Abstract
Therapeutic contact lens used in the treatment of non-infective corneal pathologies are prone to infection by microorganisms like bacteria, protozoa and fungi. Bacteria cause the majority of contact lens-related infections. Although rare, fungal invasion of soft contact lenses is a potentially severe complication which may cause keratitis and more fulminating infections. Contact lens invasion can present as acute red eye warranting its replacement to prevent the development of keratitis. Different genera and species of fungi are documented to cause contact lens invasion. We report a rare case of fungal invasion of the contact lens by Aspergillus nidulans.
Keywords: Acute red eye, contact lens, fungal invasion
Therapeutic contact lens used in the treatment of non-infective corneal pathologies is indicated for pain relief, promotion of corneal epithelial healing, mechanical support and protection. Contact lens contamination often occurs as a result of not following the recommended standard care procedures. In asymptomatic wearers, fungal spp. are isolated in only 0% to 15% of the time.[1] We report one such case of fungal invasion of the contact lens by A. nidulans and emphasize about microbiological evaluation and contact lens care.
Case Report
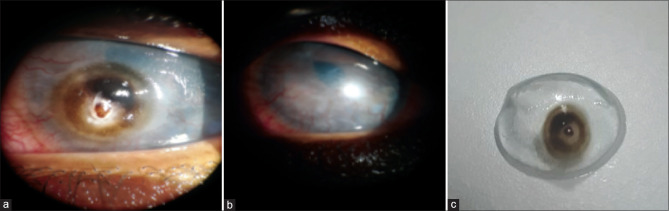
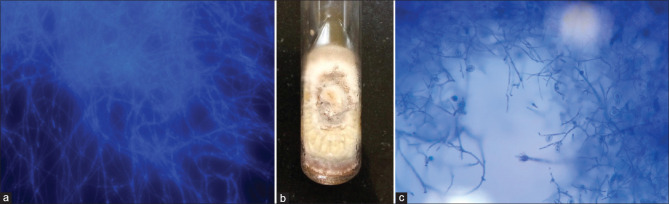
A 20-year-old farmer presented to us with complaints of redness, pain and watering in his left eye since one month. He gave a history of trauma to the same eye with copper wire two years back, which was managed medically, and a bandage contact lens was placed. He was irregular in his clinical follow-up and was still using loteprednol etabonate 0.5% eye drops. On examination of the affected eye, he denied perception of light and lid oedema with conjunctival congestion was present. A circular 3 × 3 mm, brown pigmented deposit was seen on the bandage contact lens at seven 0'clock position close to limbus which mimicked an impending corneal ulcer [Fig. 1a]. On removing contact lens, a diffusely hazy cornea with 3600 superficial vascularization was seen [Fig. 1b]. There was no epithelial defect or infiltration in the cornea. Examination of the contact lens after removal showed intact smooth posterior surface and the deposit was resistant to scrapping [Fig. 1c]. The lens was subjected to microbiology evaluation. Bacterial culture was sterile. A mass of tangled hyphae which were narrow were found on microscopy [Fig. 2a]. A buff-coloured mould grew after four days incubation [Fig. 2b]. On Czapek dox agar, it produced a similar colony with radiate folds and tan coloured reverse. A lactophenol cotton blue preparation (LPCB) from the colony showed thin septate hyphae, conidiophores, and conidia. The conidiophores were short, smooth, terminated in a dome-like vesicle with biseriate phialides. A large number of spherical and subspherical hulle cells were observed, and the fungus was identified as Aspergillus nidulans [Fig. 2c]. Meanwhile, the patient was empirically treated with topical natamycin 5% eye drops every one hourly and antibiotic moxifloxacin 0.5% eye drops four times a day for which he showed good response with resolution of redness and pain.
Figure 1.
Slit lamp examination of left eye showing (a) circular 3 × 3 mm growth with variable pigmentation (b) vascularized hazy cornea seen after removal of contact lens and (c) pigmented growth with mucus debris on the surface of the contact lens
Figure 2.
Showing (a) Calcoflour white KOH preparation showing narrow septate hyphae (b) cream-buff coloured colony with radiate folds (c) LPCB mount showing condiophores with vesicles bearing biseriate phialides. Several hulle cells are also seen
Discussion
Hydrophilic therapeutic soft contact lenses have been used to treat corneal pathologies since the early 1970s. In 1973, Bernstein first reported fungal infiltration of hydrophilic contact lens in a contact lens wearer.[2] In 2005–2006, an epidemic of contact lens associated keratitis caused by Fusarium sp. occurred with the use of a specific type of contact lens solution.[3]
A wide variety of fungi are associated with contamination of contact lenses of which Candida, Fusarium, and Aspergillus are the most commonly isolated organisms.[4] Several factors like extended wearing period, lens type, use of broad-spectrum antibiotics, steroids, warm, moist environments, and preexisting corneal disease contribute to fungal contamination of contact lenses. The ocular flora of the conjunctival sac and lid margins, improper lens handling, infrequent cleaning, cosmetics and environmental factors are the primary sources of contamination. The defects in the structural integrity of the lens surface from the manufacturing process, cosmetic brushes or repetitive handling facilitate fungal entry into the lens matrix.
MS Marque 's-Calvo[5] in an in vitro study using A. niger hypothesized that structures within the fungal cell wall and hydrolytic enzymes aids in the colonization of lens. The fungus then utilizes the glucose and peptone in the media to grow further. Similarly, Candida sp. also produces hyphae and releases hydrolytic enzymes to degrade polymers. A comparison of these two species has revealed that, strain and medium in which the lenses and microorganisms were cultured influenced colonization. The percentage of cell adhesion, invasion, the density and size of the inner colonies were always noticeably lower in C. albicans.[6]
Ahearn et al. found that Fusarium spp. adhere to and penetrate the surface of contact lenses by the formation of penetration pegs, which are fungal hyphae that traverse into the lens's matrix. The degree of attachment and numbers of penetration pegs may be affected by damage to the lens surface.[7]
Our patient used the contact lens for an extended period of two years along with topical steroids and was not on regular follow-up. These risk factors might have led to the fungal invasion of the contact lens. Though clinically it mimicked an impending perforation the fungus had invaded only locally without further spread to the cornea which is similar to the past reported cases.[8,9] Also, these pigmented deposits made us suspect A. niger, as reported in the past.[10] However, A. nidulans grew on culture, and the blackish discolouration could be due to chemical deposits on the infected contact lens.
A. nidulans has been isolated from soil, compost, fruits, and organic debris.[11] It is known to cause pulmonary, cerebral, ophthalmic, sinus, bone, and skin infections in immunocompromised patients. Cases of keratitis and endophthalmitis due to A. nidulans have been described in past. To the best of our knowledge, this is the first case in the literature of A. nidulans causing contact lens invasion
Conclusion
We emphasize the need for educating the patients about contact lens care like regular disinfection or replacement, regular follow up, use of protective gear like goggles during outdoor activities and judicious use of topical medications to prevent such infections. Microbiological evaluation is a must to identify the species and to understand the trend of organisms involved in the disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Szczotka-Flynn LB, Pearlman E, Ghannoum M. Microbial contamination of contact lenses, lens care solutions, and their accessories: A literature review. Eye Contact Lens. 2010;36:116–29. doi: 10.1097/ICL.0b013e3181d20cae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernstein HN. Fungal growth into a bionite hydrophilic contact lenses. Ann Ophthalmol. 1973;5:317–22. [PubMed] [Google Scholar]
- 3.Norina TJ, Raihan S, Bakiah S, Ezanee M, Liza-Sharmini AT, Wan Hazzabah WH. Microbial keratitis: Aetiological diagnosis and clinical features in patients admitted to Hospital Universiti Sains Malaysia. Singapore Med J. 2008;49:67–71. [PubMed] [Google Scholar]
- 4.B, Gray T, Cursons R, Sherwan J, Rose P. Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases. Br J Ophthalmol. 1995;79:601–5. doi: 10.1136/bjo.79.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marqués-Calvo MS. In vitro colonization of hydrophilic contact lenses by Aspergillus niger. J Ind Microbiol Biotechnol. 2002;29:6–9. doi: 10.1038/sj.jim.7000255. [DOI] [PubMed] [Google Scholar]
- 6.Marqués-Calvo MS. Colonization of hydrophilic contact lenses by yeast. J Ind Microbiol Biotechnol. 2004;31:255–60. doi: 10.1007/s10295-004-0141-x. [DOI] [PubMed] [Google Scholar]
- 7.Ahearn DG, Zhang S, Ward MA, Simmons RB, Stulting RD. Hyphal penetration of worn hydrogel contact lenses by fusarium. Cornea. 2009;28:914–7. doi: 10.1097/ICO.0b013e31819c189d. [DOI] [PubMed] [Google Scholar]
- 8.Hurtado I, Magran BL. Invasion of a soft contact lens by Exophiala jeanselmei. Mycopathologia. 1989;105:171–3. doi: 10.1007/BF00437251. [DOI] [PubMed] [Google Scholar]
- 9.Radhakrishnan N, Panigrahi AK, Balasubramanium A, Das M, Prajna NV. Colonization of therapeutic contact lens by dematiaceous fungi. Contact Lens Anterior Eye. 2019;42:470–2. doi: 10.1016/j.clae.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Sharma S, Gopalkrishnan S, Aasuri MK, Garg P, Rao GN. Trends in contact lens-associated microbial keratitis in Southern India. Ophthalmology. 2003;110:138–43. doi: 10.1016/s0161-6420(02)01283-6. [DOI] [PubMed] [Google Scholar]
- 11.Sugui JA, Kwon-Chung KJ, Juvvadi PR, Latgé J-P, Steinbach WJ. Aspergillus fumigatus and related species. Cold Spring Harb Perspect Med. 2014;5:a019786. doi: 10.1101/cshperspect.a019786. [DOI] [PMC free article] [PubMed] [Google Scholar]