Abstract
Thromboembolic phenomenon related to Coronavirus disease 2019 (COVID-19) has been well documented in literature; however, reported ocular manifestations of COVID-19 are limited to vision sparing ocular conditions like conjunctivitis. We report a case of a 17-year-old female who presented to us with central retinal vein occlusion with proven recent past COVID-19 infection as presumed etiology which was not known to her at the time of presentation.
Keywords: Central retinal vein occlusion, coronavirus, covid19, ocular manifestations of covid-19
Coronavirus disease 2019 (COVID-19) has become a global pandemic caused by the highly transmissible severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with numerous reports of redness of eye, irritation, and conjunctivitis in COVID-19 patients. Wu P et al.[1] in their study describing ocular manifestations in Covid-19 patients found, two (16.7%) patients had positive results of SARS-CoV-2 on reverse-transcriptase polymerase chain reaction (RT-PCR) by a conjunctival swab as well as by nasopharyngeal swabs, and the authors noted that patients with ocular symptoms had higher white blood cell and neutrophil counts, C-reactive protein, and higher levels of procalcitonin and lactate dehydrogenase compared to patients without ocular abnormalities. Other reports note findings of conjunctivitis or redness of eye.[2,3] We report a case of central retinal vein occlusion (CRVO) in a young adolescent female with proven past history of Covid-19 disease being the possible etiology. To the best of our knowledge, no other case of CRVO has been reported in Covid-19 positive patients in literature.
Case Report
A 17-year-old girl presented to us with diminished vision since 2 days in her right eye. She had a history of Polycystic ovaries for which she was not taking any medications. Her best-corrected visual acuity (BCVA) was 6/24, N24 in the right eye (OD) and 6/6 in the left eye (OS) on Snellen's chart. Intraocular pressure was 16 and 18 mmHg in OD and OS, respectively. On examination, anterior segment was quiet, and on dilated evaluation, OD showed disc swelling with splinter hemorrhages, and multiple flame-shaped and blot hemorrhages were seen in all quadrants in the retina [Fig. 1a and b] and a normal fundus in OS. Optical Coherence Tomography (OCT) showed neurosensory detachment and cystoid macular edema [Fig. 1c].
Figure 1.
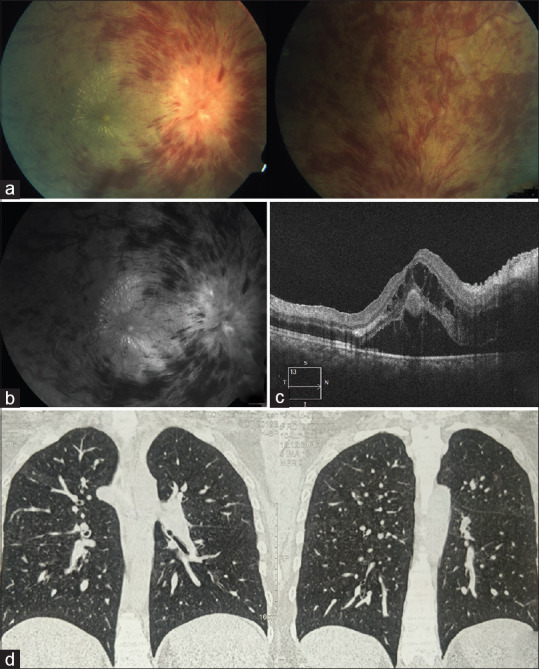
(a) Color and (b) red-free fundus images of OD showing optic disc edema and multiple hemorrhages in all quadrants with a macular star. (c) Optical coherence tomography scan of macula shows neurosensory detachment and cystoid macular edema. (d) Computed tomography scan of the chest showing multiple ground glass opacities
A diagnosis of CRVO was made and following blood reports were done: complete blood count with erythrocyte sedimentation rate, rheumatoid factor, peripheral smear, lipid profile, antinuclear antibody, urine routine micro, blood sugars, angiotensin converting enzyme, serum homocysteine, blood urea nitrogen, serum osmolality, serum creatinine, D-dimer, and were found to be within normal limits. Chest computed tomography scan [Fig. 1d] showed ground glass appearance consistent with COVID-19, but the RT PCR for Covid-19 tested negative in her case.
The patient's mother was COVID-19 positive on RT-PCR and was discharged from the hospital after testing negative a day before the patient presented to us. The patient and the rest of her family had symptoms of cough and fever 21 days before presentation for which they had taken antibiotics, nonsteroidal antiinflammatory agents, and homeopathic medication (Arsenic album). The said symptoms were relieved in 2 days with the medication. The patient was then subjected to Covid-19 Immunoglobulin test, and the test came back positive for IgG against Novel Coronavirus 2019 suggestive of past infection of COVID-19. Based on the above observations, a presumptive diagnosis of CRVO possibly secondary to COVID-19 infection was made. The patient was given intravitreal injection of Ranibizumab 0.05 mL of 10 mg/mL concentration with due precautions. On 1-month follow-up, following the first dose of injection, significant resolution of signs of CRVO was observed and BCVA in OD was 6/18, N10 [Fig. 2 left-side images]. She was advised a second dose of intravitreal anti-VEGF injection, which she received immediately. She came for next follow-up 1 month after the second injection, and her OD fundus showed further resolution of signs of CRVO and macular edema appeared resolved [Fig. 2 right-side images]. Her OD BCVA improved to 6/12, N8. She was advised a third dose of intravitreal anti-VEGF injection and received it at this visit. Her further follow-up after the third injection is due.
Figure 2.
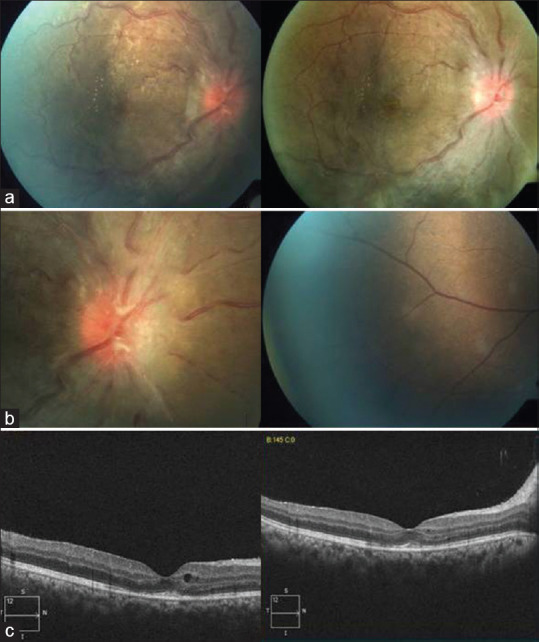
(a) Color fundus photo of the right eye showing resolution of signs after the first injection on the left and further resolution after the second injection in the image on the right. (b) Disc photo shows resolving disc edema after the first injection on the left side and resolved peripheral retinal hemorrhages after the second injection in the right-side image. (c) OCT of macula of the right eye shows dramatic resolution of CME after the first injection in the left-side image and near total resolution of CME with mild RPE atrophy and ellipsoid layer thinning noted in the right-side image
Discussion
Intraocular manifestations of COVID-19 have not been reported widely yet. Marinho et al.[4] reported hyperreflective lesions at the level of ganglion cell and inner plexiform layers more prominently at the papillomacular bundle in 12 adults (six men and six women, aged 25–69 years), examined 11–33 days after COVID-19 symptom onset. Bikdeli et al.[5] have suggested that COVID-19 may predispose patients to arterial and venous thrombosis and that initial series suggest that the occurrence of venous thromboembolic disease in patients with severe COVID-19 is common. A unique series of three young patients, less than 41 years of age with COVID-19 presenting with cerebral venous system thrombosis was reported by Calvalcanti et al.[6] Presently, the incidence of venous thromboembolic phenomena is estimated at around 25% of patients hospitalized in the intensive care unit for COVID-19 even under anticoagulant treatment at prophylactic doses. Ocular manifestations have been reported to be the first sign of COVID-19[7] Apart from conjunctivitis, feline coronaviruses were noted to cause granulomatous anterior uveitis, choroiditis with retinal detachment, and retinal vasculitis,[8] but our case had no positive inflammatory markers. COVID-19 is now being understood also as a thromboembolic disease affecting multiple organs.[9] D-dimer has been observed to be very high in patients with COVID-19 with a 10-fold increase in D-dimer compared to interleukin-6 reflecting true thrombotic disease, possibly induced by cellular activation triggered by the virus. Many different studies have shown a strong association between elevated D-dimer levels vis-à-vis severity and prognosis of disease with specific concerns about thrombotic complications of COVID-19 like pulmonary embolism, stroke, disseminated intravascular coagulation, limb, and digit infarcts.[9,10] Cutaneous and pulmonary microvascular injury with thrombosis as elicited by pathology brings to light issues with regards to thrombosis.[11] As per hypothesis postulated by some authors,[12] the involvement of microvasculature may lead to a new whole spectrum of eye diseases due to the fact that the retinal circulation is an end arterial system, which is of clinical significance because of the potentially vision-threatening nature of retinal vascular diseases.
Conclusion
We present this as an interesting case report of CRVO with previously undiagnosed recent COVID-19 infection as the presumptive etiology in the absence of any other known etiological factors. This has implications in terms of the eye surgeons being aware of COVID-19-related thromboembolic phenomena as a cause for CRVO with attendant possibilities of therapeutic options being different and also the need for looking for this in new cases of CRVO especially if a new cluster is seen. This also reiterates the need for protocols for personal protection of ophthalmologists even in “non-COVID” patients presenting with CRVO, who could have a possible underlying undiagnosed active or past coronavirus 2019 disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei province, China. JAMA Ophthalmol. 2020;138:575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marinho PM, Marcos AAA, Romano AC, Nascimento H, Belfort R., Jr Retinal findings in patients with COVID-19. Lancet. 2020;395:1610. doi: 10.1016/S0140-6736(20)31014-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950–73. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cavalcanti DD, Raz E, Shapiro M, Dehkharghani S, Yaghi S, Lillemoe K, et al. Cerebral venous thrombosis associated with COVID-19. Am J Neuroradiol. 2020;41:1370–6. doi: 10.3174/ajnr.A6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daruich A, Martin D, Bremond-Gignac D. Ocular manifestation as first sign of coronavirus disease 2019 (COVID-19): Interest of telemedicine during the pandemic context. J Fr Ophtalmol. 2020;43:389–91. doi: 10.1016/j.jfo.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28:391–5. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oudkerk M, Büller HR, Kuijpers D, van Es N, Oudkerk SF, McLoud T, et al. Diagnosis, prevention, and treatment of thromboembolic complications in COVID-19: Report of the National Institute for Public Healthof the Netherlands. Radiology. 2020;297:E216–22. doi: 10.1148/radiol.2020201629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magro C, Justin Mulvey J, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Trans Res. 2020;220:1–3. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho D, Low R, Tong L, Gupta V, Veeraraghavan A, Agrawal R. COVID-19 and the ocular surface: A review of transmission and manifestations. Ocul Immunol Inflamm. 2020;28:726–34. doi: 10.1080/09273948.2020.1772313. [DOI] [PubMed] [Google Scholar]


