Abstract
Purpose:
To evaluate the impact of 2019 COVID-19 pandemic, national lockdown, and unlocking on ophthalmic care provided by the government-funded apex health institute of India.
Methods:
Retrospective review of electronic medical records of all patients presenting to the ophthalmology department from March 23, 2020, to July 15, 2020, was compared with that from March 23, 2019, to July 15, 2019. The data between March 23, 2020, to May 31, 2020 (lockdown) and June 06, 2020, to July 15, 2020 (unlock) was compared separately. Parameters evaluated were age, gender, presenting complaints, final diagnosis, treatment advised, and surgical interventions.
Results:
During the lockdown, routine outpatient flow reduced by 97.14% (P < 0.001), the median age of presentation decreased to 29 years (55 years last year) and males increased by 4.7% (from 61.51% to 66.21%) in 2020. Emergency services decreased by 35.25%, percentage of children decreased by 4.28% (from 34.28% to 30%) and males increased by 13.53% (from 59.97% to 73.5%). Mechanical trauma, microbial keratitis, and conjunctivitis were the most common reasons for presentation. The former lessened by 41.75% while the latter two amplified by 1.25 times and 2 times, respectively. While sanitizer-associated chemical injury increased in proportion, endophthalmitis, and postoperative complications declined. The number of donor corneas collected and emergency therapeutic keratoplasties performed decreased by 99.61% and 92.39%, respectively (P < 0.001). During the unlocking phase, routine patient consultations were 71 ± 19/day, significantly lower than 978 ± 109/day of last year (P < 0.001). No voluntary eye donation was reported during this period.
Conclusion:
COVID-19 pandemic and national lockdown severely hampered the delivery of ophthalmic care by the apex-ophthalmic institute. Unlike anticipated, lifting of pandemic-associated lockdown served only minimally in improving patient inflow in its initial phases.
Keywords: COVID-19, eyebank, lockdown, microbial keratitis, SARS CoV-2; unlock
The emergence of recent COVID-19 pandemic infection induced by a highly contagious severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) has inflicted the entire world in a dreadful way and India is no exception.[1] The disease has affected more than one million individuals in the country and the numbers are still rising. In order to mitigate the unprecedented spread of the virus, a nation-wide lockdown was imposed beginning from March 25, 2020, in multiple phases, as a result of which, nonessential services including outpatientservices in the hospitals were temporarily shut down.[2] Only emergency and lifesaving procedures and essential items (medicines and food supplies) were allowed to continue. Besides, behavioral change measures like strict social distancing, frequent hand-washing, and wearing face masks, etc., were recommended strongly.
Various regions of the country were divided into different zones based on the prevalence of the disease; namely; green zone (districts having zero confirmed cases of coronavirus in the last 21 days), red zones/hotspot (districts with several active cases, high doubling rates of confirmed cases), orange zones (zones which are neither red nor green) and red zones containment areas (areas demarcated within red zones and orange zones by the district administration based on mapping and geographical dispersion of cases and contacts).[3] Based on this data, the process of partial unlocking began from June 1, 2020, onwards with a further extension of lockdown continuing in only the containment zones. While the lockdown worked positively towards curtailing an incessant spike of fatalities, the financial and geographical constraints profoundly vandalized the routine and emergency health care services, especially in hard-hit red zones.
The health sector, including the ophthalmic community, has been constantly guiding the country during this critical time, simultaneously facing extraordinarily challenges.[4] We performed a retrospective comparative study to evaluate the impact of the COVID-19 pandemic, national lockdown, and the process of unlocking on ophthalmic care provided by the apex tertiary “care” institute.of India.
Methods
This retrospective comparative study was conducted at the apex ophthalmic centre of the country. The study adhered to the tenets of the Declaration of Helsinki and at all times during the study, precautions recommended by well-established national societies were followed to prevent cross-infection.[5] These included reduction of the workforce, regular sanitization, active involvement of community ophthalmologists and infectious disease specialists, provision of adequate personal protective equipment for staff, entry point screening of patients for temperature and signs and symptoms of COVID-19, constant supervision in waiting halls for minimizing overcrowding and maintaining recommended social distancing norms.[6] Routine outpatient department (OPD) consultations, refraction, elective major and minor surgeries, and donor cornea retrieval were downsized to limit patient mobility. Community surveys and regular screening camps conducted in schools and in diabetic patients were also halted temporarily. Patients with pre-booked appointments were traced with video and audio-based teleconsultations, triaged as recommended by the largest ophthalmic community of India and advised to consult for appropriate medical help whenever deemed necessary.[5] Specialty clinics at our center including those pertaining to retina, cornea, lens, oculoplasty, squint, glaucoma, ocular oncology, low vision aids, neuro-ophthalmology, contact lenses, and pediatric ophthalmology were also suspended for the time being and all patients requiring specialty clinic referral were dealt by clinicians experienced in respective fields at the same time. Those patients who were operated before the closure of routine services were followed up separately as they needed multiple visits. As soon as their condition stabilized, they were managed by video-consultations and hospital visits planned only if needed. From May 26, 2020, onwards, the OPD was open for online appointments, and from 8th June onwards, even walk-in patents were allowed. Individuals presenting to emergency services were admitted only if they had an imminent risk of vision loss. Donor eye collection was resumed from July 3, 2020, onwards based on the All India Ophthalmological Society guidelines.[7]
A retrospective review of electronic medical records of all patients presenting to the ophthalmology department between March 25, 2020, and July 15, 2020, was performed. These data were compared with the analogous data of last year, that is, from March 25, 2019, to July 15, 2019. Also compared was data between March 25, 2020, to May 30, 2020 (lockdown) and June 1, 2020, to July 15, 2020 (unlock). The data assessed represented routine OPD services (new patients only), emergency OPD services (new patients only), routine inpatient department (IPD) services, emergency IPD services, investigational laboratories, teleconsultation, and eye bank services. Patients who needed multiple visits (postop follow-up, trauma cases, etc.,) were counted as single patients. Parameters evaluated were age, gender, presenting complaints, final diagnosis, treatment advised, and surgical interventions.
The data were compared statistically taking all gazetted and restricted holidays and Sundays into consideration. Continuous variables were expressed as mean (±standard deviation) or median (Range). P-value <0.005 was deemed statistically significant.
Results
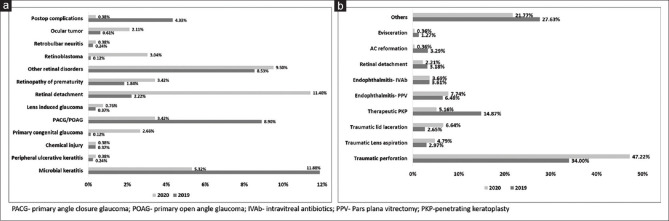
Outpatient department
The total number of routine outpatient visits decreased by 97.14% (978 ± 109/day vs 71 ± 19/day, P < 0.001) [Table 1]. As demonstrated in Fig. 1, patient inflow increased from May 26, 2020, onwards, but the recovery rate was nowhere near last year (P < 0.001). The median age of presentation fell to 29 years (0–78 years) compared to 55 years (0–92 years) in the previous year. Also noted was a 4.7% rise in the total number of males (61.51% vs 66.21%) and a 0.47% rise in the total number of children (14.75% vs 15.22%) this year.
Table 1.
Tabulated representation of retrospective comparison of data
| Category | 25th March-15th July 2019 | 25th March-15th July 2020 |
|---|---|---|
| Outpatient department | ||
| Routine OPD | 1,02,697 | 2,936 |
| Adults | 87,548 (53058M, 34490F) | 2,489 (1644M, 845F) |
| Children | 15,149 (10021M, 5128F) | 447 (300M, 147F) |
| Specialty clinics | 40,356 | -- |
| Routine refraction | 20,348 | -- |
| Emergency | 3,398 | 2,200 |
| Adults | 2233 (1339M, 894F) | 1,540 (1155M, 385F) |
| Children | 1165 (699M, 466F) | 660 (462M, 198F) |
| Medicolegal cases | 26 | 39 |
| Investigations | 1,15,683 | 2,415 |
| Teleconsultation | - | 2,616 |
| Inpatient department | ||
| Total number | 6779 | 722 |
| Elective | 5,423 | 262 |
| Emergency | 1,179 | 452 |
| Medicolegal cases | 3 | 1 |
| Employment health scheme | 174 | 7 |
| Surgeries | ||
| Elective major | 8932 | 162 |
| Elective minor | 4,686 | -- |
| Laser-based procedures | 3114 | 105 |
| Emergency major | 947 | 277 |
| Emergency minor | 818 | 450 |
| Eyebank related | ||
| Donor cornea collected | 515 | 02 |
| Emergency PKP performed | 184 | 14 |
M=Male, F=Female, PKP=Penetrating keratoplasty
Figure 1.
Week wise comparison of routine outpatient department data
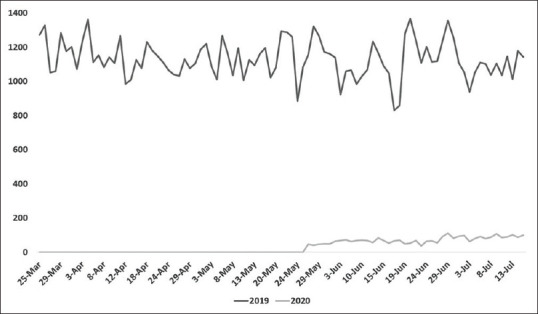
The emergency outpatient visits declined by 35.25%. During both the years, around two-thirds of patients were <40 years of age [Fig. 2] and the median age of presentation fell only marginally from 29 years (10 days to 85 years) last year to 27 years (11 days to 78 years) this year in emergency OPD. The percentage of children presenting to emergency decreased from 34.28% to 30% while the total representation of males increased significantly from 59.97% to 73.5%.
Figure 2.
Age distribution of patients presenting to emergency services
Surprisingly, the number of registered medicolegal cases increased by 22.22% with a shoot-up in cases with physical assault from a known person [Table 2].
Table 2.
Cause-specific distribution of Emergency outpatient cases
| Presentation | 2019 (n=3,398) | 2020 (n=2,200) |
|---|---|---|
| Mechanical trauma | 67.46% | 39.29% |
| Lid, adnexa, ocular surface, and cornea related | ||
| Conjunctivitis | 6.6% | 14.07% |
| Chemical injury | 0.91% | 2.34% |
| Microbial keratitis | 7.72% | 9.67% |
| Acute hydrops | 0 | 0.29% |
| Peripheral ulcerative keratitis | 0 | 0.29% |
| MGD/stye/dry eye | 0.91% | 2.93% |
| Cellulitis | 0.91% | 2.34% |
| Posterior segment related | ||
| Retinal detachment | 1.65% | 8.5% |
| Endophthalmitis | 2.38% | 1.46% |
| Retinopathy of prematurity | 0.73% | 2.05% |
| Uveitis | 0.73% | 3.8% |
| Other retinal disorders | 4.44% | 9.38% |
| Glaucoma related | ||
| Primary congenital glaucoma | 0.18% | 0.29% |
| PACG/POAG | 1.1% | 1.75% |
| Lens-induced glaucoma | 0.18% | 0.29% |
| Others | ||
| Retinoblastoma and other ocular tumors | 0.91% | 1.49% |
| Cranial nerve abnormalities | 1.65% | 4.39% |
| Postoperative complication | 0.55% | 0.29% |
| Lens drop | 0.91% | 0 |
| Medicolegal cases | n=26 | n=39 |
| Assault (known person) | 40.12% | 72.04% |
| Assault (unknown person) | 25.26% | 15.15% |
| Road traffic accidents | 11.50% | 7.69% |
| Occupational | 23.07% | 5.12% |
MGD=Meibomian gland dysfunction, POAG=Primary open angle glaucoma, PACG=Primary angle closure glaucoma
Inpatient department
Routinely, the ophthalmic department of the center is a 310 bedded hospital with an occupancy rate of 80% and an average patient stay of 5 days. However, in the present time, the routine and emergency ward admissions decreased by 95.18% and 61.66% respectively (P < 0.001). The number of government-offered employment health scheme beneficiaries and medicolegal cases seeking admissions also decreased by 95.97% and 66.66%, respectively.
Surgical data
While elective surgeries were postponed for eight weeks at our center and dropped by 98.18%, emergency surgeries decreased by 58.81%. The percentage of emergency outpatient cases needing admissions and surgical intervention was 34.69% (1179/3398), and 27.86% (947/3398) last year vs 20.54% (452/2200) and 12.59% (277/2200) this year, respectively.
Eyebank related
The number of donor corneas collected decreased by 99.61% (P < 0.001). While the number of emergency therapeutic keratoplasties decreased by 92.39% (P < 0.001). Despite starting donor cornea retrieval services, only one pair of tissue was collected from a 3-year old child succumbing to the road-traffic accident. 14 therapeutic grafts performed during this crisis were undertaken majorly with glycerin-stored donor tissues.
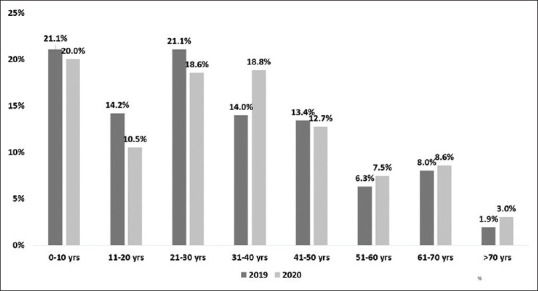
Cause specific distribution
Table 2 and Fig. 3a, b represent the cause-specific distribution of emergency outpatient, inpatient, and surgical cases respectively. Mechanical trauma, microbial keratitis, and conjunctivitis were the most common reasons for presentation in emergency OPD. However, the incidence of trauma decreased by 41.75% and that of microbial keratitis and conjunctivitis increased by 1.25 times and 2 times, respectively. While most of the retinal disorders and sanitizer-based chemical injuries (alcohol and hypochlorite) increased in proportion, the incidence of endophthalmitis, lens-drop, and postoperative complications lessened (due to decreased number of routine ophthalmic surgeries) during the COVID-19 pandemic. Traumatic globe-injury was the most common indication for emergency admissions (54.08% vs 62.35%) and surgeries. Admissions for microbial keratitis, primary adult glaucoma, and postoperative complications decreased while those for various other causes, particularly retinal disorders, increased.
Figure 3.
Diagnosis wise distribution of non-traumatic cases emergency admissions (a); Comparison of various indications for emergency surgeries at our center (b)
Discussion
The majority of previous studies have focused on the effects of the COVID-19 pandemic and lockdown on ophthalmic care provided by private institutions of the country.[4,8] We presently discuss its impact on eye-care provided by the apex institute of the nation, a government-funded multispecialty hospital providing good-quality affordable health-facilities to all economic classes besides serving COVID-19 patients. To the best of our knowledge, the present study the first of its kind in depicting results of the process of unlocking on ophthalmic care.[9]
We noted a dramatic fall in total hospital out-patient load (by 97%) particularly belonging to the elderly age-group (median age decreased from 55 years to 29 years) and systemically comorbid patients during the entire period, attributed majorly to complete lockdown and good public compliance who refrained their frail and elderly from undertaking unnecessary hospital visits. However, an unexpected delay in recovery of patient load despite initialization of the process of unlocking was attributed partly to the location of our institute, partial lockdown and restricted air and train travel in geographically surrounding hotspots, and guarded provision of e-pass to the general public for interstate travel, and partly to the suspected practice of patients preferring ophthalmic institutions not affiliated with COVID-19 care due to fear of acquiring a systemic infection during these critical times. While all this exercise may reduce fatalities in a vulnerable group, increased incidence of blindness throughout the country is expected in the future as a result of delayed ophthalmic care in the same group worsening the severity of their ocular condition.
Emergency eye-care services shrunk by two-thirds at our center and sudden flooding of younger males was witnessed due to the abrupt closure of routine outpatient services. Fortunately, >two-thirds of these cases were benign and only 12% needed emergency surgical intervention.
In total, cases of mechanical trauma decreased most probably due to indoor stay, supervised child play, and limited functioning of transport facilities and industries. However, this was contrary to recent studies by Hamroush et al. and Bapaye et al. who reported a spike in cases of mechanical ocular trauma during the lockdown period.[10,11] Occurrence of previously never witnessed mechanical injuries with plumbing instruments and electric-repairing devices in homemakers in our study signifies the impending danger associated with the dearth of adequate professional services during the current times. Additionally, ill-effects of increased indoor stay on the incidence of ocular surface disorders, myopia, and antecedent amblyopia due to exaggerated electronic media usage combined with reduced routine eye-care (refraction) during these times needs to be determined.[12] For instance, increased instances of violence among known people due to amplified home-stay is suggested by an unexpected 22.22% rise of medicolegal cases in our study. Although most of these were trivial and managed conservatively, there remains an urgent need to educate the general public about the importance of patience, peace, and harmony during these tough times. Whether an increased proportion of conjunctivitis in our study was a subtle manifestation of COVID-19 infection remains doubtful due to the lack of coexistent systemic complaints and low positivity rate of conjunctival swabs for SARS CoV-2. All conjunctivitis patients were managed conservatively and followed-up telephonically till resolution. When compared to last year where only one case of chemical injury with a sanitizer (surgical spirit) was reported in a health-care worker, this year, we encountered three cases of sanitizer-associated chemical injury (alcohol and hypochlorite) in the general public. Although none of these were grievous, it is imperative to educate the general public about the safe use of these substances to prevent serious ocular surface disorders. Some of the steps include the closure of eyes while pressing the nozzle, keeping the sanitizer below the eye level, applying it in a well-ventilated room, keeping them out-of-reach of children and administering sodium hyaluronate-based lubricants, and encouraging the use of soap and running water for hand-cleansing in individuals with the preexisting ocular surface disease.[13]
Donor eye collection suffered a major setback during this pandemic due to confusion regarding guidelines on tissue harvesting. However, unlike anticipated, even with initialization of unlocking and resumption of eye retrieval services, voluntary donations remained nil indicating that normalcy in this direction is still very far from achievement. The manner in which glycerin-stored corneas proved sight-saving during this crisis emphasizes on the importance of incorporating long-term donor storage methods in eye-banking to battle similar situations if they arise in the future. Also, ophthalmologists might consider adopting non-donor dependent and virus transmission free methods such as autologous scleral patch grafts, tenon's patch grafts, and conjunctival flaps and auto-keratoplasty, artificial corneas, and 3D-bioprinted corneas for dealing with urgent and elective keratoplasties in the future.[14]
Mirroring results of other recent studies, teleconsultations served as an effective method of triaging >93% patients as low-risk thereby limiting their unwanted hospital-based evaluation.[15] However, teleophthalmology has its own medical and medicolegal limitations in evaluating the underprivileged, the children, and subjects with posterior segment disorders. Yet, if utilized appropriately, this technology can serve as a useful aid in decreasing viral transmission while simultaneously catering to the general public.
The effect of the current situation on the psychological wellbeing of health care workers is profound and inexpressible.[16] Ongoing research and academic activities and blindness eradication programs have been disrupted thereby halting newer drug trials and unlike expected, the process of unlocking has served only minimally in reestablishing them. Minimal patient exposure has jeopardized resident learning and steps such as rotational clinical postings, online classes, simulator-based surgical practice, and extension of tenure have been undertaken to facilitate their learning.[17] Financial repercussions of national economic backlash may be expected as suboptimal government expenditure on newer blindness-eradication policies. This superadded by hampered monetary collections in our government-funded institute secondary to declined patient inflow may further worsen delivery of long-term high-quality ophthalmic care to all economic sections of the society, more so to the poor and the deprived.
We have learned tremendously from the present situation and the entire hospital administration and functioning are being re-structured towards capacity-building to cater to the accumulating patient backlog without compromising safety. Guidelines recommended by national societies are being actively incorporated to assure equal and equitable delivery of good-quality eye-care to patients from all financial backgrounds.[3,18,19,20,21,22,23,24,25]
Conclusion
To conclude, the impact of COVID-19 on ophthalmic care served by government-funded institutes is profound and should not be overlooked to protect the underprivileged from succumbing to the present situation. Unlike anticipated, lifting of pandemic-associated lockdown may serve only minimally in improving access to ophthalmic services in its initial phases and normalization may take more time than expected. Effective and efficient policies must be planned by both governmental and nongovernmental organizations to deal with the bombardment of ocular problems in the coming time and appropriate utilization of newer technology, particularly telemedicine, can aid in providing optimal-quality affordable eye-care to all sections of society.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank our Institute for allowing us to continue with our research work.
References
- 1.World Health Organization. Coronavirus Disease (COVID-2019) Situation Reports. World Health Organization; 2020. [Last accessed on 2020 Jul 19]. Available from: https://wwwwhoint/emergencies/diseases/novel-coronavirus-2019/situationreports 20 . [Google Scholar]
- 2.Gettleman J, Schultz K. (24 March 2020) “Modi Orders 3-Week Total Lockdown for All 13 Billion Indians”. The New York Times ISSN 0362-4331 [Google Scholar]
- 3.Vashist P, Senjam SS, Gupta V, Manna S, Agrawal S, Gupta N, et al. Community eye-health and vision center guidelines during COVID-19 pandemic in India. Indian J Ophthalmol. 2020;68:1306–11. doi: 10.4103/ijo.IJO_1527_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society – Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal R, Angmo D, Saxena R, Sharma N. Comment on “Possible prophylactic or preventive role of topical povidone iodine during accidental ocular exposure to 2019-nCoV” Graefes. Arch Clin Exp Ophthalmol. 2020:1–2. doi: 10.1007/s00417-020-04752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma N, D'Souza S, Nathawat R, Sinha R, Gokhale NS, Fogla R, et al. All India Ophthalmological Society - Eye Bank Association of India consensus statement on guidelines for cornea and eyebanking during COVID-19 era. Indian J Ophthalmol. 2020;68:1258–62. doi: 10.4103/ijo.IJO_1554_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madanagopalan VG, Sriram Gopal MR, Sengupta S. Perspectives of physicians in general and ophthalmologists in particular about restarting services post-COVID-19 lockdown. Indian J Ophthalmol. 2020;68:1401–6. doi: 10.4103/ijo.IJO_1221_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal R, Sharma N. Commentary: COVID-19 pandemic and national lockdown: The cascading effect. Indian J Ophthalmol. 2020;68:1545. doi: 10.4103/ijo.IJO_2100_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamroush A, Qureshi M, Shah S. Increased risk of ocular injury seen during lockdown due to COVID-19. Cont Lens Anterior Eye. 2020;43:216. doi: 10.1016/j.clae.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bapaye MM, Nair AG, Mangulkar PP, Bapaye CM, Bapaye MM. Resurgence of “bow and arrow” related ocular trauma: Collateral damage arising from COVID-19 lockdown in India? Indian J Ophthalmol. 2020;68:1222–3. doi: 10.4103/ijo.IJO_901_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sumitha M, Sanjay S, Kemmanu V, Bhanumathi MR, Shetty R. Will COVID-19 pandemic-associated lockdown increase myopia in Indian children? Indian J Ophthalmol. 2020;68:1496. doi: 10.4103/ijo.IJO_1443_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shetty R, Jayadev C, Chabra A, Maheshwari S, D'Souza S, Khamar P, et al. Sanitizer aerosol-driven ocular surface disease (SADOSD)–A COVID-19 repercussion? Indian J Ophthalmol. 2020;68:981–3. doi: 10.4103/ijo.IJO_1308_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal R, Sharma N. Commentary: A review of long-term corneal preservation techniques: Relevance and renewed interests in the COVID-19 era. Indian J Ophthalmol. 2020;68:1365–6. doi: 10.4103/ijo.IJO_1877_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murthy SI, Das S, Deshpande P, Kaushik S, Dave TV, Agashe P, et al. Differential diagnosis of acute ocular pain: Teleophthalmology during COVID-19 pandemic - A perspective. Indian J Ophthalmol. 2020;68:1371–9. doi: 10.4103/ijo.IJO_1267_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khanna RC, Honavar SG, Metla AL, Bhattacharya A, Maulik PK. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J Ophthalmol. 2020;68:994–8. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mishra D, Nair AG, Gandhi RA, Gogate PJ, Mathur S, Bhushan P, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India – Outcomes of a survey. Indian J Ophthalmol. 2020;68:999–1004. doi: 10.4103/ijo.IJO_1067_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tejwani S, Angmo D, Nayak BK, Sharma N, Sachdev MS, Dada T, et al. Preferred practice guidelines for glaucoma management during COVID-19 pandemic. Indian J Ophthalmol. 2020;68:1277–80. doi: 10.4103/ijo.IJO_1724_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manjandavida FP, Honavar SG, Kim U, Singh U, Menon V, Das S, et al. Ocular oncology practice guidelines during COVID-19 pandemic- An expert consensus. Indian J Ophthalmol. 2020;68:1281–91. doi: 10.4103/ijo.IJO_1669_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ali MJ, Hegde R, Nair AG, Bajaj MS, Betharia SM, Bhattacharjee K, et al. All India Ophthalmological Society – Oculoplastics Association of India consensus statement on preferred practices in oculoplasty and lacrimal surgery during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:974–80. doi: 10.4103/ijo.IJO_1415_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saxena R, Singh D, Jethani J, Sharma P, Sinha R, Sharma N, et al. Pediatric ophthalmology, strabismus and neuro-ophthalmology practice in the COVID-19 era: All India Ophthalmological Society guidelines. Indian J Ophthalmol. 2020;68:1300–5. doi: 10.4103/ijo.IJO_1789_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma N, Khamar P, Sachdev MS, Maheshwari S, Gupta K, Sinha R, et al. All India Ophthalmological Society - Preferred practice in refractive surgery during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:1263–8. doi: 10.4103/ijo.IJO_1754_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta V, Rajendran A, Narayanan R, Chawla S, Kumar A, Palanivelu MS, et al. Evolving consensus on managing vitreo-retina and uvea practice in post-COVID-19 pandemic era. Indian J Ophthalmol. 2020;68:962–73. doi: 10.4103/ijo.IJO_1404_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reddy JC, Vaddavalli PK, Sharma N, Sachdev MS, Rajashekar YL, Sinha R, et al. A new normal with cataract surgery during COVID-19 pandemic. Indian J Ophthalmol. 2020;68:1269–76. doi: 10.4103/ijo.IJO_1528_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jayadev C, Mahendradas P, Vinekar A, Kemmanu V, Gupta R, Pradhan ZS, et al. Tele-consultations in the wake of COVID-19 – Suggested guidelines for clinical ophthalmology. Indian J Ophthalmol. 2020;68:1316–27. doi: 10.4103/ijo.IJO_1509_20. [DOI] [PMC free article] [PubMed] [Google Scholar]