Abstract
Background:
As per the World Health Organization (WHO) Global Report 2017, among the 9.6 million cases of tuberculosis (TB) that occur annually in the world, 2.8 million are found in India. TB is the biggest killer in the 15 to 49 years age group—an age range during which people are the most productive. It is a disease that creates and thrives in poverty. Several studies have shown that TB has a negative impact on the socioeconomic status of patients. Limited data are available on the long-term impact of this disease on the families of patients.
Aims:
This study aimed to analyze the impact of TB on the socioeconomic condition and educational status of the family members of patients and the nutritional status of children younger than 12 years in the family of the patient.
Methods:
This was a retrospective cohort study conducted in Vellore, Tamil Nadu, India in the month of March 2017. The exposed group consisted of families with a member who completed treatment for TB in the past 5 years obtained from two tuberculosis units under the Revised National Tuberculosis Control Programme. The unexposed group was composed of families in the same neighborhood as the exposed families, matched for the age of one child.
Results:
Upon analysis, the multifaceted impact of TB led to an increased risk of “financial crises,” delayed and disrupted education among children, and wasting among children younger than 5 years (as measured by weight-for-height Z scores). Older children and adults were also at a higher risk of being undernourished as assessed by BMI-for-age Z scores and BMI, respectively. Reduced social participation as a marker of stigma was found to be higher but not statistically significant.
Conclusions:
This study found that despite the obvious multifaceted impact of TB on the family, the screening and protective measures often fail to encompass the scope of the disease. These are of great importance to the primary physician, often the only contact of the medical fraternity with the family members of patients.
Keywords: Family, impact, nutrition, socio-economic, tuberculosis
Introduction
According to the World Health Organization (WHO) Global Report 2019,[1] tuberculosis (TB) is the biggest killer among the most productive age group of 15 to 49 years and accounts for the highest number of workdays lost each year. It is said that TB thrives in poverty and creates poverty. Studies around the globe have shown that the poorest families are the worst affected by TB[2,3] and this, in turn, perpetuates a cycle of poverty in the family. The WHO noted in their Global Report, 2019[1] that the most prevalent factor to which development of TB could be attributed was undernourishment, followed by smoking, alcohol abuse, diabetes, and HIV coinfection.
With an incidence of 199 per 100,000 population, India accounts for 25% of the global TB burden and has one of the highest rates of incidence and transmission of TB.[1] In addition, the WHO report also makes note of the reduced incidence of TB in India over the last decade, from 268 per 100,000 in 2009. While demonstrating the efficacy of control measures implemented, it also illustrates the large population previously afflicted with TB who continue to bear the burden of the disease on their socioeconomic well-being to this day.
Various studies conducted all over the country have demonstrated a significant effect on the economic and social domains of patients' lives.[4,5,6] Considering the immense burden of TB in India, there has been a multitude of studies done on the disease and its impact on the population that it affects. One of the first studies examining the economic impact of TB on its patients was performed by the Tuberculosis Research Centre of the Indian Council of Medical Research;[4] It revealed that the total cost and indirect cost are found to be relatively high in the treatment of TB with an average period of loss of wages for 3 months. The caregiving activity of female patients had significantly decreased and one-fifth of the school children had discontinued their schooling.
With diseases like TB, which inculcate social stigma, the family members may experience shame, resentment, and guilt. A study in Nepal looking exclusively at the causes of stigma and discrimination associated with the disease found that both patients and families preferred to isolate themselves from mainstream society.[7] Prevalent misconceptions in the community include TB being a divine curse and a proposed link between TB and high-risk behavior. According to a study published in the Indian Journal of Tuberculosis,[1] children were found to bear serious disadvantages while hailing from TB-affected families. The impact of TB on these children ranged from school absenteeism, dropouts, decreased care at home, to being obliged to take up jobs. Similar results were obtained from a study performed in a state school in Punjab, suggesting that these effects transcend geographical borders.[8]
The National Tuberculosis Elimination Program (NTEP) aims at supporting the costs incurred by patients toward diagnostics and treatment of TB, which greatly reduces the burden of the disease on the patient as well as reduces the economic impact of the disease on the household. However, it does not address the wide-ranging impact of TB on the family, which is often a forgotten, indirect victim of the influence of diseases despite playing a pivotal role in patient care. We looked at how this disease affects the family members of the patients. In addition, we observed children in the families (affected by TB) for continuing effects of this deadly disease, which seem to exist much after its cure. Hence, the objectives of this study included assessing the impact of TB on the economic and educational status of the families of patients, understanding the multifaceted social stigma faced by families, and recognizing the effect of TB on the nutritional status of children younger than 12 years in the family
Methodology
A retrospective cohort study was done in Vellore, one of the largest districts in Tamil Nadu, in the southern part of India between 14 March, 2017 and 31 March, 2017. In Vellore, 57% of the population lives in rural areas, and TB services are provided by seven tuberculosis units (TUs).[9] This study included patients from an old Community Health and Development TU and Pudupadi TU by the convenience sampling technique. We calculated a required sample size of 40 patients in each study arm (exposed and unexposed). The exposed group comprised families of people diagnosed with TB in the past, who have completed treatment for TB in the last 5 years, and with children younger than 12 years of age. The unexposed group consisted of families residing in the neighborhood of the exposed group, matched for the age of one child (±3 months for children younger than 5 years and ±6 months for children older than 5 years). Families unwilling to participate or who were currently undergoing treatment were excluded.
To address the complex ethical considerations associated with a stigmatized disease, such as TB, all the families of patients were contacted over telephone by a care team member and permission was taken before visiting the neighborhood. Informed consent was taken before obtaining any information from the patients and the interviewer was accompanied by a TB treatment supporter known to the family.
An interviewer-administered, semistructured, pilot-tested questionnaire was used to assess the economic and social components related to stigma.
For this study, a “financial crisis” was defined as adversity causing a change in schooling, nutrition, or spending. The anthropometric assessment was used to measure nutritional status using a stadiometer/inch tape and an electronic weighing machine. The Annual Status of Education Report (ASER) of 2012 was used to assess the current scholastic performance among children. “Wasting” was defined, in accordance with WHO recommendations, as weight-for-height Z score of −2 standard deviations.[10]
Data management: Data entry was done using EpiData, version 3.1, and analysis was conducted using the Statistical Package for Social Sciences, version 23. Continuous variables are expressed as mean and standard deviations while categorical variables are expressed as numbers and percentages. A Chi-square test was done to assess the association and relative risk with 95% CI was calculated to assess the strength of association.
This project was done in part by medical students as a part of the community health program under the guidance of the community health department. The approval of members representing the Christian Medical College Institutional Review Board was sought before the initiation of the project.
Results
Analysis of the baseline characteristics of this study's exposed and unexposed populations revealed that they were similar in age and sex distribution, as shown in Table 1. The mean age among the exposed families was 25.9 years (SD 18.18) and among unexposed families was 24.1 years (SD 17.88). Among children, the most populous age group was between 5 and 9 years in both exposed and unexposed groups, while among adults the most populous age group was between 25 and 29 years both in exposed and unexposed groups. Distribution by sex was also similar among the groups, with 52.8% and 52.17% males among the exposed and unexposed groups, respectively. Among those aged 18 years or older, less than a fifth were unmarried in both groups (79.2% among exposed and 82.8% among unexposed were married). Among the exposed families, 42 individuals suffered major illnesses in the past, of which, 38 suffered from TB. Eight individuals among the unexposed families suffered illnesses, including thyroid disease, asthma, diabetes, cerebrovascular accidents, and cardiovascular disease, with no incidence of TB in those families.
Table 1.
Demographic details of the study population (n= 341)
| Characteristic | Exposed (n=180) | Unexposed (n=161) | |
|---|---|---|---|
| Age (Years) | |||
| Mean | 25.9 (SD 18.18) | 24.1 (SD 17.88) | |
| Median | 24 | 25 | |
| Sex, n (%) | |||
| Male | 95 (52.8) | 84 (52.17) | |
| Female | 85 (47.2) | 77 (47.83) | |
| Married (≥18 years), n (%) | 80 (79.2) | 77 (82.8) | |
| Education (≥14 years, currently not studying), n (%) | |||
| Uneducated | 12 (13.3) | 11 (13.4) | |
| Primary and high school | 75 (83.3) | 62 (75.6) | |
| Above high school | 3 (3.3) | 9 (10.9) | |
| Occupation (≥14 years), n (%) | |||
| Not gainfully employed | 28 (17.64) | 36 (27.1) | |
| Unskilled | 21 (13.2) | 17 (12.8) | |
| Semiskilled | 11 (6.9) | 7 (5.3) | |
| Skilled | 27 (16.9) | 15 (11.3) | |
| Semiprofessional and above | 8 (5) | 17 (12.9) |
We found that 61.1% of exposed families had a financial crisis, compared with only 38.7% of the unexposed families. Of the families under a financial crisis, 75% of the exposed families took loans, compared with 61.3% of unexposed families, although only 18.5% of the exposed families were able to repay their debts. On analysis of the economic impact, almost half (47.2%) of those exposed had a reduction of income, of which, the majority (56%) was because of health-related causes. Individuals in the exposed group are more than twice as likely to experience a reduction in income compared with the individuals in the unexposed group, which was statistically significant (P = 0.05). Such families were also 1.5 times more likely to experience a financial crisis, which we defined as any difficulty necessitating a change in schooling, nutrition, or spending. They were more likely to have taken loans than unexposed families (75% vs 61.3%) and were less likely to repay them (10.5% vs 18.5%).
Among children under the age of 5 years from the exposed families, 29% had normal WAZ, while 43% were marginally wasted, 14% were moderately wasted, and another 14% were severely wasted. Among unexposed families, 77% had normal WAZ, with only 18% being marginally wasted and 5% being moderately wasted.
Among children aged between 5 and 18 years in the exposed group, 26% had normal BMI-for-age Z scores, while 27% had marginally low Z scores, 27% had moderately low Z scores, and 20% had severely low Z scores. Among the BMI-for-age Z scores of the unexposed, 48% were normal, 21% were marginally low, 14% were moderately low, and 17% were severely low.
A low BMI was found in 30% of exposed adults aged above 18 years, while only 11% of the unexposed adults were found to be underweight.
Children from exposed families in the age group of 5 to 18 years had a 1.4 times higher chance of having a low BMI-for-age (RR 1.4 [95% P=0.051, CI- 0.999-1.963). Children younger than 5 years of age from exposed families were more than 3 times likely to be wasted (RR 3.143 [95% CI 1.359–7.271]; P = 0.0075). The nutritional impact of TB on these families is summarised in Table 2.
Table 2.
Nutritional status of the study population (n=341*)
| Nutritional index | Among exposed | Among unexposed |
|---|---|---|
| Weight-for-height Z score (<5 years), n (%) | ||
| Normal | 4 (29) | 17 (77) |
| Marginally wasted (−1 to −2 SD) | 6 (43) | 4 (18) |
| Moderately wasted (−2 to −3 SD) | 2 (14) | 1 (5) |
| Severely wasted (more than −3 SD) | 2 (14) | 0 |
| BMI-for-age Z score (5-18 years), n (%) | ||
| Normal | 12 (26.3) | 20 (48) |
| Marginally low | 12 (26.3) | 9 (21) |
| Moderately low | 12 (26.3) | 6 (14) |
| Severely low | 9 (20) | 7 (17) |
| BMI (>18 years), n (%) | ||
| Underweight | 17 (31) | 6 (11) |
| Normal | 28 (50) | 33 (58) |
| Overweight | 8 (14) | 15 (26) |
| Obese | 3 (5) | 3 (5) |
*n varies according to the parameter studied
Family members above 18 years of age were also at a significantly higher risk of being underweight, both inclusive and exclusive of the index cases (RR 2.884 [95% CI 1.227–6.778]; P = 0.0151).
The education status of individuals aged above 14 years was similar among exposed and unexposed families—11.8% of the exposed were educated while 11.7% of the unexposed were uneducated. Among the exposed who were educated, 73.5% were educated up to high school, while 65.9% of the unexposed were educated up to high school. Children from exposed families were over 3 times more likely to delay joining the school and over 1.5 times more likely to disrupt schooling. The economic burden of schooling is considerably reduced because of the well-functioning government school system in the community.
Our assessment of the social impact of TB showed that 7.7% of the affected people were restricted from participating in social events, compared with 3% in the unexposed group. People from the exposed families were at a 2.55 times higher risk of reducing their participation in social events. The social stigma associated with the disease among family members of patients is summarized in Figure 1. The relative risks of various socioeconomic, nutritional and educational factors are summarized in Table 3.
Figure 1.
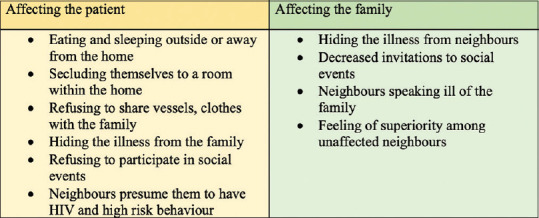
Social stigma associated with tuberculosis
Table 3.
Relative risk of exposed factors n=67 families, 341 individuals*
| Marker | Exposed | Unexposed | Risk Ratio | Confidence Interval | P |
|---|---|---|---|---|---|
| Economic Impact | |||||
| Reduction in income (n=67) | 17 (47.2%) | 13 (22.6%) | 2.091 | 1.001, 4.373 | 0.05 |
| Financial crisis (n=67) | 22 (61.1%) | 12 (38.7%) | 1.574 | 0.928, 6.666 | 0.072 |
| Taken loans (n=67) | 27 (75%) | 19 (61.3%) | 1.224 | 0.873, 1.715 | 0.240 |
| Nutritional Impact | |||||
| Low WHZ (< 5 year olds) (n=36) | 10 (71.4%) | 5 (22.7%) | 3.143 | 1.359, 7.271 | 0.007 |
| Low BMI for age Z score (5-18 years) (n=97) | 33 (73.3%) | 22 (52.3%) | 1.4 | 0.999, 1.963 | 0.051 |
| Low BMI (including index cases) (n=113) | 17 (30.3%) | 6 (10.5%) | 2.884 | 1.227, 6.778 | 0.015 |
| Low BMI (excluding index cases) (n=87) | 9 (30%) | 6 (10.5%) | 2.850 | 1.120, 7.249 | 0.028 |
| Educational Impact | |||||
| Delay in joining school(n=112) | 4 (6.3%) | 1 (2%) | 3.111 | 0.359, 26.957 | 0.303 |
| Disruption of schooling (n=112) | 4 (6.3%) | 2 (4.1%) | 1.556 | 0.297, 8.147 | 0.601 |
| Social Impact | |||||
| Reduced social participation (n=67) | 14 (7.7%) | 5 (3%) | 2.552 | 0.940, 6.932 | 0.066 |
*n varies according to the parameter studied
35% of under-5 children in exposed families were screened for TB. Among those that were screened, only a fifth received prophylaxis.
Discussion
This study found that TB has long-lasting and wide-ranging effects on the families of patients. This spans across economic, social, educational, and nutritional aspects.
According to a study done in Chennai, Tamil Nadu, India by Geetharamani et al., 11% of children in affected families dropped out of school, 34% could not afford books, and 20% had to take up jobs, with 12% discontinuing studies.[4] These observations were similar to those in a study by Chand et al. from Amritsar, Punjab, India, which found that 12% of children discontinued their studies and 7% had to take up jobs.[5] In our study, 6.3% of children in exposed families experienced delays in school admission, compared with 2.1% of unexposed families. Similarly, high rates of school disruption and dropout were noted. This aspect is expected to have been addressed by measures taken by the Government of India to provide primary education up to 15 years of age universally available, free of cost.
The concept that childhood nutrition directly reflects the socioeconomic conditions prevalent during the period of growth is not particularly novel and has been previously demonstrated by several authors.[11] Hence, approaching the socioeconomic impact of chronic disease, such as TB, comparing the growth of children from affected families with age-matched controls in the same localities provides a reliable marker of its effects. As we included families exposed to TB in the last 5 years, children in the age group of 5 to 18 years would have been directly affected by the economic impact of the exposure. Hence, low BMI-for-age in this age group is a good marker of the direct effect of the disease on the family.[10,12,13] We found that children in the exposed group were 1.4 times more likely to have low BMI-for-age.
Children under the age of 5 years are less likely to have been directly affected by the impact of TB in a family member, and their nutritional status is better indicative of the long-standing impact of TB on the family, persisting even after it is cured. Children who have a family member affected by TB were more than 3 times as likely to be wasted than those who did not, which reflects that they have been malnourished in the recent past.[10,11] Such profound long-term impacts of TB on the nutritive status of family members has not been described in prior literature.
Exposure to TB was found to be a significant risk factor for low BMI in members of the family above the age of 18 years as well. This was significant even upon excluding the index cases themselves, eliminating any form of inclusion bias.
Nikshay Poshan Yojana is a scheme established in 2016 by the Government of India based on the premise that curing TB requires not only effective drugs but also nutritious food.[16,17,18] This scheme provides money for food for the patient in the form of incentives for taking TB treatment. It is commendable that it addresses the impact of TB on the nutrition of the patient and the role of nutrition in fighting disease. However, it does not acknowledge the effect of the disease on the nutrition of the family members of the patient, which as we demonstrate, are significant.
In previously published articles, it has been found that TB patients face various kinds of social restraints and exclusion from their family and society as a whole.[7,14] Results from this study showed that members of exposed families were more socially restricted than those in unexposed families. A better reflection of the social impact of TB is perhaps the qualitative data we obtained by personal interviews of select cases, which highlight the rampant superstition and misinformation associated with TB. On more than one occasion, we encountered families that forced patients who suffered from TB to cook food in and eat from separate utensils, usually away from the family. In one particularly unfortunate situation, the patient was made to stay in a shed a short distance away from his house, and his meeting with other members of the family was severely restricted. It is important to note that this behavior persisted long after the course of treatment was completed and patients were confirmed to be sputum negative.
Less dramatic, but much more prevalent was most families' unwillingness to disclose, and, in some cases, denial of the history of TB, which they felt would lead to alienation of the family from the rest of the community. Many families noted that their community often associated TB with HIV, low hygiene, and disreputable behavior, which is consistent. As families were deterred from revealing the presence of TB to the community in the first place, it may go a long way in explaining why we did not find as high a degree of social restriction as was expected.
In addition, we found the screening and prophylaxis of family members for TB to be highly inadequate. While the Revised National Tuberculosis Control Programme guidelines recommend 100% of under-five children exposed to TB contact be screened for the disease, only 35% were screened. Of these, only a fifth received prophylaxis. This falls within the estimate by the WHO Global Report 2019, which classifies India under the 0% to 24% under-five preventive treatment coverage.
Hence, it appears that while the national and global focus for TB seems to be aimed at its eradication, as evidenced by the lofty goals set by the National Strategic Plan for Tuberculosis (2017–2025) and the End TB Strategy by the WHO in 2014,[15] the families that have experienced significant financial and social catastrophe because of TB must not be forgotten. It must be noted that families of patients with TB are major stakeholders, and they must not be left behind in our quest to cure those currently burdened with the disease.
Primary care physicians form a major point of contact between the patient, community, and healthcare system and, by extension, are responsible for the health of the family members of the patient. Physicians in their position are primed to ensure that families of patients with TB do not fall victim to its debilitating effects on economic status, nutrition, and, by extension, the health of the members. Thus, these findings are significant in informing their decisions when aiding families with patients suffering from TB.
Conclusions and Key Messages
Our findings were consistent with our hypothesis that TB as a disease ravages not just the individual but also impacts the entire family with regard to social, economic, educational, and nutritional aspects. This exposure leaves a long-standing impact and alters the economic trajectory of the family in a way that may be irreversible even after the disease is cured. This is quite evident when considering its effect on the nutritional status of all age groups. The effect of TB on families extends beyond the support that is assumed to be provided by the public distribution system and other government schemes like the mid-day meal scheme. New measures, such as Nikshay Poshan Yojana, appear to address some aspects of this, and ambitious goals to eliminate TB will further reduce the burden of the disease in India. Screening and provision of prophylaxis to members of exposed families was also found to be grossly inadequate.
Limitations
While this study assessed the rate of school discontinuation, it did not examine a change of school from private to public schools, which may have reflected some degree of educational impact. As a retrospective study, it is subject to the usual limitations of data assessed via recall.
Key Messages
Tuberculosis ravages patients and their families alike.
There is a significant long-term impact, including adverse effects on the nutritional, economic, and social status of the families.
Public health programs need to formulated while closely considering the families of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. Vinod Abraham and the department of community health, CMC Vellore.
References
- 1.Page 196, The WHO Global Report, 2019. Available from: https://www.who.int/tb/publications/global_report/gtbr2017_main_text.pdf .
- 2.Noah N. Understanding Public Health. Open University Press, London School of Hygiene & Tropical Medicine; [Google Scholar]
- 3.Jassal MS, Bishai WR. Epidemiology and challenges to the elimination of global tuberculosis. Clin Infect Dis. 2010;50:S156–64. doi: 10.1086/651486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geetharamani S, Muniyandi M, Rajeswari R, Balasubramanian R, Theresa X, Venkatesan P. Socio-economic impact of parental tuberculosis on children. Indian J Tuberc. 2001;48:91–4. [PubMed] [Google Scholar]
- 5.Chand N, Singh T, Khalsa JS, Verma V, Rathore JS. A study of socio-economic impact of tuberculosis on patients and their family. CHEST. 2004;126(4 Suppl):832S. [Google Scholar]
- 6.Ananthakrishnan R, Jeyaraj A, Palani G, Sathiyasekaran BWC. Socioeconomic impact of TB on patients registered within RNTCP and their families in the year 2007 in Chennai, India. Lung India. 2012;29:221–6. doi: 10.4103/0970-2113.99103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: A qualitative study. BMC Public Health. 2007;7:211. doi: 10.1186/1471-2458-7-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh K, Kaur RP, Bhushan B. Socio-Economic Impact of Parental Tuberculosis on School Going Children: Study at State Medical College and Hospital, Punjab, India. JMSCR. 2019;7:1043–50. [Google Scholar]
- 9.Veesa KS, John KR, Moonan PK, Kaliappan SP, Manjunath K, Sagili KD, et al. Diagnostic pathways and direct medical costs incurred by new adult pulmonary tuberculosis patients prior to anti-tuberculosis treatment-Tamil Nadu, India. PLoS One. 2018;13:e0191591. doi: 10.1371/journal.pone.0191591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. WHO Child Growth Standards: Length/Height-For-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Geneva: World Health Organization; 2006. [Google Scholar]
- 11.Frongillo EA, Jr, de Onis M, Hanson KM. Socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting of children. J Nutr. 1997;127:2302–9. doi: 10.1093/jn/127.12.2302. [DOI] [PubMed] [Google Scholar]
- 12.Stewart CP, Iannotti L, Dewey KG, Michaelsen KF, Onyango AW. Contextualizing complementary feeding in a broader framework for stunting prevention. Matern Child Nutr. 2013;9(Suppl 2):27–45. doi: 10.1111/mcn.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. WHO Child Growth Standards: Head Circumference-for-Age, Arm Circumference-for-Age, Triceps Skinfold-for-Age and Subscapular Skinfold-for-Age: Methods and Development. Geneva: World Health Organization; 2007. [Google Scholar]
- 14.Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34–42. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uplekar M, Weil D, Lonnroth K, Jaramillo E, Lienhardt C, Dias HM, et al. ; on behalf of WHO's Global TB Program. WHO's new End TB Strategy. Lancet. 2015;385:1799–801. doi: 10.1016/S0140-6736(15)60570-0. [DOI] [PubMed] [Google Scholar]
- 16.The National Strategic Plan for Tuberculosis Elimination. RNTCP 2017-2025 [Google Scholar]
- 17.Nikshay Poshan Yojana. Central TB Division tbcindiagovin [Google Scholar]
- 18.Eradicating TB by 2025. Ministry of Health and Family Welfare. Available from: https://pibgovin/PressreleaseshareaspxPRID=1578926 .


