Mask wearing by the public during the COVID-19 pandemic has proven to be a controversial mitigation measure. This review summarizes evidence about this practice, including whether masks work only as a source control measure or also provide protection to the wearer. Studies of the physical properties of mask materials and designs as well as physiologic and psychological effects of mask wearing are addressed. Societal debate about balancing mask mandates and personal freedom is discussed.
Abstract
Whether and when to mandate the wearing of facemasks in the community to prevent the spread of coronavirus disease 2019 remains controversial. Published literature across disciplines about the role of masks in mitigating severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission is summarized. Growing evidence that SARS-CoV-2 is airborne indicates that infection control interventions must go beyond contact and droplet measures (such as handwashing and cleaning surfaces) and attend to masking and ventilation. Observational evidence suggests that masks work mainly by source control (preventing infected persons from transmitting the virus to others), but laboratory studies of mask filtration properties suggest that they could also provide some protection to wearers (protective effect). Even small reductions in individual transmission could lead to substantial reductions in population spread. To date, only 1 randomized controlled trial has examined a community mask recommendation. This trial did not identify a significant protective effect and was not designed to evaluate source control. Filtration properties and comfort vary widely across mask types. Masks may cause discomfort and communication difficulties. However, there is no evidence that masks result in significant physiologic decompensation or that risk compensation and fomite transmission are associated with mask wearing. The psychological effects of masks are culturally shaped; they may include threats to autonomy, social relatedness, and competence. Evidence suggests that the potential benefits of wearing masks likely outweigh the potential harms when SARS-CoV-2 is spreading in a community. However, mask mandates involve a tradeoff with personal freedom, so such policies should be pursued only if the threat is substantial and mitigation of spread cannot be achieved through other means.
Key SummaryPoints
Masks and face coverings, if widely worn, may substantially reduce the spread of COVID-19.
The benefits of mask wearing seem to outweigh the harms when COVID-19 is spreading in a population.
Randomized trials are sparse and have not addressed the question of source control.
Psychological effects of masks are culturally framed and shape acceptance and adherence.
Mandated masking involves a tradeoff with personal freedom.
Whether and when to mandate the wearing of masks or face coverings in public in an effort to control the spread of coronavirus disease 2019 (COVID-19) remains controversial, and policies vary widely across countries (1). In many Asian countries, wearing masks was mandated or was already widespread from the start of the pandemic, but most Western countries initially discouraged it. The U.S. Centers for Disease Control and Prevention (2) and the World Health Organization (3) now recommend public masking in some circumstances. In this fast-moving field, what new evidence is available?
Method and Search Strategy
In a March 2020 review, we summarized available evidence and concluded that although the potential benefits of community masking seemed high and the potential for significant harm seemed low, there was almost no direct, definitive evidence either way (4). We tracked citations of that review and other early articles through Google Scholar to locate additional studies in any language up to the end of October 2020 on the grounds that citation tracking is more effective and efficient than keyword database searching when exploring a diverse literature in which terminology is used inconsistently (5). We used a narrative (hermeneutic) approach to summarize and critique key contributions (6). Reviewer feedback prompted additional targeted searches. We focused mainly but not exclusively on material published since our previous narrative review (4).
Transmission Dynamics of Severe Acute Respiratory Syndrome Coronavirus 2 Are More Complex Than Previously Believed
Infection control measures for respiratory diseases traditionally distinguish droplets (large, heavy, and believed to account for transmission within 1 to 2 meters) from aerosols (smaller, lighter, and believed to account for more distant transmission) (7). Precautions aimed at contact and droplet control include surface cleansing, handwashing, physical distancing, and wearing masks if less than 6 feet apart; those aimed at controlling airborne diseases include ventilation and wearing masks if sharing air.
Well-documented examples of transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection between persons separated by several meters (8, 9), identification of a potentially viable virus in the air after many hours (10, 11), and detailed case analyses of “superspreader events” (12) lend weight to the hypothesis that airborne spread can occur (13). There is growing evidence to support replacing an oversimplified, droplet-or-aerosol model of disease spread with one that accounts for multiple interacting influences on how the virus travels in and through the air (7, 10, 14–25) (Table 1). Milton (25) has proposed a more nuanced categorization of particles, taken from the field of environmental health (Figure and Table 2).
Table 1. Some of the Many Interacting Factors Facilitating Airborne Transmission of the SARS-CoV-2 Virus*.
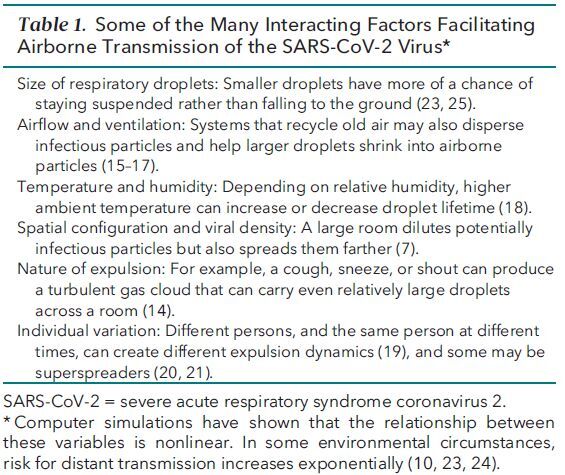
Figure. Short-range transmission potential of ballistic drops and droplet aerosols in the inhalable, thoracic, and respiratory aerosol size and the effect of facemasks as source control.
![Figure. Short-range transmission potential of ballistic drops and droplet aerosols in the inhalable, thoracic, and respiratory aerosol size and the effect of facemasks as source control. (Reproduced with permission from Milton [25].).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/beee/7774036/b733587811f6/aim-olf-M206625-M206625ff1.jpg)
(Reproduced with permission from Milton [25].).
Table 2. Summary of Particle Properties, Role in Transmission, and Implications for Infection Control.
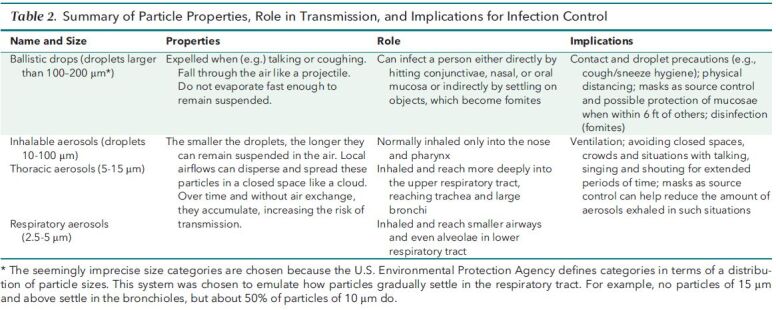
The functional receptor for SARS-CoV-2 is angiotensin-converting enzyme 2 protein, which is distributed in the oral and nasal mucosa and throughout the lungs from the trachea to the alveoli—opening up many potential entry routes for the virus (26). The smaller the particle in which the virus is carried, the deeper it can intrude into the respiratory system.
When an infected person speaks, shouts, coughs, or sneezes, the (more or less turbulent) gas cloud emitted can carry many particles of different sizes. Depending on their size, ballistic drops may fall to the ground within seconds, whereas smaller particles, aided by humidity and warmth of the exhaled air, can be carried several meters and linger in the air for extended periods (25). Four key factors influence the transmission of airborne respiratory viruses: ventilation, duration of contact, vocalization, and masking (7).
Severe acute respiratory syndrome coronavirus 2 does not spread uniformly. Many infected persons do not infect anyone else, whereas a small proportion infect many—a phenomenon known as overdispersion (κ statistic) of the reproduction number (27). The κ statistic for COVID-19 has been estimated at 0.1 to 0.45 (20, 21), indicating higher dispersion than in, for example, pandemic influenza (where κ is closer to 1, indicating that infected persons all have similar infectivity) (28). In effect, overdispersion of this magnitude means that about 10% of infectious persons, so-called superspreaders, may be responsible for about 80% of secondary transmissions (21).
Masks and Face Coverings Work as Source Control—and May Protect the Wearer
It was initially assumed that to be effective, a mask should protect the individual wearer from all or most infectious particles (29). Whereas medical masks are made to standard specifications and are intended to protect both the wearer and others, cloth face coverings vary widely in design and efficacy (30). However, as noted in 1 commentary, “The point is not that some particles can penetrate [cloth face coverings] but that some particles are stopped, particularly in the outward direction” (31).
Mathematical modeling studies have confirmed that the main benefit of population masking is source control (protecting others from particles emitted by the wearer) and have shown that if adherence is high, even small reductions in individual transmission with “imperfect” masks and face coverings could lead to large effects on population spread, especially in crowded indoor settings (32–38).
Percolation theory (which considers what happens in networks when nodes are removed) proposes that masks may cause “connection gaps” between infected and susceptible persons and spreaders, thereby increasing the threshold at which the disease becomes epidemic (39). A simulation study of transmission events (published only as a preprint so far [40]) found that if persons who infect more than 10 others are avoided, the reproduction number will decrease below 1. This suggests that interventions that can achieve this efficiently need to be prioritized—especially because 20% to 30% of persons are asymptomatic (41) and a similar proportion are presymptomatic (42, 43) when they spread the virus.
A hypothesis speculates that masking may reduce the viral inoculum to which the wearer is exposed (a phenomenon known as variolation), leading to higher rates of mild or asymptomatic infection with COVID-19 and hence, potentially, generating immunity with less risk for severe illness (44). However, human data to support this hypothesis are lacking.
Universal Masking is Associated With Fewer New Cases and Lower Mortality
Several studies have shown a strong negative correlation between the introduction of universal masking and the incidence of new COVID-19 infections. For example, the introduction of mandatory masking in many states was associated with a decline in daily COVID-19 growth rate by 0.9, 1.1, 1.4, 1.7, and 2.0 percentage points at 1 to 5, 6 to 10, 11 to 15, 16 to 20, and 21 or more days, respectively, after state facemask orders were signed (P 0.05 or less for all time periods as reported by the authors) (45). An observational study comparing 34 regions of Ontario, Canada, which introduced mask mandates on different dates, found that in the weeks after implementation, such mandates were associated with 25% fewer new cases of COVID-19 per week (46). In a study across 200 countries, in those with cultural norms or government policies supporting public masking, per capita mortality from COVID-19 increased by 16.2% per week, compared with 61.9% per week in the remaining countries (47).
All of these studies were observational, but in all cases the benefits of masking persisted after correction for potential confounding variables. A simulation modeling study estimated that universal (100%) or near-universal (85%) mask use across the United States during the pandemic could prevent 129 574 deaths (95% CI, 85 284 to 170 867 deaths) or 95 814 deaths (CI, 60 731 to 133 077 deaths), respectively, during a 5-month period (48).
Evidence From Randomized Controlled Trials Remains Sparse
A systematic review synthesized 29 adjusted and 10 unadjusted trials of masks in control of various respiratory infections and concluded that “[f]ace mask use could result in a large reduction in risk of infection” (49). However, only 3 of the included studies were done in community settings (the rest were of health care workers), and all of these related to prevention of SARS (the disease caused by SARS-CoV-1), not COVID-19 (the new disease caused by SARS-CoV-2). A living systematic review identified some additional community trials (mostly historical studies of masks to prevent influenza transmission) and highlighted the absence of experimental trials of masks for source control of COVID-19 in community settings (50).
Only 1 published randomized trial has evaluated a community mask recommendation to prevent SARS-CoV-2 infection—the DANMASK-19 (Danish Study to Assess Face Masks for the Protection Against COVID-19 Infection) trial (51). This trial was designed to evaluate only the protective effect to mask wearers and not source control. The researchers randomly assigned 6024 healthy adults in Denmark to follow local public health measures plus a recommendation to either not wear or wear a surgical mask when outside the home among others for 30 days between April and June 2020. During this time, COVID-19 infection rates were modest, social distancing was in effect, and mask wearing was uncommon outside hospitals. The mask recommendation did not decrease personal infection rates by the target of 50% that the trial was designed to detect, but results were inconclusive and compatible with an effect ranging from a 46% decrease to a 23% increase in infection. Limitations of the study have been raised (52, 53), but the greatest limitation is that it was unable to evaluate the effect of a recommendation for widespread community mask wearing that would involve both personal protection and source control. Addressing the effectiveness of masks as source control would require a more complex, larger, and lengthier trial than DANMASK-19.
Randomized controlled trials are unlikely to resolve current controversies around population masking for several reasons (54). First, mechanistic evidence from the fluid dynamics of aerosol spread and international epidemiologic data summarized in this review already strongly support the hypothesis that masks are likely to be effective in controlling the spread of the virus. Second, given this existing evidence, trials in which some persons are asked not to wear a mask may be considered unethical because the criterion of equipoise is not met. Third, if the research question relates to mask wearing as source control, the optimum design (from a scientific perspective) would be to randomly assign entire communities in a large social experiment, which in the current context would likely be both unacceptable to some and impossible to orchestrate. Fourth, given the nonlinear overdispersion (21) and percolation (39, 40) phenomena described earlier, causality would be much harder to show in a trial. Fifth, as the modeling studies have shown (32–38, 48), the incidence of new cases may be significantly reduced over time by a decrease in transmission rate, which did not reach statistical significance in the short term.
A Mask Needs to Block the Virus—and Be Comfortable
Whether the mask is worn to protect the wearer or others, 3 aspects of performance must be optimized: filtration efficiency (its ability to block the full range of hazardous particles over different levels of airflow), fit (to minimize leakage around the edges), and resistance (so the mask is not difficult to breathe through) (30, 31, 55–61). Masks undoubtedly reduce droplet spread from coughs and sneezes (23) but, to be effective, need to block smaller airborne particles too and be sufficiently comfortable and acceptable to be worn correctly and kept on for long periods (30, 31, 58–60, 62–65). Table 3 lists influences on mask performance and implications for maximizing it.
Table 3. Factors Affecting Mask Performance.
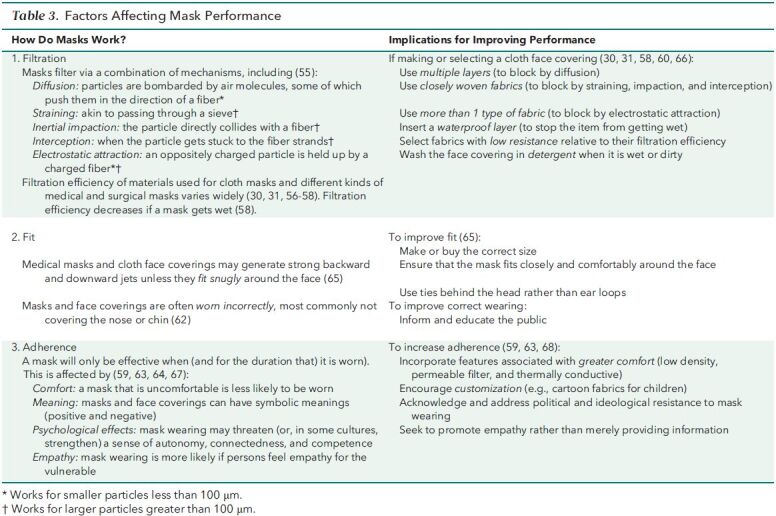
Laboratory studies have shown that both valved respirators and face shields are substantially less effective at blocking small airborne particles than either cloth or medical masks—the former because the valve (unless covered) effectively acts as an exhaust pipe and the latter because the shield may channel a powerful jet that escapes upward or downward (65, 69).
Claims of Risk Compensation and Fomite Transmission Have Not Been Substantiated
Scientists and policymakers initially expressed concern that masks or face coverings could cause risk compensation (the wearer reduces other protective behaviors out of a false sense of security) or increase risk for transmission by acting as fomites (especially if there is increased face touching followed by touching of an environmental surface) (70, 71).
A narrative review summarized evidence that refuted the risk compensation hypothesis in the examples most commonly cited by mask skeptics (cycle helmets, seat belts, and interventions to prevent sexually transmitted diseases) (72). The authors also found no evidence to support the claim that risk compensation occurs with masks or face coverings and identified 3 studies that showed that if a person is wearing a mask, protective behaviors seem to increase in those around them (73–75). A fourth study, from Germany, found no evidence of risk compensation when masks were introduced for the public (76). Video evidence from public settings (for example, stations, parks, and shopping malls) in many countries before and after the introduction of masking policies found that those wearing masks touched their faces significantly less frequently than those not wearing masks (77). A systematic review designed to identify harms from mask wearing found no evidence of risk compensation or increased face touching (71).
Although some persons argue that discarded masks could transmit COVID-19 (78), we identified no published cases of the disease being acquired this way.
Masks May Cause Discomfort and Communication Difficulties
Bakhit and colleagues' (71) systematic review identified consistent evidence of discomfort, subjective difficulty breathing, skin rashes, and headache with prolonged use of respirators and medical masks by health care workers and more limited evidence of discomfort and difficulty breathing with cloth masks. A narrative review by Scheid and colleagues (64) listed headache, skin itching, and rashes and a perception of breathlessness among health care workers who wore medical masks or respirators for prolonged periods during the COVID-19 pandemic but noted that symptoms may have been exacerbated by long working hours, stress, and anxiety. A large Polish study of self-reported symptoms among the general public found that around 20% experienced facial itching with prolonged mask wearing (79). Children seem to experience similar kinds of discomfort to adults when wearing medical masks (80).
Bakhit and colleagues' (71) review also documented reports in health care workers of difficulties in face-to-face (but not telephone) communication with all kinds of masks, although most evidence related to respirators. One trial found that only 3% of health care workers had difficulty communicating when wearing a medical mask (81). Communication while masked may be particularly challenging with young children (82), older persons (83), and those with hearing impairments (84, 85). These problems are exacerbated by physical distancing and the muffling effect of mask materials on speech (84).
There is no easy answer to the question of how to balance communication needs with the need to reduce viral transmission. Recommended strategies include speaking slowly and clearly with a minimum of background noise, encouraging use of hearing aids, and using speech-to-text technologies (84, 86), although these are not always practicable or effective. Transparent masks and modified face shields (which include a cloth apron seal around the sides and bottom [84]) allow for lip reading, but the performance of such products is largely untested. One study in health care workers found that shields were perceived as uncomfortable and cumbersome and reduced the ability to hear others (87).
Claims of Physiologic Decompensation Are Not Substantiated
We found no empirical evidence to support the claim that medical masks or cloth face coverings interfere with gas exchange to a clinically significant extent in healthy persons at rest. In nurses wearing medical masks through a 12-hour shift, no changes were seen in blood carbon dioxide or oxygen levels; minor changes in carbon dioxide levels were detected after wearing a respirator for 12 hours (88). Another study, on surgeons wearing surgical masks, showed a decrease in blood oxygen levels from 98% to 96% during prolonged surgery—a difference that was statistically significant but not clinically relevant (89).
The hypothesis that masks may cause potentially harmful physiologic changes during exercise (90) has limited empirical support (91), perhaps partly because respirators and medical masks need to comply with standards for maximum airflow resistance. Although clinically minor physiologic changes have sometimes been shown when healthy volunteers do intensive exercise while wearing tightly fitting respirators (68, 92–94), those wearing medical (94, 95) and cloth (96) masks showed no physiologic changes during moderate or intensive exercise.
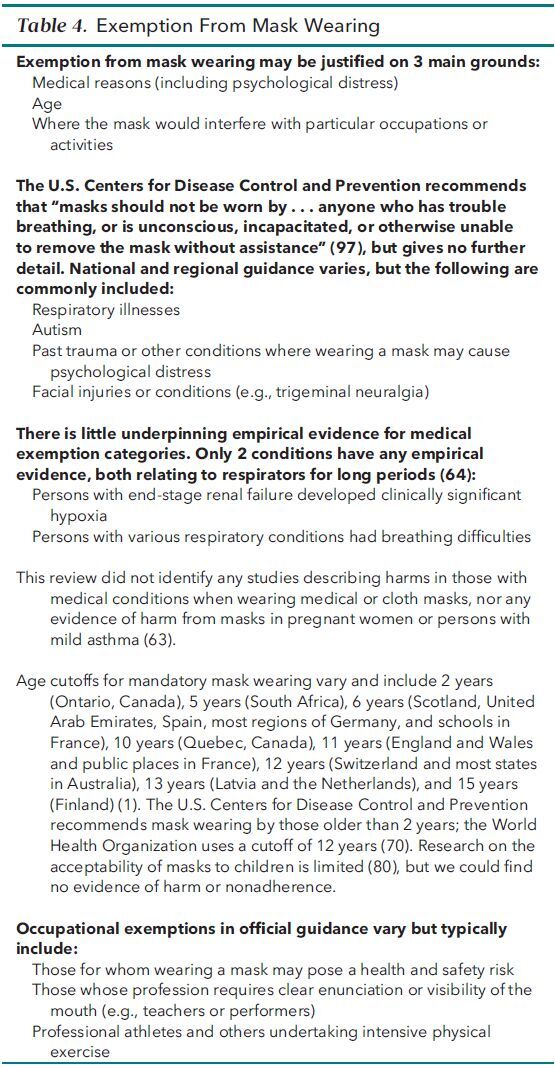
Although many policies acknowledge that some persons should be exempt from mask wearing (on the assumption that such persons could come to harm), there is no consistency—and little firm evidence—on who should be exempt (Table 4) .
Table 4. Exemption From Mask Wearing.
The Psychology of Mask Wearing Varies With Cultural Context
Scheid and colleagues (64) draw on the self-determination theory to consider the effect of mask wearing on what they call 3 universal, fundamental needs for optimal well-being: autonomy (the ability to have free will and choice over one's actions), psychological relatedness (feeling socially connected to others), and competence (the feeling that we are effective and capable and have mastery over our circumstances). Mandated mask wearing, they suggest, threatens autonomy, which may explain the high levels of resistance to such policies in some settings. Mask wearing may also threaten psychological relatedness in settings, such as the United States, where commitment to it is strongly linked to 1 political party, leading to ingroup–outgroup (us vs. them) identity issues (64). Some political and religious leaders have depicted mask wearing as female and submissive, hence inappropriate for men (64, 98). Competence, in this context, is related to people's perception of whether wearing a mask will be effective. Mixed messages about the efficacy and harms of masking in the early months of the pandemic led to confusion and lack of confidence in this intervention (64) and may partly explain occasional reports of anxiety (for example, concern about becoming infected) and perceived stigma (71).
High adherence to mask wearing in some non-Western countries is often attributed to greater conformism or collectivism but may have more complex explanations, including earlier experience of deadly epidemics, a medical tradition of using masks as protection against hay fever, and the practicalities of living with high levels of dust and atmospheric pollution (99–101). In many hot countries, both men and women traditionally wear loose pieces of cloth over the head and lower face to protect against heat and dust; such items were repurposed as protection against COVID-19 (102, 103). One Japanese anthropologist has depicted mask wearing by the Japanese as a way of restoring a sense of control in the face of uncertainties and establishing a boundary between a clean and pure inner self and a potentially polluted outside (100). For all of these reasons, mask wearing in some non-Western countries may promote rather than threaten a sense of autonomy, relatedness, and competence.
In a cultural environment where masks are common, persons may have learned to express and understand alternative cues to communicate emotions, whereas in Western societies, the readability of emotions may be hampered by masks (104). In 1 study, adherence to mask wearing was greater in those who empathized with persons who were vulnerable to COVID-19, and inducing empathy improved adherence, whereas merely informing persons of the benefits to others did not (67).
Benefits Must Be Balanced Against Harms and Acceptability
The observational studies summarized earlier (45–47, 63), along with the modeling studies (32–38, 48), suggest that across a range of scenarios the use of masks among the general public is an effective strategy in mitigating transmission of SARS-CoV-2. Even with a limited protective effect, masks can reduce total infections and deaths (especially in relation to presymptomatic transmission) and delay the peak time of the epidemic.
However, mandatory masking is unpopular with some and an infringement (albeit a relatively minor one) of individual freedom. Therefore, it should be restricted to situations where it is likely to be both effective and cost-effective (that is, when faced with a disease that is both prevalent and dangerous). It is not justified if the targeted disease is innocuous or can be prevented by other means that are more effective, more acceptable, less risky, or less expensive.
Coronavirus disease 2019 is not innocuous: It has killed millions of persons around the world (105), produced a cohort of survivors with chronic symptoms and unknown long-term prognosis (106), stretched health systems to (and sometimes beyond) their limits (107), and devastated economies (108). Voluntary masking has been successful in many Asian countries (notably Japan, South Korea, Hong Kong, and Taiwan) but less so in Western countries where the measure was less culturally acceptable (109).
Because of potential airborne transmission, COVID-19 is inherently difficult to contain. As with public masking, the effects and costs of school closures, gathering bans, border closures, quarantine regulations, travel restrictions, working from home, closing restaurants and nonessential shops, physical distancing rules, coughing etiquette, handwashing, and restricting visits to hospitals and nursing homes are difficult to quantify. Moreover, these measures play out differently and have different personal costs depending on the situation. For example, schools need to balance their duty of care to vulnerable pupils and staff with their educational mission and student welfare, which includes meeting the needs of pupils of different ages and abilities and those with (for example) autism and hearing impairments. Masking for only some groups, in some parts of schools and with exceptions granted, may be more appropriate than rigid universal mandates.
Concerns about environmental pollution from mask waste (110, 111) are well founded given that medical masks are made from petrochemicals and are nonbiodegradable. Homemade washable cloth face coverings are more environmentally friendly and may have greater cultural appeal (and hence, better adherence) (66, 109).
Conclusion
This narrative review has summarized a heterogeneous body of evidence on population masking in the context of the COVID-19 pandemic. Evidence that the virus can be airborne (and therefore be inhaled) and that masking policies, when effectively delivered, save lives is now strong. There is no evidence of serious harms from masks and face coverings, although discomfort, communication difficulties, and environmental effects are not insignificant. Psychological effects, which are culturally framed, shape acceptance and adherence.
As masking has become recommended or mandated, there is an urgent research agenda to develop alternatives that are more efficient, more comfortable, more acceptable, less disruptive of normal communication practices, and more environmentally friendly than currently available products.
Until the threat of the pandemic is behind us, we recommend that the public wear masks or face coverings in situations and settings where risk for transmission is high—notably where ventilation is poor, when large numbers of persons are gathered, when some are vocalizing (especially singing or shouting), and when contact is prolonged (7).
Footnotes
This article was published at Annals.org on 29 December 2020
* Drs. Czypionka and Greenhalgh are joint first authors.
References
- 1. Masks4All. What countries require masks in public or recommend masks? Accessed at https://masks4all.co/what-countries-require-masks-in-public on 2 December 2020.
- 2. Centers for Disease Control and Prevention. Use of masks to help slow the spread of COVID-19. Accessed at www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html on 2 December 2020.
- 3. World Health Organization. Mask use in the context of COVID-19. Accessed at https://apps.who.int/iris/bitstream/handle/10665/337199/WHO-2019-nCov-IPC_Masks-2020.5-eng.pdf?sequence=1&isAllowed=y on 2 December 2020.
- 4. Greenhalgh T , Schmid MB , Czypionka T , et al. Face masks for the public during the Covid-19 crisis. BMJ. 2020;369:m1435. [PMID: ] doi: 10.1136/bmj.m1435 [DOI] [PubMed] [Google Scholar]
- 5. Greenhalgh T , Peacock R . Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331:1064-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Greenhalgh T , Thorne S , Malterud K . Time to challenge the spurious hierarchy of systematic over narrative reviews. Eur J Clin Invest. 2018;48:e12931. [PMID: ] doi: 10.1111/eci.12931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jones NR , Qureshi ZU , Temple RJ , et al. Two metres or one: what is the evidence for physical distancing in Covid-19. BMJ. 2020;370:m3223. [PMID: ] doi: 10.1136/bmj.m3223 [DOI] [PubMed] [Google Scholar]
- 8. Guenther T, Czech-Sioli M, Indenbirken D, et al. Investigation of a superspreading event preceding the largest meat processing plant-related SARS-Coronavirus 2 outbreak in Germany. SSRN. Preprint posted online 23 July 2020. doi:10.2139/ssrn.3654517
- 9. Leclerc QJ , Fuller NM , Knight LE , et al; CMMID COVID-19 Working Group. What settings have been linked to SARS-CoV-2 transmission clusters. Wellcome Open Res. 2020;5:83. [PMID: ] doi: 10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Doremalen N, Bushmaker T, Morris DH, et al.. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1 [Letter]. N Engl J Med. 2020;382:1564-1567. [PMID: ] doi: 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ong SWX , Tan YK , Chia PY , et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610-1612. [PMID: ] doi: 10.1001/jama.2020.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Miller SL , Nazaroff WW , Jimenez JL , et al. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2020. [PMID: ] doi: 10.1111/ina.12751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Prather KA , Marr LC , Schooley RT , et al. Airborne transmission of SARS-CoV-2 [Letter]. Science. 2020;370:303-304. [PMID: ] doi: 10.1126/science.abf0521 [DOI] [PubMed] [Google Scholar]
- 14. Bourouiba L . Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. JAMA. 2020;323:1837-1838. [PMID: ] doi: 10.1001/jama.2020.4756 [DOI] [PubMed] [Google Scholar]
- 15. Li Y, Qian H, Hang J, et al. Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant. medRxiv. Preprint posted online 22 April 2020. doi:10.1101/2020.04.16.20067728
- 16. Birnir B. The build-up of aerosols carrying the SARS-CoV-2 coronavirus, in poorly ventilated, confined spaces. medRxiv. Preprint posted online 25 November 2020. doi:10.1101/2020.08.11.20173195
- 17. Chirico F , Sacco A , Bragazzi NL , et al. Can air-conditioning systems contribute to the spread of SARS/MERS/COVID-19 infection? Insights from a rapid review of the literature. Int J Environ Res Public Health. 2020;17. [PMID: ] doi: 10.3390/ijerph17176052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen LD . Effects of ambient temperature and humidity on droplet lifetime—a perspective of exhalation sneeze droplets with COVID-19 virus transmission. Int J Hyg Environ Health. 2020;229:113568. [PMID: ] doi: 10.1016/j.ijheh.2020.113568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bahl P , de Silva CM , Chughtai AA , et al. An experimental framework to capture the flow dynamics of droplets expelled by a sneeze. Exp Fluids. 2020;61:176. [PMID: ] doi: 10.1007/s00348-020-03008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adam DC , Wu P , Wong JY , et al. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat Med. 2020;26:1714-1719. [PMID: ] doi: 10.1038/s41591-020-1092-0 [DOI] [PubMed] [Google Scholar]
- 21. Endo A , Abbott S , Kucharski AJ , et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. Estimating the overdispersion in COVID-19 transmission using outbreak sizes outside China. Wellcome Open Res. 2020;5:67. [PMID: ] doi: 10.12688/wellcomeopenres.15842.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kampf G , Brüggemann Y , Kaba HEJ , et al. Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2. J Hosp Infect. 2020;106:678-697. [PMID: ] doi: 10.1016/j.jhin.2020.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vuorinen V , Aarnio M , Alava M , et al. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Saf Sci. 2020;130:104866. [PMID: ] doi: 10.1016/j.ssci.2020.104866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Feng Y , Marchal T , Sperry T , et al. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J Aerosol Sci. 2020;147:105585. [PMID: ] doi: 10.1016/j.jaerosci.2020.105585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Milton DK . A Rosetta Stone for understanding infectious drops and aerosols. J Pediatric Infect Dis Soc. 2020;9:413-415. [PMID: ] doi: 10.1093/jpids/piaa079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hamming I , Timens W , Bulthuis ML , et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus: a first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lloyd-Smith JO , Schreiber SJ , Kopp PE , et al. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fraser C , Cummings DA , Klinkenberg D , et al. Influenza transmission in households during the 1918 pandemic. Am J Epidemiol. 2011;174:505-14. [PMID: ] doi: 10.1093/aje/kwr122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization. Requirements and technical specifications of personal protective equipment (PPE) for the novel coronavirus (2019-ncov) in healthcare settings. Accessed at https://iris.paho.org/bitstream/handle/10665.2/51906/requirements-%20PPE-coronavirus-eng.pdf?sequence=1&isAllowed=y on 13 May 2020.
- 30. Clase CM , Fu EL , Ashur A , et al. Forgotten technology in the COVID-19 pandemic: filtration properties of cloth and cloth masks—a narrative review. Mayo Clin Proc. 2020;95:2204-2224. [PMID: ] doi: 10.1016/j.mayocp.2020.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Clase CM , Fu EL , Joseph M , et al. Cloth masks may prevent transmission of COVID-19: an evidence-based, risk-based approach [Editorial]. Ann Intern Med. 2020;173:489-491. doi: 10.7326/M20-2567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Eikenberry SE , Mancuso M , Iboi E , et al. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020;5:293-308. [PMID: ] doi: 10.1016/j.idm.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ngonghala CN , Iboi E , Eikenberry S , et al. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel coronavirus. Math Biosci. 2020;325:108364. [PMID: ] doi: 10.1016/j.mbs.2020.108364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kai D, Goldstein G-P, Morgunov A, et al. Universal masking is urgent in the COVID-19 pandemic: SEIR and agent based models, empirical validation, policy recommendations. arXiv. Preprint posted online 22 April 2020. arXiv:2004.13553
- 35. Silva PCL , Batista PVC , Lima HS , et al. COVID-ABS: an agent-based model of COVID-19 epidemic to simulate health and economic effects of social distancing interventions. Chaos Solitons Fractals. 2020;139:110088. [PMID: ] doi: 10.1016/j.chaos.2020.110088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fisman DN , Greer AL , Tuite AR . Bidirectional impact of imperfect mask use on reproduction number of COVID-19: a next generation matrix approach. Infect Dis Model. 2020;5:405-408. [PMID: ] doi: 10.1016/j.idm.2020.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stutt ROJH , Retkute R , Bradley M , et al. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down' in managing the COVID-19 pandemic. Proc Math Phys Eng Sci. 2020;476:20200376. [PMID: ] doi: 10.1098/rspa.2020.0376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Worby CJ , Chang HH . Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat Commun. 2020;11:4049. [PMID: ] doi: 10.1038/s41467-020-17922-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Croccolo F , Roman HE . Spreading of infections on random graphs: a percolation-type model for COVID-19. Chaos Solitons Fractals. 2020;139:110077. [PMID: ] doi: 10.1016/j.chaos.2020.110077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Althouse BM, Wenger EA, Miller JC, et al. Stochasticity and heterogeneity in the transmission dynamics of SARS-CoV-2. arXiv. Preprint posted online 27 May 2020. arXiv:2005.13689
- 41. Buitrago-Garcia D , Egli-Gany D , Counotte MJ , et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med. 2020;17:e1003346. [PMID: ] doi: 10.1371/journal.pmed.1003346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oran DP , Topol EJ . Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173:362-367. doi: 10.7326/M20-3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. He X , Lau EHY , Wu P , et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672-675. [PMID: ] doi: 10.1038/s41591-020-0869-5 [DOI] [PubMed] [Google Scholar]
- 44. Gandhi M , Beyrer C , Goosby E . Masks do more than protect others during COVID-19: reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;35:3063-3066. [PMID: ] doi: 10.1007/s11606-020-06067-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lyu W , Wehby GL . Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff (Millwood). 2020;39:1419-1425. [PMID: ] doi: 10.1377/hlthaff.2020.00818 [DOI] [PubMed] [Google Scholar]
- 46. Karaivanov A, Lu SE, Shigeoka H, et al. Face masks, public policies and slowing the spread of COVID-19: evidence from Canada. National Bureau of Economic Research working paper 27891. October 2020. Accessed at https://www.nber.org/papers/w27891 on 18 December 2020. doi:10.3386/w27891 [DOI] [PMC free article] [PubMed]
- 47. Leffler CT , Ing E , Lykins JD , et al. Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks. Am J Trop Med Hyg. 2020;103:2400-2411. [PMID: ] doi: 10.4269/ajtmh.20-1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. IHME COVID-19 Forecasting Team.. Modeling COVID-19 scenarios for the United States. Nat Med. 2020. [PMID: ] doi: 10.1038/s41591-020-1132-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chu DK , Akl EA , Duda S , et al; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973-1987. [PMID: ] doi: 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chou R , Dana T , Jungbauer R , et al. Update alert 2: masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings [Letter]. Ann Intern Med. 2020;173:132. doi: 10.7326/L20-1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bundgaard H , Bundgaard JS , Raaschou-Pedersen DET , et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers: a randomized controlled trial. Ann Int Med. 2020. [PMID: ] doi: 10.7326/M20-6817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Frieden TR , Cash-Goldwasser S . Of masks and methods. Ann Intern Med. 2020. doi: 10.7326/M20-7499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Laine C , Goodman SN , Guallar E . The role of masks in mitigating the SARS-CoV-2 pandemic: another piece of the puzzle. Ann Intern Med. 2020. doi: 10.7326/M20-7448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tufekci Z. On masks and clinical trials, Rand Paul's tweeting is just plain wrong. The New York Times. 6 November 2020. Accessed at www.nytimes.com/2020/11/06/opinion/sunday/coronavirus-masks.html on 9 November 2020.
- 55. Brosseau LM, Roland BA. N95 respirators and surgical masks. NIOSH Science Blog. 14 October 2009. Accessed at https://blogs.cdc.gov/niosh-science-blog/2009/10/14/n95 on 6 November 2020.
- 56. Rengasamy S , Eimer B , Shaffer RE . Simple respiratory protection—evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010;54:789-98. [PMID: ] doi: 10.1093/annhyg/meq044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Fischer EP , Fischer MC , Grass D , et al. Low-cost measurement of face mask efficacy for filtering expelled droplets during speech. Sci Adv. 2020;6. [PMID: ] doi: 10.1126/sciadv.abd3083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chughtai AA , Seale H , Macintyre CR . Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26. [PMID: ] doi: 10.3201/eid2610.200948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lee KP , Yip J , Kan CW , et al. Reusable face masks as alternative for disposable medical masks: factors that affect their wear-comfort. Int J Environ Res Public Health. 2020;17:6623. [PMID: ] doi: 10.3390/ijerph17186623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mishra A. Making your own Covid19 masks—a few pointers. Accessed at https://medium.com/@asit.mishra76pi/making-your-own-covid19-masks-a-few-pointers-b2f66072f9f3 on 6 November 2020.
- 61. Chua MH , Cheng W , Goh SS , et al. Face masks in the new COVID-19 normal: materials, testing, and perspectives. Research (Wash D C). 2020;2020:7286735. [PMID: ] doi: 10.34133/2020/7286735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Cumbo E , Scardina GA . Management and use of filter masks in the “none-medical” population during the Covid-19 period. Saf Sci. 2021;133:104997. [PMID: ] doi: 10.1016/j.ssci.2020.104997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mitze T, Kosfeld R, Rode J, et al. Face masks considerably reduce COVID-19 cases in Germany: a synthetic control method approach. IZA Institute of Labor Economics DP no. 13319. Accessed at http://ftp.iza.org/dp13319.pdf on 2 December 2020. [DOI] [PMC free article] [PubMed]
- 64. Scheid JL , Lupien SP , Ford GS , et al. Commentary: physiological and psychological impact of face mask usage during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6655. [PMID: ] doi: 10.3390/ijerph17186655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Viola IM, Peterson B, Pisetta G, et al. Face coverings, aerosol dispersion and mitigation of virus transmission risk. arXiv. Preprint posted online 19 May 2020. arXiv:2005.10720 [DOI] [PMC free article] [PubMed]
- 66. Centers for Disease Control and Prevention. How to store and wash masks. Accessed at www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-to-wash-cloth-face-coverings.html on 3 December 2020.
- 67. Pfattheicher S , Nockur L , Böhm R , et al. The emotional path to action: empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol Sci. 2020;31:1363-1373. [PMID: ] doi: 10.1177/0956797620964422 [DOI] [PubMed] [Google Scholar]
- 68. Fikenzer S , Uhe T , Lavall D , et al. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol. 2020;109:1522-1530. [PMID: ] doi: 10.1007/s00392-020-01704-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Verma S , Dhanak M , Frankenfield J . Visualizing droplet dispersal for face shields and masks with exhalation valves. Phys Fluids (1994). 2020;32:091701. [PMID: ] doi: 10.1063/5.0022968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. World Health Organization. Advice on the use of masks in the context of COVID-19. Accessed at www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjottfJnr3qAhU6UhUIHbVaByYQFjAAegQIBBAB&url= https%3A%2F%2Fapps.who.int%2Firis%2Frest%2Fbitstreams%2F1279750%2Fretrieve&usg=AOvVaw3OEk7GblHnLXwd5oEzXFJ1 on 8 July 2020.
- 71. Bakhit M, Krzyzaniak N, Scott AM, et al. Downsides of face masks and possible mitigation strategies: a systematic review and meta-analysis. medRxiv. Preprint posted online 19 June 2020. doi:10.1101/2020.06.16.20133207. [DOI] [PMC free article] [PubMed]
- 72. Mantzari E , Rubin GJ , Marteau TM . Is risk compensation threatening public health in the Covid-19 pandemic. BMJ. 2020;370:m2913. [PMID: ] doi: 10.1136/bmj.m2913 [DOI] [PubMed] [Google Scholar]
- 73. Marchiori M. COVID-19 and the social distancing paradox: dangers and solutions. arXiv. Preprint posted online 26 May 2020. arXiv:2005.12446
- 74. Seres G, Balleyer AH, Cerutti N, et al. Face masks increase compliance with physical distancing recommendations during the COVID-19 pandemic. Argument. 2020;20:44.
- 75. Seres G, Balleyer AH, Cerutti N, et al. Face mask use and physical distancing before and after mandatory masking: evidence from public waiting lines. SSRN. Preprint posted online 2 July 2020. doi:10.2139/ssrn.3641367 [DOI] [PMC free article] [PubMed]
- 76. Kovacs R, Dunaiski M, Tukiainen J. Compulsory face mask policies do not affect community mobility in Germany. EconStor. Preprint posted online 5 June 2020. http://hdl.handle.net/10419/218945
- 77. Chen YJ , Qin G , Chen J , et al. Comparison of face-touching behaviors before and during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3:e2016924. [PMID: ] doi: 10.1001/jamanetworkopen.2020.16924 [DOI] [PubMed] [Google Scholar]
- 78. Martin GP, Hanna E, Dingwall R. Face masks for the public during Covid-19: an appeal for caution in policy. Accessed at www.dora.dmu.ac.uk/bitstream/handle/2086/19526/Face%20masks%20caution%20in%20policy_v1_2020-04-22%20%28with%20disclaimers%29.pdf on 27 April 2020.
- 79. Szepietowski JC , Matusiak L , Szepietowska M , et al. Face mask-induced itch: a self-questionnaire study of 2,315 responders during the COVID-19 pandemic. Acta Derm Venereol. 2020;100:adv00152. [PMID: ] doi: 10.2340/00015555-3536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Smart NR , Horwell CJ , Smart TS , et al. Assessment of the wearability of facemasks against air pollution in primary school-aged children in London. Int J Environ Res Public Health. 2020;17. [PMID: ] doi: 10.3390/ijerph17113935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. MacIntyre CR , Seale H , Dung TC , et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5:e006577. [PMID: ] doi: 10.1136/bmjopen-2014-006577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shack AR , Arkush L , Reingold S , et al. Masked paediatricians during the COVID-19 pandemic and communication with children. J Paediatr Child Health. 2020;56:1475-1476. [PMID: ] doi: 10.1111/jpc.15087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Knollman-Porter K , Burshnic VL . Optimizing effective communication while wearing a mask during the COVID-19 pandemic. J Gerontol Nurs. 2020;46:7-11. [PMID: ] doi: 10.3928/00989134-20201012-02 [DOI] [PubMed] [Google Scholar]
- 84. Wolfe J, Smith J, Neumann S, et al. Optimizing communication in schools and other settings during COVID-19. Hear J. 2020;73:40-2. doi:10.1097/01.HJ.0000717184.65906.b9
- 85. Grote H , Izagaren F . Covid-19: the communication needs of D/deaf healthcare workers and patients are being forgotten. BMJ. 2020;369:m2372. [PMID: ] doi: 10.1136/bmj.m2372 [DOI] [PubMed] [Google Scholar]
- 86. Eby TL , Arteaga AA , Spankovich C . Otologic and audiologic considerations for COVID-19. Otolaryngol Head Neck Surg. 2020;163:110-111. [PMID: ] doi: 10.1177/0194599820928989 [DOI] [PubMed] [Google Scholar]
- 87. Alzunitan MA , Perencevich EN , Edmond MB . Assessing health care worker perceptions of face coverings during the COVID-19 pandemic. Am J Infect Control. 2020. [PMID: ] doi: 10.1016/j.ajic.2020.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Rebmann T , Carrico R , Wang J . Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am J Infect Control. 2013;41:1218-23. [PMID: ] doi: 10.1016/j.ajic.2013.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Beder A , Büyükkoçak U , Sabuncuoglu H , et al. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia (Astur). 2008;19:121-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 90. Chandrasekaran B , Fernandes S . “Exercise with facemask; are we handling a devil's sword?” A physiological hypothesis. Med Hypotheses. 2020;144:110002. [PMID: ] doi: 10.1016/j.mehy.2020.110002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Greenhalgh T , Dijkstra P , Jones N , et al. Exercising and face masks: an important hypothesis buried in a selective review [Letter]. Med Hypotheses. 2020;144:110255. [PMID: ] doi: 10.1016/j.mehy.2020.110255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Roberge RJ , Coca A , Williams WJ , et al. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010;55:569-77. [PMID: ] [PubMed] [Google Scholar]
- 93. Roberge RJ , Kim JH , Benson SM . Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir Physiol Neurobiol. 2012;181:29-35. [PMID: ] doi: 10.1016/j.resp.2012.01.010 [DOI] [PubMed] [Google Scholar]
- 94. Epstein D , Korytny A , Isenberg Y , et al. Return to training in the COVID-19 era: the physiological effects of face masks during exercise. Scand J Med Sci Sports. 2021;31:70-75. [PMID: ] doi: 10.1111/sms.13832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Person E , Lemercier C , Royer A , et al. Effect of a surgical mask on six minute walking distance. Rev Mal Respir. 2018;35:264-268. [PMID: ] doi: 10.1016/j.rmr.2017.01.010 [DOI] [PubMed] [Google Scholar]
- 96. Shaw K , Butcher S , Ko J , et al. Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. Int J Environ Res Public Health. 2020;17. [PMID: ] doi: 10.3390/ijerph17218110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Centers for Disease Control and Prevention. Considerations for wearing masks. Accessed at www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html on 7 November 2020.
- 98. Harsin J. Toxic White masculinity, post-truth politics and the COVID-19 infodemic. European Journal of Cultural Studies. 2020;23:1060-8. doi:10.1177/1367549420944934
- 99. Hansstein FV , Echegaray F . Exploring motivations behind pollution-mask use in a sample of young adults in urban China. Global Health. 2018;14:122. [PMID: ] doi: 10.1186/s12992-018-0441-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Horii M. Why do the Japanese wear masks? Electronic Journal of Contemporary Japanese Studies. 2014;14:1-14.
- 101. Baehr P. City under siege: authoritarian toleration, mask culture, and the SARS crisis in Hong Kong. In: Ali SH, Keil R, eds. Networked Disease: Emerging Infections in the Global City. Wiley; 2008:138-51.
- 102.From veils to turbans: face coverings in African cultures. Accessed at www.dw.com/en/from-veils-to-turbans-face-coverings-in-african-cultures/g-53340557 on 10 July 2020.
- 103. Jindal SK, Aggarwal AN, Christopher DJ, et al. Cloth face covers—a sustainable measure to mitigate COVID-19. Accessed at https://theunion.org/sites/default/files/2020-09/IJTLD-June-0220_Letter_Jindal-FINAL.pdf on 2 December 2020. [DOI] [PubMed]
- 104. Carbon CC . Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. 2020;11:566886. [PMID: ] doi: 10.3389/fpsyg.2020.566886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Worldometer. Coronavirus cases. Accessed at www.worldometers.info/coronavirus/#countries on 2 December 2020.
- 106. Greenhalgh T , Knight M , A'Court C , et al. Management of post-acute Covid-19 in primary care. BMJ. 2020;370:m3026. [PMID: ] doi: 10.1136/bmj.m3026 [DOI] [PubMed] [Google Scholar]
- 107. European Observatory on Health Systems and Policies. COVID-19 health system response monitor. Accessed at www.covid19healthsystem.org/mainpage.aspx on 9 September 2020.
- 108. OECD. OECD economic outlook, June 2020. Accessed at www.oecd.org/economic-outlook on 9 September 2020.
- 109. van der Westhuizen HM, Kotze K, Tonkin-Crine S, et al.. Face coverings for Covid-19: from medical intervention to social practice. BMJ. 2020;370:m3021. [PMID: ] doi: 10.1136/bmj.m3021 [DOI] [PubMed] [Google Scholar]
- 110. Das O , Neisiany RE , Capezza AJ , et al. The need for fully bio-based facemasks to counter coronavirus outbreaks: a perspective. Sci Total Environ. 2020;736:139611. [PMID: ] doi: 10.1016/j.scitotenv.2020.139611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Fadare OO , Okoffo ED . Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci Total Environ. 2020;737:140279. [PMID: ] doi: 10.1016/j.scitotenv.2020.140279 [DOI] [PMC free article] [PubMed] [Google Scholar]


