Abstract
BACKGROUND
Cisplatin is widely used to treat adult and pediatric cancers. It is the most ototoxic drug in clinical use, resulting in permanent hearing loss in approximately 50% of treated patients. There is a major need for therapies that prevent cisplatin-induced hearing loss. Studies in mice suggest that concurrent use of statins reduces cisplatin-induced hearing loss.
METHODS
We examined hearing thresholds from 277 adults treated with cisplatin for head and neck cancer. Pretreatment and posttreatment audiograms were collected within 90 days of initiation and completion of cisplatin therapy. The primary outcome measure was a change in hearing as defined by the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE).
RESULTS
Among patients on concurrent atorvastatin, 9.7% experienced a CTCAE grade 2 or higher cisplatin-induced hearing loss compared with 29.4% in nonstatin users (P < 0.0001). A mixed-effect model analysis showed that atorvastatin use was significantly associated with reduced cisplatin-induced hearing loss (P ≤ 0.01). An adjusted odds ratio (OR) analysis indicated that an atorvastatin user is 53% less likely to acquire a cisplatin-induced hearing loss than a nonstatin user (OR = 0.47; 95% CI, 0.30–0.78). Three-year survival rates were not different between atorvastatin users and nonstatin users (P > 0.05).
CONCLUSIONS
Our data indicate that atorvastatin use is associated with reduced incidence and severity of cisplatin-induced hearing loss in adults being treated for head and neck cancer.
TRIAL REGISTRATION
ClinicalTrials.gov identifier NCT03225157.
FUNDING
Funding was provided by the Division of Intramural Research at the National Institute on Deafness and Other Communication Disorders (1 ZIA DC000079, ZIA DC000090).
Keywords: Oncology, Otology
Keywords: Head and neck cancer, Neurological disorders
Introduction
Cisplatin is among the most effective and widely used anticancer drugs, used to treat a variety of solid tumors, including testicular, ovarian, bladder, cervical, head and neck, and numerous other malignancies. Due in part to the efficacy of cisplatin (1), there are currently an estimated 16.9 million cancer survivors in the United States (2). Consequently, there is intense clinical and research interest in issues of survivorship and quality of life for these survivors. Many individuals treated with cisplatin experience significant toxicities, including nephrotoxicity, neurotoxicity, myelosuppression, and ototoxicity. Over 50% of patients who undergo cisplatin therapy acquire a sensorineural hearing loss (3–7), which compromises daily communication with friends, family, and health care providers and can lead to loneliness, social isolation, and frustration (8). Cisplatin-induced hearing loss is permanent, and there are currently no FDA-approved therapies to reduce or prevent cisplatin ototoxicity.
Here we explore the potential for concomitant statin drug use during chemotherapy to reduce or prevent cisplatin-induced hearing loss in patients undergoing cisplatin therapy to treat head and neck cancer. Statins are hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors, a class of drugs used primarily to reduce hyperlipidemia in individuals at risk for cardiovascular disease. In addition to their effects on HMG-CoA reductase, statins have a variety of effects, including improved endothelial function and microcirculation (9), decreased inflammation (10–12), and reduced oxidative stress (13, 14). Statins have been associated with decreased risk of stroke (15, 16) and CNS disorders (17–19). Overall, statins have good safety profiles in humans; however, important side effects of statin use include myopathy, liver dysfunction, and rare cases of rhabdomyolysis (20).
Previous studies in animal models have demonstrated a protective effect of statin administration against hearing loss caused by noise trauma (21–24), age-related hearing loss (presbycusis) (25), and aminoglycoside antibiotic–induced hearing loss (26). In humans, statin use is associated with improved hearing function in older adults (27, 28), improved auditory sensitivity in subjects with noise-induced hearing loss (29), and reduced tinnitus (29, 30). More recently, our lab has shown that lovastatin reduces cisplatin-induced hearing loss in mice (31). Mice that received lovastatin during cyclic administration of cisplatin demonstrated reduced hearing loss as measured by auditory brainstem response testing (32). A recent review summarizes the role of statins as otoprotective agents in animal and human studies (33). Taken together, these data suggest that statin use may be associated with a reduced amount of hearing loss caused by a variety of stressors to the inner ear that can otherwise result in permanent damage.
Given the unmet clinical need for therapies to reduce cisplatin-induced hearing loss, we examined the relationship between statin use and cisplatin-induced hearing loss in patients undergoing cisplatin-based chemoradiation therapy (CRT) to treat head and neck cancer. Hearing test data obtained before and after cisplatin therapy from 277 subjects were examined using a combined retrospective and prospective observational study design. Using 2 established ototoxicity scales, the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) (34) and TUNE (35), we compared the incidence and severity of cisplatin-induced hearing loss between patients taking a statin compared with those not taking a statin to determine the relationship between statin use and cisplatin-induced hearing loss.
Results
Characteristics of the data set.
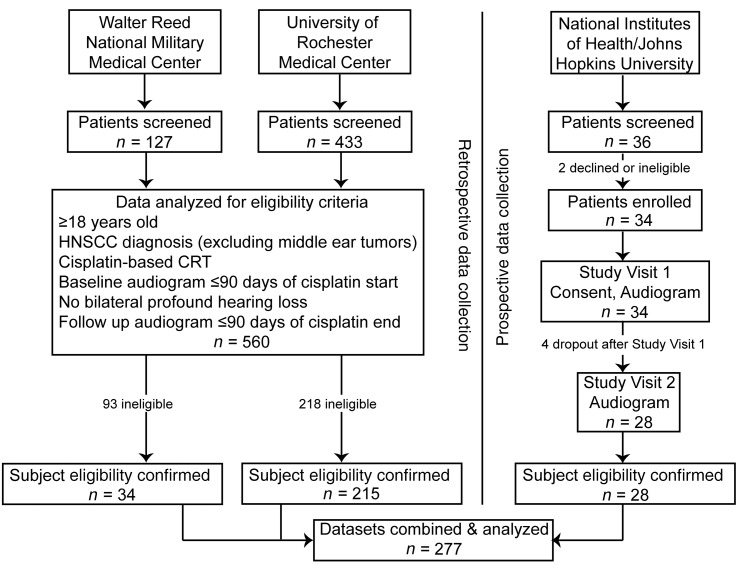
Retrospective and prospective data were combined for a total of 277 subjects (Figure 1). All subjects met study eligibility criteria; they were adults newly diagnosed with head and neck squamous cell carcinomas (HNSCCs) and treated with cisplatin-based CRT. The characteristics of the 277 subjects are shown in Table 1. Individuals with middle ear tumors were excluded at screening (n = 2) because of active middle ear disease confirmed by bone conduction audiometry. Of the eligible 277 subjects, 6 had a unilateral hearing loss at baseline that met exclusion criteria for that ear (≥95 dB HL average threshold at 1, 2, and 4 kHz or an indication of active middle ear disease). These 6 subjects with unilateral profound hearing loss were retained in the study; however, only the better ear was included in analyses. In total, 546 ears from 277 subjects were included in the analyses. Ears were treated independently in the data analysis because of ear-specific differences in baseline hearing sensitivity and differences in radiation doses to the cochlea. The use of 2 ears in the data set was controlled for statistically in a mixed-effect model analysis as a random effect.
Figure 1. Flow diagram of study design and participants.
Retrospective and prospective data were combined for analyses. Two institutions, Walter Reed National Military Medical Center and the University of Rochester Medical Center, contributed retrospective audiometric data pertaining to subjects meeting study eligibility criteria. Additional data were collected prospectively through an observational clinical study conducted by the NIH in partnership with Johns Hopkins University. Eligibility criteria were the same in both the retrospective and prospective segments. A total of 277 subjects were included in the analyses.
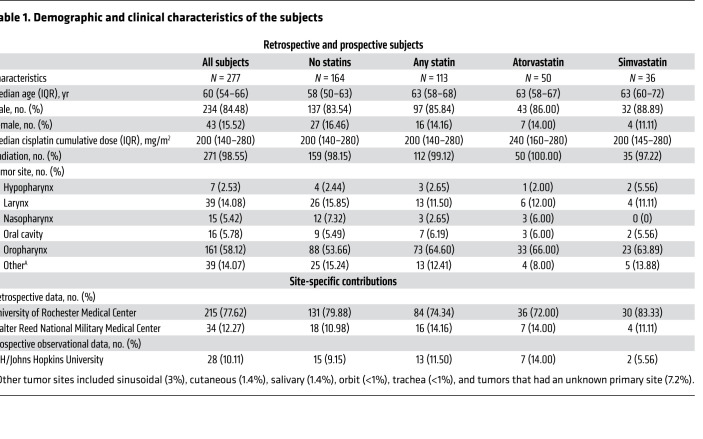
Table 1. Demographic and clinical characteristics of the subjects.
Statin use among study subjects.
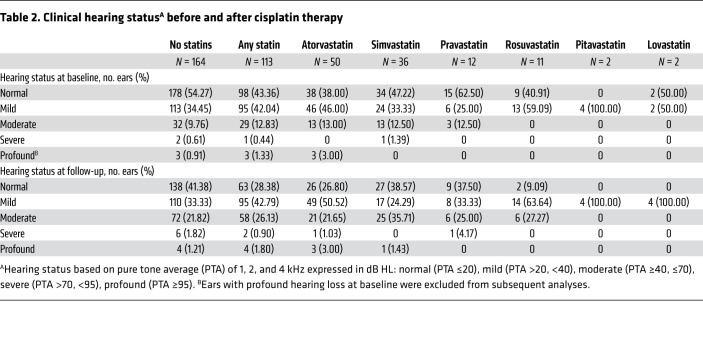
Subjects were assigned to groups based on whether they were (or were not) taking a statin medication at the onset of cisplatin therapy. Details pertaining to the duration of statin use prior to baseline data collection and the primary indication necessitating statin use were not obtained. Of the study subjects, 59.2% (27 female, 137 male) were nonstatin users and 40.8% (16 female, 97 male) were statin users. Within the statin user group, 6 different statins were represented (Table 2). Of the 113 statin users, atorvastatin (dose range 10–80 mg) was used by 44.2% of subjects (n = 50 subjects, 97 ears), simvastatin (dose range 5–40 mg) by 31.9% (36 subjects, 72 ears), pravastatin (dose range 10–80 mg) by 10.6% (12 subjects, 24 ears), rosuvastatin (dose range 10–40 mg) by 9.7% (11 subjects, 22 ears), pitavastatin (2 mg dose only) by 1.8% (2 subjects, 4 ears), and lovastatin (40 mg dose only) by 1.8% (2 subjects, 4 ears). We first compared the cisplatin-induced threshold shift between nonstatin users versus those taking any statin. Because atorvastatin and simvastatin were highly represented among our 113 statin users (76.1% of total), we also compared hearing loss between nonstatin users versus those taking atorvastatin (n = 50) or simvastatin (n = 36); however, although the comparison between atorvastatin and nonstatin users remained sufficiently powered, our study was underpowered for the comparison of simvastatin users versus those not taking a statin.
Table 2. Clinical hearing statusA before and after cisplatin therapy.
Tumor types and cisplatin regimens.
Most of our subjects had HNSCC that localized to either the oropharynx (58.1%) or the larynx (14.1%) (Table 1). A small portion of tumors localized to the oral cavity (5.8%), nasopharynx (5.4%), or the hypopharynx (2.5%). Tumor sites classified as “other” comprised 14.1% of all tumor types and consisted of sinonasal (2.9%) cutaneous (1.4%), salivary (1.4%), orbit (<1%), trachea (<1%), and tumors that had an unknown primary site (7.2%). All subjects were treated with cisplatin-based chemotherapy and nearly all (98.6%) had CRT. Low-dose, weekly cisplatin treatment, defined as cisplatin doses less than 75 mg/m2 per infusion, was administered to 53.6% of subjects. The remaining 46.4% of subjects received high-dose cisplatin (≥75 mg/m2 per infusion) administered approximately once every 3 weeks; however, 9.4% of individuals scheduled to receive high-dose therapy were switched to low-dose therapy because of drug intolerance and/or ototoxicity. The median cumulative cisplatin dose for all subjects was 200 mg/m2 (IQR, 140–280 mg/m2). This cumulative dose was consistent across all groups, and the median cumulative cisplatin dose was 200 mg/m2 (IQR, 155–280 mg/m2) for nonstatin users, 200 mg/m2 (IQR, 135–280 mg/m2) for all statin users, and 240 mg/m2 (IQR, 160–280 mg/m2) and 200 (IQR, 145–280 mg/m2) for atorvastatin and simvastatin users, respectively.
Other subject characteristics.
Other demographic characteristics, such as sex, age, and preexisting hearing loss were comparable across groups (Tables 1 And 2). The median age for all subjects was 60 years (IQR, 54–66). Nonstatin users, on average, were slightly younger than those in the any statin user group (median age 58 vs. 63) and had better hearing at baseline (Table 2). Consistent across all groups was a predominance toward males (>83% male) who received concurrent radiation (>97% with radiation). Fifty-four percent of nonstatin user ears (n = 328 ears) had normal hearing at baseline (defined as the pure tone average [PTA] ≤20 dB HL), 34% had a mild hearing loss (PTA >20, <40), and 10% had moderate hearing loss (PTA ≥40, ≤70). Statin user ears (n = 226 ears) consisted of 43% normal, 42% mild hearing loss, and 13% moderate hearing loss. Similarly, atorvastatin user ears (n = 100 ears) included 38% normal hearing, 46% mild hearing loss, and 13% moderate hearing loss. After cisplatin therapy, with the exception of those subjects on concurrent pitavastatin (n = 2) where both subjects started and ended therapy with a bilateral mild hearing loss, ears analyzed as part of the nonstatin user and other 5 statin user groups showed a decrease in the percentage of ears categorized as having normal hearing and an increase toward more severe hearing loss (Table 2).
Atorvastatin users have less cisplatin-induced hearing loss than those not taking a statin.
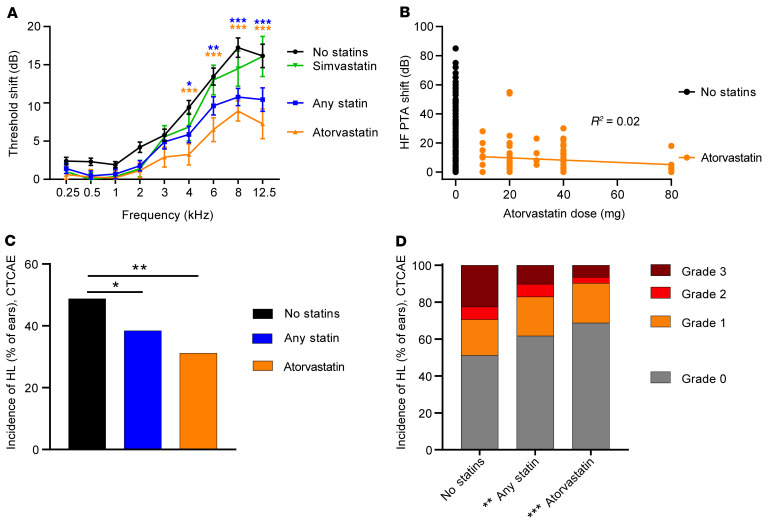
In total, 546 ears from 277 subjects were included in the analyses. The primary outcome measure was the incidence of CTCAE-defined change in hearing, which relies first on the calculation of the change in auditory thresholds (“threshold shifts”) between the baseline and posttreatment audiograms. Therefore, we began our analysis by examining threshold shift data among subjects as a function of their status of concurrent statin use at baseline. On average, cisplatin therapy resulted in a 13.7 dB ± 18.6 high-frequency threshold shift (PTA of 6, 8, and 12.5 kHz) (Figure 2A). A 2-way ANOVA indicated a significant effect of treatment group (nonstatin vs. any statin, atorvastatin, or simvastatin) on threshold shifts (2-way ANOVA, F3, 5802 = 29.06, P < 0.001) as well as a significant effect of frequency (F8, 5802 = 55.87, P < 0.001). To explore the significant interaction of the 2 effects (F24, 5802 = 1.599, P < 0.001), a Dunnett’s multiple-comparison post hoc analysis was conducted comparing threshold shift at each frequency for nonstatin users with either the any statin, atorvastatin, or simvastatin user groups. Threshold shifts at frequencies equal to or greater than 4 kHz were significantly reduced among subjects taking any statin relative to nonstatin users (P < 0.02). Threshold shifts were further reduced among atorvastatin users (P < 0.001). In contrast, no significant reduction in threshold shift was observed among simvastatin users. However, although the comparison between atorvastatin and nonstatin users remained sufficiently powered (>80% power, α = 0.05), our study was underpowered for the comparison of simvastatin users versus nonstatin users.
Figure 2. Atorvastatin use is associated with reduced cisplatin-induced hearing loss.
Baseline audiometric thresholds were compared with thresholds obtained after cisplatin treatment to determine threshold shifts. (A) In subjects not taking a statin (N = 324 ears), cisplatin treatment resulted in threshold shifts that were more severe at higher frequencies. Subjects taking any statin (N = 219 ears) had significantly less cisplatin-induced hearing loss than subjects who were not taking a statin. Atorvastatin users (N = 97 ears) had significantly less cisplatin-induced hearing loss than nonstatin users. In contrast, cisplatin-induced threshold shifts among simvastatin users (N = 70 ears) were not significantly different from those of nonstatin users. Data represent mean ± SEM, 2-way ANOVA, Dunnett’s multiple-comparison test. (B) Atorvastatin dose was not correlated with high-frequency (6–12.5 kHz) hearing loss. Each dot represents 1 ear. Nonstatin users (N = 324 ears) had 15.9 ± 20.3 dB shifts in high-frequency pure tone average (HF PTA). Atorvastatin users (N = 97 ears) had shifts of 7.8 ± 11.8 dB. There was no correlation between atorvastatin dose and threshold shift. Pearson R correlation. (C) The incidence of cisplatin-induced hearing loss among nonstatin users was 48% per CTCAE criteria. Subjects taking any statin had significantly lower incidence of hearing loss than nonstatin users. The incidence of hearing loss was further reduced among atorvastatin users. Data are percentage of ears per group. Statistical analysis consisted of the χ2 test. (D) Statin use, atorvastatin in particular, was associated with reduced severity of hearing loss. CTCAE criteria were used to categorize the severity of hearing loss. χ2 Analysis showed a significant difference in the distribution of CTCAE hearing loss grades, where the incidence of a grade 2 or higher hearing loss was reduced in statin users compared with nonstatin users. This difference was even greater for atorvastatin users. Data are percentage of ears per group. *P < 0.05, **P < 0.01, ***P < 0.001.
Our cohort included individuals taking a range of atorvastatin doses from 10 to 80 mg. We examined the relationship between high-frequency hearing loss (PTA of 6, 8, and 12.5 kHz) and atorvastatin dose and found no significant correlation (R2 = 0.023, P > 0.05, Figure 2B), suggesting that the reduction in hearing loss we observed among atorvastatin users was independent of atorvastatin dose.
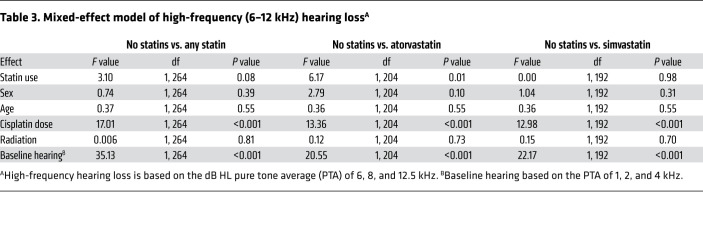
We applied a mixed-effects model (MEM) analysis to our average high-frequency threshold shift data to examine the contributions of other variables to cisplatin-induced hearing loss. Controlling for all other fixed effects in the model (sex, age, cumulative cisplatin dose, concurrent radiation, and preexisting hearing loss at baseline) and controlling for the inclusion of data from 2 ears for most subjects (random effect), atorvastatin use was significantly correlated with reduced hearing loss by applying the SAS PROC GLIMMIX procedure (F1,204 = 6.42, P = 0.02) (Table 3). Significant effects were also observed for cumulative cisplatin dose (F1, 204 = 13.45, P < 0.001) and baseline hearing (F1, 204 = 17.84, P < 0.001). Together, these data indicate that atorvastatin users had significantly less cisplatin-induced hearing loss than nonstatin users.
Table 3. Mixed-effect model of high-frequency (6–12 kHz) hearing lossA.
Atorvastatin use is associated with reduced incidence and severity of cisplatin-induced hearing loss.
We next applied CTCAE v5.0 (34) criteria to report the incidence and severity of a hearing loss. Among subjects not taking any statin, the incidence of hearing loss was 48.8% (CTCAE, Figure 2C). The incidence of a grade 1 or higher hearing loss was significantly reduced from 48.8% in nonstatin users to 38.4% (χ2 = 5.6, P < 0.02) in statin users, with further reduction to 31.2% (χ2 = 9.0, P < 0.01) among atorvastatin users. Similar results were obtained when we applied the TUNE (35) ototoxicity grading criteria (Supplemental Methods; supplemental material available online with this article; https://doi.org/10.1172/JCI142616DS1). These data indicate that the incidence of cisplatin-induced hearing loss was significantly reduced in atorvastatin users relative to those not taking a statin.
In addition to incidence, CTCAE reports severity of hearing loss using a 1–4 scale in which grade 4 denotes the most severe change in hearing. Grade 1 is considered mild where intervention may not be required, and grade 2 is considered a moderate adverse event for which intervention is indicated (34). The incidence of a hearing change with a CTCAE grade equal to or greater than 2 was significantly reduced from 29.4% in the nonstatin user group to 9.7% for atorvastatin users (χ2 = 14.9, P = 0.0001) (Figure 2D). These data indicate that cisplatin-induced hearing loss was also less severe among atorvastatin users compared with nonstatin users.
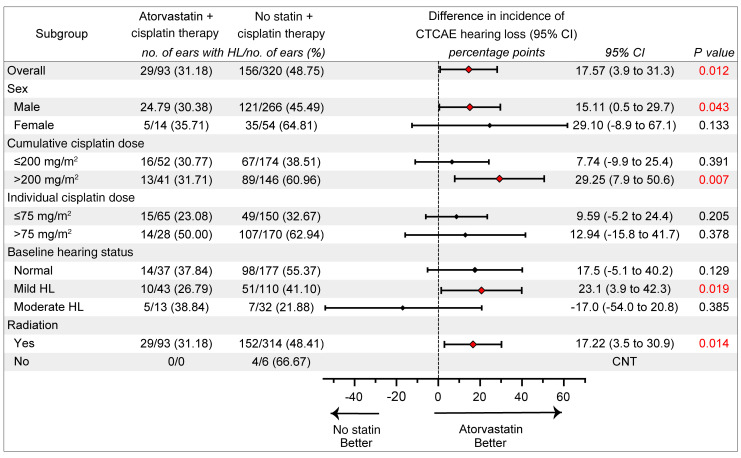
The benefits of atorvastatin to the incidence of a CTCAE-defined hearing loss were generally consistent across all subgroups (Figure 3). Overall, 48.8% (156 of 320) of ears among nonstatin users showed hearing loss, compared with 31.2% (29 of 93) of ears among atorvastatin users. In addition to a significant benefit of atorvastatin use overall, significant benefits in favor of atorvastatin users versus nonstatin users were noted among males (30.4% vs. 45.5%), those with higher cumulative cisplatin doses (>200 mg/m2) (31.7% vs. 61%), those with a mild hearing loss at baseline (26.8% vs. 41.1%), and those who underwent CRT (31.2% vs. 47.8%).
Figure 3. Atorvastatin use significantly reduces the odds of a clinically meaningful cisplatin-induced hearing loss.
An analysis of the incidence of a CTCAE-defined hearing loss due to cisplatin therapy in the full cohort and key subgroups is shown. For the full cohort and the subject subgroups, the difference in the incidence (% of ears) and 95% CI were estimated using a nonlinear mixed-effect analysis, fitting the Poisson model. Significant differences (red diamonds) in the calculated incidence of a CTCAE grade 1 or higher hearing loss were observed for the full cohort as well as for the male subgroup and for those receiving higher (>200 mg/m2) cumulative cisplatin dose, those receiving radiation, and those with mild hearing loss at baseline. CNT, could not test because of insufficient sample size in atorvastatin + cisplatin therapy comparison group.
In addition to the MEM analysis of high-frequency PTA (a continuous variable), we also used logistic regression analysis of the incidence of a CTCAE-defined hearing loss (a binary variable). The logistic regression allowed us to calculate adjusted odds ratio (OR) for the 3 variables identified in our MEM analysis (Supplemental Table 2) that were significantly associated with cisplatin-induced hearing loss: statin use, cumulative cisplatin dose, and baseline hearing status. The results indicated that for every 100 mg/m2 increase in cisplatin dose, an individual was 2.2 times more likely to develop hearing loss (OR = 2.20; 95% CI, 1.63–3.01) (Supplemental Table 4). Additionally, with every 20 dB increase in PTA threshold at baseline, a person was 40% (OR = 0.60; 95% CI, 0.44–0.83) less likely to acquire a cisplatin-induced hearing loss. Finally, an individual taking atorvastatin was 53% less likely (OR = 0.47; 95% CI, 0.28–0.77) to acquire a cisplatin-induced hearing loss compared with a nonstatin user after controlling for cumulative cisplatin dose and baseline hearing status.
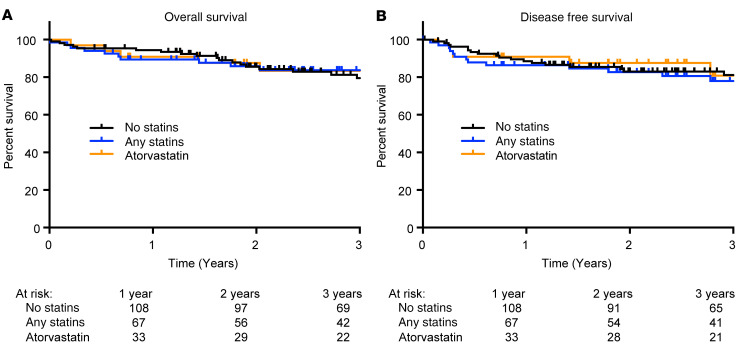
Three-year overall survival and disease-free survival do not differ between atorvastatin users and those not taking a statin.
To determine whether statin drugs may affect treatment outcomes in patients with HNSCC, we examined overall survival and disease-free survival in the available data from URMC (n = 175), which was our largest cohort and also the cohort with the longest follow-up data. Overall survival at 3 years was approximately 80% (Figure 4). An exact median survival time could not be calculated because of the number of patients censored/lost to follow-up. Importantly, however, there were no significant differences among nonstatin users, statin users, and atorvastatin users in overall (P = 0.97) or disease-free survival (P = 0.94).
Figure 4. Three-year overall survival and disease-free survival are not different among statin users, atorvastatin users, and those not taking a statin.
Kaplan-Meier estimates of overall (A) and disease-free (B) survival are shown. A log-rank (Mantel-Cox) test indicated no significant differences in either overall or disease-free survival among groups (P > 0.05). No statin group, n = 107; any statin group, n = 68; atorvastatin group, n = 33.
Discussion
We examined the relationship between statin use and cisplatin-induced hearing loss in patients with head and neck cancer. Significant hearing loss occurred in 48% of subjects, consistent with previous reports (36). The incidence of cisplatin-induced hearing loss was significantly reduced in patients taking a statin medication. Specifically, the incidence of a CTCAE grade 1 or higher hearing loss was reduced by 17.6% in atorvastatin users relative to nonstatin users. Moreover, the incidence of a CTCAE grade 2 or higher, a moderate severity adverse event that may be dose limiting, was reduced by 19.7% in atorvastatin users relative to nonstatin users. Our data suggest that concurrent use of atorvastatin during cisplatin-based chemotherapy may offer an opportunity for reduced hearing loss in these patients without reduced survival.
Large databases of health outcomes (e.g., UnitedHealthcare, Specialized Program of Research Excellence, SEER-Medicare, Kaiser Permanente Research Bank, Optum) rarely (or never) include audiometric data, and most adults with cancer do not receive a baseline hearing test prior to onset of cisplatin therapy (37). Therefore, we utilized retrospective data from 2 sites with ongoing ototoxicity monitoring programs, and we initiated a prospective study designed to provide additional subjects for this data set. Our combined retrospective and prospective data set consisted of 277 subjects with head and neck cancer, 40% of whom were taking a statin drug at the onset of cisplatin-based CRT. Significant reductions in cisplatin-induced threshold shifts were observed in the high-frequency region (≥4 kHz) among statin users, particularly for those on atorvastatin. Similarly, the incidence of a CTCAE-defined hearing loss was significantly reduced by 10% (from 48.8% to 38.4%) for those in the any statin user group and by 18% (from 48.8% to 31.2%) in the atorvastatin user group. Similar results were observed using TUNE criteria. These findings were most prominent among males receiving high cumulative doses of cisplatin (>200 mg/m2) combined with radiation therapy. This observation may be reflective of the study cohort, because head and neck cancer is more common in men than in women and is often treated with these higher cumulative cisplatin doses. Further investigation is necessary in order to fully explore the potential benefit of atorvastatin in female patients, other cancer types, and other cisplatin regimens.
The incidence of hearing loss in our study was significantly predicted by 3 variables: cumulative cisplatin dose, baseline hearing status, and statin use. Accounting for the greatest amount of variance was cumulative cisplatin dose. The median cumulative cisplatin dose in our cohort was 200 mg/m2 (IQR, 140–280). Cumulative cisplatin doses higher than 210 mg/m2 (38, 39) have been previously associated with increased risk for hearing loss (40). Individuals with normal hearing (PTA ≤20 dB HL) at baseline were more likely to experience cisplatin-induced changes in hearing than individuals with hearing loss (PTA >20 dB HL), consistent with previous reports (41). Because cisplatin ototoxicity is first observed at higher frequencies, which are also the first frequencies affected by noise-induced and age-related hearing loss, it seems plausible that individuals with normal function of the cochlear regions that detect these higher frequencies have more to lose in terms of threshold shifts during cisplatin therapy. The nonstatin users in our cohort entered the study with slightly better hearing sensitivity than the atorvastatin users: 54% of nonstatin users, compared with 38% of atorvastatin users, had clinically normal hearing (PTA of 1, 2, and 4 kHz ≤20 dB HL). However, the majority of nonstatin users (88.8%) and atorvastatin users (84%) had either normal hearing or mild hearing loss (PTA of 1, 2, and 4 kHz >20 and <40 dB HL) at baseline (Table 2). Threshold shifts across all users ranged from 0 to 85 dB, and importantly, 95% of threshold shifts were less than or equal to 50 dB (Figure 1B), indicating that the differences we observed between statin users and nonstatin users was not due to a floor effect in calculated threshold shifts.
The third variable that significantly influenced cisplatin-induced hearing loss in our study was the use of atorvastatin. The incidence of hearing loss, per CTCAE criteria, was 31% in atorvastatin users compared with 49% in those not taking a statin. OR estimates indicated that, controlling for overall cumulative cisplatin dose and the presence of a preexisting hearing loss, an individual taking atorvastatin concurrently with cisplatin therapy was 53% less likely to acquire a CTCAE-defined cisplatin-induced hearing loss compared with a nonstatin user. Similar results were obtained using the TUNE ototoxicity criteria. Both CTCAE and TUNE establish criteria for a clinically meaningful hearing loss that would be expected to affect daily communication and quality of life (8, 34). In addition to an overall loss in hearing sensitivity, a loss of hearing at frequencies above 4 kHz diminishes the ability to recognize and appreciate sounds in nature and music (35, 42). Hearing loss at or below approximately 4 kHz may compromise speech intelligibility in noisy environments. These grading scales help to identify changes in hearing relative to speech communication and define the severity of hearing loss. Adverse events that meet or exceed grade 2 can be dose limiting (34). In the current study, the incidence of a grade 2 or higher CTCAE hearing loss was significantly reduced by 19.7% in atorvastatin users relative to nonstatin users.
Previous studies have indicated that radiation to the cochlea is independently ototoxic (43, 44). We evaluated the effects of radiation on hearing loss in our prospective cohort. We did not observe a correlation between cochlear radiation dose and average high-frequency (6 to 12.5 kHz) threshold shifts (see Supplemental Methods and Supplemental Figure 2). These data are consistent with prior studies suggesting that hearing loss as a result of radiation alone is uncommon when radiation doses to the cochlea are below 35 Gy (43,44). With modern intensity-modulated radiotherapy techniques, treatment for tumors of the oropharynx, larynx, hypopharynx, and oral cavity usually results in cochlear radiation doses that are far below this threshold. In our prospective cohort, radiation doses to the cochlea ranged from 0 to 14.4 Gy. Although radiation dose data were not available in our retrospective cohorts, almost all subjects in both our nonstatin (98.2%) and atorvastatin groups (100%) received radiation, and only 5% of subjects had tumors near the cochlea (e.g., nasopharyngeal carcinoma) that might result in higher cochlear radiation doses. Thus, it is unlikely that the differences in cisplatin-induced hearing loss that we observed between atorvastatin users and those not taking a statin were influenced by differences in radiation to the cochlea.
In our study, reduced hearing loss in atorvastatin users was independent of the dose of atorvastatin they were taking (10–80 mg; R2 = 0.0246). According to the American College of Cardiology and American Heart Association statin dose guidelines, relative to simvastatin and pravastatin, atorvastatin has a higher dose-potency ratio (45–47); thus, a lower dose of atorvastatin may be as effective at reducing hyperlipidemia as a higher dose of another statin drug. It is not clear from our data whether there is an effect of the duration of atorvastatin use. Our study accounted for atorvastatin use only at the onset of cisplatin therapy, and therefore there were likely large differences in the duration of atorvastatin use among our study subjects.
With any potential drug intended to reduce the toxicities of anticancer therapy, there is a concern about introducing a negative impact on survival and other cancer-related outcomes. In our study, survival analyses of the largest retrospective cohort suggest that statin drugs, and atorvastatin in particular, did not have a significant effect on 3-year overall survival or disease-free survival. There are other preclinical and clinical studies suggesting that statins do not reduce the therapeutic efficacy of cisplatin, and several epidemiological studies have reported improved survival among statin users with cancer (48–53). Two recent, large retrospective studies using the SEER Medicare Database and the Ontario Cancer Registry showed that head and neck cancer patients who were taking statin drugs at the time of diagnosis had improved overall and disease-specific survival (54, 55). Our study was likely not powered to detect subtle survival differences in a population with a high proportion of oropharyngeal cancers with favorable prognosis. Further, our survival curves included a high proportion of censored data points due to patients lost to follow-up. Additionally, we were unable to control for compliance with oral statin medications. In practice, drug compliance is variable, especially for drugs like statins that do not have perceptible effects. It is possible that the beneficial effects of statins on cisplatin ototoxicity are greater than we observed, assuming that some statin users in our cohort skipped doses of statin medications during their cisplatin therapy. Taken together, our data suggest that adding atorvastatin to cisplatin chemoradiation did not reduce the therapeutic efficacy of cisplatin in patients with head and neck cancer.
Limitations of our study include biases inherent to retrospective studies. The statin users and nonstatin users differed slightly in their ages and anatomic tumor sites: statin users tended to be older, less likely to have normal hearing at baseline, and more likely to have oropharyngeal cancer. These factors may have contributed slightly to hearing and survival outcomes. Our study was underpowered to examine any statin other than atorvastatin; therefore, it is unclear whether users of other statin drugs would also show reduced cisplatin-induced hearing loss. Another limitation of our study is that the data do not address the role (if any) of duration of statin use. Finally, our retrospective cohort of subjects with head and neck cancer did not have sufficient representation of women to address whether atorvastatin use is associated with reduced cisplatin-induced hearing loss in women.
Our data indicate that cisplatin therapy resulted in clinically meaningful (using TUNE criteria) hearing loss in up to 53% of individuals with head and neck cancer. We observed reduced incidence and severity of cisplatin-induced hearing loss in subjects taking atorvastatin relative to those not taking a statin drug. A randomized, placebo-controlled interventional study is currently being developed to determine the extent to which atorvastatin reduces cisplatin-induced hearing loss in patients with head and neck cancer. Subjects with newly diagnosed head and neck cancer who are scheduled to receive cisplatin-based CRT and are not already taking a statin will be randomized to receive either atorvastatin (20 mg) or a placebo daily for the duration of CRT. Baseline hearing sensitivity will be measured prior to the onset of cisplatin therapy and again after completion of all cycles of cisplatin therapy. The primary endpoint is the change in hearing sensitivity between pretreatment and posttreatment audiograms defined using CTCAE ototoxicity scale criteria. In addition, studies in animal models are needed in order to examine the cellular and molecular mechanisms by which statins may reduce cisplatin-induced hearing loss. Our data suggest that atorvastatin, an inexpensive drug with a good safety profile, holds promise to reduce cisplatin-induced hearing loss in adult patients without reducing the therapeutic efficacy of cisplatin.
Methods
For additional details, see the Supplemental Methods.
Overview.
This study consisted of combined retrospective and prospective observational data from 3 clinical sites (Figure 1). The subjects were adults, 18 years or older, who were newly diagnosed with HNSCC and scheduled for treatment with cisplatin. Electronic medical record systems were reviewed at each site for subjects meeting full eligibility criteria (Supplemental Table 1). Characteristics of the subjects (age, sex), details of cancer diagnosis and treatment schedule, and history of statin medication use are shown in Table 1.
Retrospective clinical data were examined from ototoxicity monitoring programs at the University of Rochester Medical Center (URMC; n = 215) and the Walter Reed National Military Medical Center (WRNMMC; n = 34). A table describing the type of data contributed by each site is available in the supplemental materials (Supplemental Table 2). Prospective data were collected as an observational study conducted at the NIH (n = 28) in partnership with the Johns Hopkins University (JHU) Department of Otolaryngology-Head and Neck Surgery and Department of Radiation Oncology and Molecular Sciences.
Data analyses.
Based on an initial subset of retrospective data from URMC (n = 55) and WRNMMC (n = 20) showing a 2:1 ratio of nonstatin to statin users, we performed a sample size estimate using nQuery (Statsols Solutions Ltd). A sample size of 267 subjects was determined to be necessary to detect the observed 17.3% difference in the incidence of hearing loss as defined by the NCI CTCAE (34) between statin users and nonstatin users, with an α of 0.05 and 80% power. These initial 75 subjects were included in the final analysis totaling 277 subjects.
The primary outcome measure was the difference in incidence of a change in hearing between the baseline hearing test and the posttreatment hearing test, per ear, as defined by established ototoxicity grading scales. These scales report subjects who transition from normal hearing to hearing loss as well as those who transition from some hearing loss to more hearing loss. We applied the criteria of 2 different grading scales (Supplemental Table 3) to our data set. The NCI CTCAE v5.0 (34) classifies adverse changes in hearing based on auditory threshold shifts across a 1–8 kHz frequency range. We also applied TUNE ototoxicity grading criteria (35), which incorporate extended high-frequency (EHF) data (see Supplemental Table 4 and Supplemental Figure 1).
The secondary outcome measure was the change in hearing thresholds, per ear, between the baseline hearing test and the posttreatment hearing test across standard audiometric and EHFs ranging from 0.25 to 12.5 kHz. All baseline audiograms were obtained less than or 90 days prior to start of cisplatin treatment, and posttreatment audiograms were obtained less than or 90 days after the end of cisplatin treatment. Threshold shifts were calculated as the difference in threshold (dB HL) between baseline and posttreatment audiograms at each frequency.
Statistics.
Subjects were initially assigned to either the nonstatin user group or the statin user group based on their use of any statin medication at the start of cisplatin treatment. Based on the prevalence of each statin type within the statin user group (Table 2), we also examined atorvastatin and simvastatin in isolation. Both ears were used in the data analyses because of possible influences of asymmetric hearing losses either at baseline (observed in 12% of all subjects, defined as a ≥15 dB difference in the PTA of 0.5, 1, 2, and 4 kHz) and/or a result of differential radiation doses to the 2 cochleas because high doses of radiation (≥45 Gy) have been reported to be ototoxic (43). Including both ears from each subject introduces correlation among observations that can incorrectly reduce the standard error of certain estimates. We corrected for this bias by including subject-specific random intercepts in the statistical model (56). This method allowed us to make use of all of the data from each ear while accounting for the fact that the 2 ears of each individual will be correlated.
A 2-way ANOVA using Dunnett’s post hoc multiple-comparison test (GraphPad Prism 8) was conducted to compare the threshold shifts as a function of frequency (0.25–12.5 kHz) between nonstatin users and subjects taking any statin, atorvastatin, or simvastatin. However, although the comparison between atorvastatin and nonstatin users remained sufficiently powered (>0.8), our study was underpowered for the comparison of simvastatin users versus nonstatin users.
Our primary outcome measure was based on changes in hearing as defined by CTCAE v5.0 scale criteria (Supplemental Table 3) and were analyzed using categorical incidence (per ear) data. The incidence and severity distribution of a clinically meaningful hearing change, per ear, relative to statin use was analyzed using χ2 analyses (SAS PROC FREQ procedure). The rate difference, with a 95% CI, of a CTCAE-defined hearing loss between atorvastatin and nonstatin users was estimated by fitting the Poisson model using PROC NLMIXEDA for the total population as well as for subgroups (sex, cumulative cisplatin dose, individual cisplatin dose, baseline hearing status, and radiation). A logistic regression analysis (SAS PROC LOGISTIC procedure) with calculation of ORs and 95% CIs was performed to identify associations between CTCAE-defined changes in hearing and statin use after adjustment for significant covariates.
Our secondary outcome measure utilized high-frequency audiometric threshold data. A mixed-effect model analysis (SAS PROC GLIMMIX procedure) was applied to average high-frequency threshold shift data (PTA of 6–12.5 kHz) to determine the influence of other model effects on cisplatin-induced threshold shift within this high-frequency region. Fixed effects included statin use, sex, age, cumulative cisplatin dose, radiation exposure, and baseline hearing. Subject ID was defined as a random effect to account for the inclusion of 2 ears in the analysis. Statin use, sex, and radiation exposure were included as dichotomous variables, whereas age, cumulative dose, and baseline hearing based on the PTA of 1, 2, and 4 kHz were treated as continuous variables. A Pearson R correlation analysis was used to assess the association of atorvastatin drug dose and high-frequency threshold shift within Prism 8 (GraphPad Software).
Overall survival and disease-free survival were calculated as Kaplan-Meier curves using GraphPad Prism 8 software on all available data from URMC at up to 3 years after treatment (N = 175). Survival curves were compared using the log-rank (Mantel-Cox) test. Cochlear radiation dose data presented in the supplemental materials (Supplemental Figure 2) were analyzed using Pearson R and Spearman R correlation analysis within GraphPad Prism 8.
All statistical analyses were performed in SAS version 9.4 (SAS Institute Inc.) or GraphPad Prism 8. P values of less than 0.05 were considered significant
Study approval.
All retrospective study activities were approved by either the University of Rochester Research Subject Review Board (RSRB00060424) or the Defense Health Agency Human Research Protections Program (DSA 876612). The prospective study was approved by the IRBs at NIH (IRB 17-DC-0138) and JHU and registered with ClinicalTrials.gov (ID NCT03225157). Written informed consent was obtained from each subject prior to enrollment.
Author contributions
KAF, CB, NCS, and LLC designed the study. BP, JG, DM, CO, and SN provided either patient management and referral and/or patient care. Data collection was carried out by KAF, PA, MC, TT, MM, AC, CO, and SN. Statistical analyses were conducted by KAF, CML, HC, and NC, and figures were generated by KAF and NCS. KAF, JRD, NCS, and LLC interpreted the data. The manuscript was written, reviewed, and edited by KAF, PA, TT, JRD, SN, NCS, and LLC. KAF, NCS, and LLC are the guarantors of this work, and as such, had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis.
Supplementary Material
Acknowledgments
The authors would like to thank Thomas Friedman, Jeff Kim, and Bob Shamburek for their helpful comments on the manuscript and Garnett McMillan for his assistance with statistical modeling. This research was funded by the Division of Intramural Research at the National Institute on Deafness and Other Communication Disorders (project numbers 1 ZIA DC000079 and ZIA DC000090). The project described in this publication was supported in part by the University of Rochester CTSA award number UL1 TR002001 from the National Center for Advancing Translational Sciences of the NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the official policy of the Department of Army/Navy/Air Force, Department of Defense, or US government.
Version 1. 01/04/2021
Print issue publication
Footnotes
Conflict of interest: LLC, NCS, and KAF hold a provisional patent for the use of statins to prevent drug-induced hearing loss (“Use of Statins to Treat or Prevent Drug Induced Hearing Loss,” patent 62/966,794).
Role of funding source: The funding source had no role in the design of this study, its execution, analyses, interpretation of the data, or decision to submit the results.
Copyright: © 2021, Fernandez et al. This is an open access article published under the terms of the Creative Commons Attribution 4.0 International License.
Reference information: J Clin Invest. 2021;131(1):e142616.https://doi.org/10.1172/JCI142616.
Contributor Information
Maura Campbell, Email: maura_campbell@URMC.rochester.edu.
Thomas Townes, Email: thomas.g.townes.mil@mail.mil.
Chuan-Ming Li, Email: chuan-ming.li@nih.gov.
Hui Cheng, Email: hui.cheng@nih.gov.
Jaylon Garrett, Email: jharkne4@jhmi.edu.
Marcia Mulquin, Email: mmulquin@mail.nih.gov.
Anna Clements, Email: anna.clements@nih.gov.
Deborah Mulford, Email: Deborah_Mulford@URMC.rochester.edu.
Carmen Brewer, Email: brewerc@nidcd.nih.gov.
Judy R. Dubno, Email: dubnojr@musc.edu.
Nicole C. Schmitt, Email: nicole.cherie.schmitt@emory.edu.
References
- 1.Miller KD, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–385. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 2.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the ‘silver tsunami’: prevalence trajectories and co-morbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark. 2016;25(7):1029–1036. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertolini P, et al. Platinum compound-related ototoxicity in children: long-term follow-up reveals continuous worsening of hearing loss. J Pediatr Hematol Oncol. 2004;26(10):649–655. doi: 10.1097/01.mph.0000141348.62532.73. [DOI] [PubMed] [Google Scholar]
- 4.Coradini PP, Cigana L, Selistre SG, Rosito LS, Brunetto AL. Ototoxicity from cisplatin therapy in childhood cancer. J Pediatr Hematol Oncol. 2007;29(6):355–360. doi: 10.1097/MPH.0b013e318059c220. [DOI] [PubMed] [Google Scholar]
- 5.Frisina RD, et al. Comprehensive audiometric analysis of hearing impairment and tinnitus after cisplatin-based chemotherapy in survivors of adult-onset cancer. J Clin Oncol. 2016;34(23):2712–2720. doi: 10.1200/JCO.2016.66.8822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knight KR, et al. Group-wide, prospective study of ototoxicity assessment in children receiving cisplatin chemotherapy (ACCL05C1): a report from the Children’s Oncology Group. J Clin Oncol. 2017;35(4):440–445. doi: 10.1200/JCO.2016.69.2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marnitz S, et al. Age-corrected hearing loss after chemoradiation in cervical cancer patients. Strahlenther Onkol. 2018;194(11):1039–1048. doi: 10.1007/s00066-018-1347-6. [DOI] [PubMed] [Google Scholar]
- 8.Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging. 2012;7:159–163. doi: 10.2147/CIA.S26059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao JK. Clinical implications for statin pleiotropy. Curr Opin Lipidol. 2005;16(6):624–629. doi: 10.1097/01.mol.0000191913.16321.60. [DOI] [PubMed] [Google Scholar]
- 10.Ma YX, Li WH, Xie Q. Rosuvastatin inhibits TGF-beta1 expression and alleviates myocardial fibrosis in diabetic rats. Pharmazie. 2013;68(5):355–358. [PubMed] [Google Scholar]
- 11.Barbosa CP, Bracht L, Ames FQ, de Souza Silva-Comar FM, Tronco RP, Bersani-Amado CA. Effects of ezetimibe, simvastatin, and their combination on inflammatory parameters in a rat model of adjuvant-induced arthritis. Inflammation. 2017;40(2):717–724. doi: 10.1007/s10753-016-0497-x. [DOI] [PubMed] [Google Scholar]
- 12.Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005;4(12):977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigues G, et al. Simvastatin reduces hepatic oxidative stress and endoplasmic reticulum stress in nonalcoholic steatohepatitis experimental model. Oxid Med Cell Longev. 2019;2019:3201873. doi: 10.1155/2019/3201873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Wang Y-T, Koka S, Zhang Y, Hussain T, Li X. Simvastatin improves lysosome function via enhancing lysosome biogenesis in endothelial cells. Front Biosci (Landmark Ed) 2020;25:283–298. doi: 10.2741/4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aznaouridis K, Masoura C, Vlachopoulos C, Tousoulis D. Statins in stroke. Curr Med Chem. 2019;26(33):6174–6185. doi: 10.2174/0929867326666190620104539. [DOI] [PubMed] [Google Scholar]
- 16.Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo controlled trial. Lancet. 2002;360(9326):7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 17.Cucchiara B, Kasner SE. Use of statins in CNS disorders. J Neurol Sci. 2001;187(1-2):81–89. doi: 10.1016/S0022-510X(01)00529-9. [DOI] [PubMed] [Google Scholar]
- 18.Saeedi Saravi SS, Saeedi Saravi SS, Arefidoust A, Dehpour AR. The beneficial effects of HMG-CoA reductase inhibitors in the processes of neurodegeneration. Metab Brain Dis. 2017;32(4):949–965. doi: 10.1007/s11011-017-0021-5. [DOI] [PubMed] [Google Scholar]
- 19.Sparks DL, et al. Atorvastatin for the treatment of mild to moderate Alzheimer disease: preliminary results. Arch Neurol. 2005;62(5):753–757. doi: 10.1001/archneur.62.5.753. [DOI] [PubMed] [Google Scholar]
- 20. Lipitor (atorvastatin calcium). Package label. Pfizer; 2009. [Google Scholar]
- 21.Jahani L, Mehrparvar AH, Esmailidehaj M, Rezvani ME, Moghbelolhossein B, Razmjooei Z. The effect of atorvastatin on preventing noise-induced hearing loss: an experimental study. Int J Occup Environ Med. 2016;7(1):15–21. doi: 10.15171/ijoem.2016.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JS, Kim SW, Park K, Choung YH, Jou I, Park SM. Pravastatin attenuates noise-induced cochlear injury in mice. Neuroscience. 2012;208:123–132. doi: 10.1016/j.neuroscience.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Richter CP, et al. Fluvastatin protects cochleae from damage by high-level noise. Sci Rep. 2018;8(1):3033. doi: 10.1038/s41598-018-21336-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitlon DS, Grover M, Dunne SF, Richter S, Luan CH, Richter CP. Novel high content screen detects compounds that promote neurite regeneration from cochlear spiral ganglion neurons. Sci Rep. 2015;5:15960. doi: 10.1038/srep15960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Syka J, Ouda L, Nachtigal P, Solichová D, Semecký V. Atorvastatin slows down the deterioration of inner ear function with age in mice. Neurosci Lett. 2007;411(2):112–116. doi: 10.1016/j.neulet.2006.10.032. [DOI] [PubMed] [Google Scholar]
- 26.Brand Y, et al. Simvastatin protects auditory hair cells from gentamicin-induced toxicity and activates Akt signaling in vitro. BMC Neurosci. 2011;12:114. doi: 10.1186/1471-2202-12-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gopinath B, Flood VM, Teber E, McMahon CM, Mitchell P. Dietary intake of cholesterol is positively associated and use of cholesterol-lowering medication is negatively associated with prevalent age-related hearing loss. J Nutr. 2011;141(7):1355–1361. doi: 10.3945/jn.111.138610. [DOI] [PubMed] [Google Scholar]
- 28.Olzowy B, Canis M, Hempel JM, Mazurek B, Suckfüll M. Effect of atorvastatin on progression of sensorineural hearing loss and tinnitus in the elderly: results of a prospective, randomized, double-blind clinical trial. Otol Neurotol. 2007;28(4):455–458. doi: 10.1097/01.mao.0000271673.33683.7b. [DOI] [PubMed] [Google Scholar]
- 29.Sutbas A, Yetiser S, Satar B, Akcam T, Karahatay S, Saglam K. Low-cholesterol diet and antilipid therapy in managing tinnitus and hearing loss in patients with noise-induced hearing loss and hyperlipidemia. Int Tinnitus J. 2007;13(2):143–149. [PubMed] [Google Scholar]
- 30.Hameed MK, Sheikh ZA, Ahmed A, Najam A. Atorvastatin in the management of tinnitus with hyperlipidemias. J Coll Physicians Surg Pak. 2014;24(12):927–930. [PubMed] [Google Scholar]
- 31.Fernandez K, et al. Lovastatin protects against cisplatin-induced hearing loss in mice. Hear Res. 2020;389:107905. doi: 10.1016/j.heares.2020.107905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandez K, Wafa T, Fitzgerald TS, Cunningham LL. An optimized, clinically relevant mouse model of cisplatin-induced ototoxicity. Hear Res. 2019;375:66–74. doi: 10.1016/j.heares.2019.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prayuenyong P, Kasbekar AV, Baguley DM. The efficacy of statins as otoprotective agents: a systematic review. Clin Otolaryngol. 2020;45(1):21–31. doi: 10.1111/coa.13457. [DOI] [PubMed] [Google Scholar]
- 34. National Cancer Institute DCTD Division of Cancer Treatment & Diagnosis. CTEP Cancer Therapy Evaluation. Common Terminology Criteria for Adverse Events (CTCAE) — Protocol Development. 2017. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50 Cited December 29, 2019. Accessed October 14, 2020.
- 35.Theunissen EAR, et al. A new grading system for ototoxicity in adults. Ann Otol Rhinol Laryngol. 2014;123(10):711–8. doi: 10.1177/0003489414534010. [DOI] [PubMed] [Google Scholar]
- 36.Zuur CL, et al. Risk factors of ototoxicity after cisplatin-based chemo-irradiation in patients with locally advanced head-and-neck cancer: a multivariate analysis. Int J Radiat Oncol Biol Phys. 2007;68(5):1320–1325. doi: 10.1016/j.ijrobp.2007.01.042. [DOI] [PubMed] [Google Scholar]
- 37.Konrad-Martin D, et al. Applying U.S. national guidelines for ototoxicity monitoring in adult patients: perspectives on patient populations, service gaps, barriers and solutions. Int J Audiol. 2018;57(sup4):S3–S18. doi: 10.1080/14992027.2017.1398421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schell MJ, et al. Hearing loss in children and young adults receiving cisplatin with or without prior cranial irradiation. J Clin Oncol. 1989;7(6):754–760. doi: 10.1200/JCO.1989.7.6.754. [DOI] [PubMed] [Google Scholar]
- 39.Scobioala S, et al. Impact of radiation technique, radiation fraction dose, and total cisplatin dose on hearing. Strahlenther Onkol. 2017;193(11):910–920. doi: 10.1007/s00066-017-1205-y. [DOI] [PubMed] [Google Scholar]
- 40.Rademaker-Lakhai JM, et al. Relationship between cisplatin administration and the development of ototoxicity. J Clin Oncol. 2006;24(6):918–924. doi: 10.1200/JCO.2006.10.077. [DOI] [PubMed] [Google Scholar]
- 41.Fleming S, et al. Ototoxicity from cis-platinum in patients with stages III and IV previously untreated squamous cell cancer of the head and neck. Am J Clin Oncol. 1985;8(4):302–306. doi: 10.1097/00000421-198508000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Prestes R, Daniela G. Impact of tinnitus on quality of life, loudness and pitch match, and high-frequency audiometry. Int Tinnitus J. 2009;15(2):134–138. [PubMed] [Google Scholar]
- 43.Bhandare N, et al. Radiation therapy and hearing loss. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S50–S57. doi: 10.1016/j.ijrobp.2009.04.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Theunissen EA, et al. Sensorineural hearing loss in patients with head and neck cancer after chemoradiotherapy and radiotherapy: a systematic review of the literature. Head Neck. 2015;37(2):281–292. doi: 10.1002/hed.23551. [DOI] [PubMed] [Google Scholar]
- 45.Adams SP, Tsang M, Wright JM. Atorvastatin for lowering lipids. Cochrane Database Syst Rev. 2015;(3):CD008226. doi: 10.1002/hed.23551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study) Am J Cardiol. 1998;81(5):582–587. doi: 10.1016/S0002-9149(97)00965-X. [DOI] [PubMed] [Google Scholar]
- 47.Stone NJ, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 48.Beckwitt CH, Brufsky A, Oltvai ZN, Wells A. Statin drugs to reduce breast cancer recurrence and mortality. Breast Cancer Res. 2018;20(1):144. doi: 10.1186/s13058-018-1066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jian-Yu E null, Graber JM, Lu SE, Lin Y, Lu-Yao G, Tan XL. Effect of metformin and statin use on survival in pancreatic cancer patients: a systematic literature review and meta-analysis. Curr Med Chem. 2018;25(22):2595–2607. doi: 10.2174/0929867324666170412145232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee H, et al. Statin use and its impact on survival in pancreatic cancer patients. Medicine (Baltimore) 2016;95(19):e3607. doi: 10.1097/MD.0000000000003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seckl MJ, et al. Multicenter, phase III, randomized, double-blind, placebo-controlled trial of pravastatin added to first-line standard chemotherapy in small-cell lung cancer (LUNGSTAR) J Clin Oncol. 2017;35(14):1506–1514. doi: 10.1200/JCO.2016.69.7391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ung MH, MacKenzie TA, Onega TL, Amos CI, Cheng C. Statins associate with improved mortality among patients with certain histological subtypes of lung cancer. Lung Cancer. 2018;126:89–96. doi: 10.1016/j.lungcan.2018.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xie W, et al. Statin use and survival outcomes in endocrine-related gynecologic cancers: a systematic review and meta-analysis. Oncotarget. 2017;8(25):41508–41517. doi: 10.18632/oncotarget.17242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lebo NL, Griffiths R, Hall S, Dimitroulakos J, Johnson-Obaseki S. Effect of statin use on oncologic outcomes in head and neck squamous cell carcinoma. Head Neck. 2018;40(8):1697–1706. doi: 10.1002/hed.25152. [DOI] [PubMed] [Google Scholar]
- 55.Gupta A, et al. Statin use associated with improved overall and cancer specific survival in patients with head and neck cancer. Oral Oncol. 2019;90:54–66. doi: 10.1016/j.oraloncology.2019.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. John Wiley & Sons; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.