Objective:
To address which body composition (BC) measures best correlate with cardiorespiratory fitness (CRF) in firefighters and develop a model for accurate CRF estimation compared with traditional methods.
Methods:
Career firefighters had body mass index (BMI) and waist circumference (WC) measured in addition to body fat percentage (FM%) by dual-energy x-ray absorptiometry (DXA). CRF as maximum oxygen uptake (VO2max) was estimated by rowing machine and measured by indirect calorimetry in a treadmill exercise test.
Results:
Fifty two firefighters participated (92.3% men). Univariate correlations with BMI were best with WC. Univariate correlations with VO2max were best with FM%. Obesity classifications by BC measures agreed weakly at best. Multivariate analysis of several variables yielded an improved VO2max estimate (R2 = 0.70).
Conclusions:
Fire departments may benefit from more sophisticated measures of BC and CRF to evaluate firefighter fitness.
Keywords: body composition, cardiorespiratory fitness, dual-energy x-ray absorptiometry, firefighters, obesity
Firefighters are exposed to extreme metabolic and cardiopulmonary stressors in the performance of their vocation that are recognized to exceed the actual physical or environmental hazards.1 The current medical literature regarding firefighting highlights two frequently cited statistics: (1) based on body mass index (BMI), upwards of 73% to 80% of firefighters are considered overweight or obese, and (2) more than 45% of firefighter line-of-duty deaths are due to cardiovascular events.2
This finding regarding BMI has been widely reported in the US media after being published in a 2014 article in the journal Preventing Chronic Disease.3 Such a finding is particularly relevant to firefighters given that there are recommended cardiorespiratory performance standards for firefighters, commonly accepted as 12 metabolic equivalents (METs) or maximum oxygen consumption during aerobic exercise (VO2max) of 42 mL O2/kg of body weight/min.4 As a consequence, failure to meet such a standard may limit a firefighter's ability to perform (or be employed) in full-duty tasks based on individual fire station requirements, though only 27% of fire departments have been found to have programs focused on fitness and health.5,6 Few professions, other than elite athletes, require this level of cardiorespiratory fitness (CRF), especially given that full turnout gear weighs approximately 50 pounds. In addition, CRF is increasingly recognized as a vital component of health, wellness, and longevity, and has been argued as an important component of annual clinical evaluation.7
While elevated BMI is associated with cardiovascular disease morbidity and mortality, BMI has been demonstrated to be a non-specific metric of body composition. BMI performs well as a population-level measure but suboptimally as an individual-level measure. The misclassification of younger adults as well as firefighters as overweight and obese based on BMI has been discussed in several studies.8–12 These studies utilized bioimpedance testing or skin calipers for body fat percentage (fat mass percentage, FM%) measurement, methods known to have significant levels of error in terms of false positives and false negatives. A series of these studies cite a single article with a sample size of 39 individuals as validation of bioimpedance in comparison to dual-energy x-ray absorption (DXA), but also report DXA as the gold standard for FM% measurement.8–10,13 This inaccuracy of FM% compared with BMI was addressed thoroughly in one study of US firefighters, demonstrating the potential for false positive and false negative identification of obesity in this population.10 The importance of misclassification of obesity was demonstrated in a systematic review by Flegal et al,14 where it was reiterated that all-cause mortality is increased in all grades of obesity in combination relative to normal weight individuals, but that in substratification of obesity classification, grade 1 obesity (BMI 30 to less than 35) demonstrated no elevated mortality and overweight (BMI 25 to less than 30) individuals were associated with a lower all-cause mortality.
DXA is a widely-available technology that is relatively inexpensive compared with other diagnostic technologies, is safe, and can accurately measure BF%. DXA studies can be completed in less than 10 minutes and provide data that is valid and reproducible over time. The radiation from a DXA scan is less than that received from routine environmental exposure in a single day. Americans typically receive approximately 3.0 milliSieverts (mSv) of radiation exposure annually from cosmic radiation, household radon, and other environmental sources. This does not include elective diagnostic imaging sources. The radiation exposure of a DXA scan is ∼0.005 mSv, about a tenth of that from a single chest x-ray (CXR).15 By comparison a CT scan of the pelvis, chest or abdomen can expose the patient to 6.0 to 10.0 mSv in one study (the equivalent of 2 to 3 years of environmental exposure in a single medical study).16 The precept of As Low As Reasonably Achievable (ALARA) in order to minimize radiation exposure is easily honored in the case of DXA scanning due to the extremely low-dose exposures.17 Mattila et al18 have demonstrated the practical utility of DXA in young new male military conscripts with strong prediction of 12-minute running test performance (a surrogate of VO2max) in correlation with FM% and without correlation with BMI.
The misclassification of obesity via BMI is also significant as it pertains to CRF, to the extent that body composition and CRF both have age- and sex-specific changes, yet BMI as a measure is comprised only of height and weight. As a consequence, the need for appropriate BMI reference ranges in the context of age and sex has been identified and has been studied, with FM% changing independently relative to age and sex, regardless of changes in BMI.19,20 Similarly, the need for VO2max references ranges for CRF relative to age and sex have been discussed and re-evaluated in recent years, as these data can inform population health decision-making, including in the workplace.21,22 Specifically, physical activity, CRF, and obesity have been demonstrated to impact work performance, absenteeism, and presenteeism.23 This is significant for firefighters as their recommended CRF standard of 42 mL O2/kg/min does not account for the age and sex of the firefighter, thus having the potential to misclassify a firefighter as fit or unfit inappropriately.4
As such, this study, representing the initial phase of a larger observational study, aimed to address which body composition methods best correlate with CRF in firefighters. This initial phase of the study hypothesized that FM% and lean body mass percentage (lean mass percentage, LM%) correlate higher with measured CRF than traditional body composition methods, such as BMI or waist circumference (WC). Additionally, we hypothesized that these data, in conjunction with rowing machine-based CRF estimates and demographic, employment, physical activity, and medical history data, can comprise an effective means of estimating firefighter CRF.
The second phase of this study will seek to confirm the initial phase findings and, in addition, empirically test the correlations of body composition and CRF metrics with measures of cardiovascular risk. The developed CRF estimate will additionally undergo a cost analysis in comparison to direct measurement of VO2max.
METHODS
This study was a cross-sectional correlational study with individual-level measurements of cardiorespiratory fitness (CRF) and body composition for an urban fire department in the Twin Cities metropolitan area in Minnesota. The study design, methods, and implementation protocols were reviewed and approved by an Institutional Review Board (IRB Project Number A16-667).
Data Collection
All firefighters within the study fire department were sent a study invitation e-mail from their fire department administration via an internal distribution list. Inclusion criteria for the study included current and unrestricted employment within the study fire department and willingness to participate in the study; pregnancy (or anticipated pregnancy) was a primary exclusion criterion due to variations in CRF during pregnancy and the exposure to radiation implicit in the study's design. No financial incentives were offered for participation in the study, however, participants were mailed their results with a brief interpretation of the data from the study physicians after all data were collected and analyzed. Participants were also offered the opportunity to meet with one of the physician study investigators after receiving their results to review them in a 15-minute individual session.
Study data were collected and managed using REDCap electronic data capture tools hosted at the primary study.24,25 REDCap (Research Electronic Data Capture, Vanderbilt University, Nashville, NT) is a secure, web-based software platform designed to support data capture for research studies.
Individuals meeting inclusion criteria who responded with interest in the study were placed onto a list and selected for participation in the order of receipt of their response until the initial phase study population size was met. Once the individuals were selected for the study, they were notified via e-mail of their participation and were asked to attend an in-person enrollment and evaluation visit at their local fire department.
The study protocol consisted of three evaluations: (1) enrollment and evaluation at the fire department training facility, (2) a treadmill-based VO2max measurement, and (3) a DXA scan for body composition measurement. These three evaluations were scheduled to occur on separate dates, and the second and third evaluations could occur independent of the scheduling of the other.
The enrollment and evaluation visit consisted of completing informed consent for the study, completing a demographic survey, having simple body composition measurements taken, and undergoing a 2000 m rowing test (Concept 2, Morrisville, VT). The demographic survey recorded information on the participant's employment history, smoking history, and physical activity according to the Nord-Trøndelag Health Study (HUNT 2) physical activity questionnaire.26 The initial evaluation included measurement of height, weight, WC, and resting heart rate. WC was measured using the iliac crests and midaxillary lines as landmarks in accordance with National Health and Nutrition Examination Survey (NHANES) procedures.27 Participants’ completion times of the 2000 m rowing test were recorded.
VO2max was estimated using two calculations provided by the rowing machine manufacturer for self-identified “highly-trained” (specified as “training level: high”) and “non-highly-trained” (“training level: low”) populations.28 Because the definition of “training level” is subjective, both of these estimates were calculated for this study. The estimate equations compute VO2max as (Y × 1000)/weight, where Y is calculated differentially based on training level (high vs low) and sex, and in the highly-trained calculation including a binary classification of weight at or below 61.36 kg in women or 75 kg in men. These VO2max estimate equations are reported as based on mask-based indirect calorimetry measurements using rowers from the same manufacturer.
Participants were then scheduled at a local health promotion clinic (Health Strategies, White Bear Lake, MN) with appropriate equipment and facilities to complete mask-based measured VO2max testing using indirect calorimetry. VO2max was measured with a CardioCoach (KORR Medical Technologies, Salt Lake City, UT) while participants underwent a treadmill-based Bruce protocol.29 Data were collected on-site and securely transmitted to the study database.
Participants were additionally scheduled to undergo a DXA scan at a local clinic within a large health system. Women participants were offered the opportunity to undergo urine pregnancy testing at the time of this scan if their pregnancy status was not known. Whole-body DXA scans were acquired on a Hologic Horizon W system (Hologic Inc., Marlborough, MA). All scans were conducted by a radiologic technologist using Hologic APEX software (version 5.6.0.4) with body composition calibration correction based on data from NHANES enabled. Calculation of body composition metrics without NHANES body composition calibration correction was performed during data analysis due to recent demonstration of FM% overestimation with use of the NHANES body composition calibration correction.30
Data Analysis
Classifications of VO2max (relative to an individual's size, expressed as mL/kg/min, as opposed to absolute VO2max measured as L/min), and classifications of obesity by BMI, WC, FM%, were applied according to reference tables published by the American College of Sports Medicine (ACSM), which classify these measures according to age and sex for VO2max and FM%, and by sex for WC.31
The ACSM classifies BMI as “underweight,” “normal,” “overweight” (BMI 25.0 to 29.9), and “obese” (BMI more than 30.0); WC as “very low,” “low,” “high” (90 to 110 cm), and “very high” (more than 110 cm); and FM% as “very lean,” “excellent,” “good,” “fair,” “poor” (between the 40th and 20th percentiles for age and sex), and “very poor” (below the 20th percentile for age and sex). To evaluate agreement of obesity classifications for various body composition measures, a sensitivity analysis was performed by constructing two classifications of obesity with differential sensitivity—more and less likely for an individual to meet the obesity classification—for each of BMI, WC, and FM%. Obesity classifiers for BMI were labeled as BMI1 (“overweight” or “obese”) and BMI2 (“obese”), for WC as WC1 (“high” or “very high”) and WC2 (“very high”), and for FM% as FM1 (“poor” or “very poor”) and FM2 (“very poor”).
Statistical Analysis
Continuous variables were visually inspected for extreme outliers and deviation from normal distribution using Q–Q plots. To evaluate correlation of BMI with other body composition metrics (WC, total fat mass [TFM], FM%, total lean mass [TLM], LM%), Pearson correlation coefficients were calculated. Agreement of obesity classifiers was measured with the Cohen (unweighted) κ coefficient, and sensitivity and specificity of obesity as a classifier were computed, using two classifications of obesity for each of BMI (BMI1 and BMI2), WC (WC1 and WC2), and FM% (FM1 and FM2).
Simple linear regression was performed for measured VO2max as a dependent variable, and estimated VO2max rower-based “highly-trained” and “not highly-trained” metrics, body composition metrics, and demographic variables as independent variables. A multivariate regression analysis was conducted against measured VO2max using non-collinear demographic, body composition, and VO2max rower-based estimates to evaluate performance of this model in accurately representing VO2max.
Statistical analyses were performed using SAS v9.4 software (SAS Institute Inc., Cary, NC). A P value (alpha) of 0.05 was considered statistically significant.
RESULTS
A total of 52 firefighters were enrolled, 48 men, 4 women (92.3% men), with 100% completion of all three evaluation components of the study. The mean age of participants was 42.8 (±8.1) years. All participants were full-time firefighters (100%), and 63.5% had a second employment. Participants could select multiple racial designations, and 84.6% of the firefighters were White, 9.6% Hispanic, 7.7% Other, 3.9% Black, 1.9% Asian. Only two individuals reported current smoking (3.9%), but less than daily; the remaining 96.1% do not currently smoke. Of all individuals, 75% reported never smoking regularly. Physical activity was evaluated by the HUNT 2 physical activity assessment and 88.2% reported over 3 hours per week of light physical activity, and 65.4% reported over 3 hours per week of heavy physical activity. No regular prescription medication use was reported by 34 individuals (65.4%). Twenty nine of the 52 firefighters (55.8%) opted to meet with a physician study investigator to individually review their results.
Body composition measures are detailed in Table 1. For men, mean BMI (kg/m2) was 28.9 (±3.9), which corresponds to being overweight; waist circumference (cm) was 98.9 (±10.3), which corresponds to the category of low waist circumference. Mean FM% as measured by DXA scan was 23.6% (±5.7), and was distributed between the very poor, poor, and fair categories, stratified by age. For women, mean BMI (kg/m2) was 26 (±2.1), which corresponded to being overweight; waist circumference (cm) was 89.1 (±3.8), which corresponded to the category of low waist circumference. Mean FM% as measured by DXA scan was 26.1% (±4.7), and was distributed between the fair, good, and excellent categories, stratified by age.
TABLE 1.
Body Composition Measures for Males and Females, Including Categorization of Waist Circumference and Percentile Age-Stratified Categorization of Percent Fat Mass by Sex
| Male | Female | |||||
| Measure | Units /Range | Number/Mean | ±SD/% | Range | Number/Mean | ±SD/ % |
| Enrolled | 48 | 4 | ||||
| Body composition measures | ||||||
| Height | cm | 181.1 | 6.5 | 169.8 | 7.6 | |
| Weight | kg | 94.6 | 13.9 | 75.2 | 8.6 | |
| Body mass index∗ | kg/m2 | 28.9 | 3.9 | 26.0 | 2.1 | |
| Normal (18.5 to <25) | 5 | 10.4% | 1 | 25.0% | ||
| Overweight (25 to <30) | 11 | 66.7% | 3 | 75.0% | ||
| Obese (≥30) | 32 | 22.9% | ND | ND | ||
| Waist circumference† | cm | 98.9 | 10.3 | 89.1 | 3.8 | |
| Low | 70 to <90 | 31 | 64.6% | 80 to <100 | 2 | 50.0% |
| High | 90 to <110 | 15 | 31.3% | 100 to <120 | 2 | 50.0% |
| Very high | ≥110 | 2 | 4.1% | >120 | ND | ND |
| Body composition measures by DXA | ||||||
| Body mass, total | kg | 92.7 | 13.3 | 74.0 | 7.1 | |
| Fat mass, total | kg | 22.4 | 8.1 | 19.6 | 5.0 | |
| Fat mass, percent | % | 23.6 | 5.7 | 26.1 | 4.7 | |
| Very poor (<20th %ile) | 14 | 29.2% | ND | ND | ||
| Poor (20–39th %ile) | 11 | 22.9% | 2 | 50.0% | ||
| Fair (40–59th %ile) | 9 | 18.8% | ND | ND | ||
| Good (60–79th %ile) | 11 | 22.9% | 2 | 50.0% | ||
| Excellent (80–94th %ile) | 2 | 4.1% | ND | ND | ||
| Very lean (≥95th %ile) | 1 | 2.1% | ND | ND | ||
| Lean mass, total | kg | 67.2 | 7.4 | 51.8 | 2.3 | |
| Lean mass, percent | % | 72.9 | 5.4 | 70.3 | 4.6 | |
| Bone density measures by DXA | ||||||
| Bone mineral content, total | kg | 3.2 | 0.4 | 2.7 | 0.4 | |
| Bone mineral density, total | g/cm2 | 1.3 | 0.1 | 1.3 | 0.1 | |
| T-Score | 1.2 | 1.0 | 2.1 | 1.2 | ||
| Z-Score | 1.2 | 0.9 | 1.8 | 1.0 | ||
ND, no data.
No participants had “Underweight” body mass index (less than 18.5 kg/m2).
No participants had “Very Low” waist circumference (less than 70 cm for men, or less than 80 cm for women).
Correlation coefficients of BMI with other body composition measures yielded strong correlations with WC (0.87) and TFM (0.83), but otherwise only moderate correlations with the remaining variables (Table 2).
TABLE 2.
Correlation of Non-body Mass Index (BMI) Body Composition Measures With BMI
| Body Composition Measure | Correlation Coefficient With BMI |
| WC | 0.87 |
| Total FM | 0.83 |
| Total LM | 0.64 |
| FM (%) | 0.62 |
| LM (%) | −0.61 |
FM, fat mass; LM, lean mass; WC, waist circumference.
VO2max was underestimated by 8.0 to 9.6 mL/kg/min (17.1% to 20.5%) in men and 6.5 to 7.3 mL/kg/min (15.7% to 17.7%) in women using the Concept 2 rowing VO2max estimates when compared with measured VO2max by treadmill test (Table 3). Univariate linear regression of VO2max for highly- and non-highly-trained rower-based estimates were compared against measured VO2max and are shown in Fig. 1.
TABLE 3.
VO2max Measures and Estimates in Males and Females, Including Percentile Age-Stratified Categorization of Measured VO2max by Sex
| Male | Female | |||||
| VO2max, mL/kg/min | Mean | ±SD | Percent Change from Measured VO2max | Mean | ±SD | Percent Change from Measured VO2max |
| Treadmill, measured | 46.9 | 8.4 | ----- | 41.3 | 5.6 | ----- |
| Very poor (<20th %ile) | 1 | 2.1% | ND | ND | ||
| Poor (20–39th %ile) | 6 | 12.5% | ND | ND | ||
| Fair (40–59th %ile) | 7 | 14.6% | ND | ND | ||
| Good (60–79th %ile) | 10 | 20.8% | 1 | 25.0% | ||
| Excellent (80–94th %ile) | 18 | 37.5% | ND | ND | ||
| Superior (≥95th %ile) | 6 | 12.5% | 3 | 75.0% | ||
| C2, not highly-trained | 37.3 | 7.9 | −20.5% | 34.8 | 4.1 | −15.7% |
| C2, highly-trained | 38.9 | 7.9 | −17.1% | 34.0 | 7.2 | −17.7% |
C2: Concept 2 rowing machine VO2max estimates.
FIGURE 1.
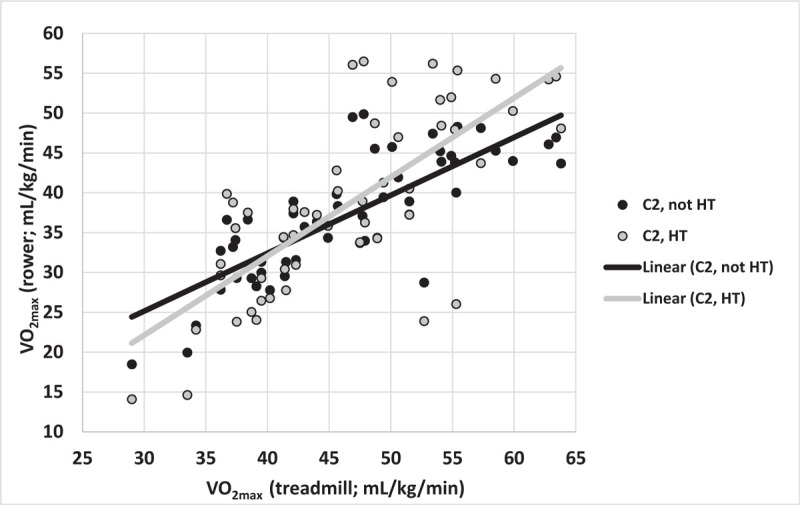
Univariate linear regression of VO2max estimates against measured VO2max. C2, Concept 2 rowing machine VO2max estimates, classified as not highly-trained or highly-trained; HT, highly-trained, not HT, not highly-trained.
Univariate linear regression of body composition measures (BMI, WC, FM%, LM%) with measured VO2max, demonstrated at best a moderate goodness-of-fit for FM% and LM%, both of which had a R2 of 0.58. BMI and WC had worse fits with VO2max, with R2 of 0.27 and 0.32, respectively (Table 4). In addition, univariate models of demographic variables and VO2max estimates were considered, demonstrating statistically significant associations (P < 0.005) with R2 = 0.63 for VO2max of non-highly trained subjects, R2 = 0.21 for BMC, R2 = 0.09 for age, and R2 = 0.07 for heavy physical activity based on the HUNT 2 questionnaire.
TABLE 4.
Univariate Linear Regression Coefficients (β Coefficients) and Goodness-of-fit (R2) for Body Composition Measures Against Measured VO2max
| Body Composition Measure | β Coefficient | R2 |
| FM (%) | −0.32 | 0.58 |
| LM (%) | +0.34 | 0.58 |
| Total FM | −0.20 | 0.51 |
| WC | −0.13 | 0.32 |
| BMI | −0.32 | 0.27 |
| Weight | −0.07 | 0.18 |
| Total LM | −0.01 | 0.002 |
All regressions were statistically significant (P < 0.005) except total LM. BMI, body mass index; FM, fat mass; LM, lean mass; WC, waist circumference.
Evaluation of sensitivity, specificity, and agreement of classifiers of obesity by Cohen κ between FM%, BMI, and WC were conducted with mixed results, with at best only moderate agreement (κ = 0.57) of obese BMI (BMI2) and very poor FM% (FM2; Fig. 2).
FIGURE 2.
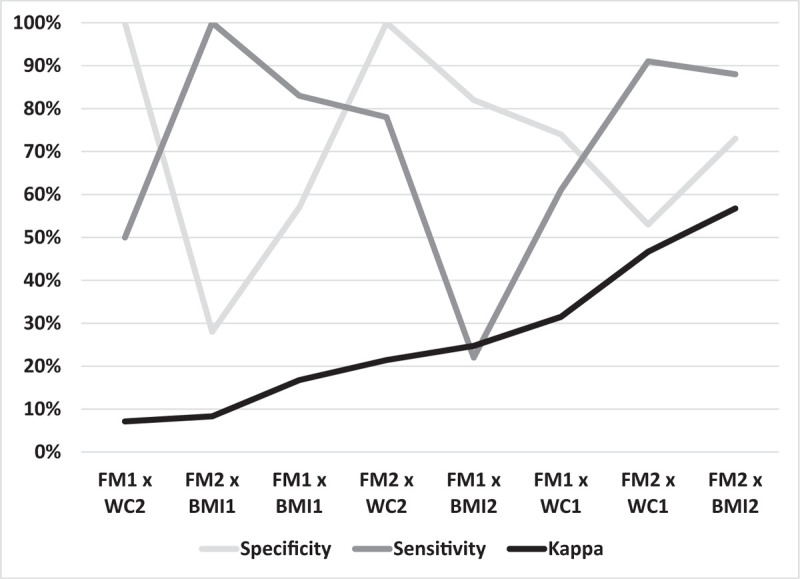
Performance metrics (specificity, sensitivity, κ coefficient) of classification of obesity by body mass index (BMI), waist circumference (WC), and percent fat mass (FM). BMI1: classification in “overweight” or “obese” BMI categories; BMI2: classification in “obese” BMI category; WC1: classification in “high” or “very high” WC categories; WC2: classification in “very high” WC category; FM1: classification in “poor” or “very poor” FM categories; FM2: classification in “very poor” FM category.
A multivariate regression model of estimated VO2max was constructed from a conjunction of demographic, body composition (BMI, BF%, LBM%, WC), and VO2max rower-based estimate variables based on their performance in univariate models. The best-fit and statistically significant measures included in the model while excluding collinear variables (such as for various body composition measures or VO2max estimates) included rower-based non-highly-trained VO2max, FM%, BMC, age, and heavy physical activity (HUNT 2), yielding a model with R2 = 0.7.
DISCUSSION
This study successfully demonstrates that various selected body composition measures of firefighters are not well-correlated. In agreement with prior studies, WC is somewhat correlated with BMI in firefighters, but to a lesser degree with FM%, and these divergences can lead to false positive (erroneous attribution of obesity) and false negative (erroneous attribution of non-obesity) in firefighters.8–11,32 This finding of BMI and WC being more highly correlated with each other than with FM% has also been reported in over 12,000 adults in the general population using NHANES data and DXA for FM% measurement.33 Implications of such erroneous classifications include the notion that obesity may be associated with poor CRF and non-obesity associated with adequate CRF among firefighters.
A striking finding of this study is that classifications of obesity did not agree well with each other unless characterizing a very obese population, and even then, correlations appeared to be moderate, an observation corroborated by Choi et al.32 This suggests that BMI as a stratifying metric of obesity in this population may be misleading. Despite the simplicity of measuring BMI, the strength of correlation with cardiorespiratory fitness (CRF) in firefighters may be weak.
Of the many body composition measures studied, VO2max is best (yet imperfectly) predicted by FM%, an observation that is in agreement with Kiss et al,34 though their results demonstrated a lesser degree of goodness-of-fit for FM% and VO2max, and a nearly equivalent goodness-of-fit for BMI and VO2max. This finding confirms the study hypothesis that FM% is a more valid measure of body composition and more predictive of CRF than BMI. This study is relatively unique amongst investigations regarding body composition in firefighters to the extent that it includes body composition measurements by DXA (a research need noted by Poston et al8), as well as correlating these more precise body composition measures with CRF. A similar study correlating body composition and measured VO2max was performed in Belgian firefighters, where a “strong” association between FM%, BMI, and VO2max was noted, though this study may not be generalizable to United States firefighters, who have arguably quite different social and dietary pressures that may affect their weight.34 However, our results diverge from another similar study using a VO2max estimate and skin caliper-based BF% measurements, which concluded that BMI is an adequate method of estimating body composition in firefighters, but limited its conclusions to the extent of noting the evident inverse association between a VO2max and BMI.35 A very recent study by Barry et al36 evaluating the correlation between WC and VO2max found a stronger statistically significant correlation (–0.55) than this study, with a similar R2 of 0.30.
In evaluating existing VO2max estimates from the Concept 2 rower, this study found that the rower-based estimates underestimated VO2max, compared with measurements that were obtained with the gold standard treadmill test with indirect calorimetry. These rower-based VO2max estimates had better correlation with measured VO2max using the “non-highly-trained” estimate as compared with “highly-trained” estimate. As estimates of VO2max may not adequately represent the true measurement, the developed multivariate model (R2 = 0.7) integrating body composition measures and VO2max estimates, in addition to other variables, can more accurately evaluate CRF. These data support continuing this study in an expanded sample size to develop a more robust model of VO2max, integrating additional VO2max estimates such as those implemented in the Survey of Activity, Fitness, and Exercise (SAFE) study and the third phase of the Nord-Trøndelag Health Study (HUNT-3), where VO2max has been estimated using simple questionnaire-based tools.37,38
A unique aspect of the study was providing the results to study participants, which historically has been a rare feature of research studies, though contemporary research methods support changing this paradigm for many reasons.39 Although not formally measured, informal feedback from study participants regarding this aspect of the study was wholly positive, and suggestive that reviewing such information may be a motivating factor in behavioral change; this feature can be evaluated more formally in future validation studies implementing this VO2max model longitudinally and alongside potential interventions to improve fitness indicators. Such future research is aligned with the need for supporting wellness in the fire service on the part of the individual, leadership, and department, including measures of body composition and CRF, as identified as part of the Wellness-Fitness Initiative developed by the International Association of Fire Fighters and the International Association of Fire Chiefs.40
A primary limitation of this study is the bias implicit in volunteer-based recruitment, to the extent that those participating in the study may represent those already motivated to evaluate their body composition and CRF, as noted by the larger prevalence of higher percentile CRF noted in Table 3. However, in terms of body composition, 89.6% of men and 75.0% of women in this study were overweight or obese according to BMI, consistent with prior reports of firefighters, while only 35.4% of men and 50.0% of women had high or very high WC. The average BMI of 28.9 kg/m2 and WC of 98.9 cm for men in this study are relatively consistent with the reported averages of 28.6 kg/m2 and 97.3 cm reported in male career firefighters by Poston et al,8 in which they reported 97% participation of solicited firefighters, suggesting that the degree of obesity represented in this study may be consistent with the career firefighter population despite a volunteer bias. Conversely, the same Poston et al8 study identified estimated VO2max by physical activity as quite different in obese (BMI more than or equal to 30) versus non-obese firefighters, which may indicate that inclusion of more obese and less fit firefighters could impact the applicability of this study's findings in such a population, with likely better convergence of body composition measures.
In addition, the small sample size of this study, particularly with respect to women (7.7%)—although greater than the proportion of women career firefighters in the fire service nationally, that is, 4%—may limit generalizability in terms of representing anthropomorphic and cardiorespiratory variability.41 Lastly, the composition and culture of career firefighters in an urban, metropolitan setting, varies from department to department, and similarly limits generalizability across departments, and can be addressed in future studies validating this model across multiple fire departments of various settings.
Whereas this study is limited to career firefighters, Martin et al42 evaluated obesity and CRF in volunteer firefighters and concluded that “the majority of volunteer firefighters may possess … inadequate physical fitness,” which may limit the generalizability of this study's findings where most firefighters had relatively high CRF. However, prior studies in volunteer firefighters have addressed the same limitations as this study of BMI in assessing obesity, with the Poston et al8 study previously discussed showing similar VO2max in non-obese career versus volunteer firefighters as opposed to divergent VO2max in obese versus non-obese firefighters, regardless of career or volunteer status.11 These inconsistencies suggest further work on evaluating body composition measures and CRF to be done in the volunteer population, where risks may be greater.
Future work in the second phase of this study will also assess whether VO2max estimates can correlate well with measures of cardiovascular risk in this population, thereby increasing the utility of these estimates in monitoring the risk and fitness of this at-risk population, which has been identified as a needed area of research to understand the relationship of these two variables.43 The second phase of this study will also evaluate the cost-effectiveness of the measures comprising the multivariate model to validate feasibility of implementing this sort of VO2max evaluation in a firefighter population.
CONCLUSIONS
Traditional body composition measures, such as BMI, may suffer from measurement error that makes the evaluation obesity inappropriate for some subpopulations, such as firefighters. Considerations of CRF as a function of obesity will, as a result, be similarly problematic. Body fat percentage can more accurately estimate obesity, and can be easily measured with widely-available and safe DXA technology. Using demographic measures and more accurate measures of body composition conjoined with estimates of CRF, this study developed a preliminary multivariate model that improved prediction accuracy of CRF over other existing estimation methods. Future work can validate this model in a larger population of firefighters or in the general population to improve precision and evaluate cost-effectiveness.
Acknowledgments
The authors would like to thank the HealthPartners Institute, HealthPartners Riverside Radiology, and Health Strategies, LLC, for their continued support and partnership in the development and progression of this study.
The authors graciously thank the St. Paul Fire Department for their time and facilities, to Chief Barton Inks for his continued support, and to the individual firefighters who volunteered to participate in this study.
Footnotes
Funding Sources: Funding for this study was provided in full by Hologic, Inc., Marlborough, MA. The results reported herein correspond to specific aims of grant A16-667 (Comparison of Body Composition Methods, Cardiorespiratory Fitness, and Obesity in Firefighters) to investigator Zeke J. McKinney (HealthPartners Institute) from Hologic, Inc.
Conflict of Interest: Drs. McKinney and Bovard have performed medical consulting in an unpaid capacity for the St. Paul Fire Department and other fire service institutions/organizations in Minnesota. While this has aided in terms of recruitment in this study, these relationships have not impacted the study design or data analysis of this study.
Ethical Considerations and Disclosures: This study was approved by the HealthPartners Institute Institutional Review Board (IRB) as study A16-667 (“Comparison of Body Composition Methods, Cardiorespiratory Fitness, and Obesity in Firefighters”).
Clinical Significance: Standard measures of obesity poorly correlate with cardiorespiratory fitness in firefighters, and fire departments may benefit from an improved approach to body composition and fitness evaluation that can more accurately represent the fitness of firefighters.
REFERENCES
- 1. National Institute for Occupational Safety and Health. Preventing Fire Fighter Fatalities Due to Heart Attacks and Other Sudden Cardiovascular Events. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication Number. 2007;133:1–6. [Google Scholar]
- 2.Smith DL, DeBlois JP, Kales SN, Horn GP. Cardiovascular strain of firefighting and the risk of sudden cardiac events. Exerc Sport Sci Rev 2016; 44:90–97. [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson ML, Brown AL, Poston WS, Haddock CK, Jahnke SA, Day RS. Physician weight recommendations for overweight and obese firefighters, United States, 2011-2012. Prev Chronic Dis 2014; 11:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Fire Protection Association (NFPA). NFPA 1582, Standard on Comprehensive Occupational Medical Programs for Fire Departments. Quincy, MA: National Fire Protection Association; 2018. [Google Scholar]
- 5.Pronk NP. Fitness of the US workforce. Annu Rev Public Health 2015; 36:131–149. [DOI] [PubMed] [Google Scholar]
- 6.National Fire Protection Association (NFPA). Fourth Needs Assessment of the US Fire Service. Quincy, MA: National Fire Protection Association; 2016. [Google Scholar]
- 7.Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a Scientific Statement From the American Heart Association. Circulation 2016; 134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 8.Poston WSC, Haddock CK, Jahnke SA, Jitnarin N, Tuley BC, Kales SN. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med 2011; 53:266–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jitnarin N, Poston WSC, Haddock CK, Jahnke S, Tuley BC. Accuracy of body mass index-defined overweight in fire fighters. Occup Med (Lond) 2013; 63:227–230. [DOI] [PubMed] [Google Scholar]
- 10.Jitnarin N, Poston WSC, Haddock CK, Jahnke SA, Day RS. Accuracy of body mass index-defined obesity status in us firefighters. Saf Health Work 2014; 5:161–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ode J, Knous J, Schlaff R, Hemenway J, Peterson J, Lowry J. Accuracy of body mass index in volunteer firefighters. Occup Med (Lond) 2014; 64:193–197. [DOI] [PubMed] [Google Scholar]
- 12.Ode JJ, Pivarnik JM, Reeves MJ, Knous JL. Body mass index as a predictor of percent fat in college athletes and nonathletes. Med Sci Sports Exerc 2007; 39:403–409. [DOI] [PubMed] [Google Scholar]
- 13.Rubiano F, Nuñez C, Heymsfield SB. A comparison of body composition techniques. Ann N Y Acad Sci 2000; 904:335–338. [DOI] [PubMed] [Google Scholar]
- 14.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013; 309:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewiecki EM, Binkley N, Morgan SL, et al. Best practices for dual-energy x-ray absorptiometry measurement and reporting: international society for clinical densitometry guidance. J Clin Densitom 2016; 19:127–140. [DOI] [PubMed] [Google Scholar]
- 16.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361:849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huda W. Radiation risks: what is to be done? AJR Am J Roentgenol 2015; 204:124–127. [DOI] [PubMed] [Google Scholar]
- 18.Mattila VM, Tallroth K, Marttinen M, Pihlajamäki H. Body composition by DEXA and its association with physical fitness in 140 conscripts. Med Sci Sports Exerc 2007; 39:2242–2247. [DOI] [PubMed] [Google Scholar]
- 19.Nevill AM, Metsios GS. The need to redefine age- and gender-specific overweight and obese body mass index cutoff points. Nutr Diabetes 2015; 5:e186–e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasco JA, Nicholson GC, Brennan SL, Kotowicz MA. Prevalence of obesity and the relationship between the body mass index and body fat: cross-sectional, population-based data. PLoS One 2012; 7:e29580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing data from the fitness registry and the importance of exercise national database. Mayo Clin Proc 2015; 90:1515–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers J, Kaminsky LA, Lima R, Christle JW, Ashley E, Arena R. A reference equation for normal standards for VO2 Max: analysis from the fitness registry and the importance of exercise national database (FRIEND Registry). Prog Cardiovasc Dis 2017; 60:21–29. [DOI] [PubMed] [Google Scholar]
- 23.Pronk NP, Martinson B, Kessler RC, Beck AL, Simon GE, Wang P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J Occup Environ Med 2004; 46:19–25. [DOI] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kurtze N, Rangul V, Hustvedt B-E, Flanders WD. Reliability and validity of self-reported physical activity in the Nord-Trøndelag Health Study (HUNT 2). Eur J Epidemiol 2007; 22:379–387. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Anthropometry Procedures Manual. 2017; Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Available at: https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2017_Anthropometry_Procedures_Manual.pdf. Accessed February 20, 2018. [Google Scholar]
- 28. Concept 2. VO2max Calculator. Available at: https://www.concept2.com/indoor-rowers/training/calculators/vo2max-calculator. Accessed December 20, 2018. [Google Scholar]
- 29.Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Hear J 1973; 85:546–562. [DOI] [PubMed] [Google Scholar]
- 30.Ng BK, Liu YE, Wang W, et al. Validation of rapid 4-component body composition assessment with the use of dual-energy X-ray absorptiometry and bioelectrical impedance analysis. Am J Clin Nutr 2018; 108:708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 10th ed.Philadephia, PA: Wolters Kluwer Health; 2018. [Google Scholar]
- 32.Choi BK, Steiss D, Garcia-Rivas J, et al. Comparison of body mass index with waist circumference and skinfold-based percent body fat in firefighters: adiposity classification and associations with cardiovascular disease risk factors. Int Arch Occup Environ Health 2016; 89:435–448. [DOI] [PubMed] [Google Scholar]
- 33.Flegal KM, Shepherd JA, Looker AC, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr 2009; 89:500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kiss P, De Meester M, Maes C, De Vriese S, Kruse A, Braeckman L. Cardiorespiratory fitness in a representative sample of Belgian firefighters. Occup Med (Lond) 2014; 64:589–594. [DOI] [PubMed] [Google Scholar]
- 35.Nogueira EC, Porto LGG, Nogueira RM, et al. Body composition is strongly associated with cardiorespiratory fitness in a large brazilian military firefighter cohort: the brazilian firefighters study. J strength Cond Res 2016; 30:33–38. [DOI] [PubMed] [Google Scholar]
- 36.Barry AM, Lyman KJ, Dicks ND, et al. Firefighters’ physical activity and waist circumference as predictors of. J Occup Environ Med 2019; 61:849–853. [DOI] [PubMed] [Google Scholar]
- 37.Ainsworth BE, Richardson MT, Jacobs DR, Arthur SL. Prediction of cardiorespiratory fitness using physical activitiy questionnaire data. Med Exerc Nutr Heal 1992; 1:75–82. [Google Scholar]
- 38.Nes BM, Janszky I, Vatten LJ, Nilsen TIL, Aspenes ST, WislØff U. Estimating V̇O2 peak from a nonexercise prediction model: The HUNT study, Norway. Med Sci Sports Exerc 2011; 43:2024–2030. [DOI] [PubMed] [Google Scholar]
- 39.Botkin JR, Mancher M, Busta ER, Downey AS. National Academies of Science. Engineering and M. The National Academies Press, Returning Individual Research Results to Participants. Washington, D.C: 2018. [PubMed] [Google Scholar]
- 40.International Association of Fire Fighters. The Fire Service Joint Labor Management Wellness-Fitness Initiative. 4th ed.Washington, D.C: International Association of Fire Fighters; 2018. [Google Scholar]
- 41.Evarts B, Stein G. NFPA's U.S. Fire Department Profile 2017. Quincy, MA: National Fire Protection Agency; 2019. [Google Scholar]
- 42.Martin ZT, Schlaff RA, Hemenway JK, et al. Cardiovascular disease risk factors and physical fitness in volunteer firefighters. Int J Exerc Sci 2019; 12:764–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kodama S. CLINICIAN ’ S CORNER cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events. J Am Med Assoc 2009; 301:2024–2035. [DOI] [PubMed] [Google Scholar]


