never” or only “Sometimes” listens).
Adjusted Differences in Primary Care Experiences by H-PACT Enrollment Groups
After controlling for potential confounders, primary care use, and exposure to other social services, H-PACT enrollment was a significant predictor of primary care experiences (Table 3). H-PACT patients were more likely to report positive primary care experiences than homeless patients receiving standard primary care in the same facilities in five domains: access (adjusted risk difference[RD]=17.4), communication (RD=13.9), office staff (RD=13.1), ratings of providers (RD=11.0), and comprehensiveness (RD=9.3). Standard primary care patients from facilities with H-PACT available were more likely than patients from facilities without H-PACT to report positive experiences in communication (RD=4.7) and self-management support (RD=4.6).
Table 3.
Adjusted probability of reporting positive primary care experiences, by H-PACT Enrollment Groups.
| Facility with H-PACT | Risk differences | ||||||
|---|---|---|---|---|---|---|---|
| Enrolled in H-PACT (n=251) |
Enrolled in standard PC (n=1,527) |
Standard PC in facility without H-PACT (n=10,079) |
H-PACT versus standard PC in facility with H-PACT |
Standard PC in facility with H-PACT versus facility without H-PACT |
|||
| Primary care domain | % | % | % | RD | 95% CI | RD | 95% CI |
| Access | 51.5 | 34.1 | 35.0 | 17.4*** | 8.1, 26.7 | −0.9 | −4.6, 2.9 |
| Communication | 71.0 | 57.1 | 52.5 | 13.9** | 5.2, 22.6 | 4.7* | 0.9, 8.4 |
| Office staff helpfulness/courtesy | 63.5 | 50.4 | 54.0 | 13.1** | 4.1, 22.2 | −3.6 | −7.5, 0.3 |
| Provider rating | 58.9 | 47.8 | 44.1 | 11.0* | 1.9, 20.1 | 3.8 | −0.1, 7.6 |
| Comprehensiveness | 62.6 | 53.3 | 52.3 | 9.3* | 0.8, 17.9 | 1.0 | −3.0, 5.0 |
| Care coordination | 63.7 | 54.8 | 52.8 | 8.9 | −1.0, 21.0 | 2.0 | −1.8, 7.1 |
| Self-management support | 59.5 | 51.4 | 46.8 | 8.0 | −1.3, 17.4 | 4.6* | 0.7, 8.5 |
| Shared decision-making | 48.0 | 39.6 | 37.5 | 8.4 | −2.3, 6.6 | 2.1 | −2.9, 19.7 |
p<.05
p<.01
p<.001
Domains were drawn from the 2014-2015 Patient-Centered Medical Home Survey of Healthcare Experiences of Patients (PCMH-SHEP). Positive experiences include optimal experiences (e.g., provider “Always” listens); while the negative experience include suboptimal experiences (e.g., provider “Never” or only “Sometimes” listens).
% = Predicted probability of reporting positive healthcare experiences, calculated separately by H-PACT enrollment groups. Probabilities were estimated from logistic regression models predicting positive versus moderate/negative experiences with care. Models, run separately for each domain of care, controlled for patient sex, age, race/ethnicity, education, marital status, rural versus urban residence, period of service, physical and mental health ratings, clinical diagnoses, number of primary care visits, and receipt of other VHA homeless services.
RD = Risk Difference. Differences in the probability of reporting positive healthcare experiences, calculated for homeless patients in facilities with an H-PACT available (enrolled versus not enrolled), and for patients receiving standard primary care (in VHA facilities with H-PACT available versus facilities without any H-PACT). Positive RD estimates indicate that H-PACT enrollment was associated with more positive primary care experiences.
As shown in Table 4, the patterns of more positive experiences associated with H-PACT enrollment were largely unchanged when controlling for study site; differences in experiences with comprehensiveness no longer reached statistical significance (p=0.11).
Table 4.
Risk Differences in Positive Care Experiences Associated with H-PACT Enrollment, Controlling for Site and Patient Covariates.
| Enrolled in H-PACT (n=251) |
Enrolled in standard primary care (n=1,527) |
Risk difference (RD) | ||
|---|---|---|---|---|
| Primary care domain | % | % | RD | 95% CI |
| Access | 56.2 | 35.0 | 21.1*** | 11.2, 31.0 |
| Communication | 71.8 | 58.7 | 13.1** | 4.5, 21.7 |
| Office staff helpfulness/courtesy | 63.6 | 51.3 | 12.3** | 3.5, 21.0 |
| Provider rating | 62.6 | 50.7 | 11.9* | 2.4, 21.4 |
| Comprehensiveness | 62.0 | 54.5 | 7.5 | −1.6, 16.6 |
| Care coordination | 65.8 | 57.2 | 8.6 | −2.9, 20.1 |
| Self-management support | 60.3 | 53.4 | 6.9 | −2.7, 16.6 |
| Shared decision-making | 51.8 | 41.7 | 10.2 | −2.0, 22.3 |
p<.05
p<.01
p<.001
Study sites included 25 VHA facilities with an H-PACT implemented by October 2013. % = Predicted probability of reporting positive healthcare experiences, calculated separately by primary care enrollment groups (H-PACT or standard primary care). Probabilities were estimated from logistic regression models predicting positive versus moderate/negative experiences with care. Models, run separately for each domain of care, controlled for patient sex, age, race/ethnicity, education, marital status, rural versus urban residence, period of service, physical and mental health ratings, clinical diagnoses, number of primary care visits, receipt of other VHA homeless services; and study site.
Discussion
This evaluation of national healthcare experience data sought to determine whether VHA’s homeless-tailored PCMH model of care offers a better healthcare experience for homeless patients, compared to VHA’s non-tailored PCMH approach. VHA is an ideal laboratory to test such primary care innovations due to its national reach, mission of caring for the most vulnerable Veterans, and standardized collection of patient experience surveys for health systems redesign efforts. In this large sample of patients with evidence of homelessness, patients enrolled in an H-PACT were much more likely to report positive experiences with care than patients receiving standard primary care in the same facilities. Our results build upon those from a prior study which found that VHA facilities with tailored PCMH approaches offer a better experience for homeless Veterans than other VHA facilities,27 and suggest that actual enrollment in H-PACT is a key factor in patient experiences with care.
Prior studies have documented negative healthcare encounters, such as perceptions of discrimination and feelings of being unwelcome, that contribute to homeless persons’ suboptimal engagement with healthcare services.42,43 That very few H-PACT patients in the current study reported negative healthcare experiences is an important finding. The percentage of H-PACT patients who reported negative experiences (3.7%-13.0% across domains) were considerably lower than percentages reported in the literature for non-homeless VHA outpatients (9.6%-28.3%).27 The patterns of results offer a hint that H-PACT may mitigate negative healthcare encounters that are thought to prevent homeless persons from seeking care.
Our finding of large differences in positive healthcare experiences in H-PACT versus standard primary care could be due to specific H-PACT services design features. For instance, some H-PACTs have expanded clinic hours, walk-in appointment capabilities, and small panel sizes to accommodate longer appointments; some use warm hand-offs to connect patients with other VHA services, conduct outreach to highly vulnerable patients who may not otherwise utilize VHA services, and offer staff training on homelessness. It is possible that features such as these could account for our observation of large difference between patients enrolled in an H-PACT versus standard primary care in the domains of access, office staff helpfulness/courtesy, and comprehensiveness. Notably, in the same domains, we observed no differences for patients receiving standard primary care in facilities with H-PACT available compared to facilities without H-PACT. Our findings imply that service design elements geared toward access, staff training, and services integration may be particularly important for enhancing homeless patient experiences with care.
Experience and interest in serving highly vulnerable populations is likely also important. VHA facilities to first implement H-PACT programs had existing homeless services and relatively large numbers of homeless Veterans.27 Therefore, it is possible that our finding of differences in experiences with communication and self-management support between standard primary care patients in facilities with H-PACT available compared to facilities without any H-PACT could be due to provider experience in and commitment to caring for homeless Veterans. Provider training in communication skills and homeless healthcare curriculum44 are potential strategies to strengthen patient-provider relationships and enhance healthcare experiences for homeless patients in facilities lacking homeless-specific services.
The study findings have implication for practice and future research. Our observation of positive care experiences builds upon evidence from other studies focused on service utilization outcomes, and provides a strong rationale for more VHA facilities to invest in tailored PCMH approaches. In facilities with an existing H-PACT, it will be important to expand the benefits of H-PACT to other patients with housing needs. In facilities with H-PACT available, only 25% of homeless patients had any H-PACT assignment; 12% were H-PACT-enrolled for a full year prior to PCMH-SHEP. Some patients with less acute clinical and social needs may not be targeted for enrollment, while others are transferred out of H-PACT when they become clinically and socially stable.20 To increase H-PACT enrollment, VHA facilities may consider hiring more providers to expand capacity, identifying H-PACT champions, and/or increasing outreach activities. To avoid disrupting existing primary care relationships for homeless patients enrolled in standard primary care, facilities might consider adapting effective H-PACT features to other primary care teams in the same facilities. To identify those service design features that matter most, one ongoing study is surveying H-PACT providers and several thousand Veteran outpatients to determine which service features (e.g., team composition, access accommodations, services integration) relate to patient experiences with care. Future research is needed to determine clinical and social benefits of H-PACT relative to standard primary care, and to identify which patients are most likely to benefit from such approaches.
This study has limitations. First, the study definition of H-PACT enrollment required a one-year threshold in VHA facilities with an H-PACT established by FY 2013. While this was necessary for internal validity, study findings may not generalize to all H-PACTs open today, to patients transferred out of H-PACT, or to patients not yet enrolled a full year. Second, generalizability is limited by modest survey response rates for all homeless patients. Veterans with homeless experiences could receive mailed surveys at their current residence (including shelters) or at addresses of a friend or family member, post office box or general delivery, or business. The study estimates of positive care experiences for all homeless Veterans may be optimistic if respondents included formerly homeless Veterans or those with less acute housing needs at the time of the mailing, and if current (as opposed to prior) homelessness is associated with worse primary care experience reporting; ongoing VHA research is examining this question.
Third, the study measure of patient experience does not assess homeless-specific concerns and service needs, such as stigma related to homelessness and assistance in obtaining food, shelter, or clothing.42 Future research that employs patient experience measures tailored to the study population, such as the Primary Care Quality-Homeless instrument,45 may provide further insights into the unique benefits of H-PACT for persons who are homeless. Finally, lack of random assignment limits causal conclusions. It is possible that unmeasured differences across groups in patient preference or motivation could account for our observation of more positive experiences within H-PACT versus other primary care teams.
This is a first national study to document positive healthcare experiences within a PCMH model tailored to the clinical and social service needs of homeless Veterans. The significance of these findings is underscored by prior literature documenting substantial patient and health system benefits associated with positive care experiences.46,47 The pro-active and compassionate philosophy of caring for vulnerable populations that is fostered by VHA through the H-PACT initiative is likely a factor leading to positive healthcare experiences of homeless Veterans. This philosophy, and the lessons learned from H-PACT, can be scaled throughout VHA and form the basis for caring for vulnerable patients in other healthcare settings.
Supplementary Material
Acknowledgements and Disclosure of Funding:
Research reported in this publication was supported by the Department of Veterans Affairs, Veterans Health Administration, National Center on Homelessness among Veterans; the VISN19 and VA Salt Lake City Health Care System’s Vulnerable Veteran – Innovative PACT (VIP) Initiative; the VA Office of Academic Affiliations Post-Doctoral Fellowship in Medical Informatics (TMI 95-660); and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538 and KL2TR002539. Dr. Kertesz’s (IIR 15-095) and Dr. Gundlapalli’s (IIR 12-084) efforts were supported under VA Health Services Research & Development Grants. Resources were provided by the Informatics, Decision Enhancement and Analytic Sciences Center (IDEAS 2.0), VA Salt Lake City Health Care System, Salt Lake City, UT, USA. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the National Institutes of Health, or the United States government. The supporting organizations had no role in the preparation, review, or approval of the manuscript or decision to submit the manuscript for publication. Preliminary study results were presented as a poster at the 2018 AcademyHealth Annual Research Meeting in Seattle, WA.
Footnotes
Conflict of Interest: No potential conflicts exist.
References
- 1.Anhang Price R, Elliott MN, Zaslavsky AM, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev 2014;71(5):522–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med 2011;9(2):100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making 2015;35(1):114–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villani J, Mortensen K. Patient-provider communication and timely receipt of preventive services. Prev Med 2013;57(5):658–663. [DOI] [PubMed] [Google Scholar]
- 5.Stevens GD, Shi L, Vane C, Peters AL. Do experiences consistent with a medical-home model improve diabetes care measures reported by adult medicaid patients? Diabetes Care 2014;37(9):2565–2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lebrun-Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: Findings from the 2009 patient survey. Health Serv Res 2013;48(3):992–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Serv Res 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 8.Chwastiak L, Tsai J, Rosenheck R. Impact of health insurance status and a diagnosis of serious mental illness on whether chronically homeless individuals engage in primary care. Am J Public Health 2012;102(12):e83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA 2001;285(2):200–206. [DOI] [PubMed] [Google Scholar]
- 10.Baggett TP, Hwang SW, O'Connell JJ, et al. Mortality among homeless adults in boston: Shifts in causes of death over a 15-year period. JAMA Intern Med 2013;173(3):189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steward J, Holt CL, Pollio DE, et al. Priorities in the primary care of persons experiencing homelessness: Convergence and divergence in the views of patients and provider/experts. Patient Pref Adherence 2016;10:153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Department of Housing and Urban Development. 2018. PIT estimates of veteran homelessness in the U.S. 2018; https://www.hudexchange.info/resource/5772/2018-pit-estimate-of-veteran-homelessness-in-the-us/. Accessed Nov 8, 2018.
- 13.O'Toole TP, Pirraglia PA, Dosa D, et al. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med 2011;26 Suppl 2:683–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: Associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Internal Medicine 2014;174(8):1350–1358. [DOI] [PubMed] [Google Scholar]
- 15.Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care 2013;19(7):e263–272. [PubMed] [Google Scholar]
- 16.VA Office of Public Affairs. Fact sheet: VA programs for homeless veterans. Washington, DC: U.S. Department of Veterans Affairs; 2018. [Google Scholar]
- 17.O'Toole TP, Johnson EE, Borgia M, et al. Population-tailored care for homeless veterans and acute care use, cost, and satisfaction: A prospective quasi-experimental trial. Prev Chronic Dis 2018;15:E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gabrielian S, Gordon AJ, Gelberg L, et al. Building primary care medical homes for homeless veterans at 3 VA facilities. Fed Pract 2014;31(10):10–19.30369784 [Google Scholar]
- 19.O'Toole TP, Bourgault C, Johnson EE, et al. New to care: Demands on a health system when homeless veterans are enrolled in a medical home model. Am J Public Health 2013;103 Suppl 2:S374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: The Veterans Health Administration's "Homeless Patient Aligned Care Team" program. Prev Chronic Dis 2016;13:E44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones AL, Thomas R, Hedayati DO, Saba SK, Conley J, Gordon AJ. Patient predictors and utilization of health services within a medical home for homeless persons. Subst Abus 2018. doi: 10.1080/08897077.2018.1437500. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Gundlapalli AV, Redd A, Bolton D, et al. Patient-aligned care team engagement to connect veterans experiencing homelessness with appropriate health care. Med Care 2017; 55(9) Suppl 2:S104–S110. [DOI] [PubMed] [Google Scholar]
- 23.Behl-Chadha B, Savageau JA, Bharel M, Gagnon M, Lei PP, Hillerns C. Comparison of patient experience between a practice for homeless patients and other practices engaged in a patient-centered medical home initiative. J Health Care Poor Underserved 2017;28(3):1151–1164. [DOI] [PubMed] [Google Scholar]
- 24.Kertesz SG, Holt CL, Steward JL, et al. Comparing homeless persons' care experiences in tailored versus nontailored primary care programs. Am J Public Health 2013;103 Suppl 2:S331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.VHA Office of Analytics and Business Intelligence. The shep patient centered medical home (PCMH) survey technical specifications. Washington DC: Department of Veterans Affairs; 2012. [Google Scholar]
- 26.Peterson R, Gundlapalli AV, Metraux S, et al. Identifying homelessness among veterans using va administrative data: Opportunities to expand detection criteria. PLoS One 2015;10(7):e0132664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones AL, Hausmann LR, Kertesz SG, et al. Differences in experiences with care between homeless and nonhomeless patients in Veterans Affairs facilities with tailored and non-tailored primary care teams. Med Care 2018;56(7):610–618. [DOI] [PubMed] [Google Scholar]
- 28.VHA Support Service Center (VSSC). Vast snapshot - VHA station listing reports documentation. Washington, DC: U.S. Department of Veterans Affairs; 2017. [Google Scholar]
- 29.Agency for Healthcare Research and Quality. What's available for the CAHPS Clinician & Group Survey 3.0. Rockville, MD: Agency for Healthcare Research and Quality; November 12, 2015. [Google Scholar]
- 30.Hays RD, Berman LJ, Kanter MH, et al. Evaluating the psychometric properties of the CAHPS patient-centered medical home survey. Clin Ther 2014;36(5):689–696 e681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scholle SH, Vuong O, Ding L, et al. Development of and field test results for the CAHPS PCMH survey. Med Care 2012;50 Suppl:S2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hausmann LR, Gao S, Mor MK, Schaefer JH Jr., Fine MJ. Understanding racial and ethnic differences in patient experiences with outpatient health care in Veterans Affairs medical centers. Med Care 2013;51(6):532–539. [DOI] [PubMed] [Google Scholar]
- 33.Hausmann LR, Gao S, Mor MK, Schaefer JH Jr., Fine MJ. Patterns of sex and racial/ethnic differences in patient health care experiences in U.S. Veterans Affairs hospitals. Med Care 2014;52(4):328–335. [DOI] [PubMed] [Google Scholar]
- 34.Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD. Adjusting for subgroup differences in extreme response tendency in ratings of health care: Impact on disparity estimates. Health Serv Res 2009;44(2 Pt 1):542–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weech-Maldonado R, Elliott MN, Oluwole A, Schiller KC, Hays RD. Survey response style and differential use of CAHPS rating scales by Hispanics. Med Care 2008;46(9):963–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burnett-Zeigler I, Zivin K, Ilgen MA, Islam K, Bohnert AS. Perceptions of quality of health care among veterans with psychiatric disorders. Psychiatr Serv 2011;62(9):1054–1059. [DOI] [PubMed] [Google Scholar]
- 37.Campbell JL, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients' assessments of primary health care. Qual Health Care 2001;10(2):90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones AL, Hausmann LRM, Haas GL, et al. A national evaluation of homeless and nonhomeless veterans' experiences with primary care. Psychol Serv 2017;14(2):174–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol 2011;64(7):749–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frayne SM, Miller DR, Sharkansky EJ, et al. Using administrative data to identify mental illness: What approach is best? Am J Med Qual 2010;25(1):42–50. [DOI] [PubMed] [Google Scholar]
- 41.Bao Y, Sturm R. How do trends for behavioral health inpatient care differ from medical inpatient care in U.S. community hospitals? J Ment Health Policy Econ 2001;4(2):55–63. [PubMed] [Google Scholar]
- 42.O'Toole TP, Johnson EE, Redihan S, Borgia M, Rose J. Needing primary care but not getting it: The role of trust, stigma and organizational obstacles reported by homeless veterans. J Health Care Poor Underserved 2015;26(3):1019–1031. [DOI] [PubMed] [Google Scholar]
- 43.Zerger S, Bacon S, Corneau S, et al. Differential experiences of discrimination among ethnoracially diverse persons experiencing mental illness and homelessness. BMC Psychiatry 2014;14:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asgary R, Naderi R, Gaughran M, Sckell B. A collaborative clinical and population-based curriculum for medical students to address primary care needs of the homeless in new york city shelters: Teaching homeless healthcare to medical students. Perspect Med Educ 2016;5(3):154–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kertesz SG, Pollio DE, Jones RN, et al. Development of the primary care quality-homeless (PCQ-H) instrument: A practical survey of homeless patients' experiences in primary care. Med Care 2014;52(8):734–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bundesmann R, Kaplowitz SA. Provider communication and patient participation in diabetes self-care. Patient Educ Couns 2011;85(2):143–147. [DOI] [PubMed] [Google Scholar]
- 47.Keller AO, Gangnon R, Witt WP. The impact of patient-provider communication and language spoken on adequacy of depression treatment for U.S. Women. Health Commun 2014;29(7):646–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


