A 25-year-old male presented with decreased vision 2 days after right eye open globe injury (OGI) repair. Patient's records mentioned OGI (Type A Zone I Grade III)[1] OD following a trivial blunt trauma while rubbing his eye by his finger. The patient denied any other history of ocular trauma. On ocular examination, his best corrected visual acuity was 20/400 OD (+11.0 DS/-4.5 × 90 DC) and 20/30 OS (-3.5 × 90 DC). Slit-lamp examination revealed repaired limbal perforation in the right eye, with iatrogenic superior aniridia [Fig. 1a]. There was presence of 360° peripheral corneal thinning adjacent to limbus, with superficial vascularization and lipid deposition at its leading edge in both eyes [Fig. 1b-f]. Corneal thinning was maximum in superior cornea, with intact overlying epithelium. Crystalline lens was absent in the right eye; and might have expulsed at the time of primary repair. Fundus examination and systemic history were unremarkable. Corneal topography revealed “against-the-rule” corneal astigmatism of 4.8 Diopters OS (K1 = 41.6D@92.6°; K2 = 46.4D@ 2.6°) [Fig. 2]. Anterior segment optical coherence tomography of the left eye revealed peripheral corneal thinning [Fig. 3]. Both the investigations were distorted for right eye. A diagnosis of bilateral Terrien's Marginal Degeneration (TMD) was made. Advanced TMD led to globe rupture in the area of superior thinning following eye rubbing in our patient. Patient was kept under close observation and planned for sclerokeratoplasty with aniridia scleral-fixated intraocular lens OD.
Figure 1.
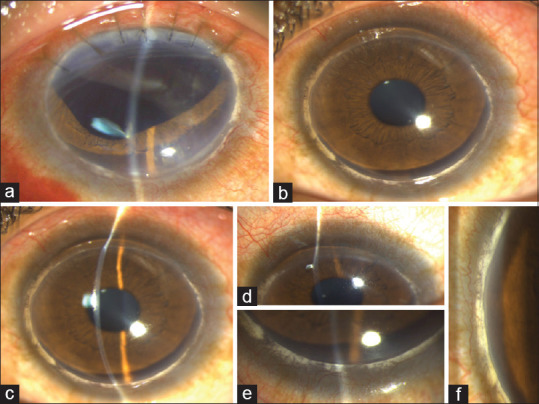
(a) Slit lamp photograph OD showing repaired limbal perforation, superior aniridia and aphakia. (b) Slit lamp photograph OS (diffuse illumination) showing 360° peripheral corneal thinning, maximum in the superior cornea. (c) Slit illumination OS showing superior stromal thinning. (d) Superior stromal thinning with a clear zone separating the limbus and intact overlying epithelium. (e) Lipid deposition with superficial vascularization at the inferior limbus. (f) Extensive lipid deposition with superficial vascularization at nasal limbus OS
Figure 2.

Four refractive maps of the left eye on Pentacam (Oculus GmBH, Germany) showing corneal astigmatism of 4.8 Diopters, peripheral corneal thinning (maximum at superior limbus) and 570 μm corneal thickness at apex
Figure 3.

Anterior segment optical coherence tomography (Casia2, Tomey GmBH, Germany) of the left eye showing peripheral corneal thinning (superior and inferior)
Discussion
TMD is a rare, slowly progressive, bilateral peripheral ectatic disorder seen in males in third to fifth decade of life. It may cause decreased vision due to “against- the-rule” astigmatism.[2,3] Imbalance in corneal homeostasis has been believed to cause corneal stromal loss in TMD, causing spontaneous perforation in 9% of such cases.[4,5] Early diagnosis and close observation is essential in TMD to prevent ocular injuries spontaneously or following trivial trauma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, Bridges WZ, Jr, Capone A, Jr, Cardillo JA, Jr, et al. A system for classifying mechanical injuries of the eye (globe) Am J Ophthalmol. 1997;123:820–31. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 2.Doggart JH. Marginal degeneration of the cornea. Br J Ophthalmol. 1930;14:5106. doi: 10.1136/bjo.14.10.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Austin P, Brown SI. Inflammatory Terrien's marginal corneal disease. Am J Ophthalmol. 1981;92:189–92. doi: 10.1016/0002-9394(81)90768-6. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan S, Murphy CC, Fisher AC, Freeman LB, Kaye SB. Terrien marginal degeneration presenting with spontaneous corneal perforation. Cornea. 2006;25:977–80. doi: 10.1097/01.ico.0000226367.41925.ab. [DOI] [PubMed] [Google Scholar]
- 5.Hafezi F, Gatzioufas Z, Seiler TG, Seiler T. Corneal collagen cross-linking for Terrien marginal degeneration. J Refract Surg. 2014;30:498–500. doi: 10.3928/1081597X-20140527-02. [DOI] [PubMed] [Google Scholar]


