Abstract
Corona virus disease 2019 (COVID-19) outbreak has become a severe community health threat across the world. Covid-19 is a major illness, presently there is no as such any medicine and vaccine those can claim for complete treatment. It is spreading particularly in a feeble immune people and casualties are expanding abruptly and put the health system under strain. Among the strategic measures face mask is one of the most used measures to prevent spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Wearing a face mask possibly create a false sense of security lead to decline others measures. Face mask could be risk for the people of under lying medical conditions, old age group, outdoor exercise, acute and chronic respiratory disorders and feeble innate immune. Restrictive airflow due to face mask is the main cause of retention of CO2 called hypercapnia that can lead to respiratory failure with symptoms of tachycardia, flushed skin, dizziness, papilledema, seizure and depression. According to latest updates face shield and social distancing could be better substitute of face mask.
Keywords: SARS-CoV-2, Face mask, Hypoventilation, Hypercapnia, COPD
1. Introduction
Corona virus disease 2019 (COVID-19) outbreak has been emerged as a serious global public health threat. COVID-19 is an infectious pandemic outbreak caused by SARS-CoV-2 and this novel strain of SARS-CoV-2 belongs to same family of coronaviruses those are responsible for SARS-CoV and MERS-CoV (Rasmussen et al., 2020, Chan et al., 2020, Wahab et al., 2020, Wahab et al., 2020). The cases are still rising in haste across the world and infected 235 countries, areas or territories estimated with approximately over 35.35 million people infected with 1.03 million deaths. United States America has highest number of cases 7,341,406 among the all nations with the highest total death 208,433 according to WHO report on October 6, 2020. As of October 6, 2020, cases from WHO region reported 6,337,772 in Europe, 17,176,705 in Americas, 2,503,734 in Eastern Mediterranean, 633,080 in Western Pacific, 7,488,605 in South East Asia and 1,206,767 in Africa (WHO, 2020).
Cascella et al., stated strategic measures for COVID-19 prevention in health personnel aspects of patient isolation and infection control that include steps to be measured during the diagnosis and care of infected patient, contact, droplet, blood and precaution should be adopted during specimen collection and induction (Cascella et al., 2020). Different modes of transmission are investigated including contact, droplet, airborne, fomite, fecal-oral, blood borne, mother to child and animal to human. Among them contact and droplet, airborne, fomite transmissions are considered to be major contributors for the spread of COVID-19. Moreover, the fecal-oral transmission is a potential source due to the presence of viral RNA in stool (Perisetti et al., 2020a). A number of studies uncovered the potential of the fecal-oral route of transmission of SARS-CoV-2. A pooled prevalence of 48.1% for stool RNA positivity was obtained after review of 12 studies (Perisetti et al., 2020b). Other factors too may be responsible for stool RNA positivity. As per the report of Ling et al., 82% of the patients had persistent stool RNA positivity even after viral respiratory clearance. The fecal-oral transmission of COVID-19 may be considered for the cause of diarrhea in the community (Ling et al., 2020). Among the COVID-19 patients diarrhea is found to be commonly noted GI symptoms. A number studies were performed to investigate the prevalence of diarrhea. Accordingly, the result of prevalence of diarrhea was found to be 5–10% (Sultan et al., 2020, Cheung et al., 2020), 2–50% (D’Amico et al., 2020), 22.1% (Hajifathalian et al., 2020) and 36.6% from different studies performed elsewhere. It is not clear factor play key role in causing the diarrhea in COVID-19 patients (Perisetti et al., 2020, Perisetti et al., 2020).
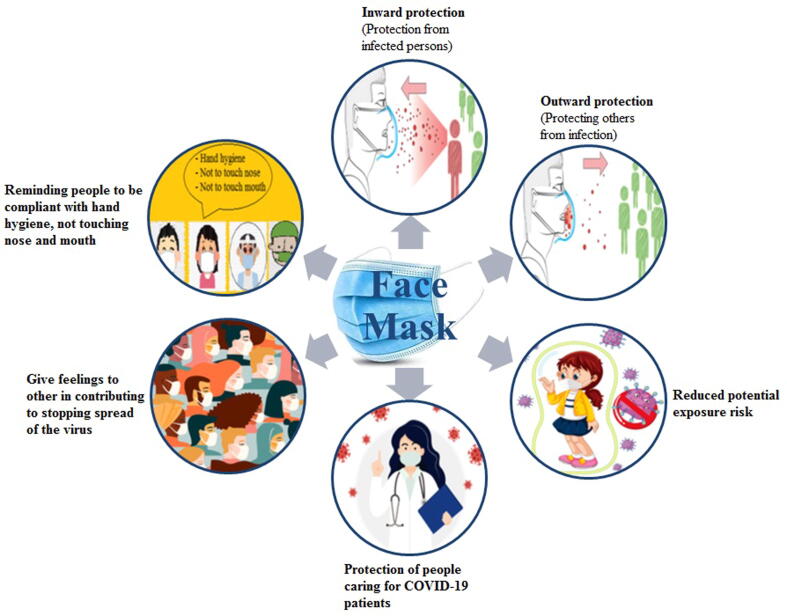
The significant measures for the public to clean hands subsequent to non living and living contacts, use sanitizers, face mask, social distancing etc. Among the various measures applied by the people face mask play an important role to control the spread of SARS-CoV-2 through protecting from infected persons and protecting others from infection and reduce the risk of exposure (Fig. 1) ( Siddiqui et al., 2020a). Despite the fact that strategic measures of face mask exhibits false sense of security and may lead to death in specific group of the people.
Fig. 1.
Contribution of face mask in control and prevention of severe acute respiratory syndrome coronavirus (SARS-CoV-2) in the community people and health personnel.
2. Rationale
Introduction of mouth and nose coverage by using face mask can be traced back to the 20th century (Matuschek et al., 2020). Historically, face mask had been a part of traditional sanitary practices against contagious diseases in early modern Europe. Face masks used in today health care system and in the community can be seen as preventative measure to mitigate or prevent the spread of infectious disease such as COVID-19. Earlier report suggests that, many of these non-pharmaceutical measures likewise face mask had been used for the control of community transmission of severe acute respiratory syndrome (SARS) in 2003 and pandemic influenza A H1N1 in 2009 in Hong Kong and other parts of the world (Cheng et al., 2020). Since the outbreak of SARS-CoV-2, the use of face masks has become ubiquitous around the world and it has become an important health measure or we can say as become a new normal after COVID-19 pandemic (Feng et al., 2020). Al-though, several recommendations as well as usage guidelines have been made available by World Health Organization (WHO), Centers for Disease Control and Prevention (CDC) and other health agencies to prevent transmission of air droplets by holding it back. In addition, despite of various fact sheet or technical report available regarding the face mask, its usage in healthy population is still controversial (Cheng et al., 2020). Subsequently according to our literature survey, we observed that, a lot of information published discussing majorly the benefits of face mask rather than its drawback while worn for longer duration. We found that, there is several other health aspect associated with face mask, which need to address in this current pandemic.
Various studies have been conducted on face mask, studies were individually evaluated for their reporting and methodological quality using methods described in the Table 1. It is worthy of evaluating above all 11 studies examined the effectiveness and efficacy of face masks in Hajj setting. One investigation is related to students on or off-campus. In the clinical trials, faces mask to be the best performing intervention as compared to other physical non-pharmaceutical intervention across different populations and settings. Wearing a face mask was actually associated with greater likelihood of respiratory illness. This finding is consistent with previous findings that face masks either offered no significant protection or were associated with sore throat and with longer duration of sore throat and fever symptoms. The efectiveness of face mask in source control hinges on the specific mode of transmission of etiological agent. The results from these types of studies could then be used to develop evidence based interventions to help prepare for future pandemics.
Table 1.
Various studies on effectiveness and efficacy of face masks.
| Participants | Interventions | Comparisons | outcomes | Study design | References |
|---|---|---|---|---|---|
| 1437 young adults living in university residence halls during the 2006–2007 | Residence halls were randomly assigned to 1 of 3 groups—face mask use, face masks with hand hygiene, or control— for 6 weeks. Generalized models estimated rate ratios for clinically diagnosed or survey-reported influenza like illness (ILI) weekly and cumulatively. | We observed significant reductions in ILI during weeks 4–6 in the mask and hand hygiene group, compared with the control group, ranging from 35% (confidence interval [CI], 9%–53%) to 51% (CI, 13%–73%), after adjusting for vaccination and other covariates. | These findings suggest that face masks and hand hygiene may reduce respiratory illnesses in shared living settings and mitigate the impact of the influenza A(H1N1) pandemic. | Residence halls were randomly assigned to 1 of 3 groups—face mask use, face masks with hand hygiene, or control— for 6 weeks. Generalized models estimated rate ratios for clinically diagnosed or survey-reported ILI weekly and cumulatively. | ClinicalTrials.gov identifier: NCT00490633. (Aiello et al., 2010) |
| NPIs in households with a febrile, influenza-positive child. Households. | Study nurses conducted home visits within 24 h of enrollment and on days 3, 7, and 21. Respiratory swabs and serum were collected from all household members and tested for influenza by RT-PCR or serology | Influenza transmission was not reduced by interventions to promote hand washing and face mask use. | This may be attributable to transmission that occurred before the intervention, poor facemask compliance, little difference in hand-washing frequency between study groups. | Respiratory swabs and serum were collected from all household members and tested for influenza by RT-PCR or serology. | (Simmerman et al., 2011) |
| 1,178 young adults living in 37 residence houses in 5 university residence halls during the 2007–2008 influenza season. | Discrete-time survival models using generalized estimating equations to estimate intervention effects on ILI and confirmed influenza A/B infection over a 6-week study period were examined. | A significant reduction in the rate of ILI was observed in weeks 3 through 6 of the study, with a maximum reduction of 75% during the final study week (rate ratio [RR] = 0.25, [95% CI, 0.07 to 0.87]). Both intervention groups compared to the control showed cumulative reductions in rates of influenza over the study period, although results could not reach to statistical significance. | Face masks and hand hygiene combined may reduce the rate of ILI and confirmed influenza in community settings. These non-pharmaceutical measures should be recommended in crowded settings at the start of an influenza pandemic. | Participants were assigned to face mask and hand hygiene, face mask only, or control group during the study. | Clinicaltrials.gov NCT00490633 (Aiello et al., 2012) |
| Australian pilgrims of attending Haj | Tents were randomised to 'supervised mask use' versus 'no supervised mask use'. Pilgrims with ILI symptoms for>3 days were recruited as 'cases' and those who slept within 2 m of them as 'contacts' | Mask use compliance was 76% in the 'mask' group and 12% in the 'control' group. Based on developing syndromic ILI, less contacts became symptomatic in the 'mask' tents compared to the 'control' tents (31% versus 53%, p = 0.04) | This pilot study shows that a large trial to assess the effectiveness of facemasks use at Hajj is feasible | Pilot study, The Hajj pilgrimage, where the incidence of influenza and other respiratory infections is high, provides an excellent opportunity to test the effectiveness of facemasks against syndromic and laboratory-confirmed infections | (Barasheed et al., 2014) |
| Malaysian Hajj pilgrims | A total of 387 survey forms were available for analysis. The mean age was 50.4 +/- 11.0 years. | Malaysian Hajj pilgrims were: cough 91.5%, runny nose 79.3%, fever 59.2%, and sore throat 57.1%. The prevalence of Hajj pilgrims with triad of cough, subjective fever, and sore throat were 40.1%. The symptoms lasted<2 weeks in the majority of cases. Only 3.6% did not suffer from any of these symptoms | The prevalence of respiratory symptoms was high among Malaysian Hajj pilgrims | A cross-sectional study was conducted by distributing survey forms to Malaysian Hajj pilgrims at transit center before flying back to Malaysia. | (Deris et al., 2010) |
| 405 Hajj pilgrims | Pilgrims were administered a post-travel questionnaire by telephone that addressed compliance with preventive measures against respiratory infections and the occurrence of disease during their 4-week stay in Saudi Arabia | A total of 165 (60.2%) individuals presented with at least one health problem during their stay in Saudi Arabia, including cough (48.5% of all pilgrims), sore throat (36.1%),rhinorrhea (23.7%), sputum (13.5%), shortness of breath (2.9%), voice failure (2.9%), subjective fever(10.9%), myalgia (9.5%), gastrointestinal symptoms(9.5%), conjunctivitis (0.4%) and Influenza like illness | Results suggest that vaccination against influenza and the use of surgical facemasks were not efficient against respiratory infections | Pre and post travel questionnaire | (Gautret et al., 2011) |
| 1507 Hajjis | A cross-sectional study during November and December 2009 among Hajjis registered while visiting Primary Health Care Centers of Riyadh, Kingdom of Saudi Arabia to get mandatory meningococcal meningitis vaccination. On return from Hajj, Hajjis were contacted on telephone to collect information on occurrence of URTI and diarrhea along with other associated activities in Hajj. | Out of 1507 Hajjis, 54.7% developed symptoms, 97% reported upper respiratory tract symptoms, and 9.3% reported diarrheal symptoms. People < 40 years of age were more likely to develop URTI. | Upper respiratory tract infections is a common health problem among studied domestic Hajjis. Generally, there is room for improvement in the adoption of preventive measures by Hajjis; and there is still limited information on the use of facemasks in spite of the fact that using it significantly decreases the risk for URTI. | A cross-sectional study | (Saeed et al., 2012) |
| 186 US Hajjis | Surveys assessed demographics, knowledge, attitudes, and practices (KAP) related to influenza A(H1N1), vaccination, health seeking behaviors, sources of health information, protective behaviors during the Hajj, and respiratory illness | In contrast to other studies that have found protective effects of face masks at Hajj. Evidence for the efficacy of face masks for preventing the transmission of influenza is limited. The protective practices and respiratory illness among US travelers to the 2009 Hajjis study of influenza transmission suggests that poor face mask compliance decreases their utility in mitigating the spread of disease. | Pre and post travel surveys were completed by 186 participants. Respiratory illness was reported by 76 (41.3%) respondents; 144 (77.4%) reported engaging in recommended protective behaviors during the Hajj. Reduced risk of respiratory illness was associated with practicing social distancing, hand hygiene, and contact avoidance. of respiratory illness. | Survey | (Balaban et al., 2012) |
| 7448 school-aged children in South Korea | Investigation of epidemiological factors related to H1N1 infection in school-aged children | H1N1 infection was associated with body mass index (BMI), waist circumference (WC), the use of facemasks, contact history with H1N1-infected persons, and overseas travel history (P < 0·05) | Providing education on wearing facemasks and specific planning for abdominally obese children and adolescents may be effective means of reducing the spread of the influenza pandemic in school-aged children | This study analyzed data collected from the participants. | (Kim et al., 2012) |
| 119 French Hajj pilgrims. | Clinical follow-up, adherence to preventive measures and PCR-based pharyngeal bacterial carriage pre- and post-Hajj | The prevalence of S. pneumoniae carriage (1.8% pre-, 9.8% post-Hajj), H. influenzae carriage (0.9%, 45.4%) and K. pneumoniae (2.8%, 9.8%) significantly increased post-Hajj. | Majority of pilgrims used facemasks at least sometimes during their stay in Saudi Arabia, only 14.3% used masks frequently and less than half reported compliance with frequent hand washing | Cohort study | (Hoang et al., 2019 |
| Malaysian hajj pilgrims of 2013 | A self-administered proforma on social demographics, previous experience of hajj or umrah, smoking habits, co-morbid illness and practices of preventive measures against respiratory illness were to obtain. | Only 31.8% of them practiced good hand hygiene, ~82.9% of pilgrims used surgical face masks, N95 face masks, dry towels, wet towels or veils as their face masks. Nearly one-half of the respondents (44.4%) took vitamins as their food supplement. Malaysian hajj pilgrims with previous experience of hajj (OR 0.24; 95% CI 0.10–0.56) or umrah | All preventive measures which include hand hygiene, wearing face masks and influenza vaccination must be practiced together as bundle of care to reduce respiratory illness effectively | A cross-sectional study | (Hashim et al., 2016) |
3. Pre-to post COVID-19 face mask compliance scenario
Yang et al., 2011 carried a study during the year 2007–2008 to see the compliance rate of face mask on 400 HCWs and they found that only 70% were in compliant of wearing mask while in contact with patients (Yang et al., 2011). A single-center, cross-sectional study performed by McGaw et al., during the March and May 2009 on total 132 HCWs. They reported that face mask and safety goggles were 87%, and 56% respectively (McGaw et al., 2012). One of the studies conducted on nurses (n-1074) to see the compliance of PPE and they reported that only 44% nurses were adhering to the recommended uses of PPE (Nichol et al., 2013). Chughtai et al., suggested both medical and cloth masks were in use during the 4 weeks of their study and reported that medical mask used were 77% (Chughtai et al., 2016). Similarly, Haile et al., reported that HCWs were following standard precaution while in the hospital setting was 12% (Haile et al., 2017). Based upon the above mentioned pre-covid-19 face mask and safety goggles compliance rate, we can say it actually varied from the region to region so it becomes very difficult to say a particular compliance rate.
However, since the declaration of COVID-19 outbreak on March 11, 2020, a global pandemic from the WHO there has been seen a sharp surge in the usage of facemask by the healthcare work as well as the mass populations. Several studies have been carried out by various authors to show the real representation of compliance rate for facemask and safety goggle during the current pandemic. Picard et al observed that wearing of face mask in HCWs showed a data published in the media during the pandemic and conformed to show good practice guidelines in 70.8% of the photographs collected on some of the main French information websites (Picard et al., 2020). Parkash et al., conducted a study on compliance and perception about personal protective equipments among health care workers involved in the surgery during COVID-19 pandemic. They found that overall compliance for PPE usage was 96.3% (Prakash et al., 2020, Purushothaman et al., 2020). Sarfarz et al., performed a survey study in hospital setting with 397 participants and thye found that the overall compliance with face mask was 90.4% (Sarfraz et al., 2020). In addition, Alhassan et al., performed a cross sectional study to see the facemask compliance among the HCWs and they found that facemask compliance was proportionally higher 85.0% among nurses followed by physician (50.0%). Majority (94.9%) of the respondents reported facemask use during procedures likely to generate splashes. (Alhassan et al., 2020). Earlier reports suggest that, HCWs had good knowledge (69%) and compliance (68%) with Covid19 control (Amanya et al., 2020). Tripathi et al., revealed a study on 1000 participants, they presented that 86.5% respondent were wearing the face mask Tripathi et al., 2020). Moreover, major non-compliance of face mask and other personnel protective equipment (PPE) were reported due to following reason such as unavailability, uncomfortable while operating, poor visibility, fogging while operating, re-use compromises, can’t wear along with other PPE, prefer to use goggles over other PPE other difficulty includes breathing on exertion, acne, itchy nose, difficulty breathing, discomfort, allergy and pain (Prakash et al., 2020, Purushothaman et al., 2020). Overall, these findings suggest that post COVID-19 declaration; the use of PPE or face mask in particular has increased which is seen as important non pharmaceutical tools to mitigate the COVID-19 pandemic among the health workers as well as in mass population. However, these findings suggest that there are still opportunities for improvement in rates of public face mask use and a potential decrease in the spread of COVID-19 in our population.
4. A pleiotropic approach of face mask in the prevention of SARS-CoV-2 spread
Covid-19 is a severe disease which does not currently have a known cure or vaccine. It is a contagious infection which can be transmitted through respiratory droplets. Deaths are rapidly raising and there is a continuous strain on health care systems. To slow the spread of deadly SARS-CoV-2 policymakers as a precautionary principle have highly recommended wearing face mask along with other social distancing steps (Greenhalgh et al., 2020, Siddiqui et al., 2020). WHO recognizes that the wearing of masks by populace exhibits remarkable effects in severe pandemics as a single partial preventive measure may have a substantial impact on the transmission of infection (Organization, 2019).
The most important benefit of wearing a mask is the person can limit the spread of the virus to others if someone knows or doesn’t know about their infection, especially the asymptomatic person. Although the most effective way to avoid the spread of COVID-19 infections is to take proper hand hygiene steps and to maintain physical distancing but wearing a mask in public may restrict the transmission of COVID-19 by individuals who have the virus. The United States Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) from the beginning integrated face masks into their guidelines to minimise virus transmission. The face mask is very crucial to cover the face, especially in the areas where other social distancing steps are hard to hold (Desai and Aronoff, 2020). CDC initially encourages the face mask use during the pandemic later on the advice was updated that nose and mouth covering with only cloth face cover when in public can prevent others from infection. But coving the face with cloth cover doesn’t mean that one can forget social distancing. CDC guidelines suggest fabric face masks to the public rather than the surgical and N95 masks that healthcare professionals use (How to Protect Yourself & Others | CDC, 2020). However, it was found that there is no claim that the mask is competent enough to spread the transmission of the virus, but carrying a mask could make someone feel safer and remind of a preventive measure.
There are several reasons to wear a face mask. Firstly it reduces 95% of the respiration that transmits the virus in an area up to 6 feet away, and it minimizes oral/fecal transmission by preventing the virus from getting into persons nose or mouth if the personal touch the infected surface and then their face. Masks, therefore, encourage us to continue to practice physical distancing. Mask reminds people to be compliant with hand hygiene and not to touch the nose and mouth. Mask provides feeling to others in contributing to stopping the further spread and most importantly mask gives protection to front line workers caring for COVID-19 patients. Infants younger than two years should not wear masks, and people who cannot become unaware of a mask by themselves (Why Face Masks Are Crucial, 2020). In the studies, it was found that the SARS-CoV-2 is viable in the air for several hours under experimental conditions in aerosol emission, but surgical masks appear to block aerosols in such laboratory experiments (Van Doremalen et al., 2020, Leung et al., 2020, Leung et al., 2020) that strongly supports public wearing masks during the COVID-19 pandemic. Presymptomatic individuals tend to be responsible for around 50 percent of infections (Ganyani et al., 2020), so a marginal decrease in community transmission with mask might make a big difference. Such essential preventive steps may be used to monitor the demand for hospital bed spaces and ventilation systems. Face mask guidelines vary across countries. Many countries enforced compulsory face mask regulations in public places and releases recommendations on face mask use in community settings that are listed in Table 2 (Feng et al., 2020).
Table 2.
Recommendations on the use of face mask in various countries in community settings during covid-19 pandemic.
| Country | Recommendations | References |
|---|---|---|
| Japan |
|
(Q&A about the new coronaviru, 2020) |
| Germany |
|
(Coronavirus: Germany′s new face mask regulations, 2020) |
| China |
|
(The state council’s joint prevention and control mechanism, 2020) |
| UK |
|
(Hutchings, 2020) |
| Saudi Arabia |
|
(MOH, 2020) |
| India |
|
(Guidelines on use of masks, 2020) |
| Hong Kong |
|
(Guidelines on Prevention of Coronavirus Disease, 2019, Guidelines on use of masks, 2020) |
| USA |
|
(How to Protect Yourself & Others | CDC, 2020) |
| UAE |
|
(Gulf News, 2020) |
| Singapore |
|
(Ministry of health, Singapore updates on COVID-19) |
5. Efficacy and infiltrating capability of face mask
There is lack of direct evidences from published data or randomized controlled trials (RCT) on the use of masks as source control for SARS-CoV-2. Efficacy of surgical masks against influenza, rhinovirus as well as seasonal coronavirus was studied and it was reported that mask has significant role in source control for the seasonal coronavirus droplets of all sizes but found less effective at blocking small influenza droplets and of blocking rhinovirus droplets of any size (Leung et al., 2020, Leung et al., 2020). So, efficacy of mask on current SARS-CoV-2 is not yet clearly known. Vander et al. reported that almost all kind of mask may decrease viral exposure and risk of infection on population regardless of unfitness and poor adherence (Vander et al., 2008). A case report of china regarding the efficacy of mask on controlled setting of airplane passengers was published. A person onboard was later on found positive for COVID-19 but during the flight from China to Toronto he was wearing the mask and when nearby close seated 25 other passengers along with flight attendants were tested they all found negative (Schwartz et al., 2020).
Filtering capability of masks depends upon different types of mask, as mask could be made of the various designs and materials. A typical droplet size is 5 μm–10 μm while the particle sizes for speech are on the order of 1 μm (Howard et al., 2020). Surgical mask are also known as medical mask which have better bacteria filtration and air permeability and can protect from contact with droplets and splashes by reducing exposure to the saliva and respiratory secretions. A surgical mask also filters out large particles in the air and should only be used once. N95 mask provides more safety and security than a surgical mask. Surgical N95 respirators are most widely used as personal protective equipment in health care environments such as hospitals among healthcare professionals. When the person who wears, inhales, it can filter out the big and small both kind of particles. An N95 mask may block 95% of very small particles and when wearer breathes out, it releases unfiltered air (Gulf News, 2020, COVID-19: How much protection do face masks offer?, 2020). Various characteristics of face mask can be seen Table 3.
Table 3.
Different types of face masks with their characteristic, advantage and disadvantage.
| S.N. | Types | Characteristics | Advantages | Disadvantages | References |
|---|---|---|---|---|---|
| 1 | Filtering face piece (FFP) Respirator masks |
|
|
|
(Jefferson et al., 2009; Nikiforuk et al., 2017, Leung et al., 2020, Leung et al., 2020, Cheung et al., 2020) |
| FFP 1 |
|
|
|
(Jefferson et al., 2009; Nikiforuk et al., 2017, Leung et al., 2020, Leung et al., 2020) | |
| FFP2-N95 respirator |
|
|
|
(Leung et al., 2020, Leung et al., 2020, Leung et al., 2020) | |
| FFP3-N100/N99/P100/P100 respirator/gas mask |
|
|
|
(Rodriguez et al., 2020) | |
| 2 | Medical mouth–nose protection (MNP) Surgical Mask |
|
|
|
(Leung et al., 2020, Leung et al., 2020; Burnettet et al., 2020; Mansour et al., 2009) |
| 3 | Non-medical mask(NMM)Cloth face mask |
|
|
|
Davies et al., 2013, Konda et al., 2020,Sharma et al., 2020) |
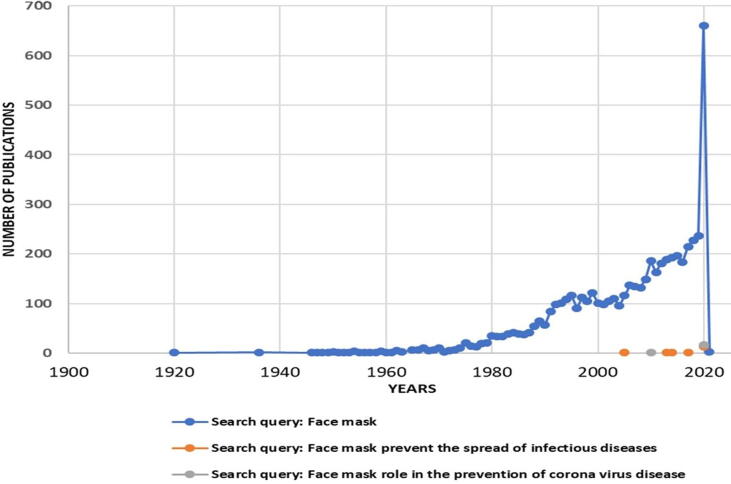
A cloth mask is intended to capture droplets emitted while the user is talking, coughing, or sneezing. Studies reported filtration efficacy of cloth mask as compared to surgical mask. Cloth mask made up of household materials had filtration rate between 49% and 86% for 0.02 μm exhaled particles while surgical masks filtered 89% of those type particles (Davies et al., 2013). Data suggest that a surgical mask was found to filtered 75% of particles between 0.02 μm to 1 μm on the other hand the cloth mask was found to filter 60% (Van der Sande et al., 2008). Overall, it was concluded face mask exhibit significant role to prevent the speared of SARS-CoV-2. A detailed discussion of the fascinating world of face masks in the current scenario is needed, which requires an extensive and overwhelming literature survey. The main focus of this review article is on various aspects of the face mask. The search for the word “Face mask” the phrases “Face mask prevent the spread of infectious diseases” and “Face mask role in the prevention of corona virus disease” PubMed database reveals a growing trend in the number of the published articles, especially a rapid rise in publications from 2019 onward. It was concluded that research on face mask is desperately needed to know the veracity in community health. The search results are depicted in Fig. 2 illustrates a global trend in the number of published works on the Face masks from 1920 to 2020.
Fig. 2.
Graphically represented statistical data of number of publications in PubMed from 1900 to 2020. Publications in PubMed by using search bar for searching keywords/phrases: (1) Face mask (blue); (2) Face mask prevent the spread of infectious diseases (orange) and (3) Face mask role in the prevention of corona virus disease (grey). Moving average trend lines show the importance and urgent need for research concerning the development of face mask in present scenario of COVID-19.
6. Factual facts of face mask
According Belgium’s Federal Public Service for Health use of face mask to prevent infection of coronavirus barely creates sense in hospitals where coronavirus patients are treated and patients specimens are tested (Lifesaver or false protection, 2020). Beijing’s Centre for Disease Control and Prevention (CDC) in its guidelines confirmed people can go outdoors without wearing mask to confirm COVID-19 outbreak is under control. CDC also guided that residents must have to compliance rules of social distancing (China: CDC issues new guidelines, 2020).
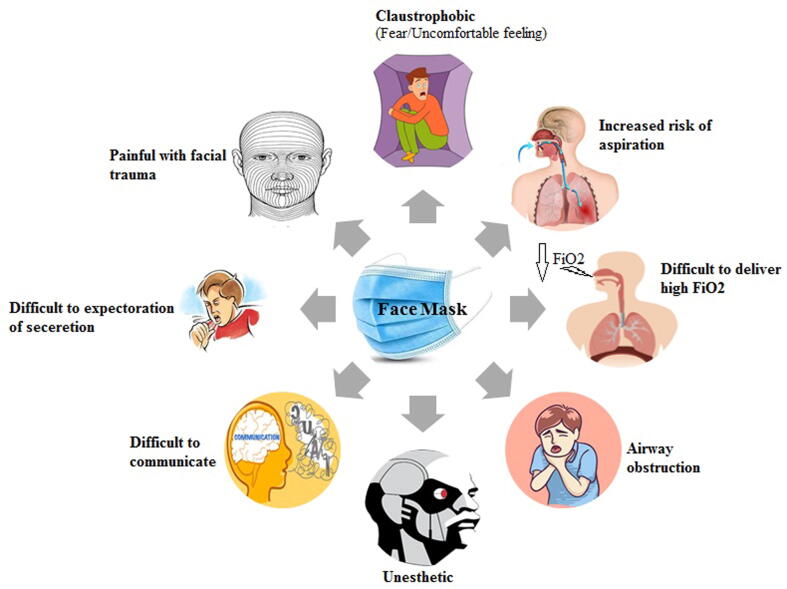
Wearing a face mask may possibly provide a false sense of safety and lead to decline social distancing and hands washing compliance (Greenhalgh et al., 2020). Face mask wearers get irritation and feel awkward that lead to touch and adjust mask repeatedly. This irritation leads to infect face, ears and eyes. Exhaled air with wearing face mask get into eyes contact that leads to uneasiness and makes an impulse to finger the eyes, nose and face that could be a cause of infection. Speech of volume and quality gets hampered owing to wearing face mask that lead to involuntarily make closer to each other consequently people be inclined to noncompliance of social distancing. Most of us are new face mask users, so level of mask safety could not achieve by all of us and it leads to noncompliance aspects of its use, reuse and dispose consequentially chances of infections will increase. Wearers have long nose or face deformities cannot fix mask accurate manner and may cause of infection from SARS-CoV-2 and other microbial pathogens. People ignorance and lack of knowledge how to wear face mask may be cause of infect themselves and infect to others. It is the need of the hour to get proper training under the supervision of expert in each and every concern to maintain hygiene and achieve the optimum benefits of face mask. Complications with face mask can be seen in Fig. 3.
Fig. 3.
Complications with face mask lead to increase risk of aspiration, difficult to deliver fraction of inspired oxygen (FiO2), painful facial trauma, difficult to expectoration of secretion, difficult to communicate, claustrophobic etc.
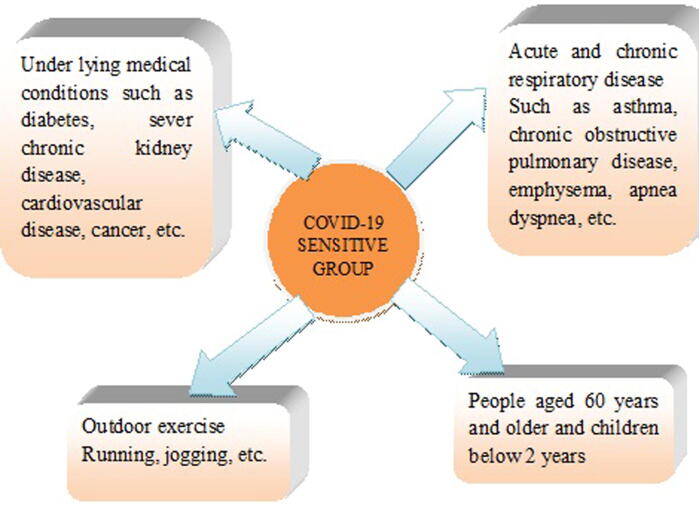
7. Face mask induced risk populace and allied health impediments
According to WHO SARS-CoV-2 infects all age groups. Nevertheless, proofs suggest that 2 category of people are vulnerable to COVID-19 infection disease. They are under lying medical conditions that include chronic respiratory disease, diabetes, cardiovascular disease and cancer and other category are over 60 year old age people (Fig. 4). The possibility of severe disease steadily rises with time starting from approximately 40 years. Face mask is used to protect from infections but it is not advisable to sensitive illness group such as chronic obstructive pulmonary disease (COPD), acute and chronic respiratory infection, asthma, apnea and dyspnea etc. (Patel and Majmundar, 2018). Patients exhibit clinical manifestations primarily related to the pulmonary system that include dyspnea, cough with sputum production, fatigue and in severe cases, ARDS, respiratory failure. COVID-19 patients were found to exhibit extra pulmonary clinical manifestations including affect multiple other organs and organ systems including gastrointestinal, ocular, hepatic, cardiovascular, renal, dermatologic, and neurological systems (Johnson et al., 2020, Ramachandran et al., 2020). Furthermore, the vulnerability to infection is not same for male and female patients. Due to the elevated level of estrogen, females are investigated to be at lower risk of severity and mortality than male COVID-19 patients. Similarly, the different ethnic groups are found to have different infectivity and mortality. Due to a higher prevalence of diabetes, obesity, hypertension, asthma and heart rate in minority groups, African American and Hispanic communities have revealed increased rates of infection and hospitalization compared to Caucasian populations (Kopel et al., 2020).
Fig. 4.
Face mask wearers under risk specially old age, children, acute and chronic respiratory disease, outdoor exercise and underlying medical condition.
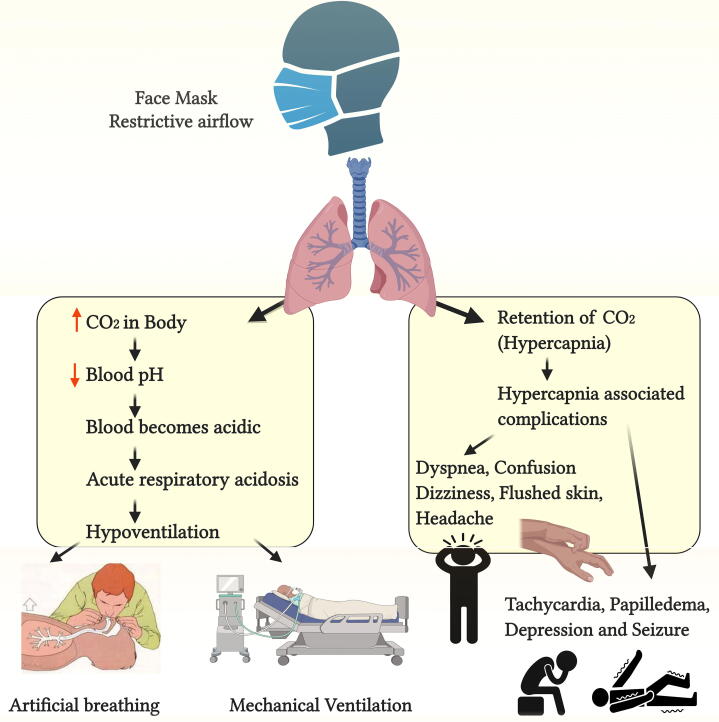
In Current covid-19 pandemic outbreak US Centers for Disease Control and Prevention recommended some guidelines regarding wearing face masks. Everybody should use a cloth face cover in public place but it should be avoided to be applied on children who are below 2 years or someone who has breathing difficulties, incapacitated or incapable to remove face mask without others assistance (How to Protect Yourself & Others | CDC, 2020). Restrictive airflow owing to face mask is the main reason for secondary complications that may cause of retention of CO2 is called hypercapnia. Furthermore, complications associated with hypercapnia include tachycardia, dyspnea, confusion, flushed skin, dizziness, and headache. Severe hypercapnia can lead to respiratory failure with symptoms of papilledema, seizure and depression (Patel and Majmundar, 2018). COPD patients wearing mask may lead to hypercapnia and they should be monitored by medical practitioners to avoid critical illness. Restrictive airflow due to face mask creates high concentration of CO2 in body in sensitive groups that exhibits fatal reaction by decreasing pH and leading to respiratory acidosis. The important issue is that CO2 regulates blood pH and high concentration CO2 in blood makes blood acidic and law concentration makes alkaline both conditions either acidic or alkaline could lead to health hazards (Fig. 5). Overall, it is concluded that it is better to avoid face mask and maintain social distancing and other measures particularly to sensitive group (Diaz Milian et al., 2019).
Fig. 5.
Restrictive airflow due to face mask may lead to hypercapnia and hypercapnia associated secondary complications include tachycardia, dyspnea, confusion, flushed skin, dizziness and headache, and severe hypercapnia can lead to respiratory failure with symptoms of depression, papilledema and seizure.
The innate immune comprises a rapid response mechanism of first line barrier to avert microbial invasion. The major use of the innate immune reaction is to instantly prevent the spread of foreign pathogens in the body (Chen et al., 2018). Efficacy of innate immunity is depending on load of virus. Humidity accumulates inside mask due to restricted air flow that is favourable condition for SARS-CoV-2 survival. Particularly children and infant discharge nasal fluid frequently and have lack of sense to maintain hygiene. Hence, children and infant should be monitored by parents and caretakers to avoid moisture and humidity inside face mask by nasal and mouth discharges. That could be the reason of increase viral load or other contamination. Consequentially, viral load and possibility of infection increase and innate immunity decreases in mask wearing people. Present pandemic COVID-19 infection direct depending on immune system of individual. As a consequence, the most of the old age people and underlying health conditions people are more susceptible for SARS-CoV-2 infection. Face mask and gloves sometimes misguide the people that they are fully protected. Wearers believe face mask is enough to protect from infection and with gloved hand touch their body and face while the efficacy of innate immunity reveals on skin surface rather than gloves. Consequentially, people leave the habits of hand sanitization and increases chances of exposure.
There should be proper precaution particularly at the time of exercise with mask. Restriction of air flow is common during physical activity or exercise. It has been observed exercise with face mask lead to disturb the equilibrium of oxygen and carbon dioxide exchange. Use of face mask continuously for a long period of time during exercise may affect supply of oxygen throughout the body and people may suffer from hypoxia. People with asthma, hypoxia and high blood pressure, and others underlying health conditions must take advice from healthcare practitioners regarding the use of face mask during physical exercise (Patel and Majmundar, 2018, Diaz Milian et al., 2019).
The Sun UK news paper reported that 26 years old jogger died due to running 2 miles with face mask in Wuhan, China. After surgery doctors confirmed collapsed lung was the reason for death and revealed that the runner left lung was compressed by 90%. Moreover, it was also reported that in Hunan province of China 14 years old two boys died due to abruptly collapsed. They were running in school track during physical education class with face mask. According to death certificate reason for death was sudden cardiac arrest (China: CDC issues new guidelines, 2020).
8. A novel approach for alternate of face mask
United States Health care Infection Control Practices Advisory Committee (HICPAC) suggests to health professionals that face and eyes should be fully protected throughout the patient care procedures. Fluids sprays and splashes comprise infectious pathogens that could affect heath care personnel. These fluids droplets can be adhered to mouth, eyes, nose mucous membrane and broken skin surface consequentially patient handlers may get infected. The present HICPAC guidelines clearly recommend wearing face shield during handling patients particularly for SARS-CoV-2 and avian influenza (Siegel et al., 2007). It has been seen in in vitro study that cloth mask may cause of filtration of natural and anthropogenic aerosols that could be virus and same size of aerosol particles. Face shield decreased 96% instant exposure of virus in simulated health worker in a simulation study. Same study with physical distancing decreased inhaled virus by 92%. (Lindsley et al., 2014, Perencevich et al., 2020). Face shields exhibit several benefits over face mask. They can be repeatedly use by cleaning them with disinfectants, soap and detergents. Face shield cover complete face, so exposure of infection through nose, mouth and eyes will be reduced. To get entire efficacy, clinical trials should be conducted on broad scale on different parameters to achieve optimum benefits.
Despite face shields numerous benefits, some adverse effects have also been noted. Clinicians dealing with airway management are susceptible of airborne respiratory pathogens exposure (Ho et al., 2004). Most of them particularly anesthesiologist using extra precautions, including face shield. It has been observed numerous times face shield sharp lower edge pressed the patients eyes, potential causing sever eyes injuries (Kamming et al., 2003). Hyperbaric oxygen (HBO) has been employed for several years to treat diving-related diseases that include arterial gas embolism and decompression sickness. Ocular refractive changes have been reported to the patients who received HBO by oronasal mask or face shield (Evanger et al., 2004).
Social distancing is not a novel notion it has been employed to avert the spread of infection through across the world since ancient times. Current pandemic outbreak made it more popular. It minimises the interaction between people either they are healthy or sick by residing at home. It was reported that the effect of exposure was reduced after following the norms of social distancing for endoscopist during endoscopy. The occurrence rate was reduced by 2.2 when endoscopy was performed at 6 feet away (Johnston et al., 2019). Similar study was performed on 227 endoscopists face shield for colony-forming units (CFU). The result was found to be significantly higher after endoscopy; 1–15 CFU 40%, 16–3 CFU 2.6%, 30 or more CFU 2.6% (Perisetti et al., 2020c). Moreover, in another similar study on endoscopists, the splash rate to the skin of face, forearms and, feet was 9.5% and overall splash rate to the eyes was 4.1%.
Current pandemic outbreak made it more popular. It minimises the interaction between people either they are healthy or sick by residing at home. Social distancing include strictly avoid contact, stop social gathering and stay home etc. It is a non pharmaceutical self effort to control the spread of infectious disease chiefly current COVID-19. WHO define social distancing in 2009 during flu pandemic to maintain an arm’s length distance from others. Furthermore, CDC revised it in pandemic COVID-19 that avoid mass gathering and in practice avoid close proximity to each other and suggest maintaining 6 feet distance. Among various types of infections control social distancing most effective to prevent fomites infection (Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19, 2020, Kinlaw et al., 2009).
9. Conclusion
COVID-19 outbreak has been appeared globally as a serious public health threat. Even extremely equipped nations are now facing second subsequent wave of this pandemic outbreaks that have obligated for social distancing measures. Application of face mask in the public will be contemplated only as temporary measures for several perceptive groups of people not as a substitute for established precautionary procedures. It is the need of the hour to search alternates that could prove better efficacy than present face mask. Face shield and social distancing could be better substitute of face mask for individual group of people that include COPD, acute and chronic respiratory disease, outdoor exercise, old age, underlying medical conditions and hypercapnia sensitive group but further clinical studies are required to be carried out.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors express thanks to every front‐line personnel in the fight against COVID-19.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aiello A.E., Murray G.F., Perez V., Coulborn R.M., Davis B.M., Uddin M., Shay D.K., Waterman S.H., Monto A.S. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: A randomized intervention trial. J. Infect. Dis. 2010;201:491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- Aiello A.E., Perez V., Coulborn R.M., Davis B.M., Uddin M., Monto A.S. Facemasks, hand hygiene, and influenza among young adults: A randomized intervention trial. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhassan A.R., Ed K., Em D. Surgical healthcare providers’ compliance to hand hygiene and facemask use: A case of tamale teaching hospital, Ghana. J. Prev. Infect. Control. 2020:6. [Google Scholar]
- Amanya S.B., Nyeko R., Obura B., Acen J., Nabasirye C., Oyella F., Afayo V., Okwir M. Knowledge and compliance with covid-19 infection prevention and control measures among health workers in regional referral hospitals in Northern Uganda: A cross-sectional online survey. Res. Sq. 2020;18:268–276. [Google Scholar]
- Balaban V., Stauffer W.M., Hammad A., Afgarshe M., Abd-Alla M., Ahmed Q., Memish Z.A., Saba J., Harton E., Palumbo G., Marano N. Protective practices and respiratory illness among US travelers to the 2009 Hajj. J. Travel Med. 2012;19:163–168. doi: 10.1111/j.1708-8305.2012.00602.x. [DOI] [PubMed] [Google Scholar]
- Barasheed, O., Almasri, N., Badahdah, A.-M., Heron, L., Taylor, J., McPhee, K., Ridda, I., Haworth, E., Dwyer, D., Rashid, H., Booy on behalf of the Hajj Research Team, R., 2014. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like Illness transmission among Australian Hajj pilgrims in 2011. Infect. Disord. Drug Targets. 14, 110–116. [DOI] [PubMed]
- Burnett R., Chen H., Szyszkowicz M., Fann N., Hubbell B., Pope C.A., Apte J.S., Brauer M., Cohen A., Weichenthal S., Coggins J., Di Q., Brunekreef B., Frostad J., Lim S.S., Kan H., Walker K.D., Thurston G.D., Hayes R.B., Lim C.C., Turner M.C., Jerrett M., Krewski D., Gapstur S.M., Diver W.R., Ostro B., Goldberg D., Crouse D.L., Martin R.V., Peters P., Pinault L., Tjepkema M., Van Donkelaar A., Villeneuve P.J., Miller A.B., Yin P., Zhou M., Wang L., Janssen N.A.H., Marra M., Atkinson R.W., Tsang H., Thach T.Q., Cannon J.B., Allen R.T., Hart J.E., Laden F., Cesaroni G., Forastiere F., Weinmayr G., Jaensch A., Nagel G., Concin H., Spadaro J.V. Global estimates of mortality associated with longterm exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. U. S. A. 2018;115:9592–9597. doi: 10.1073/pnas.1803222115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; StatPearls: 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [PubMed] [Google Scholar]
- Chan J.F.W., Kok K.H., Zhu Z., Chu H., To K.K.W., Yuan S., Yuen K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Zhou Z., Min W. ‘Mitochondria, oxidative stress and innate immunity Frontiers in Physiology. Frontiers Media S.A. 2018:1487. doi: 10.3389/fphys.2018.01487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S.C., Chuang V.W.M., So S.Y.C., Chen J.H.K., Sridhar S., To K.K.W., Chan J.F.W., Hung I.F.N., Ho P.L., Yuen K.Y. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung K.S., Hung I.F.N., Chan P.P.Y., Lung K.C., Tso E., Liu R., Ng Y.Y., Chu M.Y., Chung T.W.H., Tam A.R., Yip C.C.Y., Leung K.H., Fung A.Y.F., Zhang R.R., Lin Y., Cheng H.M., Zhang A.J.X., To K.K.W., Chan K.H., Yuen K.Y., Leung W.K. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China: CDC issues new guidelines saying wearing face mask is not compulsory - Republic World (no date). Available at: https://www.republicworld.com/world-news/rest-of-the-world-news/china-cdc-issues-guidelines-saying-wearing-face-mask-in-not-compulsory.html (Accessed: 13 August 2020).
- Chughtai A.A., Seale H., Dung T.C., Hayen A., Rahman B., Raina MacIntyre C. Compliance with the use of medical and cloth masks among healthcare workers in Vietnam. Ann. Occup. Hyg. 2016;60:619–630. doi: 10.1093/annhyg/mew008. [DOI] [PubMed] [Google Scholar]
- Coronavirus: Germany′s new face mask regulations explained | Germany| News and in-depth reporting from Berlin and beyond. https://www.dw. com/en/coronavirus-germanys-new-face-mask-regulations-explained/a-53260732 (Accessed: 14 September 2020).
- Covid-19: Gulf News. https://gulfnews.com/uae/covid-19-dubai-releases-new-guidelines-on-wearing-masks-1.15909 39 965613 (Accessed: 6 October 2020).
- COVID-19: How much protection do face masks offer? - Mayo Clinic. https:// www. mayoclinic .org/diseases-conditions/coronavirus/in-depth/coronavirus-mask/art-20485449 (Accessed: 14 September 2020).
- D’Amico F., Baumgart D.C., Danese S., Peyrin-Biroulet L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin. Gastroenterol. Hepatol. 2020 doi: 10.1016/j.cgh.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A. ‘Testing the efficacy of homemade masks: would they protect in an influenza pandemic?’, Disaster medicine and public health preparedness. Disaster Med Public Health Preparedness. 2013;7(4):413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A., Thompson K.A., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med. Public Health Prep. 2013;7:413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deris Z.Z., Hasan H., Sulaiman S.A., Wahab M.S.A., Naing N.N., Othman N.H. The prevalence of acute respiratory symptoms and role of protective measures among Malaysian Hajj pilgrims. J. Travel Med. 2010;17:82–88. doi: 10.1111/j.1708-8305.2009.00384.x. [DOI] [PubMed] [Google Scholar]
- Desai, A.N., Aronoff, D.M., 2020. Masks and coronavirus disease 2019 (covid-19). Jama. [DOI] [PubMed]
- Diaz Milian R. Expiratory central airway collapse in adults: anesthetic implications (Part 1) J. Cardiothoracic Vascular Anesthesia. W.B. Saunders. 2019:2546–2554. doi: 10.1053/j.jvca.2018.08.205. [DOI] [PubMed] [Google Scholar]
- Evanger K., Haugen O.H., Irgens Å., Aanderud L., Thorsen E. Ocular refractive changes in patients receiving hyperbaric oxygen administered by oronasal mask or hood. Acta Ophthalmol. Scand. 2004;82:449–453. doi: 10.1111/j.1395-3907.2004.00290.x. [DOI] [PubMed] [Google Scholar]
- Feng, S., et al., 2020. ‘Rational use of face masks in the COVID-19 pandemic’, The Lancet Respiratory Medicine. Lancet Publishing Group, pp. 434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed]
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020;1:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganyani, T., et al., 2020. ‘Estimating the generation interval for COVID-19 based on symptom onset data’, medRxiv. Cold Spring Harbor Laboratory Press, p. 2020.03.05.20031815. doi: 10.1101/2020.03.05.20031815.
- Gautret P., Vu Hai V., Sani S., Doutchi M., Parola P., Brouqui P. Protective measures against acute respiratory symptoms in French pilgrims participating in the Hajj of 2009. J. Travel Med. 2011;18:53–55. doi: 10.1111/j.1708-8305.2010.00480.x. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T. Face masks for the public during the covid-19 crisis. The BMJ. BMJ Publishing Group. 2020;369 doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
- Guidelines on Prevention of Coronavirus Disease 2019 (COVID-19) for the General Public (no date). https://www.chp.gov.hk/en/healthtopics/content/24/102466.html (Accessed: 8 August 2020).
- Guidelines on use of masks: Ministry of Health and Family Welfare. https://ncdc.gov.in/ showfile.php?lid=363 (Accessed: 8 September 2020).
- Haile, T.G., Engeda, E.H., Abdo, A.A., 2017. Compliance with Standard Precautions and Associated Factors among Healthcare Workers in Gondar University Comprehensive Specialized Hospital, Northwest Ethiopia. J. Environ. Public Health 2017. [DOI] [PMC free article] [PubMed]
- Hajifathalian K., Krisko T., Mehta A., Kumar S., Schwartz R., Fortune B., Sharaiha R.Z., Kaplan A., Gonzalez S., Skaf D., Ang B., Choi A., Wong A., Aboubakr A., Niec R., Rohan E., Speiser J., Ying X., Pan Y., Ianelli M., Rajan A., Ravishankar A., Tewani S., Dawod E., Dawod Q., Rosenblatt R., Carr-Locke D., Shah S., Mahadev S., Wan D., Crawford C., Sholle E., Brown R., Cohen D. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: Clinical implications. Gastroenterology. 2020;159:1137–1140. doi: 10.1053/j.gastro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashim S., Ayub Z.N., Mohamed Z., Hasan H., Harun A., Ismail N., Rahman Z.A., Suraiya S., Naing N.N., Aziz A.A. The prevalence and preventive measures of the respiratory illness among Malaysian pilgrims in 2013 Hajj season. J. Travel Med. 2016;23 doi: 10.1093/jtm/tav019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho A.M.H., Lam G.C.S., Karmakar M.K. Potential eye injury due to protective face shields [10] Anesthesiology. 2004;100:201. doi: 10.1097/00000542-200401000-00050. [DOI] [PubMed] [Google Scholar]
- Hoang V.T., Meftah M., Anh Ly T.D., Drali T., Yezli S., Alotaibi B., Raoult D., Parola P., Pommier de Santi V., Gautret P. Bacterial respiratory carriage in French Hajj pilgrims and the effect of pneumococcal vaccine and other individual preventive measures: A prospective cohort survey. Travel Med. Infect. Dis. 2019;31 doi: 10.1016/j.tmaid.2018.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- How to Protect Yourself & Others | CDC (no date a). https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (Accessed: 13 August 2020).
- Howard J. Face mask against COVID-19: An evidence review. Br. Med. J. April 2020:1–8. doi: 10.20944/preprints202004.0203.v1. [DOI] [Google Scholar]
- Hutchings, R., 2020. The impact of Covid-19 on the use of digital technology in the NHS.
- Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19 | CDC (2020). https://www.cdc.gov/coronavirus/2019-ncov/ hcp/guidance-risk-assesment-hcp.html (Accessed: 13 August 2020).
- Jefferson, T., Del Mar, C.B., Dooley, L., Ferroni, E., Al-Ansary, L.A., Bawazeer, G.A., van Driel, M.L., Nair, S., Jones, M.A., Thorning, S., Conly, J.M., 2011. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane database Syst. Rev. [DOI] [PMC free article] [PubMed]
- Johnson K.D., Harris C., Cain J.K., Hummer C., Goyal H., Perisetti A. Pulmonary and extra-pulmonary clinical manifestations of COVID-19. Front. Med. 2020;7:526. doi: 10.3389/fmed.2020.00526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston E.R., Habib-Bein N., Dueker J.M., Quiroz B., Corsaro E., Ambrogio M., Kingsley M., Papachristou G.I., Kreiss C., Khalid A. Risk of bacterial exposure to the endoscopist’s face during endoscopy. Gastrointest. Endosc. 2019;89:818–824. doi: 10.1016/j.gie.2018.10.034. [DOI] [PubMed] [Google Scholar]
- Kamming D., Gardam M., Chung F. Editorial I anaesthesia and SARS. Br. J. Anaesth. 2003:715–718. doi: 10.1093/bja/aeg173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C.O., Nam C.M., Lee D.C., Chang J., Lee J.W. Is abdominal obesity associated with the 2009 influenza A (H1N1) pandemic in Korean school-aged children? Influenza Other Resp. 2012;6:313–317. doi: 10.1111/j.1750-2659.2011.00318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlaw K., Barrett D.H., Levine R.J. Ethical guidelines in pandemic influenza: recommendations of the ethics subcommittee of the advisory committee of the director, centers for disease control and prevention. Disaster Med. Public Health Prep. 2009;3(suppl 2):S185–S192. doi: 10.1097/DMP.0b013e3181ac194f. [DOI] [PubMed] [Google Scholar]
- Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- Kopel J., Perisetti A., Roghani A., Aziz M., Gajendran M., Goyal H. Racial and gender-based differences in COVID-19. Front. Public Health. 2020;8:418. doi: 10.3389/fpubh.2020.00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L. Respiratory virus shedding in exhaled breath and efficacy of face masks nature medicine. Nat. Res. 2020;26(5):676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N., Chu D., Shiu E., Chan K.H., McDevitt J.J., Hau B., Yen H.L., Li Y., Ip D., Peiris J., Seto W.H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26(5):676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., Yen H.L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifesaver or false protection: do face masks stop coronavirus? | Financial Times. Available at: https://www.ft.com/content/64ac8848-a005-466a-bc93-fb1e38b19182 (Accessed: 13 August 2020).
- Lindsley, W.G., et al., 2014. ‘Efficacy of face shields against cough aerosol droplets from a cough simulator’, J. Occupational and Environ. Hygiene. Taylor and Francis Inc., 11(8), pp. 509–518. doi: 10.1080/15459624.2013.877591. [DOI] [PMC free article] [PubMed]
- Ling Y., Xu S.B., Lin Y.X., Tian D., Zhu Z.Q., Dai F.H., Wu F., Song Z.G., Huang W., Chen J., Hu B.J., Wang S., Mao E.Q., Zhu L., Zhang W.H., Lu H.Z. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin. Med. J. 2020;133:1039–1043. doi: 10.1097/CM9.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansour A.A., Even J.L., Phillips S., Halpern J.L. Eye protection in orthopaedic surgery. An in vitro study of various forms of eye protection and their effectiveness. J. Bone Joint Surg. Am. 2009;91:1050–1054. doi: 10.2106/JBJS.H.00460. [DOI] [PubMed] [Google Scholar]
- Matuschek C., Moll F., Fangerau H., Fischer J.C., Zänker K., Van Griensven M., Schneider M., Kindgen-Milles D., Knoefel W.T., Lichtenberg A., Tamaskovics B., Djiepmo-Njanang F.J., Budach W., Corradini S., Häussinger D., Feldt T., Jensen B., Pelka R., Orth K., Peiper M., Grebe O., Maas K., Bölke E., Haussmann J. The history and value of face masks. Eur. J. Med. Res. 2020;25:1–8. doi: 10.1186/s40001-020-00423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGaw C.D., Tennant I., Harding H.E., Cawich S.O., Crandon I.W., Walters C. Healthcare workers’ attitudes to and compliance with infection control guidelines in the operating department at the university hospital of the West Indies, Jamaica. Int. J. Infect. Control. 2012:8. [Google Scholar]
- Ministry of Health, Singapore Updates on COVID-19 (Coronavirus disease 2019) local situation. https://www.moh.gov.sg/covid-19. (Accessed: 14 August 2020).
- MOH News - MOH: Proper Use of Face Mask Increases Its Efficiency. https://www.moh.gov.sa/ en/Ministry/MediaCenter/News/Pages/News-2020-07-04-003.aspx (Accessed: 8 August 2020).
- Nichol K., McGeer A., Bigelow P., O’Brien-Pallas L., Scott J., Holness D.L. Behind the mask: Determinants of nurse’s adherence to facial protective equipment. Am. J. Infect. Control. 2013;41:8–13. doi: 10.1016/j.ajic.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikiforuk A.M., Cutts T.A., Theriault S.S., Cook B.W.M. Challenge of liquid stressed protective materials and environmental persistence of Ebola virus. Sci. Rep. 2017:7. doi: 10.1038/s41598-017-04137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization W.H. Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza: annex: report of systematic literature reviews. World Health Organization. 2019 [Google Scholar]
- Patel, S., Majmundar, S.H., 2018. Physiology, Carbon Dioxide Retention, StatPearls. StatPearls Publishing. Available at: http://www.ncbi.nlm.nih.gov/pubmed/29494063 (Accessed: 13 August 2020). [PubMed]
- Perencevich E.N., Diekema D.J., Edmond M.B. Moving personal protective equipment into the community. JAMA. Am. Med. Assoc. 2020;323(22):2252. doi: 10.1001/jama.2020.7477. [DOI] [PubMed] [Google Scholar]
- Perisetti A., Gajendran M., Goyal H. Putative mechanisms of diarrhea in COVID-19. Clin. Gastroenterol. Hepatol. 2020 doi: 10.1016/j.cgh.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perisetti A., Gajendran M., Mann R., Elhanafi S., Goyal H. COVID-19 extrapulmonary illness - special gastrointestinal and hepatic considerations. Dis. Mon. 2020:101064. doi: 10.1016/j.disamonth.2020.101064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perisetti A., Goyal H., Gajendran M., Boregowda U., Mann R., Sharma N. Prevalence, mechanisms, and implications of gastrointestinal symptoms in COVID-19. Front. Med. 2020;7:741. doi: 10.3389/fmed.2020.588711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picard J., Cornec G., Baron R., Saliou P. Wearing of face masks by healthcare workers during COVID-19 lockdown: what did the public observe through the French media? J. Hosp. Infect. 2020;106:617–620. doi: 10.1016/j.jhin.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash G., Shetty P., Thiagarajan S., Gulia A., Pandrowala S., Singh L., Thorat V., Patil V., Divatia J.V., Puri A., Pramesh C.S. Compliance and perception about personal protective equipment among health care workers involved in the surgery of COVID-19 negative cancer patients during the pandemic. J. Surg. Oncol. 2020;122:1013–1019. doi: 10.1002/jso.26151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purushothaman P.K., Priyangha E., Vaidhyswaran R. Effects of prolonged use of facemask on healthcare workers in tertiary care hospital during COVID-19 pandemic. Indian J. Otolaryngol. Head Neck Surg. 2020:02124. doi: 10.1007/s12070-020-02124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Q&A (English) about the new coronavirus. https://www.mhlw.go.jp/stf/seisakunitsuite /bunya/kenkou_iryou/dengue_fever_qa_00014.html (accessed August 14, 2020).
- Ramachandran P., Onukogu I., Ghanta S., Gajendran M., Perisetti A., Goyal H., Aggarwal A. Gastrointestinal symptoms and outcomes in hospitalized coronavirus disease 2019 patients. Dig. Dis. 2020;38:373–379. doi: 10.1159/000509774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Martinez C.E., Sossa-Briceño M.P., Cortés J.A. Decontamination and reuse of N95 filtering facemask respirators: A systematic review of the literature. Am. J. Infect. Control. 2020 doi: 10.1016/j.ajic.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed K.M.I., Mofleh J., Hafiz Rasooly M., Iabal Aman M. Occurrence of acute respiratory infection, diarrhea and jaundice among Afghan pilgrims, 2010. J. Epidemiol. Glob. Health. 2012;2:215–220. doi: 10.1016/j.jegh.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarfraz S., Raza R., Aziz K., Umar M., Noreen K., Shehryar M. Compliance on the use of different types of face mask by healthcare workers and general public in tertiary care hospital of RMU during COVID-19 pandemic. J. Rawalpindi Med. Coll. 2020;24:71–76. [Google Scholar]
- Schwartz K.L. Lack of COVID-19 transmission on an international flight. CMAJ. Can. Med. Assoc. 2020:E410. doi: 10.1503/cmaj.75015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S.K., Mishra M., Mudgal S.K. Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: A systematic review and meta-analysis. J. Educ. Health Promot. 2020;28:192. doi: 10.4103/jehp.jehp_533_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui A.J., Jahan S., Ashraf S.A., Alreshidi M., Ashraf M.S., Patel M., Snoussi M., Singh R., Adnan M. Current status and strategic possibilities on potential use of combinational drug therapy against COVID-19 caused by SARS-CoV-2. J. Biomol. Struct. Dyn. 2020;5:1–14. doi: 10.1080/07391102.2020.1802345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui A.J., Danciu C., Ashraf S.A., Moin A., Singh R., Alreshidi M., Patel M., Jahan S., Kumar S., Alkhinjar M.I.M., Badraoui R., Snoussi M., Adnan M. Plants-derived biomolecules as potent antiviral phytomedicines: New insights on ethnobotanical evidences against coronaviruses. Plants (Basel). 2020;21:1244. doi: 10.3390/plants9091244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel J.D., Rhinehart E., Jackson M., Chiarello L., H.C.I.C.P.A. Committee 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am. J. Infect. Control. 2007;35(10):S65. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmerman J.M., Suntarattiwong P., Levy J., Jarman R.G., Kaewchana S., Gibbons R.V., Cowling B.J., Sanasuttipun W., Maloney S.A., Uyeki T.M., Kamimoto L., Chotipitayasunondh T. Findings from a household randomized controlled trial of hand washing and face masks to reduce influenza transmission in Bangkok, Thailand. Influenza Other Resp. 2011;5:256–267. doi: 10.1111/j.1750-2659.2011.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultan S., Altayar O., Siddique S.M., Davitkov P., Feuerstein J.D., Lim J.K., Falck-Ytter Y., El-Serag H.B. AGA institute rapid review of the gastrointestinal and liver manifestations of COVID-19, meta-analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology. 2020;159:320–334. doi: 10.1053/j.gastro.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The State Council’s Joint Prevention and Control Mechanism issued the ‘Technical Guidelines for the Selection and Use of Masks for the Prevention of New Coronavirus Infection by Different Populations’_Department Government_Chinese Government Network. http://www.gov.cn /xinwen/2020-02/05/content_5474774.htm (Accessed: 8 August 2020).
- Tripathi R., Alqahtani S.S., Albarraq A.A., Meraya A.M., Tripathi P., Banji D., Alshahrani S., Ahsan W., Alnakhli F.M. Awareness and preparedness of COVID-19 outbreak among healthcare workers and other residents of south-West Saudi Arabia: A cross-sectional survey. Front. Public Heal. 2020;8:482. doi: 10.3389/fpubh.2020.00482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Sande M., Teunis P., Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS ONE. 2008;3(7) doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. Massachussetts Medical Society. 2020:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahab S., Ahmad I., Usmani S., Ahmad M.P. Epidemiological situation and efficacy of dexamethasone for the treatment planning of COVID-19: A perspective review. Curr. Drug Deliv. 2020;17 doi: 10.2174/1567201817666201006144008. [DOI] [PubMed] [Google Scholar]
- Wahab S., Ahmad I., Usmani S., Ahmad M.P. Epidemiological situation and efficacy of dexamethasone for the treatment planning of COVID-19: A perspective review. Curr. Drug Deliv. 2020;17 doi: 10.2174/1567201817666201006144008. [DOI] [PubMed] [Google Scholar]
- WHO, 2020. Coronavirus (COVID-19). https://covid19.who.int (accessed 6.10.20).
- Why Face Masks Are Crucial Now in the Battle Against COVID-19 (no date). https://www. healthline.com/health-news/face-masks-importance-battle-with-covid19 (Accessed: 11 August 2020).
- Yang P., Seale H., Raina MacIntyre C., Zhang H., Zhang Z., Zhang Y., Wang X., Li X., Pang X., Wang Q. Mask-wearing and respiratory infection in healthcare workers in Beijing, China. Brazilian J. Infect. Dis. 2011;15:102–108. doi: 10.1016/S1413-8670(11)70153-2. [DOI] [PMC free article] [PubMed] [Google Scholar]