Dear Editors of Journal of Infection,
We read with interest of the recent article in your journal about the viral load and infectivity over the course of an SARS-CoV-2 infection,1 which has showed that there is a relatively consistent trajectory of SARS-CoV-2 viral load over the course of COVID-19 from respiratory tract samples, however the duration of infectivity remains uncertain. Therefore, it is of great significance to explore the duration of viral clearance and related factors, which may have important implication for making clinical decisions regarding the isolation precautions and treatment in patients with COVID-19.2 , 3
We did this retrospective study to explore risk factors associated with viral clearance and to develop a risk prediction model to help identify patients who are likely to have prolonged duration viral clearance based on two cohorts of Chinese discharged patients with COVID-19. We collected the epidemiological, clinical symptoms and signs, laboratory findings, treatments and outcomes data from the hospital electric medical records based on two cohorts led by the Sichuan and Wuhan Collaboration Research Group for COVID-19, China. The least absolute shrinkage and selection operator (LASSO) and logistic regression analysis was used to develop the multivariable risk prediction model.
As of March 12, 2020, there were a total of 1179 discharged patients with COVID-19 were screened out from two cohorts. There were no data concerning the duration of viral clearance in 260 patients. Finally, there were 919 patients were included in this study. Based on the median of the duration of viral clearance (17 [11, 27] days), the study population were divided into two groups: the prolonged duration of viral clearance group (PDVC) (n = 474) and the early duration of viral clearance group (EDVC) (n = 445).
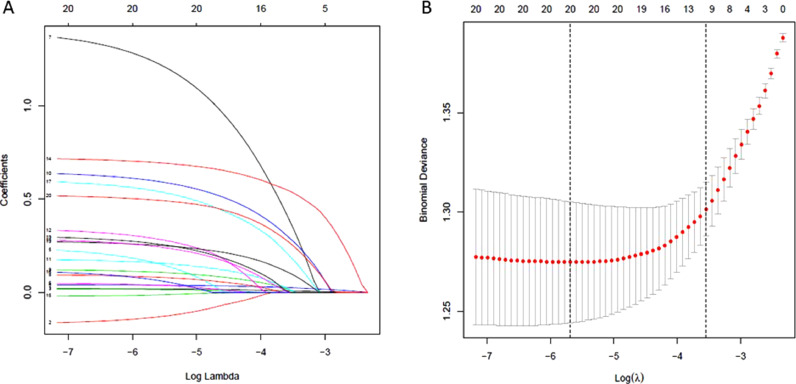
All of potential predictive variables were included in the LASSO regression. After LASSO regression, 10 variables with nonzero coefficients were retained as potential predictor, including age, time from illness onset to admission (TIOA), haemoptysis, chest distress, diarrhea, any complication, use of antibiotics, use of systemic glucocorticoids (GCs), white blood cell (WBC) count and alanine transaminase (ALT) (Fig. 1 A). The coefficient of lambda min was 0.0289 (Fig. 1B).
Fig. 1.
Selection of potential predictors of the mode applying the LASSO regression analysis. (A) LASSO coefficient profiles of the potential included predictors. The coefficient profile plot was produced against the log(lambda) sequence. (B) Befitting λ selection in the LASSO regression analysis based on the 5-fold cross-validation. Partial likelihood deviance (binomial deviance) curve was plotted versus log (λ). Dotted vertical lines were drawn based on the minimum criteria and 1 standard error of the minimum criteria (the 1-SE criteria).
Inclusion of the LASSO-selected 10 variables in a multivariate logistic regression resulted in 7 variables that were independently statistically significant, which were finally identified as the predictor of predictive model. They were age (OR=1.016, 95%CI=[1.008, 1.025], P < 0.001), TIOA (OR=1.040, 95%CI=[1.027, 1.055], P < 0.001), haemoptysis (OR=3.756, 95%CI=[1.443, 11.692], P = 0.011), diarrhea (OR=1.959, 95%CI=[1.742, 3.394], P < 0.001), use of GCs (OR=2.423, 95%CI=[1.742, 3.394], P < 0.001), WBC < 4 × 10⁹/L (OR=1.74, 95%CI=[1.14, 2.67], P = 0.010), ALT > 40 U/L (OR=1.838, 95%CI=[1.340, 2.533], P < 0.001).
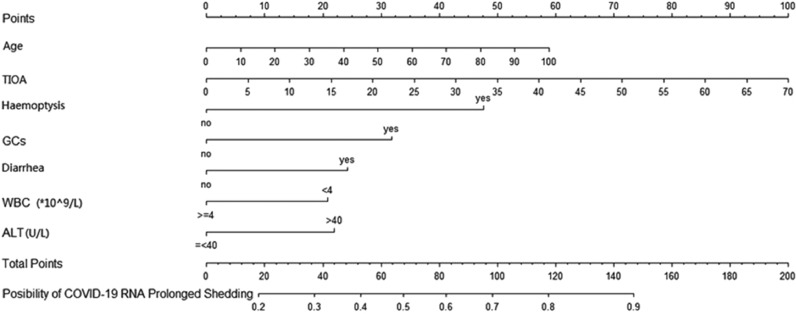
The prolonged SARS-CoV-2 RNA clearance risk predictive model was developed based on the identified independent predictors including age, TIOA, haemoptysis, diarrhea, use of GCs, WBC (< 4 × 10⁹/L), and ALT (> 40 U/L). Based on the results of the multivariate analysis, a nomogram was further constructed (Fig. 2 ). The C-index of the nomogram in the training set was 0.710(95%CI: 0.677–0.743). And area under the curve of ROC analysis was 0.710 for training set, which was confirmed to be 0.702 by 1000 bootstrap validation. The Hosmer-Lemeshow test told the Chi-square of 11.10 and p-value of 0.27, suggesting the good model fit and calibration. The calibration plot by 1000 bootstrap validation also indicate great agreement between the biased-corrected curve and the ideal curve.
Fig. 2.
Nomogram for predicting prolonged SARS-CoV-2 RNA clearance risk. The score of each predictors were added to obtain the total score and a vertical line was drawn on the total score to obtain the corresponding possibility of SARS-CoV-2 RNA prolonged shedding.
Our results found that older age was independently associated with prolonged duration of virus clearance, which was supported by previous study.4 Older age has been proved to be associated with poor clinical outcomes in COVID-19 patients.5 Innate and adaptive immune are largely compromised with aging, resulting in limiting the viral clearance and host inflammatory responses. At the same time, our results demonstrated that delayed hospital admission was associated with prolonged duration of virus clearance, which was also proved by the study of Xu et al.6 Our findings further contributed to address that hospital admission and treatments should be started as soon as possible in patients with COVID-19. Notablely, haemoptysis and diarrhea deserved special attention at admission, which were independently associated with prolonged duration of virus clearance. Haemoptysis was also included in the COVID risk score to predict the development of critical illness among hospitalized COVID-19 infected patients by the study of Liang et al.7 Besides, hemoptysis has been described as an infrequent COVID clinical symptom by several retrospective analysis, which may indicate the venous thrombosis, particularly pulmonary embolism. As to the lab findings, our study found that the peripheral blood white count, especially lymphocyte count was relatively lower in patients with prolonged duration of viral clearance. The SARS-CoV-2 caused lymphocytic depletion in infected patients,3 and the mechanism may be caused by direct attack of coronavirus on lymphocytes or by immune-mediated apoptosis of lymphocytes, which may infect the capacity to clear the virus. In addition, we also found that ALT was increased in the prolonged duration of viral clearance group, indicated hepatic dysfunction was associated with prolonged duration of viral clearance. The recent systematic review and meta-analysis has also indicated that patients with COVID-19 have a higher than expected prevalence of liver injury, and the extent of the injury is associated with the severity of the disease.8 However, the underlying mechanism and its association with viral clearance require more studies to elucidate
Glucocorticoids have been widely used in conjunction with other drugs to treat patients infected with SARS-CoV-2. However, current interim guidance from WHO on clinical management opinions for the COVID-19 advises against the use of corticosteroids unless indicated for another reason9 as the use of glucocorticoids may delay the clearance of viral nucleic acids in patients with MERS and SARS.10 Our study further demonstrated that the usage of systemic GCs was independently associated with a delay in viral clearance in discharged COVID-19 patients, most of which were mild or general patients. Therefore, glucocorticoid treatment is not recommended for patients with COVID-19, especially for mild disease.
In conclusion, prolonged duration of viral clearance was independently associated with older age, prolonged time from illness onset to admission, haemoptysis, diarrhea, use of glucocorticoids, leukopenia and elevated alanine transaminase. Estimating these risk factors could help identify patients who are or are not likely to develop prolonged duration of viral clearance, which could promote individual precision therapy and optimizing the use of medical resources.
Declaration of Competing Interest
All of the authors have no conflict of interest.
Funding source
This study was supported by the National Natural Science Foundation of China (Nos. 81670023, 81870027 and 81920108002), Science and Technology Foundation of Sichuan Province (No. 2018SZ0167), Sichuan Provincial Program for Diagnostic and Treatment of Covid-19 (2020YFS002 and 2020YFS005) and Science and Technology Innovation Project of Chengdu City (No. 2020-YF08-00080-GX).
References
- 1.Walsh KA, Jordan K, Clyne B, Rohde D, Drummond L, Byrne P. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Infect. 2020;81(3):357–371. doi: 10.1016/j.jinf.2020.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang L, Gao YH, Lou LL, Zhang GJ. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J. 2020;55 doi: 10.1183/13993003.00398-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan D, Liu XY, Zhu YN, Huang L, Dan BT, Zhang GJ. Factors Associated With Prolonged Viral Shedding and Impact of Lopinavir/Ritonavir Treatment in Hospitalised non-critically ill patients with SARS-CoV-2 infection. Eur Respir J. 2020;56(1) doi: 10.1183/13993003.00799-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zou L, Ruan F, Huang M, Liang LJ, Huang HT, Hong ZS. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu K, Chen Y, Yuan J. Factors Associated With Prolonged Viral RNA Shedding in Patients With COVID-19. Clin Infect Dis. 2020;71(15):799–806. doi: 10.1093/cid/ciaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang W, Liang H, Ou L, Chen B, Chen A, Li C. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern Med. 2020;180(8):1–9. doi: 10.1001/jamainternmed.2020.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong YJ, Tan M, Zheng Q, Li W, Kumar R, Fock KM. A systematic review and meta-analysis of the COVID-19 associated liver injury. Ann Hepatol. 2020 doi: 10.1016/j.aohep.2020.08.064. S1665-2681(20)30161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395:473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arabi YM, Mandourah Y, Al-Hameed F, Sindi AA, Almekhlafi GA, Hussein MA. Corticosteroid therapy for critically ill patients with middle east respiratory syndrome. Am J Respir Crit Care Med. 2018;197:757–767. doi: 10.1164/rccm.201706-1172OC. [DOI] [PubMed] [Google Scholar]