Abstract
Globally, Indigenous populations experience a disproportionately higher burden of disease related to substance use. Effective prevention of harm related to substance use is a key strategy for improving the health and wellbeing of Aboriginal and Torres Strait Islander peoples in Australia. To inform preventative approaches, this review synthesised the evidence of risk and protective factors of substance use and related harms among Aboriginal and Torres Strait Islander peoples. Eight peer-reviewed and two grey literature databases were systematically searched for quantitative or qualitative studies assessing factors associated with substance use and related harms among Aboriginal and Torres Strait Islander peoples, published between 1 January 1990 and 30 April 2018. Study quality was assessed using validated instruments. Risk or odds ratios were extracted or calculated and factors were summarised in an ecological model into individual, relationship, community, societal or culturally-distinct levels. Thirty-eight relevant studies were identified and reviewed. Individual-level risk factors for substance use were identified including low socio-economic status, high psychological distress, poly drug use and being male. Relationship-level factors were peer pressure and partner/family substance use; protective factors were supportive environments and positive role models. Community-level risk factors included availability of substances. Culturally-distinct factors included cultural connection as a protective factor, but cultural obligations around sharing was a risk factor. Societal risk factors included intergenerational trauma caused by government policies. These findings highlight the importance of tailored preventative approaches for Aboriginal and Torres Strait Islander communities that address identified risk factors and promote protective factors across all ecological levels.
Keywords: Aboriginal and Torres Strait Islander people, Indigenous, Alcohol, Drug, Tobacco, Cannabis, Substance use, Risk factors, Protective factors, Prevention
1. Introduction
Worldwide, alcohol, tobacco and illicit substance use and related harms account for 12% of deaths (World Health Organization, 2009) and these substances and mental disorders are the leading causes of years lived with disability (Whiteford et al., 2013). Disadvantaged groups within high-income countries generally experience a disproportionately higher burden of disease related to substance use (Collins, 2016). In Australia, Aboriginal and Torres Strait Islander peoples1, who make up 2.8% of the population, experience significant disadvantage as is evident from their life expectancy of 74 and 69 years compared to 84 and 80 years for non-Aboriginal Australian females and males, respectively (Australian Bureau of Statistics, 2017). Among Aboriginal and Torres Strait Islander peoples, 12% and 8% of the burden of disease is attributed to tobacco and alcohol respectively (Australian Institute for Health and Welfare, 2016), compared to 9% and 5% respectively for non-Indigenous Australians. Together, substance use and mental disorders account for 14% of the gap in health outcomes between Aboriginal and Torres Strait Islander and non-Indigenous Australians (Australian Institute for Health and Welfare, 2016).
An effective substance use prevention system requires knowledge of why people use substances and whether this differs between population groups (United Nations, 2018). For Aboriginal and Torres Strait Islander peoples, like many Indigenous populations across the United States, Canada and Aotearoa/New Zealand, ongoing impacts of colonisation, intergenerational trauma, disempowerment, remote living, inequity and overcrowded housing have been identified as contributors to elevated substance use and related harms (Midford et al., 2002, King et al., 2009). However, a connection to culture and Country appears to protect Aboriginal and Torres Strait Islander peoples against substance use and related harms (Midford et al., 2002).
Individual studies are an important step to identifying the risk and protective factors associated with substance use for Aboriginal and Torres Strait Islander peoples. Synthesising the available evidence on all ecological levels into one model is a critical next step and has the potential to holistically inform approaches to address substance use and related harms experienced by Aboriginal and Torres Strait Islander peoples (Burnette and Figley, 2017, Bronfenbrenner et al., 1998).
This is the first study to develop an ecological model of individual, relationship, community, societal and culturally-distinct factors that influence substance use and related harms among Aboriginal and Torres Strait Islander peoples. It systematically reviewed, synthesised and critically appraised research findings from studies assessing the risk and protective factors associated with substance use and related harms among Aboriginal and Torres Strait Islander peoples. Synthesis of this literature is critical for informing strategies to prevent harm among Aboriginal and Torres Strait Islander peoples, and has the potential to guide frameworks for research among other Indigenous populations.
2. Methods
2.1. Search strategy and selection criteria
This systematic review followed a pre-specified, published review protocol (PROSPERO no.: CRD42017073734) that used the PRISMA guidelines to detail the methods (Snijder et al., 2018). In line with the Consolidated criteria for strengthening reporting of health research involving indigenous peoples (the CONSIDER statement) (Huria et al., 2019) our methodology was informed by Aboriginal and Torres Strait Islander peoples’ worldviews through authorship (AS, JW) and consultation with our research teams’ expert advisory group. We included studies published between 1 January 1990 and 30 April 2018 that examined factors associated with substance use and/or related harms with a sample of at least 50% Aboriginal and Torres Strait Islander peoples, or those that conducted specific sub-analyses for Aboriginal and Torres Strait Islander peoples. Quantitative and qualitative cross-sectional and longitudinal studies were included.
Studies were included if they examined risk and protective factors associated with substance use outcomes across three levels, as defined in a previous systematic review (Stone et al., 2012): 1) use frequency; 2) regular, problem, heavy use or binge; 3) use disorder or abuse or dependence (see Table 1). For risk factors (i.e., increase in levels 1–3) the following definitions were used:
-
•
Use or frequency refers to likelihood of substance use initiation, irregular substance use or frequency of use not further specified;
-
•
Regular, problem, heavy use or binge. Regular use is at least weekly substance use. Problem use is use that contributes to harms, including substance related injuries or hospitalisations. Heavy and binge use relates to large consumption during one occasion of use;
-
•
Use disorder or abuse or dependence covers use and symptoms consistent with probable substance use disorder.
Table 1.
Characteristics of included studies (n = 38).
| First author (year) | Population | Sample size (age) | Substance | Outcome |
Outcomes of interest assessed in the study | ||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | |||||
| Quantitative (n = 26) | |||||||
| ABS, 1995 | Community | 15,700 (13 + ) | Tobacco, alcohol | x | x | Sex, location | |
| ABS, 1996 | Community | (15–24) | Tobacco, alcohol | x | Sex, age, location | ||
| ABS, 2004 | Community | 9,359 (15 + ) | Tobacco, alcohol | x | Sex, education | ||
| ABS, AIHW (2008) | Community | Tobacco, alcohol, illicit substances | x | x | x | Sex, education, psychological, other substance use, location | |
| ABS, 2009 | Community | 13,307 (15 + ) | Tobacco | x | Location | ||
| ABS, 2016 | Community | 6,611 (15 + ) | Tobacco, alcohol, illicit substances, analgesics | x | x | x | Sex, location |
| Brown et al (2016) | New mothers | 337 (15–43) | Tobacco, cannabis | x | x | Age, education, employment, psychological, health, other substance use, children, peer substance use, violence, stressors, peer finance | |
| Clough et al (2004) | Community | 516 (13–36) | Tobacco, alcohol, cannabis, petrol, kava | x | x | Sex, other substance use | |
| Cunningham et al (1997) | Community | 8,783 (15 + ) | Tobacco | x | x | Age, education, employment, housing, other substance use, language, location, cultural, colonization | |
| DiGiacomo et al (2007) | Primary care patients | 37 (18–70) | Tobacco | x | Psychological | ||
| Dingwall et al (2012) | Rehabilitation clinic visitors | 56 | Petrol | x | x | Support, housing, location, availability | |
| Fitts et al (2013) | Drink driving offenders | 7,834 (15 + ) | Alcohol | x | Age, location | ||
| Fitts et al (2017) | Drink driving offenders | 1,583 (14–24) | Alcohol | x | Location | ||
| Gazis et al (2010) | High school students | 274 (12–16) | Tobacco, alcohol, cannabis | x | Peer substance use, cultural | ||
| Hall et al (1993) | Community | 478 (15–80) | Alcohol | x | Sex, age | ||
| Heath et al (2006) | Maternal and child health clinic visitors | 66 (m = 26) | Tobacco | x | Recreation, psychological, other substance use, peer substance use | ||
| Jacups and Rogerson, 2015 | Prisoners | 101 (18–40) | Cannabis | x | x | Education, employment, psychological, health, other substance use, incarceration, support, peer substance use, availability | |
| Lee et al (2009) | Community | 83 (13–30 + ) | Cannabis | x | x | Other substance use | |
| Maddox et al (2015)a | Community | 204 (12–75) | Tobacco | x | x | Education, peer substance use | |
| Maksimovic et al (2013) | Health workers | 85 (21–67) | Tobacco | x | Employment, income, psychological, health, other substance use, support, children, stressors, peer substance use | ||
| Noble et al (2015) | Health clinic visitors | 377 (18 + ) | Tobacco, alcohol, illicit substances | x | Sex, age, employment, violence | ||
| Passey et al (2012) | Pregnant women | 264 | Tobacco | x | x | Education | |
| Passey et al (2014) | Pregnant women | 257 (16 + ) | Tobacco, alcohol, cannabis | x | x | Education, other substance use, location | |
| Smirnov et al (2016) | Community | 566 (17–65) | Stimulants | x | Employment, psychological, incarceration | ||
| Thomas et al (2008) | Community | 9,400 (15 + ) | Tobacco | x | x | Education, employment, income, housing, recreation, psychological, health, other substance use, incarceration, support, violence, location, colonization | |
| Thrift et al (2011) | Community | 211,482 (<20–35 < ) | Tobacco | x | x | Income, location | |
| Qualitative (n = 12) | |||||||
| Bond et al (2012) | Community | 20 (18 + ) | Tobacco | x | x | Psychological, health, resilience, support, stressors, workplace, colonization, policy | |
| Dawson et al (2012) | Health service staff | 34 | Tobacco | x | x | Psychological, health, support, stressors, peer substance use, housing, workplace, cultural, policy | |
| Gamarania et al (1998) | Students | 220 (5–17) | Tobacco | x | Age, health | ||
| Gould et al (2017) | Community, health and maternity services | 20 (17–38) | Tobacco | x | x | Age, income, other substance use, pregnancy, psychological, peer substance use, support | |
| Johnston and Thomas, 2008 | Community | 38 | Tobacco | x | x | Employment, income, psychological, resilience, other, support, peer substance use, housing, cultural, colonization, availability | |
| Johnston et al (2012) | Students | 65 (5–17) | Tobacco | x | x | Other substance use, support, peer substance use, housing, location, marginalization, cultural, policy, availability | |
| Leavy et al (2010) | Students | 92 (12–15) | Tobacco | x | x | Recreation, psychological, peer substance use, cultural | |
| MacLean et al (2017) | Health centre visitors, drug and alcohol workers | 26 (18–49) | Crystal methamphetamine | x | Recreation, other substance use, stressors, support, peer substance use, cultural, intergenerational trauma, availability | ||
| Maddox et al (2015)a | Community | 50 (12–60) | Tobacco | x | x | Cultural, availability | |
| Passey et al (2011) | Aboriginal health workers, community | 36 (<25 < ) | Tobacco | x | x | Education, employment, recreation, age, psychological, support, peer substance use, housing, cultural, colonization, availability | |
| Senior et al (2006) | Community | (13–39) | Petrol | x | x | Recreation, psychological, peer substance use, housing, availability | |
| Tsourtos et al (2015) | Community health centre visitors | 31 (19–78) | Tobacco | x | x | Education, psychological, health, resilience, support, peer substance use, cultural | |
| Wood et al (2008) | Pregnant women, Aboriginal health workers | 50 (14–50) | Tobacco | x | x | x | Employment, psychological, health, pregnancy, support, peer substance use, cultural |
Outcome 1: use or frequency; outcome 2: regular, problem, heavy use or binge; outcome 3: use disorder or abuse or dependence. aMaddox et al., 2015 reported both quantitative and qualitative data.
For protective factors (i.e., decrease in levels 1–3) the following definitions were used:
-
•
Use or frequency refers to a delay in initiation, abstinence or a reduction in frequency of use not further specified;
-
•
Regular, problem, heavy use or binge refers to cessation or reduction of use following a period of regular, heavy or problem substance use and a reduction in substance-related harms;
-
•
Use disorder or abuse or dependence refers to substance reduction or recovery from substance use disorder.
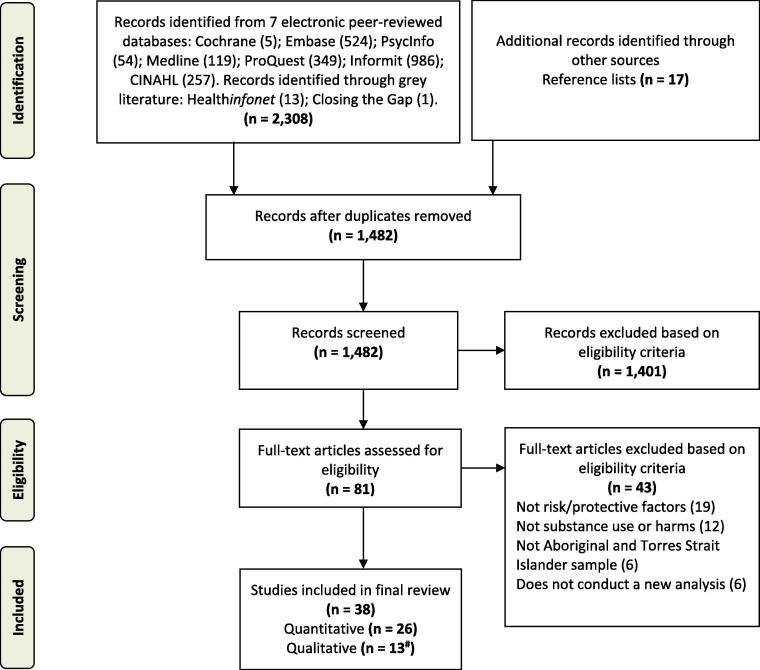
The complete search and selection strategy are summarised in Fig. 1. Search terms were based on previous reviews (Burnette and Figley, 2017, Stone et al., 2012) and aimed to identify studies that assessed the risk and protective factors of substance use and related harms for Aboriginal and Torres Strait Islander peoples: ((Aborigin* OR “Torres Strait Islander” OR Indigenous) and Australia) AND ((risk OR protec* OR resilienc* OR underlying OR ecological OR vulnerab* OR psychosocial) AND (factor OR mechanism OR character*)) AND (wellbeing OR mental health OR substance OR alcohol OR drug OR tobacco), see Supplementary Table 1 (Snijder et al., 2018). Searches were conducted in May 2017 and repeated in May 2018.
Fig. 1.
PRISMA flow diagram: Systematic search strategy to identify studies examining the risk and protective factors for substance use and related harms among Aboriginal and Torres Strait Islander Australians.
# One study included in the systematic review reported both quantitative and qualitative data.
In total, the titles and abstracts of 1,482 studies were screened by BL, with inter-rater reliability tested on a random sample of 25% of studies by MS. There was agreement on the application of the eligibility criteria for 94% of studies based on their titles and abstracts. The eligibility of 81 full text articles was independently assessed by BL and MS, with 92% agreement (κ = 0.821; strong agreement (McHugh, 2012). At all stages of study selection, differences were reconciled in consultation between the two authors.
2.2. Statistical analysis
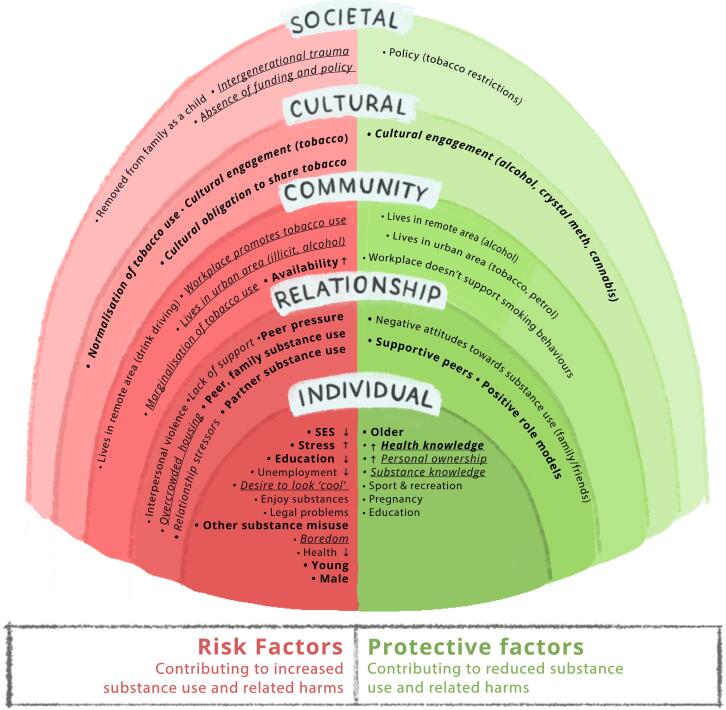
Data relating to study design, participant characteristics and study outcomes were extracted by BL into an Excel spreadsheet and reviewed for accuracy by MS. Risk and protective factors extracted from studies were organised by ecological level, in accordance with Burnette and Figley’s ecosystemic framework of historical oppression, resilience and transcendence (Burnette and Figley, 2017) and Bronfenbrenner and Morris’ ecological model (Bronfenbrenner et al., 1998), see the review protocol for details (Snijder et al., 2018). Ecological levels include: Individual, relationship, community, culturally-distinct and societal (Fig. 2). Where available, odds and risk ratios were also extracted. In studies that provided crude and adjusted results, only adjusted odds were considered. No studies included multiple adjusted estimates. We calculated the odds ratios in studies where these were not provided and relevant data were available. Authors of two studies were contacted and both provided us with data to calculate odds ratios. To calculate, we extracted the number of participants who (a) displayed the risk or protective factor and used substances; (b) did not display the risk or protective factor but used substances; (c) displayed the risk or protective factor but did not use substances; and (d) did not display the risk or protective factor and did not use substances. The odds ratio was calculated from the product of (a) and (d), divided by the product of (b) and (c). All available odds ratios were collated in forest plots, organised by substance type (see Supplementary Figs. 1–4).
Fig. 2.
Legend: Factors included in the model were reported in at least two studies as a risk and/or protective factor for substance use and/or related harms. Bolded factors were reported in more than seven studies. Factors in underlined italics were reported only in qualitative studies.
2.3. Critical appraisal of study methodology
We used the Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data (Munn et al., 2015) to assess the methodological quality of quantitative studies and the qualitative tool by Long and Godfrey (Long et al., 2002) for qualitative studies. The assessment of both quantitative and qualitative studies was conducted by BL. MS independently reviewed a random sample of 25% of studies. There was 92% agreement between authors, with differences in opinion reconciled in discussions between the two authors.
2.4. Ethics
Ethics approval was not required for this study as it was systematic review of publicly accessible documents and involved no new data collection.
3. Results
A total of 38 publications reported on risk and/or protective factors of substance use and related harms for Aboriginal and Torres Strait Islander peoples (Table 1). Twenty-five were quantitative, 12 were qualitative studies and one used a mixed methods approach. Studies examined factors related to tobacco (n = 28), alcohol (n = 12), cannabis (n = 8), petrol sniffing (n = 4), methamphetamine (n = 2), kava (n = 1) and opioid use (n = 1). Detailed results of the included studies can be found in Supplementary Table 2.
3.1. Critical appraisal of research methods used
A total of 32 cross-sectional (nine qualitative) studies and six longitudinal (three qualitative) studies, spanning one to seven years, were included in this review. Sixteen (62%) quantitative studies received a high score, rating between seven and nine out of nine (Table 2). Testing methods, sample size and participant selection were considered appropriate in 14 (54%) studies. Table 3 summarises the critical appraisal of the qualitative studies.
Table 2.
Critical appraisal of included quantitative studies (n = 26).
 |
Table note. Total scores were calculated by sum of checkmarks, with scores indicating poor (red; 0–3), moderate (orange; 4–6), or high (green; 7–10) quality.
Table 3.
Critical appraisal of included qualitative studies (n = 13).
| First author (year) | Sample | Data collection | Data analysis | Potential bias | Implications |
|---|---|---|---|---|---|
| Bond et al. (2012) | Purposive and snowball selection | Detailed description | Detailed description | Position of local researcher described | Discussed implications for practice |
| Dawson et al. (2012) | Purposive selection | Detailed description | Detailed description | Position of researcher described | Discussed implications for practice and policy |
| Gamarania et al. (1998) | Convenience selection, sample not appropriate for aims | Little detail | Very little detail | Not described | Discussed implications for practice |
| Gould et al. (2017) | Purposive selection | Detailed description | Detailed description | Position of researcher described | Discussed implications for practice and policy |
| Johnston and Thomas, 2008 | Purposive and snowball selection | Detailed description | Detailed description | Not described | Discussed implications for practice |
| Johnston et al. (2012) | Purposive selection | Detailed description | Detailed description | Position of researcher described | Discussed implications for practice and policy |
| Leavy et al. (2010) | Purposive selection | Little detail | Very little detail | Not described | Discussed implications for practice |
| MacLean et al. (2017) | Convenience selection | Little detail | Little detail | Not described | Discussed implications for practice and policy |
| Maddox et al. (2015) | Convenience and snowball selection | Detailed description | Detailed description | Position of researcher described | Discussed implications for practice and policy |
| Passey et al. (2011) | Purposive selection | Detailed description | Detailed description | Position of researcher described | Discussed implications for practice |
| Senior et al. (2006) | Purposive selection | Little detail | Very little detail | Not described | Not described |
| Tsourtos et al. (2015) | Purposive and snowball selection | Detailed description | Detailed description | Not described | Discussed implications for practice |
| Wood et al. (2008) | Convenience selection | Detailed description | Detailed description | Not described | Discussed implications for practice and policy |
3.2. Risk and protective factors
Fig. 2 provides an ecological model (Burnette and Figley, 2017, Bronfenbrenner et al., 1998) showing risk and protective factors for substance use and related harms experienced by Aboriginal and Torres Strait Islander peoples that were identified by at least two studies. Table 4 lists the number of studies identifying each factor. Supplementary Figs. 1 to 4 display all available odds ratios per drug type and factor. The findings are described for factors identified in at least two studies, odds and risk ratios are provided where available.
Table 4.
Summary of factors associated with substance use among Aboriginal and Torres Strait Islander peoples.
| Factors |
n studies reporting as risk factor |
n studies reporting as protective factor |
||
|---|---|---|---|---|
| Qual | Quant | Qual | Quant | |
| Individual-level factors | ||||
| Psychological distress | 8 | 8 | – | – |
| Incomplete > complete education | 2 | 10 | – | – |
| Concurrent substance use | 3 | 8 | – | – |
| Unemployed > employed | 3 | 7 | – | – |
| Males > females | – | 9 | – | – |
| Younger > older | 1 | 6 | 1 | 1 |
| Poor health > prioritize health | 1 | 4 | 1 | – |
| Boredom > engaged | 4 | 1 | – | – |
| Personal ownership (self-esteem, resilience) | – | – | 3 | – |
| Legal problems | – | 3 | – | – |
| Low income > high income | 1 | 2 | – | – |
| Enjoy substances | 2 | 1 | – | – |
| Knowledge of substance health effects | – | – | 2 | – |
| Desire to portray image of being cool | 2 | – | – | – |
| Pregnancy | 1 | – | 1 | 1 |
| Engaged in sport, recreational activities | – | – | 1 | 1 |
| Having own money | 1 | – | – | – |
| Negative stressors | 1 | – | – | – |
| Children’s age | 1 | – | – | – |
| n children | – | 1 | – | – |
| English as second language | – | 1 | – | – |
| Home owner | – | – | – | 1 |
| Relationship-level factors | ||||
| Peer substance use, pressure (including living with users) | 10 | 6 | – | – |
| Supportive peers | – | – | 8 | 2 |
| Inter-personal violence | – | 3 | – | – |
| n living in home | 2 | – | – | 1 |
| Negative stressors | 1 | 1 | – | – |
| Peer financial strain | – | 1 | – | – |
| Married | – | – | – | 1 |
| Peer death | – | – | – | 1 |
| Social engagement | – | – | – | 1 |
| Community-level factors | ||||
| Substance availability | 5 | 2 | – | – |
| Urban > remote | 1 | 2 | – | 3 |
| Urban > capital city | – | 4 | – | 2 |
| Marginalisation for substance use | 2 | – | – | – |
| Remote > capital city | – | 2 | – | 1 |
| Workplace promotes substance use | 2 | – | – | – |
| Access to substance use services | – | – | 1 | – |
| Social opportunities in community | 1 | – | – | – |
| Recreational opportunities in community | 1 | – | – | – |
| Culturally distinct-level factors | ||||
| Normalisation of tobacco use | 8 | – | – | – |
| Cultural obligation to share tobacco | 3 | |||
| Cultural engagement | – | 2 | 2 | – |
| Conflict from living between two cultures | 1 | – | – | – |
| Societal-level factors | ||||
| Removed from family as child | – | 2 | – | – |
| Intergenerational trauma | 3 | – | – | – |
| Policy | 1 | – | 2 | – |
| Racism | 1 | – | – | – |
| Westernised health promotion | 1 | – | – | – |
3.2.1. Individual factors
3.2.1.1. Mental health
Psychological stress or distress was consistently reported as a risk factor for substance use. Participants who reported psychological distress were 2.20 times more likely to use tobacco (Brown et al., 2016), 4.19 times more likely to use cannabis (Brown et al., 2016), 2.67 times more likely to use opioids (Smirnov et al., 2016) and 4.86 times more likely to use both opioids and methamphetamines (Smirnov et al., 2016), compared to those who did not report distress. Participants not experiencing stress were 1.30 times more likely to abstain from tobacco use (Thomas et al., 2008). Individual stressors that were consistently linked with substance use in qualitative studies included emotional and financial pressures and fear of failure (Dawson et al., 2012, Passey et al., 2011, Johnston and Thomas, 2008, Tsourtos et al., 2015, Gould et al., 2017). Qualitative studies identified that low self-esteem was associated with tobacco use (Bond et al., 2012), while higher self-esteem, resilience, confidence and a sense of ownership was associated with tobacco abstinence or quitting (Johnston and Thomas, 2008, Tsourtos et al., 2015, Bond et al., 2012).
3.2.1.2. Multiple substance use
Three studies reported on risks of poly substance use. Pregnant women with other substance use problems were 5.71 times more likely to use tobacco and 36.17 times more likely to use cannabis than those without other substance use problems (Brown et al., 2016). Community members who used cannabis were 9.10 times more likely to sniff petrol, 19.00 times more likely to use tobacco and less likely to use kava (OR = 0.40), compared to those who abstained from cannabis use (Clough et al., 2004). Participants who sniffed petrol were 3.90 times more likely to use cannabis and 4.40 times more likely to engage in heavy cannabis use, compared to those who did not sniff petrol (Lee et al., 2009).
3.2.1.3. Health and lifestyle factors
Eleven studies reported on health and lifestyle factors and substance use. Overall, health prioritisation and knowledge of health effects were protective against substance use. Enjoying smoking was identified as a risk factor for continued smoking (Johnston and Thomas, 2008, Maksimovic et al., 2013, Gamarania et al., 1998), but prioritising health was consistently reported to protect against tobacco and cannabis use (Brown et al., 2016, Thomas et al., 2008, Bond et al., 2012, Maksimovic et al., 2013, Jacups and Rogerson, 2015, Wood et al., 2008). Qualitative studies reported that health prioritisation occurred after a personal health crisis, which led to a positive life transition encouraging substance cessation (Bond et al., 2012, Wood et al., 2008). Pregnancy was similarly found to motivate substance cessation (Gould et al., 2017, Maksimovic et al., 2013). One qualitative study found individuals were more likely to abstain or cease tobacco use if they gained knowledge of the adverse health effects of smoking (Gamarania et al., 1998). Conversely, another study found that those who had limited knowledge of the health effects were more likely to smoke (Dawson et al., 2012). Engaging in sporting or recreational activities was associated with 1.49 times more tobacco abstinence (Thomas et al., 2008, Passey et al., 2011).
3.2.1.4. Socioeconomic status (SES) factors
Lower levels of education were consistently reported as a risk factor for substance use. Participants who did not complete high school, compared to those who completed high school, were 1.95 to 3.58 times more likely to use tobacco according to two studies (Brown et al., 2016, Maddox et al., 2015) and up to 21.50 times more likely according to a third study (Passey et al., 2012). Participants who did not complete high school were also 3.97 to 5.43 times more likely to use cannabis (Brown et al., 2016, Jacups and Rogerson, 2015) and 3.08 times more likely to use multiple substances (Passey et al., 2014). High school completion was associated with less tobacco use (OR = 0.56) (Cunningham, 1997) and 1.60 times more tobacco abstinence (Thomas et al., 2008). Those who did not complete a post-secondary qualification were 1.59 to 7.74 times more likely to use tobacco (Brown et al., 2016, Passey et al., 2012), 1.93 to 6.66 times more likely to use cannabis (Brown et al., 2016) and 2.81 times more likely to use multiple substances (Passey et al., 2012).
Unemployment and low SES was consistently reported as a risk factor for substance use. Unemployment, compared to employment, was associated with 1.43 to 3.31 times more tobacco use (Brown et al., 2016, Cunningham, 1997), 3.42 times more cannabis use (Brown et al., 2016), 2.82 times more multiple substance use (Noble et al., 2015) and 8.98 times more dual use of methamphetamines and opioids (Smirnov et al., 2016). Qualitative studies identified that unemployment contributed to minimal routine and boredom, which was associated with increased petrol sniffing (Senior et al., 2006), cannabis use (Jacups and Rogerson, 2015) and tobacco use (Passey et al., 2011, Johnston and Thomas, 2008, Wood et al., 2008, Heath et al., 2006, Leavy et al., 2010). Individuals in higher SES quintiles were 1.49 to 2.50 times more likely to abstain from tobacco compared to those in the lowest SES quintile (Thomas et al., 2008). Of note, pregnant women with low SES were 2.64 times more likely to smoke during pregnancy than higher SES pregnant women (Thrift et al., 2011). Individuals who did not experience financial distress were also 2.33 times more likely to abstain from tobacco use, compared to those that did (Thomas et al., 2008).
Legal problems were also associated with risk of substance use. Legal problems were associated with 4.27 times more cannabis use (Jacups and Rogerson, 2015) and less tobacco abstinence (OR = 0.40) (Thomas et al., 2008). Those who had been incarcerated were more likely to use cannabis (Jacups and Rogerson, 2015), less likely to abstain from tobacco use (OR = 0.35) (Thomas et al., 2008), 3.70 times more likely to use opioids (Smirnov et al., 2016) and 3.78 times more likely to use both opioids and methamphetamines compared to those that had never been incarcerated (Smirnov et al., 2016).
3.2.1.5. Age and sex
Across studies, males were more likely than females to use substances. Studies indicated that males were 1.01 to 3.17 times more likely to use tobacco and 1.08 to 3.35 more likely to drink alcohol than females (Australian Bureau of Statistics, 1995, Australian Bureau of Statistics, 1996, Australian Bureau of Statistics, 2004, Australian Bureau of Statistics, 2016, Australian Bureau of Statistics, 2008, Hall et al., 1993). Males were also 2.35 times more likely to be fined for drink driving (Fitts et al., 2017) and 3.11 times more likely to use any substance compared to females (Noble et al., 2015). A complex relationship between substance use and age emerged. Individuals aged 15–24 years and 45 years and older were less likely to use tobacco than 25–44 year olds (OR = 0.82 and 0.48–0.56, respectively) (Cunningham, 1997). Aboriginal and Torres Strait Islander peoples older than 55 years were less likely to use any substances compared to Aboriginal and Torres Strait Islander peoples younger than 55 years (OR = 0.17) (Noble et al., 2015). The risk of repeat drink driving offences decreased with age: 40 year olds were less likely to be fined than 15–24 year-olds (OR = 0.73) (Fitts et al., 2013). Specifically, 14–17-year old’s were 4.44 times more likely, and 18–20-year old’s were 2.36 times more likely to have repeat drink driving offences compared to 21–24-year old’s (Fitts et al., 2017).
3.2.2. Relationship factors
Peer substance use was consistently found to be a risk factor for personal substance use. Individuals who had tobacco using peers were 1.60 times more likely to smoke, and those who had peers who used alcohol or cannabis were 1.40 times more likely to use alcohol or cannabis themselves (Gazis et al., 2010). Pregnant women whose partner had substance use problems were 1.99 times more likely to smoke and 6.44 times more likely to use cannabis than those whose partner did not have substance use problems (Brown et al., 2016). Qualitative studies also indicated peer substance use was a risk factor for personal substance use (Maksimovic et al., 2013, Jacups and Rogerson, 2015, Heath et al., 2006). Specifically, peer substance use created pressure for individuals to use tobacco (Dawson et al., 2012, Johnston and Thomas, 2008, Gamarania et al., 1998, Leavy et al., 2010, Johnston et al., 2012) or sniff petrol (Senior et al., 2006). Participants with non-smoking friends and families and who explicitly disapproved of tobacco use were less likely to initiate tobacco use (Passey et al., 2011, Gould et al., 2017, Gamarania et al., 1998, Johnston et al., 2012). The anti-smoking advice and reinforcing messages from peers against tobacco use was associated with less tobacco use in youth compared to adults (Passey et al., 2011, Johnston et al., 2012). Conversely, participants who viewed smoking as an opportunity to yarn, had a desire to fit in and received encouragement to smoke from peers were more likely to smoke (Johnston and Thomas, 2008, Tsourtos et al., 2015, Wood et al., 2008).
Seven studies reported that participants who had a higher level of support from friends and families were more likely to abstain from, or quit using, tobacco (Johnston and Thomas, 2008, Tsourtos et al., 2015, Bond et al., 2012, Clough et al., 2004, Wood et al., 2008), cannabis (Jacups and Rogerson, 2015) and petrol (Dingwall et al., 2012). Individuals who did not have support in a time of crisis were less likely to abstain from tobacco (OR = 0.59) (Thomas et al., 2008, Dawson et al., 2012). Having positive role models, who did not use tobacco, was also identified as a protective factor against tobacco use (Passey et al., 2011, Johnston and Thomas, 2008, Johnston et al., 2012), while a lack of positive role models increased the likelihood of tobacco use (Dawson et al., 2012).
Interpersonal violence was consistently found to be a risk factor for substance use. Participants who had experienced interpersonal violence were 3.24 times more likely to use cannabis (Brown et al., 2016) and 3.87 times more likely to use substances compared to those who had not (Noble et al., 2015). Participants who had experienced violence in the past 12 months were less likely to abstain from smoking compared to those who had not (OR = 0.56) (Thomas et al., 2008). Furthermore, relationship difficulties and death of a loved one were identified as stressors that contributed to tobacco, cannabis and crystal methamphetamine use (Brown et al., 2016, Dawson et al., 2012, Maksimovic et al., 2013, MacLean et al., 2017). Furthermore, living in overcrowded housing was associated with tobacco use (Johnston and Thomas, 2008) and both increased sniffing (Senior et al., 2006) and sniffing abstinence (Dingwall et al., 2012).
3.2.3. Community factors
Complex relationships between geographic location and substance use were identified. Aboriginal and Torres Strait Islander peoples in urban areas were more likely to use alcohol (Australian Bureau of Statistics, 1996) and illicit drugs (OR = 1.40) (Australian Bureau of Statistics, 2016), but also more likely to abstain from sniffing petrol, compared to those in remote areas (Dingwall et al., 2012). Aboriginal and Torres Strait Islander peoples in remote areas were 1.54 to 1.58 times more likely to use tobacco (Australian Bureau of Statistics, 2016, Australian Bureau of Statistics, 2008, Australian Bureau of Statistics, 2009), 2.53 times more likely to have repeat drink driving offences (Fitts et al., 2013), but were also more likely to abstain from alcohol (Australian Bureau of Statistics, 2008) compared to those in urban areas. One study identified an interaction between remoteness and sex, whereby females in remote areas were 1.25 times more likely to abstain from smoking compared to females living in urban areas; whereas males in remote areas were less likely to abstain from smoking compared to males in urban areas (OR = 0.66) (Thomas et al., 2008).
Three qualitative studies reported on substance use discouragement and marginalisation from the community and found it was both a risk and protective factor for personal substance use. One study reported higher tobacco use in work settings that accepted smoking (Dawson et al., 2012), while a second study found smoking was lower in workplaces where tobacco use was actively discouraged (Bond et al., 2012). One qualitative study identified that experiencing stigma and social exclusion for being a non-smoker contributed to higher tobacco use (Dawson et al., 2012). Another study identified that marginalisation of smokers was linked to increased smoking and seeking out other smokers to normalise the behaviour (Johnston et al., 2012).
In terms of availability, there was an increased risk of substance use among young people when cannabis, crystal methamphetamine, petrol and tobacco were highly accessible with unregulated access (Passey et al., 2011, Johnston and Thomas, 2008, Jacups and Rogerson, 2015, Maddox et al., 2015, Johnston et al., 2012, Dingwall et al., 2012, MacLean et al., 2017).
3.2.4. Culturally-distinct factors
Complex associations between substance use and connection to culture and Country emerged from the review. Aboriginal and Torres Strait Islander Australians with high cultural participation, exploration, affirmation and belonging, combined with peers who did not use alcohol or cannabis, were less likely to use alcohol or cannabis (Gazis et al., 2010). Connection to culture and Country were also important protective factors linked to crystal methamphetamine abstinence and cessation among Aboriginal and Torres Strait Islander populations (MacLean et al., 2017).
Individuals who spent time learning about their culture were more likely to use tobacco (Gazis et al., 2010). Furthermore, tobacco use was lower among people who did not identify the role of Elders as important (OR = 0.66 males and 0.81 females) and those who did not recognise their homelands (OR = 0.76 females) (Cunningham, 1997). Qualitative studies indicated that sharing and accepting tobacco from relatives and peers was a cultural obligation among Aboriginal and Torres Strait Islander peoples (Passey et al., 2011, Johnston and Thomas, 2008, Johnston et al., 2012). Sharing tobacco has been passed down through generations, reinforcing tobacco use as normal, acceptable and highly prevalent (Dawson et al., 2012, Passey et al., 2011, Johnston and Thomas, 2008, Johnston et al., 2012). Qualitative studies consistently identified that tobacco was used extensively within Aboriginal Australian networks, which reinforced the perception that tobacco use was normal and acceptable (Collins, 2016, World Health Organization, 2009, Maddox et al., 2015, Leavy et al., 2010, Johnston et al., 2012, Dawson et al., 2012, Passey et al., 2011, Johnston and Thomas, 2008, Tsourtos et al., 2015).
3.2.5. Societal factors
Intergenerational trauma, caused by colonisation and government policies, was identified in qualitative papers as a contributor to crystal methamphetamine use (MacLean et al., 2017) and tobacco use (Passey et al., 2011, Johnston and Thomas, 2008). Participants who were removed from their family as a child were 1.37 (females) to 1.88 (males) times more likely to use tobacco (Cunningham, 1997) and less likely to abstain from tobacco use (OR = 0.46) (Thomas et al., 2008).
A number of qualitative studies identified that smoke free policies, including tobacco restrictions, had a protective effect (Dawson et al., 2012, Johnston et al., 2012), while the absence of smoke-free policies and short-term funding impeded tobacco cessation (Dawson et al., 2012).
4. Discussion
This was the first study to synthesise the evidence and create an ecological model of risk and protective factors of substance use and related harms experienced by Aboriginal and Torres Strait Islander peoples. This systematic literature review identified 38 studies and the most commonly identified (i.e. in more than two studies) risk and protective factors have been depicted in Fig. 2. Overall, individual-level risk factors included low SES, high psychological distress, multiple substance use, being young and and being male. Individual-level protective factors were being over the age of 45 years and health prioritisation and knowledge. Relationship-level risk factors were substance use by peers, family members or partner, as well as peer pressure; while protective factors were supportive environments and positive role models. A community-level risk factor was availability of substances. Associations between other community-level factors (i.e., geographic location, substance use marginalisation) and substance use emerged as both risk and protective factors across different studies. Culturally-distinct risk factors included the obligation share and accept tobacco and normalisation of tobacco use in Aboriginal communities. Cultural engagement was identified as a protective factor for alcohol, cannabis and crystal methamphetamine use, but showed a complex relationship with tobacco use. Finally, a societal-level risk factor of substance use was intergenerational trauma and a protective factor against tobacco use was smoke free policies.
These factors can inform entry points for approaches addressing substance related harms at the different ecological levels. The findings can also inform a systems approach by addressing factors on each level, as well as the interaction between the factors across levels (Rutter et al., 2017). This ecological approach aligns with the holistic perspective on health and wellbeing of Aboriginal and Torres Strait Islander peoples that goes beyond the health of the individual and includes the interconnections between family, community and culture (NACCHO, 2001).
The majority of risk and protective factors associated with substance use and related harms identified in this review are not unique to Aboriginal and Torres Strait Islander peoples (Baler and Volkow, 2011, Li and Burmeister, 2009). However, this review highlights the impact of intergenerational trauma, caused by past and current government policies, on individual substance use and related harms experienced by Aboriginal and Torres Strait Islander peoples. Intergenerational trauma likely contributes to increased psychological distress experienced by Aboriginal and Torres Strait Islander peoples (Azzopardi et al., 2018), which was the most commonly identified individual risk factor for substance use and related harms. Increasing agency and autonomous decision-making are important factors to protect against further trauma and associated psychological distress (Tsey, 2008).
In terms of cultural factors, connection to Country and culture have been identified as protective factors for methamphetamine (MacLean et al., 2017), cannabis and alcohol use (Gazis et al., 2010). However, studies included in this review identified cultural connection as a risk factor for tobacco use, albeit this finding needs to be considered with caution. While desert bush tobacco was traditionally used by Aboriginal communities prior to colonisation, tobacco was introduced by the colonisers as a friendship gesture and as a currency for trade (Van der Sterre et al., 2012). The traditional use of tobacco has become indistinguishable from ‘modern’ tobacco use. The cultural obligation of sharing has likely contributed to the normalisation of tobacco use among Aboriginal communities, contributing to smoking being viewed as a cultural activity (Johnston et al., 2012, Dawson et al., 2012, Passey et al., 2011, Johnston and Thomas, 2008). Another potential explanation for the bidirectional link between connection to culture and tobacco use is the confounding factors of living in remote areas and low SES, which likely has an indirect effect on other identified individual- and relationship-level risk factors. Aboriginal and Torres Strait Islander peoples in remote areas have lower SES and higher smoking rates (Australian Bureau of Statistics, 2016, Australian Bureau of Statistics, 2008, Australian Bureau of Statistics, 2009) but also increased connection to culture and Country (Australian Bureau of Statistics, 2010, Dockery, 2017). Therefore, it is possible that remoteness is the primary factor influencing higher smoking rates, rather than the connection with culture. Further exploration into moderators of identified risk and protective factors is needed to better inform substance use intervention strategies and public health initiatives. Given that this review only found three culturally-distinct risk and protective factors, ongoing research into connection to culture and wellbeing is timely and important (Lovett et al., 2017).
The evidence for most individual risk and protective factors was based on multiple well-conducted qualitative and quantitative studies, particularly for tobacco use and the factors of psychological distress, education, employment, gender, age and concurrent substance use. However, most risk and protective factors on relationship, community, cultural and societal levels were primarily drawn from single studies of poorer quality. For this reason, a threshold of just two studies was required for a risk or protective factor to be included in the ecological model which limits the generalisability and representativeness of the model. More rigorous research is required to strengthen the evidence of relationship, community, societal and culturally-distinct factors contributing to substance use and related harms among Aboriginal and Torres Strait Islander peoples. Developing a more comprehensive ecological understanding of the risk and protective factors of substance use and harms can inform the development of approaches addressing substance use that go beyond individual behavioural health promotion strategies. While there is some evidence that behavioural health promotion strategies can make small improvements in health outcomes, their effectiveness is often reduced by structural impediments experienced by Aboriginal and Torres Strait Islander peoples (e.g. low SES or low education levels) to respond to health promotion messages (Baum and Fisher, 2014). While some of these structural impediments are identified in this review, further research is required to expand and strengthen the ecological understanding presented in this paper. It is critical that public health approaches acknowledge these structural, and resultant social, determinants (Marmot, 2011), including the impacts of intergenerational trauma; and in turn prioritise Aboriginal and Torres Strait Islander leadership in policy and decision-making. It is only by allowing Aboriginal and Torres Strait Islander communities to lead the process that the structural and social determinants will be addressed (Sterne et al.).
The varying quality of the included studies also likely contributed to large differences in the outcomes reported in different studies for the same factors. This variation in study quality relates to a small number of participants, the use of different outcome measures and a lack of randomised participant recruitment. In order to strengthen the quality of the evidence around risk and protective factors of substance use, there is a need to use comparable, standardised and validated measures of drug and alcohol use and related harms for Aboriginal and Torres Strait Islander peoples.
While positive progress is being made in reducing substance use rates among Aboriginal and Torres Strait Islander peoples, especially in terms of tobacco use (Lovett et al., 2017, Institute, 2015), substance use and related harms remain significantly higher among Aboriginal and Torres Strait Islander peoples compared to non-Indigenous Australians (Australian Aboriginal and Torres Strait Islander Health Survey, 2013, Australian Institute of Health and Welfare, 2006). Overall, this review highlights psychological distress, socio-economic status (including income, employment and education), concurrent substance use, positive and supportive family and peer relations, availability of substances, normalisation of tobacco use and intergenerational trauma as factors with the most evidence for influencing substance use and related harms. Therefore, these are likely priority areas to address substance use and related harms among Aboriginal and Torres Strait Islander peoples.
Funding
The research is supported by funding from the Australian Government Department of Health, and via a Centre of Research Excellence in the Prevention and Early Intervention in Mental Illness and Substance Use (PREMISE; GNT11349009). LS is supported by the National Health and Medical Research Council (GNT1132853). NN is supported by the National Health and Medical Research Council (GNT1166377). JW is supported by the National Health and Medical Research Council (GNT1125983). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Role of the funding source
The funders of this review had no role in the study’s design, analysis, or interpretation of findings. The corresponding author had full access to all the data used in this review and had final responsibility for the decision to submit for publication.
CRediT authorship contribution statement
Mieke Snijder: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Project administration. Briana Lees: Methodology, Formal analysis, Investigation, Data curation, Writing - original draft. Annalee Stearne: Conceptualization, Methodology, Writing - review & editing. James Ward: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition. Sophia Garlick Bock: Formal analysis, Writing - review & editing. Nicola Newton: Conceptualization, Methodology, Writing - review & editing, Funding acquisition. Lexine Stapinski: Conceptualization, Methodology, Writing - review & editing, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
In this paper we use the term “Indigenous” when referring to broadly to Indigenous peoples globally. When referring to the First people of Australia, we use the term “Aboriginal and Torres Strait Islander peoples”, or “Aboriginal” when a shorter term is required following guidelines from the NSW Aboriginal Health and Medical Research Council.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101277.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Australian Aboriginal and Torres Strait Islander Health Survey, 2013. Canberra, Australian Bureaus of Statistics.
- Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2010. The City and the Bush: Indigenous Wellbeing Across Remoteness Areas. [Google Scholar]
- Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2017. 2016 Census Data Summary: Aboriginal and Torres Strait Islander Population. [Google Scholar]
- Australian Bureau of Statistics, 1995. National Aboriginal and Torres Strait Islander Survey 1994.
- Australian Bureau of Statistics, 1996. National Aboriginal and Torres Strait Islander Survey: Australia's Indigenous Youth, 1994.
- Australian Bureau of Statistics, 2004. National Aboriginal and Torres Strait Islander Social Survey 2002.
- Australian Bureau of Statistics, 2008. The Australians Institute of Health and Welfare. The Health and welfare of Australia's Aboriginal and Torres Strait Islander Peoples 2008.
- Australian Bureau of Statistics, 2009. National Aboriginal and Torres Strait Islander Social Survey 2008.
- Australian Bureau of Statistics, 2016. National Aboriginal and Torres Strait Islander Social Survey 2014-15.
- Australian Institute for Health and Welfare . AIHW; Canberra: 2016. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Aboriginal and Torres Strait Islander People 2011. [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare . AIHW; Canberra: 2006. Drug use among Aboriginal and Torres Strait Islander peoples: an assessment of data sources. [Google Scholar]
- Azzopardi P.S., Sawyer S.M., Carlin J.B., Degenhardt L., Brown N., Brown A.D. Health and wellbeing of Indigenous adolescents in Australia: a systematic synthesis of population data. Lancet. 2018;391(10122):766–782. doi: 10.1016/S0140-6736(17)32141-4. [DOI] [PubMed] [Google Scholar]
- Baler R.D., Volkow N.D. Addiction as a systems failure: focus on adolescence and smoking. J. Am. Acad. Child Adolesc. Psychiatr. 2011;50(4):329–339. doi: 10.1016/j.jaac.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum F., Fisher M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol. Health Illness. 2014;36(2):213–225. doi: 10.1111/1467-9566.12112. [DOI] [PubMed] [Google Scholar]
- Bond C., Brough M., Spurling G., Hayman N. 'It had to be my choice' Indigenous smoking cessation and negotiations of risk, resistance and resilience. Health Risk Soc. 2012;14(6):565–581. [Google Scholar]
- Bronfenbrenner U., Morris P.A. The ecology of developmental processes. In: Damon W., Lerner R., editors. Handbook of Child Psychology. John Wiley & Sons; Hoboken, NJ, US: 1998. pp. 993–1028. [Google Scholar]
- Brown S.J., Mensah F.K., Ah Kit J., Stuart-Butler D., Glover K., Leane C. Use of cannabis during pregnancy and birth outcomes in an Aboriginal birth cohort: a cross-sectional, population-based study. BMJ Open. 2016;6(2):e010286. doi: 10.1136/bmjopen-2015-010286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette C.E., Figley C.R. Historical oppression, resilience, and transcendence: can a holistic framework help explain violence experienced by indigenous people? Social Work. 2017;62(1):37–44. doi: 10.1093/sw/sww065. [DOI] [PubMed] [Google Scholar]
- Clough A.R., D'Abbs P., Cairney S., Gray D., Maruff P., Parker R. Emerging patterns of cannabis and other substance use in Aboriginal communities in Arnhem Land Northern Territory– a study of two communities. Drug Alcohol Rev. 2004;23(4):381–390. doi: 10.1080/09595230412331324509. [DOI] [PubMed] [Google Scholar]
- Collins S.E. Associations between socioeconomic factors and alcohol outcomes. Alcohol Res. Curr. Rev. 2016;38(1):83–94. [PMC free article] [PubMed] [Google Scholar]
- Cunningham J., Australian Bureau of Statistics . Cigarette Smoking Among Indigenous Australians, 1994. Australian Bureau of Statistics; Canberra: 1997. [Google Scholar]
- Dawson A.P., Cargo M., Stewart H., Chong A., Daniel M. Aboriginal health workers experience multilevel barriers to quitting smoking: a qualitative study. Int. J. Equity Health. 2012;11:27. doi: 10.1186/1475-9276-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingwall K.M., Maruff P., Clough A.R., Cairney S. Factors associated with continued solvent use in Indigenous petrol sniffers following treatment. Drug Alcohol Rev. 2012;31(1):40–46. doi: 10.1111/j.1465-3362.2010.00279.x. [DOI] [PubMed] [Google Scholar]
- Dockery A.M. Ninti One Limited; Alice Springs: 2017. Culture, Housing, Remoteness and Aboriginal and Torres Strait Islander Child Development: Evidence from the Longitudinal Study of Indigenous Children. [Google Scholar]
- Fitts M.S., Palk G.R., Lennon A.J., Clough A.R. What are the offence and offender risk factors for Indigenous repeat drink drivers in Queensland? J. Austral. College Road Safety. 2013;24(2):39–47. [Google Scholar]
- Fitts M.S., Palk G.R., Lennon A.J., Clough A.R. The characteristics of young Indigenous drink drivers in Queensland, Australia. Traffic Inj. Prev. 2017;18(3):237–243. doi: 10.1080/15389588.2016.1186273. [DOI] [PubMed] [Google Scholar]
- Gamarania G., Malpraburr T., Johnston F., Beecham R., Dalgleish P. The Maningrida:'Be Smoke Free'project. Health Promotion J. Austr. J. Austr. Assoc. Health Promotion Professionals. 1998;8(1):12. [Google Scholar]
- Gazis N., Connor J.P., Ho R. Cultural identity and peer influence as predictors of substance use among culturally diverse australian adolescents. J. Early Adolesc. 2010;30(3):345. [Google Scholar]
- Gould G.S., Bovill M., Clarke M.J., Gruppetta M., Cadet-James Y., Bonevski B. Chronological narratives from smoking initiation through to pregnancy of Indigneous Australian women: a qualitative study. Midwifery. 2017;52:27–33. doi: 10.1016/j.midw.2017.05.010. [DOI] [PubMed] [Google Scholar]
- Hall W., Hunter E., Spargo R. Alcohol-related problems among Aboriginal drinkers in the Kimberley region of Western Australia. Addiction. 1993;88(8):1091–1100. doi: 10.1111/j.1360-0443.1993.tb02128.x. [DOI] [PubMed] [Google Scholar]
- Heath, D.L., Panaretto, K., Manessis, V., Larkins, S., Malouf, P., Reilly, E., et al., 2006. Factors to consider in smoking interventions for Indigenous women.
- Huria T., Palmer S.C., Pitama S., Beckert L., Lacey C., Ewen S. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med. Res. Methodol. 2019;19(1):173. doi: 10.1186/s12874-019-0815-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare, 2015. The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples. Canberra, AIHW.
- Jacups S., Rogerson B. Lifetime influences for cannabis cessation in male incarcerated Indigenous australians. J. Psychoactive Drugs. 2015;47(2):117–124. doi: 10.1080/02791072.2015.1014949. [DOI] [PubMed] [Google Scholar]
- Johnston V., Thomas D.P. Smoking behaviours in a remote Australian indigenous community: the influence of family and other factors. Social Sci. Med. 2008;67(11):1708–1716. doi: 10.1016/j.socscimed.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Johnston V., Westphal D.W., Earnshaw C., Thomas D.P. Starting to smoke: a qualitative study of the experiences of Australian Indigenous youth. BMC Public Health. 2012;12:963. doi: 10.1186/1471-2458-12-963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M., Smith A., Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet. 2009;374(9683):76–85. doi: 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- Leavy J., Wood L., Phillips F., Rosenberg M. Try and try again: qualitative insights into adolescent smoking experimentation and notions of addiction. Health Promotion J. Austr. 2010;21(3):208–214. doi: 10.1071/he10208. [DOI] [PubMed] [Google Scholar]
- Lee K., Conigrave K.M., Clough A.R., Dobbins T.A., Jaragba M.J., Patton G.C. Five-year longitudinal study of cannabis users in three remote aboriginal communities in Arnhem Land, Northern territory, Australia. Drug Alcohol Rev. 2009;28(6):623–630. doi: 10.1111/j.1465-3362.2009.00067.x. [DOI] [PubMed] [Google Scholar]
- Li M.D., Burmeister M. New insights into the genetics of addiction. Nat. Rev. Genet. 2009;10(4):225. doi: 10.1038/nrg2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long A.F., Godfrey M., Randall T., Brettle A.J., Grant M.J. Nuffield Institute for Health; Leeds: 2002. Developing Evidence Based Social Care Policy and Practice. Part 3: Feasibility of Undertaking Systematic Reviews in Social Care. [Google Scholar]
- Lovett R., Thurber K.A., Wright A., Maddox R., Banks E. Deadly progress: changes in Australian Aboriginal and Torres Strait Islander adult daily smoking, 2004–2015. Public Health Res. Pract. 2017;27(5) doi: 10.17061/phrp2751742. [DOI] [PubMed] [Google Scholar]
- Lovett R., Banks E., Brown N., D'Este C.A., Du W., Dunbar T. National Health and Medical Research Council; Australia: 2017. Understanding the Connections between Aboriginal and Torres Strait Islander Culture, Health and Wellbeing to Support Action to Improve Outcomes. [Google Scholar]
- MacLean S., Hengsen R., Stephens R. Critical considerations in responding to crystal methamphetamine use in Australian Aboriginal communities. Drug Alcohol Rev. 2017;36(4):502–508. doi: 10.1111/dar.12468. [DOI] [PubMed] [Google Scholar]
- Maddox R., Davey R., Lovett R., Cochrane T., van der Sterren A., Corbett J. The smoke ring: a mixed method study. Int. J. Health Wellness Soc.. 2015;5(2) [Google Scholar]
- Maksimovic L., Paquet C., Daniel M., Stewart H., Chong A., Lekkas P. Characterising the smoking status and quit smoking behaviour of Aboriginal health workers in South Australia. Int. J. Environ. Res. Public Health. 2013;10(12):7193–7206. doi: 10.3390/ijerph10127193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. Social determinants and the health of Indigenous Australians. Medical J. Austr. 2011;194(10):512–513. doi: 10.5694/j.1326-5377.2011.tb03086.x. [DOI] [PubMed] [Google Scholar]
- McHugh M.L. Interrater reliability: the kappa statistic. Biochem. Med. (Zagreb). 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- Midford, R., Stockwell, T., Gray, D., 2002. Prevention of alcohol-related harm: community-based interventions. In: Commonwealth Department of Health and Ageing (Ed.), National Alcohol Research Agenda. Canberra: Commonwealth Department of Health and Ageing, pp. 91–112.
- Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int. J. Evidence Based Healthcare. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- NACCHO Constitution for the national Aboriginal Community Controlled Health Organisation. Canberra: Natl. Aboriginal Commun. Controlled Health Organisation. 2001 [Google Scholar]
- Noble N.E., Paul C.L., Turner N., Blunden S.V., Oldmeadow C., Turon H.E. A cross-sectional survey and latent class analysis of the prevalence and clustering of health risk factors among people attending an Aboriginal Community Controlled Health Service. BMC Public Health. 2015;15:666. doi: 10.1186/s12889-015-2015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passey M.E., Gale J.T., Sanson-Fisher R.W. “It's almost expected”: rural Australian Aboriginal women's reflections on smoking initiation and maintenance: a qualitative study. BMC Women's Health. 2011;11:55. doi: 10.1186/1472-6874-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passey M.E., D'Este C.A., Stirling J.M., Sanson-Fisher R.W. Factors associated with antenatal smoking among Aboriginal and Torres Strait Islander women in two jurisdictions. Drug Alcohol Rev. 2012;31(5):608–616. doi: 10.1111/j.1465-3362.2012.00448.x. [DOI] [PubMed] [Google Scholar]
- Passey M.E., Sanson-Fisher R.W., D'Este C.A., Stirling J.M. Tobacco, alcohol and cannabis use during pregnancy: clustering of risks. Drug Alcohol Dependence. 2014;134:44–50. doi: 10.1016/j.drugalcdep.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Rutter H., Savona N., Glonti K., Bibby J., Cummins S., Finegood D.T. The need for a complex systems model of evidence for public health. Lancet. 2017;390(10112):2602–2604. doi: 10.1016/S0140-6736(17)31267-9. [DOI] [PubMed] [Google Scholar]
- Senior, K., Chenhall, R., Daniels, D., 2006. ‘Stuck nose': experiences and understanding of petrol sniffing in a remote Aboriginal community.
- Smirnov A., Kemp R., Ward J., Henderson S., Williams S., Dev A. Patterns of drug dependence in a Queensland (Australia) sample of Indigenous and non-Indigenous people who inject drugs. 2016;35(5):611–619. doi: 10.1111/dar.12392. [DOI] [PubMed] [Google Scholar]
- Snijder M., Stapinski L., Lees B., Newton N., Champion K., Champman C. Substance use prevention programs for indigenous adolescents in the United States of America, Canada, Australia and New Zealand: protocol for a systematic review. JMIR Res. Protocols. 2018;7(2) doi: 10.2196/resprot.9012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stearne, A., Wright, M., Shakeshaft, A., Symons, M., Allsop, S., UNDER REVIEW. Identifying how the principles of self-determination could be applied to create effective alcohol policy for First Nations Australians: synthesising the lessons from the development of general public policy. [DOI] [PubMed]
- Stone A.L., Becker L.G., Huber A.M., Catalano R.F. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Thomas D.P., Briggs V., Anderson I.P.S., Cunningham J. The social determinants of being an Indigenous non-smoker. Austr. New Zealand J. Public Health. 2008;32(2):110–116. doi: 10.1111/j.1753-6405.2008.00185.x. [DOI] [PubMed] [Google Scholar]
- Thrift A.P., Nancarrow H., Bauman A.E. Maternal smoking during pregnancy among Aboriginal women in New South Wales is linked to social gradient. Austr. New Zealand J. Public Health. 2011;35(4):337–342. doi: 10.1111/j.1753-6405.2011.00728.x. [DOI] [PubMed] [Google Scholar]
- Tsey K. The control factor: a neglected social determinant of health. Lancet. 2008;372(9650):1629. doi: 10.1016/S0140-6736(08)61678-5. [DOI] [PubMed] [Google Scholar]
- Tsourtos G., Ward P.R., Lawn S., Winefield A.H., Hersh D., Coveney J. Is resilience relevant to smoking abstinence for Indigenous Australians? Health Promot. Int. 2015;30(1):64–76. doi: 10.1093/heapro/dau087. [DOI] [PubMed] [Google Scholar]
- United Nations . United Nations; Geneva: 2018. World Drug Report 2018. [Google Scholar]
- Van der Sterre A., Knoche B. Tobacco use among aboriginal peoples and Torres Strait Islanders. In: Scollo M., Winstanley M., editors. Tobacco in Australia: Facts and issues. Cancer Council Victoria; Melbourne: 2012. [Google Scholar]
- Whiteford H.A., Degenhardt L., Rehm J., Baxter A.J., Ferrari A.J., Erskine H.E. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Wood, L., France, K., Hunt, K., Eades, S., Slack-Smith, L., 2008. Indigenous women and smoking during pregnancy: Knowledge, cultural contexts and barriers to cessation. [DOI] [PubMed]
- World Health Organization . WHO Press; Geneva, Switzerland: 2009. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.