ABSTRACT
Background
Suboptimal infant and young child feeding (IYCF) practices contribute to child undernutrition. Sierra Leone Demographic and Health Survey data show that IYCF practices remain poor despite modest improvements. Recent studies have identified the role of grandmothers as critical to child nutrition; however, in Sierra Leone to date, the potential for grandmothers to influence IYCF practices has not been investigated.
Objectives
We examined how an innovative grandmother-inclusive approach (GMIA) can be used to address suboptimal IYCF practices.
Methods
Using a quasi-experimental design, we compared IYCF beliefs and practices between GMIA intervention communities (receiving monthly dialogue sessions on nutrition, quarterly community praise sessions, and intergenerational forums) and comparison communities (receiving standard nutrition education) in Bum chiefdom from 2013 and 2016. The quantitative endline survey targeted 101 pregnant women, 291 women with children aged <2 y, and 219 grandmothers. Statistical analyses utilized t tests and χ2 tests to examine differences between intervention and comparison communities at endline. Multivariate regression was used to determine the intervention's effect on IYCF outcomes of interest.
Results
Awareness of and participation in the GMIA was high among mothers and grandmothers in intervention communities. The percentage of infants and young children aged 0–23 mo (n = 291) exclusively breastfed during the first week of life was significantly higher in the intervention group (90.2% compared with 79.4%, P = 0.01). Among infants aged 6–23 mo (n = 219), the percentage achieving minimum dietary diversity and minimum acceptable diet was significantly higher in the intervention group (77.2% compared with 51.8%, P < 0.001; and 53.8% compared with 22.6%, P < 0.001, respectively). Differences in percentages achieving minimum meal frequency (MMF) were only significant for infants aged 9–23 mo, with the intervention group achieving a higher MMF (54.6% compared with 36.9%, P = 0.02).
Conclusions
Results suggest that a GMIA that recognizes grandmothers’ roles and strengthens their knowledge can contribute to improved IYCF practices.
Keywords: infant and young child feeding, breastfeeding, diet diversity, grandmothers, Grandmother Inclusive Approach, innovation, behavior change communication
Introduction
In communities of the Global South, grandmothers and other senior women play vital roles in child nutrition, supporting mothers after delivery and with young children (1–6). A review of Demographic and Health Survey (DHS) data from 31 sub-Saharan countries concluded that co-residency with a grandmother is positively associated with reduced child stunting (7). In Sierra Leone, we found that grandmothers, aunts, and other older women (hereafter referred to as “grandmothers”) support younger family members by sharing traditions, knowledge, experiences, and caring for mothers and their children (8). Prior experiences of the Grandmother Project (GMP) and other researchers empowering grandmothers with appropriate information in Senegal (9), Malawi (10, 11), and Kenya (12) have shown improvements in infant and young child feeding (IYCF) knowledge, attitudes, and practices of mothers and grandmothers and child growth.
Sierra Leone made improvements in some IYCF practices between 2010 and 2013, such as increasing exclusive breastfeeding (EBF) from 12% to 32%, whereas other practices like early breastfeeding (BF) initiation (infants put to breast within 1 h of birth) remained static, increasing only from 51% to 53% (13, 14). Definitions of minimum dietary diversity (MDD, or children receiving ≥4 of 7 prespecified food groups) and minimum acceptable diet [MAD, or children meeting an MDD in addition to a minimum meal frequency (MMF) based on age and BF status] (15) changed between the 2 consecutive DHSs in Sierra Leone. The switch from using ≥3 food groups to ≥4 in defining MDD makes comparisons difficult; however, the 2013 DHS revealed alarmingly low rates of 14.5% and 7%, respectively (13, 14).
Optimal nutrition practices during pregnancy and the first 2 y of a child's life (the first 1000 d) are critical to survival rates, optimal growth, and development of children (16), as well as long-term social, economic, and development outcomes (17). Advantages of adequate nutrition for both individuals and nations place interventions to improve young child nutrition as one of the top investment priorities a country can make, given associations with reduced morbidity and mortality, enhanced child schooling, and later adult productivity (18).
To address low levels of IYCF practices and building on our formative research identifying grandmothers as key influencers of maternal and child health and nutrition (MCHN) we designed a pilot program targeting grandmothers as change agents, referred to as the grandmother-inclusive approach (GMIA), developed by the GMP (8, 19). Although our qualitative formative research showed that grandmothers can be critical assets for positive social and behavior change, grandmothers’ potential for changing critical IYCF practices in Sierra Leone has not been carefully examined.
This article describes the GMIA intervention, and endline differences in IYCF practices in mothers with children under 2 y of age (MCU2) who participated in the GMIA compared with comparison communities.
Methods
Study site
The project, known as Mamanieva—“for our grandmothers” in the Mende language—was implemented in Torma section of World Vision's (WV's) operational area in Bum Chiefdom, Bonthe District, Southern Province of Sierra Leone. The Mende tribe predominates in Bum Chiefdom, with a population of ∼23,000; main economic activities are agriculture, fishing, and petty trading.
Study design
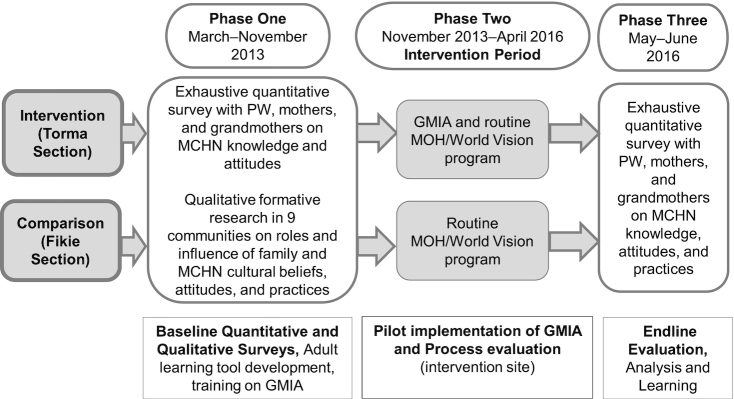
The pilot study, implemented from 2013 to 2016 by WV and evaluated by Njala and Emory Universities, used a phased approach, incorporating a quasi-experimental design with mixed methods to evaluate GMIA intervention effects (Figure 1). Two geographically delineated administrative sections of Bum Chiefdom (Torma and Fikie) were purposively selected for the study based on accessibility for most part of the year (in absence of heavy rains), both with similar population size, people groups, culture, climate, and economic activities. The Torma section of the Bum Chiefdom (population 2527) was allocated to receive the intervention (GMIA) whereas the Fikie section (population 2747) was allocated to the comparison group.
FIGURE 1.
Overall study design. GMIA, grandmother-inclusive approach; MCHN, maternal and child health and nutrition; MOH, Ministry of Health; PW, pregnant women.
The study was implemented in 3 phases (Figure 1): phase 1 included a quantitative cross-sectional baseline survey and qualitative formative research with development of appropriate adult education tools and training in the GMIA (8, 20); phase 2 involved the implementation of the GMIA and a qualitative process evaluation to identify potential gaps and areas to strengthen (21); and phase 3 involved an endline survey of MCHN knowledge, attitudes, and practices. This article describes the intervention and reports on endline IYCF knowledge, beliefs, and practices.
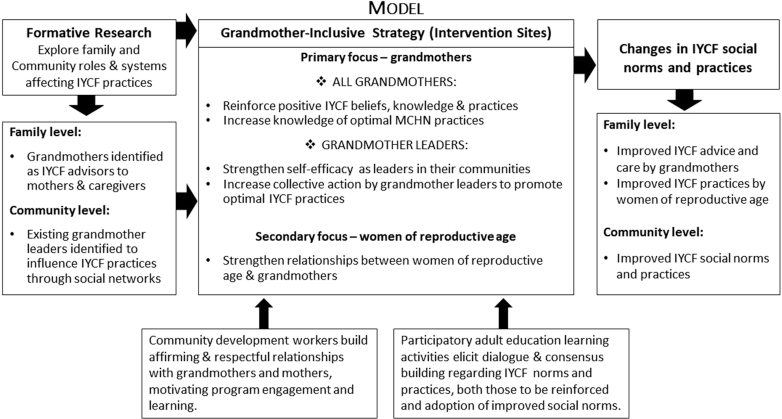
Intervention description: the GMIA
Following formative qualitative research that informed the intervention (8), we designed the Mamanieva Project to explicitly involve all grandmothers along with mothers. We used the GMIA developed by GMP (19) that builds on grandmothers’ culturally designated role as caregivers and advisors and puts them at the center of program. The conceptual model for this project utilized the GMIA, a family-centered and assets-based approach for promoting improved IYCF in MCU2 (19).The approach involves 5 key steps: 1) assess roles, relationships, and knowledge; 2) affirm grandmother's role as a cultural resource or asset; 3) build consensus for change through dialogue; 4) build capacity of grandmother leaders (GMLs); and 5) evaluate results and document for learning. These steps are fully detailed elsewhere (19) and described briefly below.
Figure 2.
Grandmother-inclusive conceptual model. IYCF, infant and young child feeding; MCHN, maternal and child health and nutrition. Aubel & World Vision International 2014.
Step 1: Assess roles, relationships, and knowledge
The first step of the GMIA was qualitative research (a component of phase 1) investigating both the roles and influences of family members on MCHN and their cultural beliefs, attitudes, and practices related to MCHN, with details and results recently published (8). Three WV field staff with experience and training in participatory adult education and community engagement methods led implementation of Mamanieva activities including steps 2 to 4 in phase 2.
Step 2: Affirm grandmother's role as a cultural resource
Activities began and continued intermittently throughout the project with special community-wide “days of praise of grandmothers” facilitated by WV staff where grandmothers’ roles and experience were recognized through songs praising them and stories describing their important roles (19). Affirming all grandmothers collectively, in all intervention communities is a key element of this collective approach. From an educational and learning perspective, praising an individual for who he/she is and what they know and do, boosts self-esteem and self-confidence, and increases their openness (22) to new ideas.
Step 3: Build consensus for change through dialogue
Monthly group sessions for all grandmothers in intervention communities used a dialogue approach that reinforces positive existing MCHN practices and the role of grandmothers in fostering those practices, while eliciting dialogue on the practices that need to be modified. Each month, in each community, a new MCHN topic was covered during group dialogue sessions facilitated by WV staff, with all grandmothers in each community using adult education tools. An adult education expert supported the project team coordinating with the District Ministry of Health (MoH) staff to develop and pretest locally appropriate MCHN curriculum and tools targeting grandmothers. Curriculum topics included optimal IYCF practices, reinforcing local practices that align with current international recommendations, and building consensus on those needing to be modified (8). Tools including songs, games, picture discussion cards, and stories-without-an-ending developed for each topic were used in the regular program activities (i.e., monthly dialogue sessions and intergenerational meetings) (19).
WV staff also facilitated monthly intergenerational forums in each community where grandmothers and young mothers came together to discuss MCHN topics. Although these forums were designed to focus on grandmothers and mothers, during the process evaluation men asked to attend and were then permitted to do so.
Step 4: Build capacity of GMLs
GMLs were selected by their communities based on community-defined criteria [e.g., well respected, experience caring for pregnant women (PW) and mothers with young children, and/or traditional birth attendants]. The GMLs from all communities attended quarterly stakeholder meetings, facilitated by WV and Bonthe District MoH staff, where their leadership abilities and facilitation skills were strengthened in addition to their understanding of optimal MCHN practices reinforced. After the first year of implementation, GMLs began cofacilitating and then leading group nutrition education activities. The GMLs were not remunerated in any form.
This article reports on a portion of step 5, evaluating and documenting results for ongoing learning (phase 3).
Both intervention and comparison communities received the standard of care for nutrition education delivered by the MoH through antenatal and postnatal care visits, and home visits for PW/MCU2 by community health workers (CHWs) trained by WV staff. Key MCHN messages covered by CHWs include feeding during pregnancy, health-seeking behaviors, facility delivery, care for newborns and sick children, and IYCF, using WV's program model, Timed and Targeted Counselling. In WV's Timed and Targeted Counselling model, WV trained CHWs to provide unique messages to families of young children timed to a child's growth and development to promote health behaviors, nutrition, and early childhood development (23, 24).
Survey sample and data collection
Eligible participants for the baseline and endline surveys were 1) women aged ≥17 y, either PW or with a child under 2 y (CU2), and 2) grandmothers residing with eligible mothers and women aged >45 y living in the community. Due to the limited number of potentially eligible respondents in each community, exhaustive census-based sample measures were employed for both surveys. Available sample sizes were estimated prior to data collection using Sierra Leone census-based population estimates from 2004 and 2015 (25) for the baseline and endline surveys, respectively, and accounting for a 10% refusal rate and assuming 3% of the population in Bum are PW and 9% have a CU2. If there was >1 CU2 in the household, the enumerator selected the index child by coin flip. In the event of >1 grandmother residing in an eligible household, the senior woman most involved in the feeding and care of women and children, as reported by the mother, was selected.
The baseline data were collected in March 2013 by Njala University with a total of 474 eligible women, 295 (217 MCU2 and 78 PW) from intervention communities and 179 (126 MCU2 and 53 PW) from comparison communities. A total of 147 grandmothers were interviewed, 97 from intervention and 50 from comparison communities. The baseline survey focused on household sociodemographic and respondent characteristics, MCHN knowledge and attitudes, and key influencers, using a series of 16 knowledge questions and 11 scenarios concerning diet and nutrition in pregnancy and recommended IYCF practices. IYCF knowledge questions addressed: timing of BF initiation, giving colostrum, timely introduction of complementary foods, meal frequency, and introduction of specific food items such as meat, eggs, fruits, and vegetables as per WHO/UNICEF child feeding recommendations (26). Knowledge questions were aggregated to create a maternal and child nutrition (MCN) knowledge score with each correct answer given 1 point to a maximum of 16 points. Scenarios based on formative qualitative research findings (8) were included to explore attitudes and beliefs. Although planned, IYCF practices were not collected during the baseline survey; this was rectified during the endline survey (see below). Trained enumerators used paper-based surveys that were scanned and securely transmitted electronically to Emory University for data entry and analysis.
The endline cross-sectional survey was conducted by Emory University following pilot testing and revision of survey tools, using the electronic Open Data Kit (ODK) platform. The enumerators recorded data on tablets and uploaded survey data to the ODK server at the end of each day. A total of 101 PW and 291 MCU2 participated in the endline survey: 54 PW and 184 MCU2 from intervention, and 47 PW and 107 MCU2 from comparison communities. A total of 219 grandmothers were interviewed, 157 from intervention and 62 from comparison communities. Of the 157 grandmothers in intervention communities, 63 were GMLs. Of those identified as eligible using an exhaustive screening process, ∼9–12% of women and 16% of grandmothers could not be tracked despite ≤2 attempts made within a 1-wk period.
The endline cross-sectional survey collected similar data as the baseline (Supplemental Material). In addition, we collected information on MCHN practices, information sources, child birth weight, uptake of program activities, and household food deprivation using the household hunger scale (27). Information on IYCF practices was collected using methods described by WHO (15, 26, 28). We included BF indicators of early BF initiation (within 1 h of birth), EBF (breastmilk only for 6 mo), and continued BF for children aged 6–23 mo, based on the 24-h recall method. In addition, we assessed maintenance of early EBF (i.e., in the first week of life) and duration of EBF using a since-birth recall for the introduction of nonbreastmilk liquids or foods.
Complementary feeding practices in children aged 6–23 mo followed international standards and included MMF (2 times for breastfed infants aged 6–8 mo; 3 times for breastfed children aged 9–23 mo; 4 times for nonbreastfed children aged 9–23 mo), MDD (≥4 of 7 prespecified food groups), MAD (children meeting MDD in addition to MMF based on age and BF status), feeding practices of children while ill, receipt of vitamin A supplementation, and provision of iron drops (15, 26). We used the open recall of foods consumed by infants and children in the 24 h prior to the survey, which enumerators recorded on dietary recall forms (hard copies); foods were then categorized into their respective food groups. This approach is recommended for areas with limited diet diversity because it reduces respondent burden and response bias. However, initial data quality checks comparing 10% of the diet recall forms against entered data found that enumerators miscategorized ≥1 food group question per form checked. Thus, the entire dataset was cleaned using the hard copy recall forms.
Baseline and endline surveys lasting from 60 to 90 min were conducted in the local language, Mende, in respondents’ homes. Because Mende is not a written language, during baseline and endline trainings, enumerators, aided by professional translators, reviewed each question and decided on the English to Mende translations, which were then pilot tested before final agreement on the use of Mende language terminologies during the survey.
Ethical review and informed consent
All study procedures and tools were approved by the local review boards in Sierra Leone and at Emory University. Participants were informed of the nature and purpose of the research, expectations of the participants, potential risks/benefits of the study, and all provided written consent or thumbprint prior to enumeration. Copies of the consent document and research team contact information were provided to participants.
Statistical analysis
Survey data were analyzed using Excel and SAS v.9.4 (SAS Institute). Normally distributed continuous variables were analyzed using t tests and F-tests; non-normally distributed continuous variables were analyzed using Wilcoxon rank sum test. Categorical variables were analyzed with χ2 test. Differences between the intervention and comparison sections at endline were considered significant at P < 0.05. Multivariable regression models using SAS v.9.4 were developed for IYCF indicators described that were significant in preliminary analyses, 2 of which are reported in this article: MDD and MAD. These models were adjusted for differences in sociodemographic variables at endline including child age and sex, maternal schooling and parity, schooling and occupation of household head, and household hunger category. Because the baseline survey only examined knowledge, attitudes, and beliefs, we are unable to assess the changes in IYCF practices from baseline to endline.
Results
Descriptive statistics of respondents at baseline and endline
Detailed results of the qualitative formative research and baseline survey are presented elsewhere (8, 20). Briefly, women and heads of household in intervention communities had more years of education (3.0 compared with 2.0, P = 0.01; and 3.8 compared with 2.9, P = 0.01, respectively), larger households (7.7 compared with 6.8, P < 0.01), and a greater percentage had grandmothers residing in their households (83% compared with 63%, P < 0.001); participants did not differ with respect to other sociodemographic characteristics. At baseline, women's MCN knowledge scores were lower in intervention than in comparison communities (5.3 compared with 6.8, P < 0.05; maximum score = 16). In both areas, most qualitative research participants reported giving water from birth, introducing ngwoh bayei (rice water and salt) at 2 mo, and introducing thin porridge between 3 and 5 mo (8).
At endline survey, MCU2 were on average 26 y old and approximately two-thirds had ≥3 children. No differences were found between intervention and comparison sites in the average ages of mothers, number of children in households, employment, or marital status (Table 1). However, a greater percentage of women and household heads in comparison communities had never attended school. Of concern was a much higher percentage of respondents reporting household hunger in comparison than in intervention communities (50.7% compared with 7.6%, P < 0.001). These differences were controlled for in regression models, as noted above.
TABLE 1.
Selected demographics of households: heads, mothers with children aged <2 y, and children at Mamanieva endline survey1
| Intervention (n = 184) | Comparison (n = 107) | P | |
|---|---|---|---|
| Average maternal age,2 y | 26.0 ± 6.0 | 26.5 ± 5.8 | 0.61 |
| No. of children | 0.37 | ||
| 1–2 | 37.5 | 31.8 | |
| ≥3 | 62.5 | 68.2 | |
| Sex of index child, % male | 46.2 | 50.5 | 0.48 |
| Mean age of index child | 11.7 ± 7.0 | 11.6 ± 7.0 | 0.70 |
| Age of index child, mo | 0.60 | ||
| 0–5.9 | 26.4 | 22.4 | |
| 6–8.9 | 13.2 | 16.8 | |
| 9–23.9 | 60.4 | 60.8 | |
| Schooling | 0.02 | ||
| Never attended | 53.8 | 70.1 | |
| Some or completed primary | 21.7 | 11.2 | |
| Some or completed secondary or more | 24.5 | 18.7 | |
| Employment | 0.60 | ||
| Agriculture | 83.7 | 88.8 | |
| Informal business/trader | 5.4 | 4.7 | |
| Marital status | 0.39 | ||
| Married/partnered (monogamous) | 78.3 | 72.9 | |
| Married/partnered (polygamous) | 15.8 | 15.0 | |
| Head of household schooling (n = 287)3 | 0.003 | ||
| Never attended | 68.5 | 87.7 | |
| Some or completed primary | 7.2 | 1.9 | |
| Head of household occupation (n = 287)3 | 0.05 | ||
| Agriculture | 83.4 | 91.5 | |
| Household hunger category | <0.001 | ||
| Little to no hunger | 92.4 | 49.1 | |
| Moderate to severe hunger | 7.6 | 50.9 |
1Values are % or mean ± SD. MCU2, mothers with children aged <2 y.
One hundred and sixty-eight MCU2 could recall age: intervention, n = 108; comparison, n = 60.
Four MCU2 respondents are heads of their household.
The mean age of grandmothers was 57 y, although this is likely underestimated because only 40 respondents could remember their age. No differences were found between length of time in the household and average number of children, although grandmothers in the comparison communities reported more grandchildren, on average (Table 2).
TABLE 2.
Demographic statistics for grandmothers at Mamanieva endline survey1
| Intervention (n = 157) | Comparison (n = 62) | P | |
|---|---|---|---|
| Mean number of years in household (n = 86)2 | 30.5 ± 19.6 | 38.1 ± 21.8 | 0.13 |
| Number of children (n = 141)3 | 5.4 ± 2.3 | 6.0 ± 2.8 | 0.15 |
| Mean number of grandchildren (n = 141)3 | 6.6 ± 4.7 | 8.9 ± 7.2 | 0.02 |
| Employment | 0.48 | ||
| Agriculture | 85.7 | 79.1 | |
| Schooling | 0.39 | ||
| Never attended | 85.7 | 79.1 | |
| Some or completed primary | 1.9 | 2.3 | |
| Marital status | 0.3 | ||
| Married monogamous | 36.2 | 44.2 | |
| Married polygamous | 24.8 | 11.6 | |
| Widowed | 35.2 | 41.9 |
1Grandmothers included mothers, mothers-in-laws, aunts, or nonrelated elder women.
Eighty-six grandmothers knew the number of years they had lived in household (intervention n = 63, comparison n = 23).
One hundred and forty-one grandmothers had children and grandchildren (intervention n = 99, comparison n = 42).
Program participation
Awareness of and participation in the Mamanieva program activities by grandmothers, PW, and MCU2 was high in the intervention sites (Table 3). Almost all (98%) had heard of the Mamanieva project, 93% had participated in ≥1 WV-facilitated dialogue session, and 91% in a community praise session. Most had participated in WV-facilitated (>88%) and grandmother-led (>86%) sessions within the past 2–3 mo. Nearly half of respondents reported participating in WV-led dialogue sessions at least once a month.
TABLE 3.
Percentages of women and grandmothers from intervention communities participating in Mamanieva activities1
| Women (n = 225) | Grandmothers (n = 157) | |
|---|---|---|
| Heard of Mamanieva project | 98.2 | 96.8 |
| Participated at least once in WV-facilitated Mamanieva sessions (n = 373)2 | 92.8 | 94.1 |
| Frequency of participation in WV-facilitated sessions (n = 347)2 | ||
| Only a few times | 18.1 | 10.5 |
| Several times/y but <1/mo | 36.3 | 37.1 |
| ∼1/mo | 8.8 | 5.6 |
| >1/mo | 36.8 | 46.9 |
| Most recent WV-facilitated session attended (n = 347)2 | ||
| Within the past 2–3 mo | 88.3 | 88.0 |
| >3 mo ago but within the past 6 mo | 10.7 | 9.9 |
| >6 mo ago | 1.0 | 1.4 |
| Participated at least once in GML-led Mamanieva sessions (n = 373)2 | 92.8 | 95.4 |
| Most recent GML-led session attended (n = 349)2 | ||
| Within the past 2–3 mo | 88.8 | 86.8 |
| >3 mo ago but within the past 6 mo | 9.3 | 11.1 |
| >6 mo ago but within the last year | 2.0 | 2.1 |
| Participated at least once in a community praise session (n = 373)2 | 89.6 | 94.1 |
| Number of times attended a community praise session (n = 367)2 | ||
| Never | 10.6 | 6.0 |
| 1–2 times | 49.2 | 35.0 |
| 3–4 times | 25.6 | 20.0 |
| >4 times | 25.1 | 18.8 |
| Last praise session attended | ||
| Within the past 2–3 mo | 84.9 | 83.9 |
| >3 mo ago but within the past 6 mo | 11.6 | 11.9 |
| >6 mo ago | 3.5 | 4.2 |
1GML, grandmother leader; WV, World Vision.
n refers to total applicable number of respondents.
IYCF knowledge, beliefs, and attitudes of grandmothers and mothers
We found higher overall nutrition knowledge among grandmothers in intervention than comparison sites at endline (12.0 ± 1.7 compared with 9.8 ± 3.1, P < 0.001; maximum score = 16 points). As with grandmothers, the knowledge scores of PW and mothers were significantly higher in intervention sites (11.6 ± 1.9 compared with 10.2 ± 2.8, P < 0.001; maximum score = 16) at endline. Responses to individual nutrition questions used in deriving scores are provided for grandmothers (Table 4) and PW and MCU2 (Table 5). We found alignment not only of women's knowledge, but also of women's beliefs with those of grandmothers. Further, improvements from baseline to endline were seen in the intervention grandmothers’ attitudes and beliefs but not in those of comparison grandmothers, as illustrated by difference-in-difference analyses of attitudes toward early and exclusive BF practices (Supplemental Figures 1and2). The largest endline differences for both grandmothers and mothers clustered around timely introduction of protein-rich foods, with a higher percentage in the intervention communities indicating that infants could begin consuming eggs, fish, and legumes at age 6–7 mo. The one exception to this trend in greater knowledge of intervention communities was that a significantly lower percentage of intervention than comparison grandmothers and mothers responded correctly that children can receive thick porridge at 6–7 mo.
TABLE 4.
Percentages of grandmothers correctly responding to maternal and child nutrition knowledge questions at Mamanieva endline survey1
| Intervention (n = 157) | Comparison (n = 62) | P | |
|---|---|---|---|
| PW should eat more | 95.5 | 64.5 | <0.0001 |
| PW should work less | 93.0 | 69.4 | <0.0001 |
| Infants should breastfeed immediately after delivery | 100 | 72.6 | <0.0001 |
| Mothers should feed baby first yellow milk | 98.7 | 66.1 | <0.0001 |
| Mothers should not give baby anything before it is put to breast for first time | 96.8 | 82.3 | 0.0002 |
| Mothers should not give baby anything other than breastmilk in first week of life | 100 | 82.3 | <0.0001 |
| Baby should be aged ≥6 mo before receiving water for first time | 98.1 | 72.6 | <0.0001 |
| Baby should be 6–7 mo old before it receives light porridge for the first time | 85.4 | 72.6 | 0.0276 |
| Baby can receive thick porridge beginning at 6–7 mo | 5.7 | 41.9 | <0.0001 |
| Baby can receive eggs for the first time at 6–7 mo | 47.1 | 24.2 | 0.0018 |
| Baby can receive meat or fish for the first time at 6–7 mo | 39.5 | 22.6 | 0.0179 |
| Baby can receive vegetables or fruits for the first time at 6–7 mo | 15.3 | 21.0 | 0.3121 |
| Baby can receive mashed beans, peas, lentils, or nuts for the first time at 6–7 mo | 69.4 | 32.3 | <0.0001 |
| At 6–9 mo should be fed foods other than breastmilk ≥2–3 times/d | 100 | 98.4 | 0.1107 |
| At 9–12 mo should be fed foods other than breastmilk ≥3 times/d | 100 | 88.7 | <0.0001 |
| At 12–24 mo should be fed foods other than breastmilk ≥4 times/d | 57.3 | 67.7 | 0.1558 |
1PW, pregnant women.
TABLE 5.
Percentages of pregnant women and mothers with children aged <2 y correctly responding to maternal and child nutrition knowledge questions at Mamanieva endline survey1
| Intervention (n = 225) | Comparison (n = 150) | P | |
|---|---|---|---|
| PW should eat more | 95.6 | 70.0 | <0.0001 |
| PW should work less | 95.1 | 78.0 | <0.0001 |
| Should breastfeed immediately after delivery | 99.6 | 85.3 | <0.0001 |
| Should feed baby first yellow milk | 100 | 76.0 | <0.0001 |
| Should not give baby anything before it is put to breast for first time | 97.8 | 94.0 | 0.0587 |
| Should not give baby anything other than breastmilk in first week of life | 99.1 | 90.0 | <0.0001 |
| Baby should be aged ≥6 mo before receiving water for first time | 97.3 | 83.3 | <0.0001 |
| Baby should be 6–7 mo old before it receives light porridge for the first time | 89.8 | 82.0 | 0.0300 |
| Baby can receive thick porridge beginning at 6–7 mo | 34.2 | 62.7 | <0.0001 |
| Baby can receive eggs for the first time at 6–7 mo | 56.0 | 34.7 | <0.0001 |
| Baby can receive meat or fish for the first time at 6–7 mo | 47.1 | 36.7 | 0.0453 |
| Baby can receive vegetables or fruits for the first time at 6–7 mo | 24.4 | 24.7 | 0.9609 |
| Baby can receive mashed beans, peas, lentils, or nuts for the first time at 6–7 mo | 72.4 | 48.0 | <0.0001 |
| At 6–8.9 mo should be fed foods other than breastmilk ≥2–3 times/d | 86.2 | 90.0 | 0.2746 |
| At 9–11.9 mo should be fed foods other than breastmilk ≥3 times/d | 51.1 | 51.3 | 0.9664 |
| At 12–23.9 mo should be fed foods other than breastmilk ≥4 times/d | 18.7 | 17.3 | 0.7427 |
1PW, pregnant women.
IYCF practices in mothers with children aged <2 y
Among all children aged 0–23 mo (n = 291), we found no differences in early initiation of BF between intervention and comparison groups at endline (Table 6), although we noted a greater percentage in the intervention communities exclusively breastfed during the first week of life (90.2% compared with 79.4%, P = 0.01; Table 6). In infants aged 0–6 mo there were no significant differences in the percentage of children exclusively breastfed in the previous 24 h, nor in the percentage of those who were continuing to breastfeed in children aged 6–23 mo.
TABLE 6.
Percentages of mothers with children aged <2 y who met recommended infant and young child feeding practices at Mamanieva endline survey1
| Intervention | Comparison | P | OR (95% CI)2 | |
|---|---|---|---|---|
| Children aged 0–23 mo | (n = 184) | (n = 107) | ||
| Early BF initiation (within 1 h of birth) (0–23 mo) | 64.7 | 73.8 | 0.12 | |
| EBF first week (0–23 mo) | 90.2 | 79.4 | 0.01 | |
| Children aged 0–5.9 mo | (n = 48) | (n = 24) | ||
| EBF previous 24 h | 89.6 | 91.7 | 0.78 | |
| Children aged 6–23 mo | (n = 136) | (n = 83) | ||
| Continued BF | 74.3 | 72.3 | 0.75 | |
| MDD (≥4 food groups) | 77.2 | 51.8 | <0.001 | 3.4 (1.5, 7.8), P < 0.004 |
| MMF for age | 61.0 | 50.6 | 0.13 | |
| MAD3 | 53.8 | 22.6 | 0.001 | 3.3 (1.5, 7.2), P < 0.004 |
1Model adjusted for maternal schooling, parity and pregnancy, household head schooling and occupation, household hunger category, and child age and sex. Four infants excluded due to missing outcome or covariate data. BF, breastfeeding; EBF, exclusive breastfeeding; MAD, minimum adequate diet; MDD, minimum dietary diversity; MMF, minimum meal frequency.
n = 217 for regression analyses.
n = 168.
Regarding complementary feeding, the percentage of children aged 6–23 mo achieving MDD (77.2% compared with 51.8%, P < 0.001) and MAD (53.8% compared with 22.6%, P < 0.001) was significantly higher in the intervention group. No significant differences were observed between intervention and comparison communities for meal frequency overall. However, we noted a higher percentage of intervention infants aged 9–23 mo achieving MMF than those in the comparison group (54.6% compared with 36.9%, P = 0.02).
In adjusted analyses, children in the intervention group had higher odds of achieving MDD (OR: 3.4; 95% CI: 1.5, 7.8) and MAD (OR: 3.3; 95% CI: 1.5, 7.2) than children in comparison communities (Table 6).
Discussion
In Sierra Leone, children meeting MDD and MAD remain extremely low, and child malnutrition rates remain high (14). Past programs in Sierra Leone had not explicitly involved grandmothers. Literature suggests that successful social and behavior change strategies target >1 category of family actors, including direct influencers such as grandmothers and partners/fathers (12, 29–31). The limited effectiveness of nutrition education strategies targeting only mothers, especially in low-income contexts, suggests the need to develop and test innovative and contextualized social and behavior change approaches grounded in behavioral theory and formative research (32, 33).
Our Mamanieva project, implemented over 28 mo in southern Sierra Leone, tested 1 innovative community-based, grandmother-inclusive participatory approach (the GMIA), which explicitly engaged grandmothers as change agents for MCHN while also involving women of reproductive age. At endline, we found significantly higher percentages of children aged 6–23 mo achieving MDD and MAD in intervention communities. These differences remained significant after adjusting for influential covariates, including household food deprivation, suggesting the differences could be due to the GMIA intervention. Research in western Kenya, Malawi, and Senegal that explicitly involved grandmothers in nutrition program designs also reported improvements in some IYCF practices and/or child nutrition (10–12). In western Kenya, a study engaging grandmothers (n = 79) and fathers (n = 85) as change agents over a 6-mo period in social actions supporting IYCF practices reported improvements in child MDD in the grandmother intervention areas only, when the interaction effects of social supports were taken into account (12). In Malawi (10, 11), participatory and grandmother-inclusive approaches for improving child nutrition, along with agricultural interventions, showed significant reductions in child underweight over a 6-y period. In Senegal (9), grandmothers’ advice to mothers was more aligned with optimal IYCF practices than previous following a 12-mo intervention.
The intervention grandmothers’ significantly higher nutrition knowledge scores at endline than those of comparison communities, a reversal from baseline, also suggest that the positive IYCF practices in intervention communities are associated with grandmothers’ knowledge and support.
Recent studies in Nepal, Ghana, Rwanda, Malawi, and Cambodia have identified the pivotal role of grandmothers in supporting IYCF practices and highlight the links between grandmothers’ knowledge and IYCF practices (3, 29–31). In Nepal, cross-sectional survey data (n = 4080) testing associations between grandmothers’ knowledge and IYCF practices found the adjusted odds of optimal IYCF practices to be 2 to 4 times higher in households where grandmothers had correct knowledge compared with those with incorrect knowledge (P < 0.001) (31). In our study, we found that children were >3 times more likely to achieve MDD and MAD in the GMIA intervention, where grandmothers had higher knowledge scores, than in comparison communities.
Our findings, combined with those in the literature, have led WV and partners to replicate this GMIA in program areas in Sierra Leone, Mauritania, and Cambodia.
In our study, although reported EBF rates during the first week of life were higher in the intervention group than the comparison group at endline, we observed no differences in other BF indicators, and all reported BF indicators were high (>70%) in both intervention and comparison communities, contrary to qualitative research findings that most mothers did not practice optimal BF (8). These findings could be due in part to a social desirability bias, where respondents reported following optimal feeding practices, whereas actual beliefs and practices differed. In our formative research we found that both grandmothers and mothers initially reported following optimal BF practices, but with subsequent probing almost all reported limited EBF (8).
Limitations
An important limitation of our study is the lack of baseline IYCF practice indicators, so that differences occurring over time unrelated to the intervention and/or due to sample selection bias, cannot be ruled out. The baseline survey and ethnographic research focused on characterizing communities and households; influencers MCN knowledge, attitudes, and beliefs; and understanding culturally designated family roles and responsibilities. We found few differences in MCN attitudes at baseline between intervention and comparison communities, and those found favored comparison communities (e.g., attitudes toward EBF for 6 mo and nutrition knowledge scores). The higher levels of nutrition knowledge and attitudes in the comparison than intervention communities at baseline might be due to differences in accessibility. A portion of intervention communities could only be accessed by canoe or foot, limiting government outreach services and access to health care, and thus nutrition knowledge. This barrier was overcome during the study as WV facilitators and the grandmothers lived within the intervention communities.
Using the 2013 Sierra Leone DHS to approximate baseline IYCF practices would suggest baseline levels of children meeting MDD and MAD to be 14.5% and 7%, respectively. At the time of the endline survey (2016), the percentage of infants in our project's intervention sites meeting MDD and MAD were 77.2% and 53.8%, respectively, and in comparison sites 51.8% and 22.6%, respectively, suggesting that the intervention could have had a positive effect. However, households in DHS surveys were selected using a 2-stage cluster-randomized sampling strategy of eligible households across all sections in Bonthe. For our endline survey, although all eligible households in the 2 sections of Bonthe were included, the difference in sampling limits the use of DHS data for baseline comparisons.
Another limitation of our study was the purposive allocation to comparison and intervention groups, based largely on accessibility for staff to communities to implement project activities. Future research using a cluster-randomized design, with measurement of IYCF practices, growth, and nutritional status at baseline and endline, would allow attribution of the effects to the intervention.
Conclusions
The Mamanieva project findings suggest that, in southern Sierra Leone, a GMIA has potential to improve knowledge, attitudes, and IYCF practices of both grandmothers and mothers. These findings add to those of previous grandmother-inclusive programs in Kenya, Malawi, and Senegal, suggesting that explicitly including and building on grandmothers’ cultural roles can improve IYCF practices in non-Western contexts. They point to the importance of testing the GMIA with more rigorous designs and including not only IYCF practices but also growth and nutritional status at baseline and endline. Appropriately designed evaluations will increase confidence that empowering grandmothers and improving their knowledge of and attitudes toward recommended nutrition practices creates an enabling environment that supports optimal IYCF practices.
Supplementary Material
ACKNOWLEDGEMENTS
We are deeply grateful to the grandmothers and mothers who participated in this project, and the Bonthe District Ministry of Health who supported us. We also acknowledge the following contributions: Christina Gruenewald for project oversight and administration; Alice Senesie and Wilma Mui for program implementation and curriculum design; Evelyn Kamgang and Sarah Alberastine for contributions to the literature review; and Claire Hultquist and Loria Kulathungam for editorial review.
The authors’ responsibilities were as follows—BAA, RW, CAM, and AWG: wrote the manuscript; BAA, CAM, AWG, and JA: were involved in the study design; AWG, RW, and JA: supported data collection and analysis; JS, BAA, CAM, and AWG: provided oversight for implementation; KR: provided major revisions to manuscript; and all authors: contributed to, read, and approved the final manuscript.
Notes
Supported by World Vision Canada, World Vision Germany, and World Vision International.
Author disclosures: The authors report no conflicts of interest.
Supplemental material and Supplemental Figures 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Abbreviations used: BF, breastfeeding; CHW, community health worker; CU2, children under 2 y; DHS, Demographic and Health Surveys; EBF, exclusive breastfeeding; GMIA, grandmother-inclusive approach; GML, grandmother leader; GMP, Grandmother Project; IYCF, infant and young child feeding; MAD, minimum acceptable diet; MCHN, maternal and child health and nutrition; MCN, maternal and child nutrition; MCU2, mothers with children under 2 y of age; MDD, minimum dietary diversity; MMF, minimum meal frequency; MoH, Ministry of Health; ODK, Open Data Kit; PW, pregnant women; WV, World Vision.
Contributor Information
Bridget A Aidam, Email: bridgetaidam@gmail.com, Action Against Hunger USA. Previously of Evidence and Learning Unit, World Vision International, Washington, DC, USA.
Carolyn A MacDonald, World Vision International, Nutrition Centre of Expertise, Mississauga, Ontario, Canada.
Rebecca Wee, Hubert Department of Global Health and Nutrition, Rollins School of Public Health, Emory University, Atlanta, GA, USA.
Joseph Simba, World Vision Sierra Leone, Freetown, Sierra Leone.
Judi Aubel, Grandmother Project: Change through Culture, Rome, Italy.
Kathryn R Reinsma, World Vision International, Nutrition Centre of Expertise, Mississauga, Ontario, Canada.
Amy Webb Girard, Hubert Department of Global Health and Nutrition, Rollins School of Public Health, Emory University, Atlanta, GA, USA.
Data Availability
The data underlying this article are available in Figshare at https://doi.org/10.6084/m9.figshare.8016383.
References
- 1. Aubel J. The role and influence of grandmothers on child nutrition: culturally designated advisors and caregivers. Matern Child Nutr. 2012;8:19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scelza BA, Hinde K. Crucial contributions: a biocultural study of grandmothering during the perinatal period. Hum Nat. 2019;30:371–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gupta ML, Aborigo RA, Adongo PB, Rominski S, Hodgson A, Engmann CM, Moyer CA. Grandmothers as gatekeepers? The role of grandmothers in influencing health-seeking for mothers and newborns in rural northern Ghana. Glob Public Health. 2015;10:1078–91. [DOI] [PubMed] [Google Scholar]
- 4. Mukunya D, Nankabirwa V, Ndeezi G, Tumuhamye J, Tongun JB, Kizito S, Napyo A, Achora V, Odongkara B, Arach AA et al. Key decision makers and actors in selected newborn care practices: a community-based survey in northern Uganda. Int J Environ Res Public Health. 2019;16:1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Iganus R, Hill Z, Manzi F, Bee M, Amare Y, Shamba D, Odebiyi A, Adejuyigbe E, Omotara B, Skordis‐Worrall J. Roles and responsibilities in newborn care in four African sites. Trop Med Int Health. 2015;20:1258–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Faye CM, Fonn S, Kimani‐Murage E. Family influences on child nutritional outcomes in Nairobi's informal settlements. Child Care Health Dev. 2019;45:509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schrijner S, Smits J. Grandparents and children's stunting in sub-Saharan Africa. Soc Sci Med. 2018;205:90–8. [DOI] [PubMed] [Google Scholar]
- 8. MacDonald CA, Aubel J, Aidam BA, Girard AW. Grandmothers as change agents: developing a culturally appropriate program to improve maternal and child nutrition in Sierra Leone. Curr Dev Nutr. [Internet]2020;4(1):nzz141 Available from: 10.1093/cdn/nzz141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aubel J, Toure I, Diagne M. Senegalese grandmothers promote improved maternal and child nutrition practices: the guardians of tradition are not averse to change. Soc Sci Med. 2004;59:945–59. [DOI] [PubMed] [Google Scholar]
- 10. Bezner Kerr R, Berti PR, Shumba L. Effects of a participatory agriculture and nutrition education project on child growth in northern Malawi. Public Health Nutr. 2011;14:1466–72. [DOI] [PubMed] [Google Scholar]
- 11. Bezner Kerr R, Dakishoni L, Shumba L, Msachi R, Chirwa M. “We Grandmothers Know Plenty”: breastfeeding, complementary feeding and the multifaceted role of grandmothers in Malawi. Soc Sci Med. 2008;66:1095–105. [DOI] [PubMed] [Google Scholar]
- 12. Mukuria AG, Martin SL, Egondi T, Bingham A, Thuita FM. Role of social support in improving infant feeding practices in western Kenya: a quasi-experimental study. Glob Health-Sci Prac. 2016;4:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Statistics Sierra Leone, ICF Macro Sierra Leone demographic and health survey 2008. [Internet] Calverton (MD); 2009; [cited 2017 Dec 11] Available from: http://dhsprogram.com/pubs/pdf/FR225/FR225.pdf [DOI] [PubMed] [Google Scholar]
- 14. Statistics Sierra Leone, ICF International Sierra Leone demographic and health survey 2013. [Internet] Freetown, Sierra Leone and Rockville (MD); 2014; [cited 2018 Jul 20] Available from: https://www.dhsprogram.com/pubs/pdf/FR297/FR297.pdf [Google Scholar]
- 15. World Health Organization Indicators for assessing infant and young child feeding practices. Part 2: measurement. Geneva (Switzerland): WHO; 2010. [Google Scholar]
- 16. Bhutta Z, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?. Lancet. 2013;382:452–77. [DOI] [PubMed] [Google Scholar]
- 17. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 13;382:427–51. [DOI] [PubMed] [Google Scholar]
- 18. Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS, Maternal and Child Undernutrition Study Group . Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aubel J. Involving grandmothers to promote child nutrition, health, and development: a guide for program planners and managers. World Vision International; 2014. 108 p. [Google Scholar]
- 20. Mui W, Webb Girard A . Mamanieva formative research report: combined qualitative and quantitative baseline evaluation. [Internet] World Vision International; 2015[cited 2020 Sep 21]. Available from: https://www.wvi.org/publications/report/mamanieva-formative-research-report [Google Scholar]
- 21. Theis L, Webb Girard A . Mamanieva process evaluation report. [Internet] World Vision International; 2015; [cited 2020 Sep 21] Available from: https://www.wvi.org/publications/report/mamanieva-project-process-evaluation-report. [Google Scholar]
- 22. APA Dictionary of Psychology Unconditional positive regard. [Internet] Washington (DC): American Psychological Association [cited 2020 Nov 5] Available from: https://dictionary.apa.org/unconditional-positive-regard [Google Scholar]
- 23. Al-Rabadi H, Sharif N.. Effectiveness of timed and targeted counselling about feeding and caring practices for infants and young children to mothers in West Bank: a randomized controlled trial. Lancet. 2017;390:S23. [Google Scholar]
- 24. World Vision International TTC: a family-inclusive behavior change model for the life course. [Internet] [cited 2020 Nov 5] Available from: https://www.wvi.org/health/timed-and-targeted-counseling-ttc [Google Scholar]
- 25. Statistics Sierra Leone Homepage. [Internet] [cited 2017 Dec 11]. Available from: https://www.statistics.sl/
- 26. World Health Organization Complementary feeding. [Internet] [cited2020 Nov 13] Available from: http://www.who.int/nutrition/topics/complementary_feeding/en/
- 27. Ballard T, Coates J, Swindale A, Deitchler M. Household Hunger Scale: indicator definition and measurement guide. Washington (DC): Food and Nutrition Technical Assistance II Project, FHI 360; 2011. p. 23. [Google Scholar]
- 28. World Health Organization Indicators for assessing infant and young child feeding practices: conclusions of a consensus meeting held 6–8 November 2007 in Washington, D.C., USA. Geneva (Switzerland): WHO; 2007. [Google Scholar]
- 29. Ahishakiye J, Bouwman L, Brouwer ID, Matsiko E, Armar-Klemesu M, Koelen M. Challenges and responses to infant and young child feeding in rural Rwanda: a qualitative study. J Health Popul Nutr. 2019;38:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Muehlhoff E, Wijesinha-Bettoni R, Westaway E, Jeremias T, Nordin S, Garz J. Linking agriculture and nutrition education to improve infant and young child feeding: Lessons for future programmes. Matern Child Nutr. 2017;13(Suppl 2):e12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Karmacharya C, Cunningham K, Choufani J, Kadiyala S. Grandmothers’ knowledge positively influences maternal knowledge and infant and young child feeding practices. Public Health Nutr. 2017;20:2114–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aboud FE, Singla DR.. Challenges to changing health behaviours in developing countries: a critical overview. Soc Sci Med. 2012;75:589–94. [DOI] [PubMed] [Google Scholar]
- 33. Pelto GH, Martin SL, van Liere MJ, Fabrizio CS. Perspectives and reflections on the practice of behaviour change communication for infant and young child feeding. Matern Child Nutr. 2016;12:245–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in Figshare at https://doi.org/10.6084/m9.figshare.8016383.