Abstract
Wearing face masks has become the new normal worldwide due to the global spread of the coronavirus disease 2019. The inhalation of microplastics due to the wearing of masks has rarely been reported. The present study used different types of commonly used masks to conduct breathing simulation experiments and investigate microplastic inhalation risk. Microplastic inhalation caused by reusing masks that underwent various treatment processes was also tested. Results implied that wearing masks considerably reduces the inhalation risk of particles (e.g., granular microplastics and unknown particles) even when they are worn continuously for 720 h. Surgical, cotton, fashion, and activated carbon masks wearing pose higher fiber-like microplastic inhalation risk, while all masks generally reduced exposure when used under their supposed time (<4 h). N95 poses less fiber-like microplastic inhalation risk. Reusing masks after they underwent different disinfection pretreatment processes can increase the risk of particle (e.g., granular microplastics) and fiber-like microplastic inhalation. Ultraviolet disinfection exerts a relatively weak effect on fiber-like microplastic inhalation, and thus, it can be recommended as a treatment process for reusing masks if proven effective from microbiological standpoint. Wearing an N95 mask reduces the inhalation risk of spherical-type microplastics by 25.5 times compared with not wearing a mask.
Keywords: Masks, COVID-19, Microplastics, Particles, Reuse
Graphical Abstract
1. Introduction
As the coronavirus disease 2019 (COVID-19) spreads throughout the entire world, face masks have become a necessity for the citizens of many countries (Greenhalgh and Howard, 2020, Chu et al., 2020). Surgical and N95 masks have been regarded as the most effective masks for reducing the risk of COVID-19 transmission. However, given the shortage of surgical masks and the relatively high price of using them as disposable items, people have used cotton masks or other types of masks to replace surgical masks (Shakya et al., 2017, Davies et al., 2013, Santos et al., 2020). Consequently, reusing masks after a disinfection process or simply reusing them directly has become a common practice (Song et al., 2020). However, the improper use of masks can increase the transmission risk of COVID-19. Moreover, the inhalation of microplastics should be considered when wearing masks.
Melt-blown fabric is the core material used in the production of surgical masks, and its major component is polypropylene (PP) (Pu et al., 2018). The fiber diameter of melt-blown fabric is approximately 1–5 µm; thus, it exhibits high filtration performance that is sufficient for rejecting bacteria, suspended particles, droplets, and aerosols. Surgical masks have three layers. The front and back covers are made of PP, with a fiber diameter of approximately 20 µm. The middle layer of surgical masks is melt-blown fabric, which is the core material for virus rejection. Microplastics or nanoplastics can be generated during the use and reuse of masks made from the aforementioned materials (Aragaw, 2020, Fadare and Okoffo, 2020). This condition can lead to the risk of microplastic inhalation via breathing. Microplastics are also present in the air and can be inhaled during breathing (Gasperi et al., 2015; Gasperi et al., 2018, Zhang et al., 2020, Dris et al., 2017). Liu et al. (2019) investigated the source and potential risk of suspended microplastics in Shanghai, China. Their results indicated that suspended atmospheric microplastics (SAMs) are distributed ubiquitously, and the estimated annual weight of SAMs is approximately 120.72 kg in Shanghai. Vianello et al. (2019) simulated human exposure to indoor airborne microplastics and found that a mannequin inhaled up to 272 microplastic particles over 24 h. Abbasi et al. (2019) reported that 900 microplastics and 250 microrubbers of varying sizes and shapes were found in 15 g of street dust collected in Iran. Thus, microplastic inhalation from the air should also be considered to ensure human health. In such case, wearing masks can potentially reduce microplastic inhalation from the air during breathing by acting as a barrier (Faridi et al., 2020).
At present, the most commonly used commercial masks include surgical, N95, cotton, fashion, activated carbon, and nonwoven masks. Wearing masks potentially results in microplastic inhalation, including microplastics from the air and from the materials of the masks. The common disinfection processes for masks include simple washing, ultraviolet (UV) light irradiation, air blower disinfection, alcohol disinfection, and sunlight exposure (Chua et al., 2020). Melt-blown fabric is fragile; washing with water, alcohol disinfection, and drying can damage its fiber structure and lead to the loss of its protective function. Common disinfection processes can damage the structure of masks and increase the risk of inhaling exogenous substances and microplastics generated from the masks.
This study selected seven typical commercial masks. Microplastic inhalation through different types of masks was investigated using simulated breathing equipment. Microplastic inhalation caused by wearing different types of masks after various disinfection processes was also investigated. This study can provide guidance for selecting masks to use or reuse based on requirements.
2. Materials and methods
2.1. Experimental setup
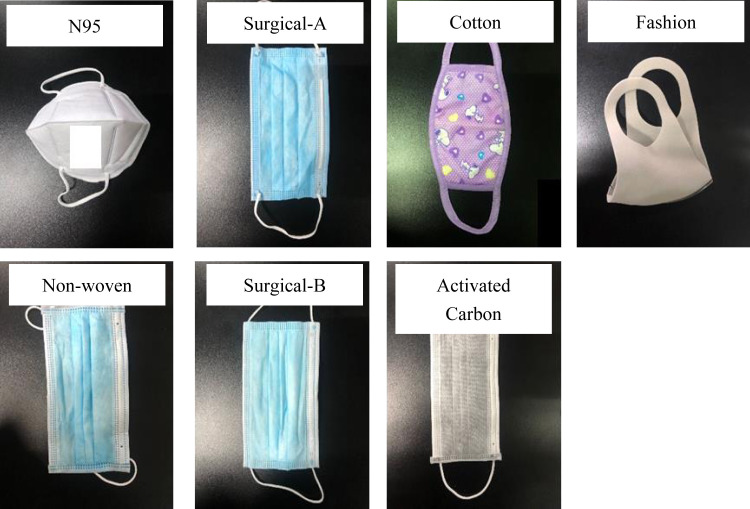
Seven types of commonly used masks were selected for investigation in this study ( Fig. 1): N95 respirator, surgical masks (A and B from different companies), cotton mask, fashion mask, nonwoven mask, and activated carbon mask. The difference between surgical and nonwoven masks is their middle layer. The middle layer of surgical masks is made from melt-blown fabric. By contrast, all the layers of nonwoven masks are made from nonwoven fiber. Cotton masks are made of cotton. Activated carbon masks have inner and outer layers made from nonwoven fabric and a middle layer made from activated carbon cloth. Fashion masks are made of three layers of organic polymer with a stereoscopic network structure. N95 respirators are made of five PP layers; the outer and inner layers are spunbonded and the three middle layers are melt-blown. All the aforementioned masks are commercially available and commonly used. A vacuum pump (ZK290, VMSTR, China) with a flow rate 15 L/min was used, with the tested masks fixed tightly on top of the suction cup (Fig. S1). Thus, all the microplastics filtrated from the air or from the masks were ejected into the cup. After completing one test, Milli-Q water was used to clean the suction cup carefully, and the ejected microplastics were transferred onto the membrane via vacuum suction. A blank test, a suction test without mask, and a test that only allows air to pass through the filter membrane were also conducted during the entire experiment. The microplastics ejected onto the membrane were then transferred to clean glass culture ware to allow them to dry naturally. Thereafter, the microplastics were observed and counted under a microscope. The experiments in this study were not conducted in super-clean laboratory, no contamination control measures were applied. This is designed for reflect a realistic situation of microplastics inhalation, and blank test were designed for providing comparative analysis.
Fig. 1.
Commonly used masks tested in this study (N95, surgical A, cotton, fashion, nonwoven, surgical B, and activated carbon masks). Surgical A and B masks are produced by different companies.
Microplastic inhalation risk posed by reusing masks that underwent different disinfection processes was also investigated. The disinfection processes were as follows: (1) UV irradiation for 30 min (15 min each for the front and back sides), (2) alcohol disinfection (alcohol was sprayed on both sides of the mask and then the mask was allowed to dry naturally indoor), (3) air blower disinfection (an air blower was used to blow heated air onto both sides of the mask for 15 min), (4) washing (both sides of the mask was washed gently with running water and then the mask was allowed to dry naturally indoor), and (5) sunlight disinfection (the mask was placed under sunlight for 3 h at noon when the outdoor temperature was 35 °C). A blank test without a disinfection process for a new mask was also conducted for comparison. The treated masks were then use in a breathing simulation to investigate the potential for microplastic inhalation.
2.2. Microplastic detection
Microplastics were observed and counted under a microscope. Typical microplastics were selected and examined via Raman spectroscopy (inVia, Renishaw, the UK). The collected Raman spectra were tested within the range of 100–3200 cm−1 for 785 nm laser. The spectra of samples were then compared with the reference library based on the characteristic peaks. The remaining microplastics on the membrane were transferred to a test tube, dried using a nitrogen-blowing instrument, added with 0.5 mL of absolute ethanol, vortexed for 1 min, and then examined with a Fourier transform infrared (FTIR) spectrometer (Nicolet 5700, Thermo Fisher) and a laser infrared imaging system (8700 LDIR, Agilent). The FTIR analysis was performed at 32 scans per replicate within the range of 4000–400 cm−1, and the resolution is 4 cm−1. The LDIR analyzer can identify major types and size fractions of microplastics. A detailed description of the technology used in LDIR can be found in Scircle et al., 2020, da Costa Filho et al., 2020. One drop of sample with water on a slide was rapidly scanned, and the information obtained was automatically matched in the library of Agilent Clarity software.
2.3. Ranking of microplastic inhalation risk
Microplastic inhalation risk was ranked in this study. The amount of microplastics counted from each mask was divided by the blank case, which was tested in parallel. The resulting values were then arranged from high to low. The ranking was also listed from high to low. Only risk ranking was obtained in this study.
2.4. Kinetics
The breathing simulation test for potential microplastic inhalation was conducted for 2, 4, 8, 24, 48, 96, 120, 168, 360, and 720 h. The test for mask reuse after different disinfection processes was conducted for 2, 4, 6, 8, 10, and 12 h. Microplastics in spherical and fiber-like types were counted separately. The accumulated microplastic amount in spherical and fiber-like types was then fitted with the zero-order reaction linear regression model. The corresponding slope, i.e., the k value, was also calculated under each condition.
2.5. Statistical analysis
The significance of the results was evaluated via ANOVA, and P < 0.05 was regarded as statistically significant. SPSS 20.0 was used in this study.
3. Results and discussion
3.1. Microplastic inhalation risks posed by using different types of masks
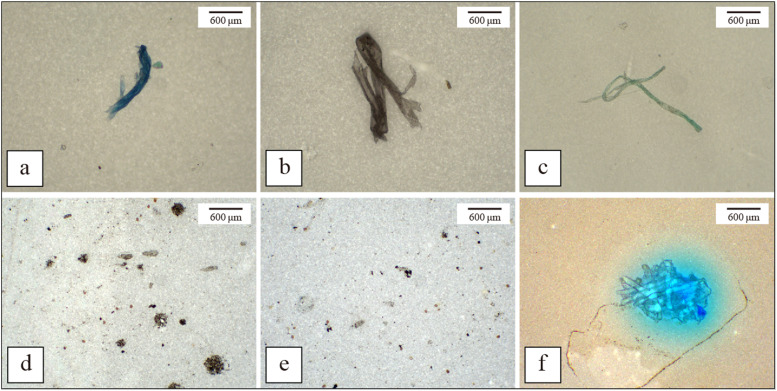
Microplastics were observed during the breathing simulation experiment with masks ( Fig. 2). The observed microplastics were mostly fiber-like and spherical types. The accumulated amounts of fiber-like microplastics during the 720 h breathing simulation test using different types of masks are provided in Table 1. The fiber-like microplastics accumulated after 720 h of vacuum suction exhibited the highest amount with the activated carbon mask. The N95 respirator had the lowest amount of fiber-like microplastics even when compared with not wearing a mask. For the test without mask, 1835 fiber-like microplastics were found after 720 h of vacuum suction. These microplastics came from the air. On the basis of these findings, a conclusion can be drawn that N95 respirators can mitigate fiber-like microplastic inhalation from the air even when they are used for a long time. The other types of masks, i.e., surgical, cotton, fashion, nonwoven, and activated carbon masks, can reduce fiber-like microplastic inhalation risk when they are worn for 2–4 h. The microplastic inhalation risk posed by using the seven types of masks was tested for suction time ranging from 2 h to 720 h. The results showed that the increase in fiber-like microplastic amount exhibits a highly linear correlation with time (P < 0.01). The amount of fiber-like microplastics was determined to be 25, 38, 92, 69, 47, 112, 153, and 172 particles after the continuous use of N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, and in the blank case, respectively, based on 2 h of simulated respiration. The amount of fiber-like microplastics in the blank case (i.e., without mask) was always higher than those of the cases with masks when suction time was less than 24 h, except for the activated carbon mask. The activated carbon mask used in this study was a low-priced brand (i.e., 0.2 RMB/piece, 1 RMB ≈ 0.14 USD; the prices of the other masks are listed in Table S1). The high risk of fiber-like microplastic inhalation posed by using the studied activated carbon mask can be attributed to the inferior materials used in the production of this mask (Neupane et al., 2019). The poor-quality material of the mask was easily damaged, and the generated microplastics were inhaled by the user. In summary, all the tested masks can help reduce microplastic inhalation from the air when used for less than 2 h compared with not wearing a mask. Wearing low-quality masks for longer than 4 h can pose higher fiber-like microplastic inhalation risk than not wearing a mask. When the masks are reused for a long time, only N95 respirators pose less fiber-like microplastic inhalation risk compared with not wearing a mask. When reused masks are worn for 720 h, fiber-like microplastic inhalation risk is 0.04, 0.54, 0.40, 0.16, 0.73, and 1.17 times higher than that without wearing a mask. The inhalation risks of fiber-like microplastics posed by wearing a reused mask for 2 h are arranged from high to low as follows: no mask > activated carbon mask > surgical-B mask > cotton mask > fashion > nonwoven mask > surgical-A mask > N95 respirator. The inhalation risks of fiber-like microplastics posed by wearing a reused mask for 720 h are arranged from high to low as follows: activated carbon mask > surgical-B mask > cotton mask > fashion mask > nonwoven mask > surgical-A mask > no mask > N95 respirator. This could summarize that most masks after using for 720 h present higher fiber-like microplastics than without mask, those fiber-like microplastics could mostly originate from the mask itself.
Fig. 2.
Fiber-like and spherical-type microplastics observed in this study (a – from surgical A mask, b – from activated carbon mask, c – from surgical B mask, d – from cotton mask, e – from nonwoven mask, and f – from fashion mask).
Table 1.
Accumulated amount of fiber-like microplastics observed during the 720 h breathing simulation with different types of commonly used masks.
| Times (h) | N95 | Surgical-A | Cotton | Fashion | Non- woven | Surgical-B | Activated carbon | Blank -No mask |
|---|---|---|---|---|---|---|---|---|
| 2 | 25 | 38 | 92 | 69 | 47 | 112 | 153 | 172 |
| 4 | 45 | 57 | 123 | 83 | 69 | 138 | 249 | 197 |
| 8 | 80 | 91 | 180 | 133 | 115 | 214 | 447 | 237 |
| 24 | 110 | 137 | 222 | 185 | 150 | 264 | 540 | 275 |
| 48 | 179 | 202 | 303 | 245 | 211 | 374 | 725 | 348 |
| 96 | 268 | 301 | 484 | 397 | 341 | 516 | 958 | 428 |
| 120 | 308 | 392 | 581 | 478 | 418 | 620 | 1120 | 482 |
| 168 | 366 | 515 | 741 | 654 | 540 | 780 | 1352 | 643 |
| 360 | 719 | 961 | 1337 | 1318 | 1026 | 1556 | 2086 | 911 |
| 720 | 1521 | 1913 | 2824 | 2576 | 2134 | 3180 | 3984 | 1835 |
The accumulated amounts of spherical-type microplastic particles observed during the 720 h breathing simulation test using different types of masks are provided in Table 2. The amount of accumulated spherical-type microplastics was significantly correlated with suction time (P < 0.01). When suction time was 2 h, the spherical-type particles observed with the N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, and without a mask were 1695, 1808, 2241, 3110, 2152, 3090, 2212, and 3918, respectively. When suction time was increased, spherical-type particle inhalation risk continuously decreased compared with that without mask. The particle amount when N95 was used for 2 h was 43% that of the no mask case and only 4% after 720 h of suction. Nevertheless, spherical-type particle inhalation risk remained high regardless of whether masks were worn or not (the filter membrane image after the breathing test is shown in Fig. S2). In conclusion, reusing all the types of masks tested in this study for 720 h poses less microplastic inhalation risk compared with not wearing a mask. If masks are used as disposable products and changed into new ones every 2–4 h, then the amount of particles inhaled can also be calculated after wearing masks for 720 h (Table S2). The ratio of the predicted particle amount after masks were worn for a long time to the actual counted amount was calculated (Table S3). The results indicated that frequently changing masks, e.g., every 2 h, poses higher particle inhalation risks compared with using old masks for a long time. This finding also implied that wearing masks for a long time reduces the particle penetration rate of masks, particularly for N95 respirators. For example, people are likely to wear masks for 8 h since it is a full working day, it could reduce the microplastics inhalation with a continuous wearing of 8 h instead of change new mask per 2–4 h, if not considering the virus issue (Table 2, Table S2). Meanwhile, breathing rate may also be enhanced because more air is required to pass through the mask. The amount of particles can also change with increasing breathing rate. In this study, a suction rate of 15 L/min was selected on the basis of the average medium breathing rate of humans (Garcia et al., 2015, Tian et al., 2017, Liu et al., 2014). Further research on microplastic inhalation risk under different breathing rates should be conducted in the near future.
Table 2.
Accumulated amount of particle observed during the 720 h breathing simulation with different types of commonly used masks.
| Times (h) | N95 | Surgical -A | Cotton | Fashion | Non- woven | Surgical -B | Activated carbon | Blank -No mask |
|---|---|---|---|---|---|---|---|---|
| 2 | 1695 | 1808 | 2241 | 3110 | 2152 | 3090 | 2212 | 3918 |
| 4 | 2268 | 2648 | 3567 | 6622 | 3612 | 6568 | 3417 | 7946 |
| 8 | 3290 | 3797 | 6963 | 12,158 | 6292 | 12,625 | 6033 | 15,732 |
| 24 | 4678 | 6631 | 12,848 | 24,643 | 7814 | 24,279 | 9988 | 39,700 |
| 48 | 6790 | 10,495 | 26,690 | 47,722 | 14,598 | 42,119 | 16,174 | 92,236 |
| 96 | 9294 | 22,081 | 46,892 | 91,800 | 25,705 | 76,833 | 29,912 | 184,618 |
| 120 | 10,810 | 26,585 | 55,932 | 109,986 | 29,269 | 99,487 | 34,814 | 212,994 |
| 168 | 12,660 | 36,953 | 72,006 | 145,374 | 36,423 | 128,054 | 47,028 | 249,114 |
| 360 | 23,265 | 71,545 | 158,660 | 295,832 | 85,664 | 268,897 | 92,453 | 562,842 |
| 720 | 44,853 | 140,069 | 302,242 | 597,980 | 169,316 | 523,791 | 181,017 | 1,121,316 |
Fiber-like microplastic inhalation risk posed by wearing masks for less than 168 h (7 days) was lower than that posed by not wearing a mask, except for surgical-B and activated carbon masks. This result implied that reusing masks will not increase fiber-like microplastic inhalation risk. It also suggested that the microplastics were from the air, and only a low percentage of microplastics was rejected by the masks. N95 exhibited the highest rejection performance in all the tested masks. The high fiber-like microplastic inhalation risk posed by using surgical B and activated carbon masks suggested that these masks can generate fiber-like microplastics from the materials used in their manufacture, such as PP and polyethylene (Jung et al., 2020). For spherical-type particles, the amount of microplastic inhalation using N95 was 43% compared with that of the blank case after 2 h of testing and 4% after 360 h of testing. This result implied that spherical-type microplastics from the air that passed through N95 masks decrease with time. Some particles from the air can be ejected into the inner structure hole of N95 masks, reducing spherical-type microplastic inhalation in the long term. Fiber-like microplastic inhalation risk is considerably lower ( Table 3, k = 2.0–5.0) than that of spherical-type microplastics ( Table 4, k = 58.2–1545.0). N95 masks always pose lower microplastic inhalation risk compared with the other types of masks. The same trend was also observed in other types of masks. Wearing masks for a long time can increase breathing resistance. This phenomenon should also be considered in future research.
Table 3.
Kinetic coefficients of fiber-like microplastics accumulation after the 720 h breathing simulation test with different types of masks.
| N95 | Surgical -A | Cotton | Fashion | Non-woven | Surgical-B | Activated carbon | Blank- No mask | |
|---|---|---|---|---|---|---|---|---|
| R2 | 0.9961 | 0.9989 | 0.9972 | 0.9996 | 0.9983 | 0.9979 | 0.9876 | 0.9924 |
| k | 2.0 | 2.6 | 3.7 | 3.5 | 2.8 | 4.2 | 5.0 | 2.2 |
Table 4.
Kinetic coefficients of particle accumulation after the 720 h breathing simulation test with different types of masks.
| N95 | Surgical-A | Cotton | Fashion | Non-woven | Surgical-B | Activated carbon | Blank- No mask | |
|---|---|---|---|---|---|---|---|---|
| R2 | 0.9964 | 0.9994 | 0.9993 | 0.9995 | 0.9987 | 0.9996 | 0.9994 | 0.9984 |
| k | 58.2 | 192.0 | 417.4 | 820.5 | 230.8 | 721.5 | 246.6 | 1545.0 |
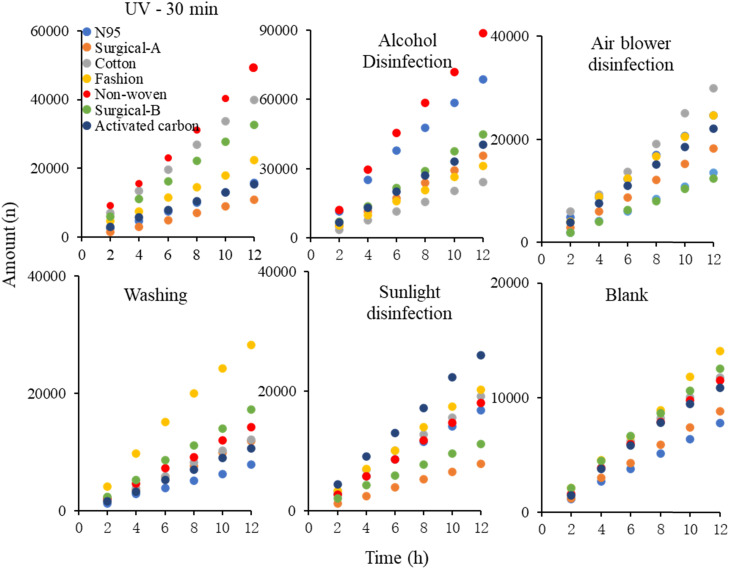
3.2. Microplastic inhalation risks posed by using masks treated with various disinfection processes
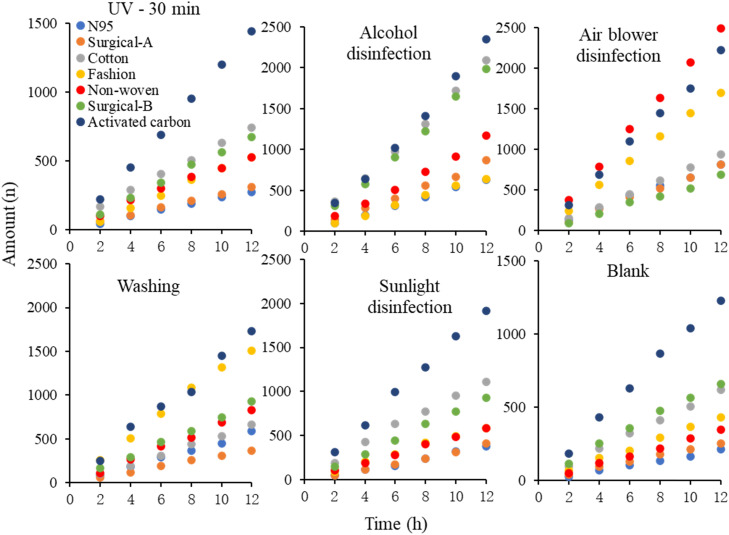
Considering poverty and resource reuse behavior worldwide, reusing masks with or without applying a disinfection process is a common practice. Microplastic inhalation risk posed by using common commercial masks that underwent different disinfection processes was also investigated. Spherical- and fiber-like microplastic inhalation risks posed by using N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks treated via UV irradiation, alcohol disinfection, air blower treatment, washing with water, exposure to sunlight, and without treatment, were tested ( Fig. 3, Table 5, Table S4, Table S5). Spherical- and fiber-like microplastic inhalation risks increased after treatment. After treating via UV irradiation for 30 min, spherical-type microplastic inhalation risk posed by wearing masks for 2 h increased 1.33, 0.23, 3.72, 1.28, 4.84, 1.86, and 1.07 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. After treating via alcohol disinfection, spherical-type microplastic inhalation risk posed by wearing masks for 2 h increased 9.07, 3.41, 1.40, 1.57, 6.68, 2.35, and 3.51 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For air blower treatment, spherical-type microplastic inhalation risk posed by wearing masks for 2 h increased 3.31, 1.45, 2.99, 0.96, 0.25, −0.06, and 1.64 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For washing with water treatment, spherical-type microplastic inhalation risk posed by wearing masks for 2 h increased 0.16, 0.47, 0.15, 0.97, 0.38, 0.17, and 0.10 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For sunlight irradiation, spherical-type microplastic inhalation risk posed by wearing masks for 2 h increased 1.52, 0.01, 1.20, 0.60, 0.74, 0.03, and 1.99 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively.
Fig. 3.
Accumulated particles observed with the seven commonly used masks after different treatments for reuse.
Table 5.
Kinetic coefficients of particle accumulation after the 12 h breathing simulation test with different types of masks that underwent various treatment processes for reuse.
| N95 | Surgical-A | Cotton | Fashion | Non-woven | Surgical-B | Activated carbon | ||
|---|---|---|---|---|---|---|---|---|
| UV - 30 min | R2 | 0.998 | 0.9986 | 0.9995 | 0.9957 | 0.996 | 0.9996 | 0.9993 |
| k | 1322.1 | 951.8 | 3310.1 | 1755.6 | 4033.5 | 2706.4 | 1236.2 | |
| Alcohol disinfection | R2 | 0.9956 | 0.9997 | 0.9994 | 0.9992 | 0.9974 | 0.9994 | 0.9995 |
| k | 5659.6 | 3034.6 | 2069.5 | 2619.5 | 7452.7 | 3832.5 | 3360.0 | |
| Air blower disinfection | R2 | 0.9992 | 0.9994 | 0.9929 | 0.9987 | 0.9959 | 0.9993 | 0.9997 |
| k | 1982.7 | 1534.4 | 2460.9 | 2026.9 | 1147.8 | 1045.4 | 1822.3 | |
| Washing | R2 | 0.9965 | 0.9995 | 0.999 | 0.9952 | 0.9987 | 0.9987 | 0.9988 |
| k | 635.1 | 1013.7 | 1047.6 | 2410.5 | 1202.9 | 1471.1 | 913.5 | |
| Sunlight irradiation | R2 | 0.9994 | 0.9996 | 0.9978 | 0.9984 | 0.9997 | 0.9983 | 0.9987 |
| k | 1398.2 | 670.56 | 1544.7 | 1720.2 | 1520.2 | 894.8 | 2167.9 | |
| Blank -New mask | R2 | 0.9988 | 0.9987 | 0.9959 | 0.9975 | 0.998 | 0.9982 | 0.994 |
| k | 656.3 | 756.3 | 1024.7 | 1207.0 | 993.5 | 1039.8 | 945.0 |
The increase in microplastic inhalation risk after different treatments exhibited minimal changes when the masks were worn for 2, 4, 6, 8, 10, and 12 h. The results indicated that washing with water and natural drying indoor is the gentlest method for treating masks for reuse, in which damage to all mask structures and spherical-type microplastic inhalation risk were the lowest. Alcohol disinfection caused the heaviest damage to the masks’ structures, particularly for N95. Sunlight irradiation has the lowest effect on surgical masks. These results can also be observed in Table 5, where the k value of the masks was considerably increased after treatment with alcohol compared with the other treatment processes. This finding can also be related to the quality of commercially available masks (Cherrie et al., 2018).
Fiber-like microplastic inhalation risk also increased after disinfection treatment for mask reuse compared with that without treatment ( Fig. 4 and Table 6 and Table S3). The amount of fiber-like microplastics was still lower than that of spherical-type microplastics in all the cases. After treating with UV irradiation for 30 min, fiber-like microplastic inhalation risk posed by wearing masks for 2 h increased 0.80, 0.66, 0.83, −0.13, 1.17, 0, and 0.21 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. After treating with alcohol disinfection, fiber-like microplastic inhalation risk posed by wearing masks for 2 h increased 2.96, 2.63, 2.91, 0.48, 2.89, 1.79, and 0.89 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For air blower treatment, fiber-like microplastic inhalation risk posed by wearing masks for 2 h increased 4.28, 1.68, 0.66, 2.48, 6.91, −0.17, and 0.70 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For washing with water, fiber-like microplastic inhalation risk posed by wearing masks for 2 h increased 2.24, 0.58, 0.13, 2.74, 1.30, 0.47, and 0.38 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. For sunlight irradiation, fiber-like microplastic inhalation risk posed by wearing masks for 2 h increased 1.04, 0.26, 1.10, 0.39, 1.23, 0.34, and 0.72 times for N95, surgical-A, cotton, fashion, nonwoven, surgical-B, and activated carbon masks, respectively. The increase in fiber-like microplastic inhalation risk after different treatment processes was slightly reduced by wearing masks for 2, 4, 6, 8, 10, and 12 h. The results implied that nearly all the disinfection treatments exerted the highest effect on N95 (Liao et al., 2020, Mills et al., 2018, Xiang et al., 2020). Meanwhile, the amount of fiber-like microplastics observed when using N95 after different disinfection treatments was still lower than those of the other masks (k = 23.1–66.6 for N95, k = 25–211.8 for the other masks). This finding provides the conclusion that N95 achieves better performance in reducing fiber-like microplastic inhalation risk even after undergoing different disinfection treatments.
Fig. 4.
Accumulated fiber-like microplastics observed with the seven commonly used masks after different treatments for reuse.
Table 6.
Kinetic coefficients of fiber-like microplastic accumulation after the 12 h breathing simulation test with different types of masks that underwent various treatment processes for reuse.
| N95 | Surgical-A | Cotton | Fashion | Non-woven | Surgical-B | Activated carbon | ||
|---|---|---|---|---|---|---|---|---|
| UV - 30 min | R2 | 0.9964 | 0.9989 | 0.9994 | 0.9964 | 0.9924 | 0.9978 | 0.9997 |
| k | 23.1 | 25.0 | 57.1 | 47.5 | 41.7 | 56.2 | 122.9 | |
| Alcohol disinfection | R2 | 0.9985 | 0.9931 | 0.9967 | 0.995 | 0.9937 | 0.9956 | 0.9931 |
| k | 54.4 | 70.7 | 174.3 | 56.4 | 98.4 | 169.5 | 202.6 | |
| Air blower disinfection | R2 | 0.994 | 0.9957 | 0.9986 | 0.9985 | 0.9997 | 0.9911 | 0.9975 |
| k | 66.6 | 68.5 | 79.7 | 146.6 | 211.8 | 56.7 | 186.9 | |
| Washing | R2 | 0.994 | 0.9949 | 0.9964 | 0.9959 | 0.9962 | 0.9966 | 0.9878 |
| k | 48.9 | 30.9 | 56.9 | 128.3 | 70.7 | 75.4 | 142.6 | |
| Sunlight irradiation | R2 | 0.9936 | 0.9939 | 0.992 | 0.9954 | 0.9978 | 0.9984 | 0.9987 |
| k | 33.6 | 35.4 | 89.8 | 49.0 | 48.7 | 79.2 | 161.6 | |
| Blank -New mask | R2 | 0.9956 | 0.9952 | 0.9971 | 0.997 | 0.9969 | 0.9945 | 0.9968 |
| k | 17.8 | 21.1 | 51.0 | 36.0 | 29.6 | 54.0 | 103.8 |
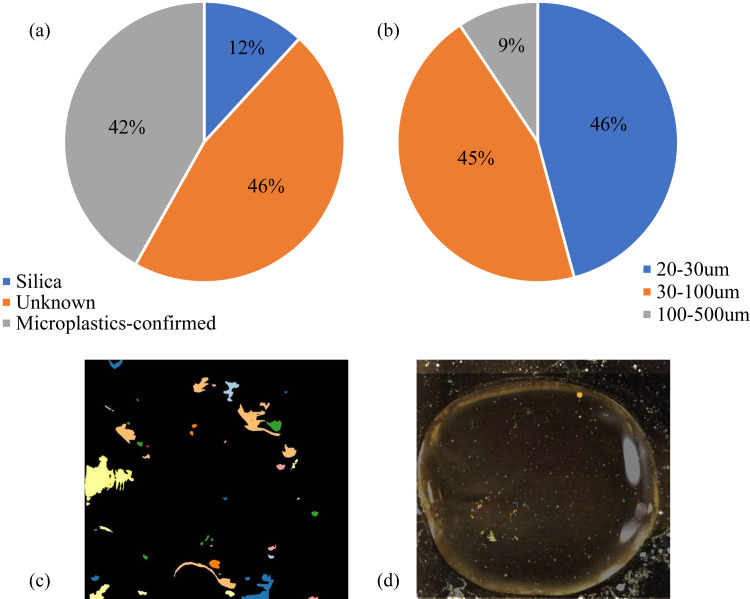
3.3. Microplastic identification from the breathing test
The spherical- and fiber-like microplastics collected during the breathing test by using different type of masks were identified under a microscope. To increase accuracy, the new platform, LDIR, was used. In this separate test, surgical-A mask was used for the breathing test for 2 h, and the collected microplastics were identified under LDIR. The microplastics observed and counted under the microscope were comparable with those identified under LDIR. The results indicated that 12% of the collected particles are silica, 42% can be confirmed as microplastics (12 different materials), and 46% are unknown ( Fig. 5). The unknown components can be due to the lack of data in the system database, but they also exhibit high potential to be classified as microplastics. The FTIR spectrometry results indicated that nearly all the particles found are plastics, although some of the materials cannot be identified due to lack of information in the database. The diameter of the identified particles ranged from 20 µm to 500 µm, with 20–30, 30–100, and 100–500 µm accounting for 46%, 45%, and 9%, respectively. Detailed information of the microplastic materials are provided in Fig. S3. The amount of available microplastics observed via Raman spectrometry of per 100 particles on the filtered membrane during the 2 h suction tests for all the masks were also determined (Fig. S4). The results indicated that 20–30% of the particles (mostly spherical-type particles) were microplastics. This value was slightly lower compared with the results of LDIR. Such discrepancy can be attributed to the detection limitation of Raman spectroscopy, wherein small particles are not detected and some peaks are unavailable in the library. Nonetheless, nearly all the fiber-like particles were easily identified as microplastics. The spherical microplastics still has a large amount even when calculated in terms percentage. The LDIR results also supported the finding that over 90% of the identified particles are 20–100 µm. Although the effects of microplastics and other particles in the air on humans remain unclear, the results of this study still provide sufficient guidance in wearing masks.
Fig. 5.
Particle material identification results of LDIR (a – microplastic percentage, b – particle diameter distribution, c – observed microplastic fragments, d – one drop of sample with water prepared and observed under this platform).
3.4. Microbiology concern of reusing masks
In this study, we conducted experiments with mask reuse from 2 to 720 h. Wearing masks is recommended for 2–4 h during the COVID-19 pandemic. Reusing masks may increase the risks posed by the virus remaining on a mask’s surface and being passed through the mask or transferred to the body. However, some people reuse masks with or without applying disinfection treatment. Changing mask is recommended when it was used in a public place for 2–4 h or similar cases where droplet transmission can occur. In this study, we tested microplastic inhalation risk posed by wearing masks after undergoing different disinfection treatments. However, virus detection was not included in this study. Hence, the results of this study regarding mask reuse will be unable to provide suggestions for preventing COVID-19 transmission. Masks become an environmental problem when improper used and disposed of. The results of this study can provide suggestions for mask use and reuse and for reducing microplastic and particle inhalation risks in places where COVID-19 is under control.
3.5. Perspectives
In this study, the experiments with mask reuse were conducted from 2 to 720 h. Even though the data quantity was quite large, it is still recommended to conduct triplicate test to ensure the reliability of the data. A triplicate inhalation test of all the masks tested in this study for 2–4 h was conducted (Table S6). The results revealed that the amount of spherical- and fiber like microplastics amount error between triplicate test of all the masks were acceptable. 50% of the data has an error at 0–10%, 35.38% of the data has an error at 10–20%, 15.63% of the data has an error at over 20%. The highest error occurred with surgical-B mask, which the fiber-like microplastics has error of 37.85% for 2 h inhalation test, and 29.96% for 4 h inhalation test for triplicate test of three masks. At the same time, it is also important to identify the source of the fiber-like microplastics, whether it is come from the mask itself or the air. We also conducted tests by observing the fiber-like microplastics under the microscope, with the microplastics from inhalation test and by rub the masks manually (Fig. S5). The fiber-like microplastics from the air are too small to be picked by tweezer, thus little amount of fiber were shown on Fig. S5 from blank. The results show that the fiber-like microplastics could source from both the air the mask itself, more study to identify also can be conducted in the near future if new reliable technology are developed.
4. Conclusions
This study investigated spherical- and fiber-like microplastic inhalation risks posed by using masks for 2–720 h and reusing masks that underwent different disinfection processes. The inhalation risk posed by spherical- and fiber-like microplastics was high regardless of with or without wearing a mask. N95 exhibited good performance in reducing spherical- and fiber-like microplastic inhalation compared with the other masks and no mask even after undergoing different disinfection treatments. For masks without treatment used for 720 h, spherical-type microplastic inhalation risk continuously decreased compared with not wearing a mask. Meanwhile, fiber-like microplastic inhalation risk increased, except for N95. All the investigated disinfection processes led to varying extents of microplastic inner structure damage, increasing the risk of microplastic inhalation. Nonetheless, the use of masks is crucial during the pandemic scenario even though they might contribute some microplastics inhalation, it is minor problem as compared with protecting humans from COVID-19.
CRediT authorship contribution statement
Lu Li: Writing, Methodology, Data curation. Xiaoli Zhao: Review, Editing. Zhouyang Li: Data curation, Methodology. Kang Song: Review, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The research was supported by National Natural Science Foundation of China (Grant number 41925031), China Postdoctoral Science Foundation (Grant no. 2019M652738), Dr. Kang Song acknowledges the supports from 100 Talents Program of Chinese Academy of Sciences (E029040201, E051040101) and the supports from National Natural Science Foundation of China (Grant number 41877344).
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jhazmat.2020.124955.
Appendix A. Supplementary material
Supplementary material
.
Supplementary material
.
References
- Abbasi S., Keshavarzi B., Moore F., Turner A., Kelly F.J., Dominguez A.O., Jaafarzadeh N. Distribution and potential health impacts of microplastics and microrubbers in air and street dusts from Asaluyeh county, Iran. Environ. Pollut. 2019;244:153–164. doi: 10.1016/j.envpol.2018.10.039. [DOI] [PubMed] [Google Scholar]
- Aragaw T.A. Surgical face masks as a potential source for microplastic pollution in the COVID-19 scenario. Mar. Pollut. Bull. 2020;159 doi: 10.1016/j.marpolbul.2020.111517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherrie J.W., Apsley A., Cowie H., Steinle S., Mueller W., Lin C., Loh M. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup. Environ. Med. 2018;75(6):446–452. doi: 10.1136/oemed-2017-104765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua, M.H., Cheng, W., Goh, S.S., Kong, J., Li, B., Lim, J.Y.,. Ye, E. 2020. Face Masks in the New COVID-19 Normal: Materials, Testing, and Perspectives. Research, 2020. [DOI] [PMC free article] [PubMed]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J. 2020. Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. published online June 1. DOI: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed]
- da Costa Filho P.A., Cobuccio L., Mainali D., Rault M., Cavin C. Rapid analysis of food raw materials adulteration using laser direct infrared spectroscopy and imaging. Food Control. 2020;113 [Google Scholar]
- Davies A., Thompson K., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med. Public Health Prep. 2013;7:413–418. doi: 10.1017/dmp.2013.43. 413-8.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dris R., Gasperi J., Mirande C., Mandin C., Guerrouache M., Langlois V., Tassin B. A first overview of textile fibers, including microplastics, in indoor and outdoor environments. Environ. Pollut. 2017;221:453–458. doi: 10.1016/j.envpol.2016.12.013. [DOI] [PubMed] [Google Scholar]
- Fadare O.O., Okoffo E.D. Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faridi S., Nodehi R.N., Sadeghian S., Tajdini M., Hoseini M., Yunesian M., Naddafi K. Can respirator face masks in a developing country reduce exposure to ambient particulate matter? J. Expo. Sci. Environ. Epidemiol. 2020;30:606–617. doi: 10.1038/s41370-020-0222-6. [DOI] [PubMed] [Google Scholar]
- Garcia G.J., Schroeter J.D., Kimbell J.S. Olfactory deposition of inhaled nanoparticles in humans. Inhal. Toxicol. 2015;27(8):394–403. doi: 10.3109/08958378.2015.1066904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasperi, J., Dris, R., Mirande-Bret, C., Mandin, C., Langlois, V., Tassin, B. (2015, September). First overview of microplastics in indoor and outdoor air. [DOI] [PubMed]
- Gasperi J., Wright S.L., Dris R., Collard F., Mandin C., Guerrouache M., Tassin B. Microplastics in air: are we breathing it in? Curr. Opin. Environ. Sci. Health. 2018;1:1–5. [Google Scholar]
- Greenhalgh T., Howard J. Masks for all? The science says yes. April 13, 2020. Available from: 〈https://www.fast.ai/2020/04/13/masks-summary/〉.
- Jung S., Lee S., Dou X., Kwon E.E. Valorization of disposable COVID-19 mask through the thermo-chemical process. Chem. Eng. J. 2020;405 doi: 10.1016/j.cej.2020.126658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao L., Xiao W., Zhao M., Yu X., Wang H., Wang Q., Cui Y. Can N95 respirators be reused after disinfection? How many times? ACS Nano. 2020;14:6348–6356. doi: 10.1021/acsnano.0c03597. [DOI] [PubMed] [Google Scholar]
- Liu K., Wang X., Fang T., Xu P., Zhu L., Li D. Source and potential risk assessment of suspended atmospheric microplastics in Shanghai. Sci. Total Environ. 2019;675:462–471. doi: 10.1016/j.scitotenv.2019.04.110. [DOI] [PubMed] [Google Scholar]
- Liu P., Wang B., Zhao X., Duan X., Huang N., Chen Y. Chinese adult respiratory volume study. J. Environ. Health. 2014;31(011):953–956. [Google Scholar]
- Mills D., Harnish D.A., Lawrence C., Sandoval-Powers M., Heimbuch B.K. Ultraviolet germicidal irradiation of influenza-contaminated N95 filtering facepiece respirators. Am. J. Infect. Control. 2018;46(7):e49–e55. doi: 10.1016/j.ajic.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neupane B.B., Mainali S., Sharma A., Giri B. Optical microscopic study of surface morphology and filtering efficiency of face masks. PeerJ. 2019;7 doi: 10.7717/peerj.7142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu Y., Zheng J., Chen F., Long Y., Wu H., Li Q., Ning X. Preparation of polypropylene micro and nanofibers by electrostatic-assisted melt blown and their application. Polymers. 2018;10(9):959. doi: 10.3390/polym10090959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos, M., Torres, D., Cardoso, P.C., Pandis, N., Flores-Mir, C., Medeiros, R., Normando, D. 2020. Are Cloth Masks a Substitute to Medical Masks in reducing transmission and contamination? A Systematic Review. medRxiv. [DOI] [PubMed]
- Scircle A., Cizdziel J.V., Tisinger L., Anumol T., Robey D. Occurrence of microplastic pollution at oyster reefs and other coastal sites in the Mississippi sound, USA: impacts of freshwater inflows from flooding. Toxics. 2020;8(2):35. doi: 10.3390/toxics8020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakya K., Noyes A., Kallin R., Peltier R. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J. Expo. Sci. Environ. Epidemiol. 2017;27:352–357. doi: 10.1038/jes.2016.42. [DOI] [PubMed] [Google Scholar]
- Song, W., Pan, B., Kan, H., Xu, Y., Yi, Z. 2020. Heat Inactivating and Reusing of Virus-Contaminated Disposable Medical Mask. medRxiv.
- Tian L., Shang Y., Dong J., Inthavong K., Tu J. Human nasal olfactory deposition of inhaled nanoparticles at low to moderate breathing rate. J. Aerosol Sci. 2017;113:189–200. [Google Scholar]
- Vianello A., Jensen R.L., Liu L., Vollertsen J. Simulating human exposure to indoor airborne microplastics using a breathing thermal manikin. Sci. Rep. 2019;9(1):1–11. doi: 10.1038/s41598-019-45054-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y., Song Q., Gu W. Decontamination of surgical face masks and N95 respirators by dry heat pasteurization for one hour at 70° C. Am. J. Infect. Control. 2020;48:880–882. doi: 10.1016/j.ajic.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Xu E.G., Li J., Chen Q., Ma L., Zeng E.Y., Shi H. A review of microplastics in table salt, drinking water, and air: direct human exposure. Environ. Sci. Technol. 2020;54(7):3740–3751. doi: 10.1021/acs.est.9b04535. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Supplementary material