Abstract
Retinal vasospasm was visualized in a young female; a known case of systemic lupus erythematosus (SLE) retinopathy with unaffected vision. The fundus fluorescein angiogram showed a cyclical filling and emptying of the retinal vessels which was suggestive of vasospasm and a retinal Raynaud's-like phenomenon with no obvious perfusion deficit. There was retinal thinning involving the superficial layers that was seen on optical coherence tomography (OCT), capillary fill voids on OCT angiography, and retinal surface undulations seen on multicolor imaging. All imaging was performed on Spectralis (Heidelberg, Germany).
Keywords: FFA, lupus, optical coherence tomography, optical coherence tomography angiography, raynauds, retina, vasospasm
Systemic lupus erythematosus (SLE) is a well-recognized multi-system collagen vascular disorder with protean manifestations and possible involvement of the eye and the nervous system.[1] The ocular findings reported include uveitis, cotton wool spots, microaneurysms, and arteriolar narrowing.[1,2,3] Occlusive retinal arterial disease has been reported which is characterized by multifocal arterial occlusion and non-perfusion areas of the obstructed arteries and capillary beds fed by them.[4,5]
A study in 1982 detailed three patterns of fluorescein angiography (FFA) associated with SLE retinopathy, involving disc vasculitis, cotton wool spots, and normal fundal appearance associated with vascular leakage.[6] Another group have demonstrated narrower arteriolar and venular diameters on fluorescein angiography in these patients.[7] OCT Angiography has revealed enlarged foveal avascular zones and decreased vessel density.[8]
There exist no reports however of a cyclical filling and emptying of the retinal vessels suggestive of a retinal Raynaud's like phenomenon. We hereby present multimodal imaging findings in a case of a 20-year-old female in whom we observed the above during FFA.
Case Report
A 20-year-old female with a 2-year history of systemic lupus erythematosus (SLE) presented with complaints of painless progressive decrease in vision in her right eye of 5 months duration. She had been diagnosed with SLE 5 years back, and had additionally developed lupus nephritis and pulmonary artery thrombosis, for which she was on treatment in the form of systemic corticosteroids, immunosuppressive medication mycophenolate mofetil at a dosage of 2 g a day (divided), tablet hydroxychloroquine 400 mg a day and an anticoagulant. Her systemic condition was well controlled, according to her rheumatologist. A year earlier, she had undergone treatment for SLE retinopathy with intravitreal ranibizumab and pan-retinal photocoagulation in both eyes, elsewhere. She had undergone a carotid doppler test at that stage, which had been reported to be within normal limits.
Her best corrected visual acuity was 20/20 with a normal intro-ocular pressures and an anterior segment exam. Fundus evaluation revealed a rhegmatogenous retinal detachment in the right eye. Left eye revealed a healthy disc with no disc pulsations, a healthy macula on direct examination with a 78 D lens, and clinically normal retinal vessels with no active neovascularization noted at the disc or elsewhere. Trace old vitreous hemorrhage inferiorly with peripheral laser scars and regressed neovascularization was noted in the temporal periphery. An FFA [Fig. 1 and Video 1], multicolor imaging, optical coherence tomography (SD-OCT), and SD-OCT angiography (OCTA) (Spectralis, Heidelberg, Germany) was performed. Two interesting features were noted.
Figure 1.
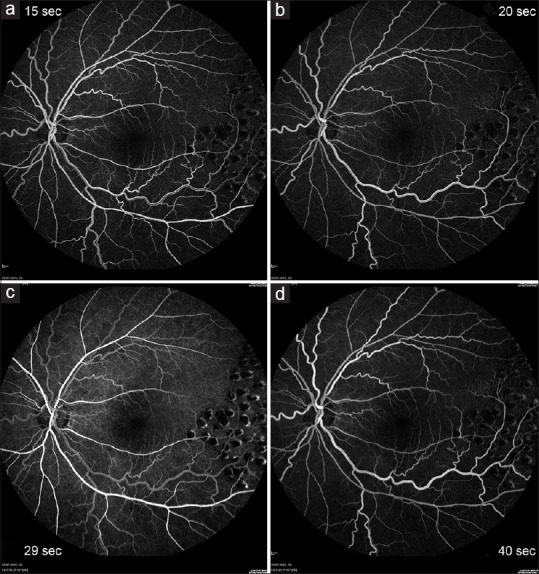
FFA images (a) at 15 s and (c) at 29 s show the arteriole hyperfluorescent in comparison to the venule which shows laminar filling; (b) at 20 s and (d) at 40 s show the venule hyperfluorescent compared to the arteriole
Firstly, the FFA was unremarkable till the peak phase. At 27 s an increase in arteriolar fluorescence in all the four major arterioles, with a simultaneous decrease in venular fluorescence without a change in vessel caliber was seen. Fluorescence increased in the venules at 29 s, with a reduction in arterioles. This cycle repeated at 43 s. Peripheral areas of nonperfusion with areas of leakage were seen suggestive of neovascularization.
Secondly, the multicolor image of the left eye [Fig. 2] showed an undulating retinal surface infero-temporal to the disc, apparent in the blue and green channel, absent in the infrared. Corresponding changes were seen on the SD-OCT [Fig. 2] as an area of inner retinal thinning, on the enface OCT image as dark patches, on the OCTA [Fig. 2] as a flow void in the superficial and deep capillary plexus and on the FFA as a subtle ill-defined hypofluorescence in the early phase, persisting into the mid and late phase of the angiogram.
Figure 2.
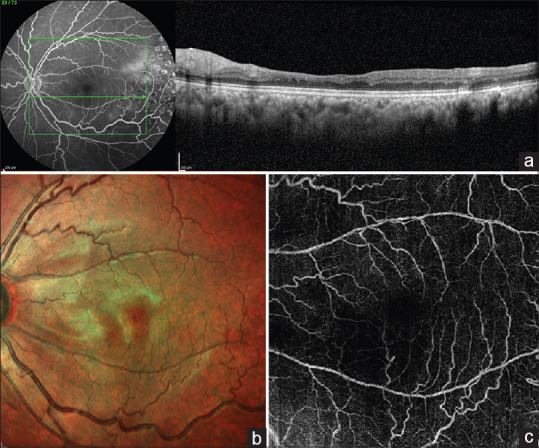
(a) – SD-OCT image of the left eye through the area of retinal thinning predominantly involving the inner layers; (b) – multicolor image showing the retinal undulations corresponding to the area of retinal thinning and (c) – Composite OCTA image of the superficial and deep capillary plexus showing capillary dropout in the corresponding area
No conjunctival blanching was noted when the patient was examined earlier or after the fluorescein angiography. The patient was re-evaluated by the rheumatologist who advised no additional treatment. The right eye retinal detachment was managed surgically and the left eye was treated with additional laser photocoagulation.
Discussion
The reappearance of laminar flow in the dynamic FFA after the first pass is intriguing and we checked that the dye was administered as a single bolus. The emptying of the venule with simultaneous brightening of the arteriole can be suggestive of spasm at the precapillary arteriole level. Very few angiographic documentations of vasospasm exist in the literature.[9]
SLE in particular may be associated with Raynaud's phenomenon, which is a peripheral arteriolar and capillary vasospasm.[10] The appearance noted on the dynamic angiogram in our case is very suggestive of a spasm at the same level, indicating a Raynaud's like vasospasm in the eye. There exists an interesting report[11] of an intense vasospasm with CRAO like functional loss in a patient with SLE, 7 attacks per week each lasting 5 min. However, this is different from our case where the vision was unaltered, and the patient was asymptomatic.
The retinal surface undulation seen on multicolor imaging corresponded with inner retinal thinning on SD-OCT, flow voids, and reduced capillary density on OCTA in the superficial and deep vascular plexus. These findings have been reported as a sequelae to lupus retinopathy which is caused due to microvascular thrombosis and immune complex mediated vascular injury.[8] Hypothetically in the presence of a flow void on OCTA the dye in FFA should not perfuse the macula producing a clear area of capillary non-perfusion. However, we saw an ill-defined subtle hypofluorescence in the early and mid-phase persisting in the late phase. The presence of corresponding retinal thinning on OCT probably indicates that this could be an effect of chronic decreased blood flow. The above OCTA and OCT observations may indicate chronic and highly localized vasospasm episodes.
A significant association of retinopathy with central nervous system lupus has been reported.[2] Ocular involvement in SLE can be a manifestation of widespread systemic disease[4] and may help in prognosticating Lupus activity and to monitor efficacy of systemic medications.[3]
The significance of these localized vasospasm or Reynaud's like phenomenon on angiography and findings on multimodal imaging especially OCTA may be that it is indicative of the extent of systemic disease and disease control in SLE vasculitis. The association of pulmonary vasculature pathology further adds weight to this suggestion.
Conclusion
To our knowledge this is the first report in literature describing the “Retinal Raynaud's like Phenomenon” seen on dynamic FFA along with a correlating OCTA finding of an ischemic event involving the deep capillary plexus in a systemic vasculitic entity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.ijo.in
References
- 1.Gold DH, Morris DA, Henkind P. Ocular findings in systemic lupus erythematosus. Br J Ophthalmol. 1972;56:800–4. doi: 10.1136/bjo.56.11.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ushiyama O, Ushiyama K, Koarada S, Tada Y, Suzuki N, Ohta A, et al. Retinal disease in patients with systemic lupus erythematosus. Ann Rheum Dis. 2000;59:705–8. doi: 10.1136/ard.59.9.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kouprianoff S, Chiquet C, Bouillet L, Romanet JP. OCT follow-up of systemic lupus erythematosus choroidopathy. Ocul Immunol Inflamm. 2010;18:113–5. doi: 10.3109/09273940903353785. [DOI] [PubMed] [Google Scholar]
- 4.Gold D, Feiner L, Henkind P. Retinal arterial occlusive disease in systemic lupus erythematosus. Arch Ophthalmol. 1977;95:1580–5. doi: 10.1001/archopht.1977.04450090102008. [DOI] [PubMed] [Google Scholar]
- 5.Snyers B, Lambert M, Hardy J-P. Retinal and choroidal vaso-occlusive disease in systemic lupus erythematosus associated with antiphospholipid antibodies. Retina (Philadelphia, Pa) 1990;10:255–60. doi: 10.1097/00006982-199010000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Lanham JG, Barrie T, Kohner EM, Hughes GR. SLE retinopathy: evaluation by fluorescein angiography. Ann Rheum Dis. 1982;41:473–8. doi: 10.1136/ard.41.5.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JH, Kim SS, Kim GT. Microvascular findings in patients with systemic lupus erythematosus assessed by fundus photography with fluorescein angiography. Clin Exp Rheumatol. 2013;31:871–6. [PubMed] [Google Scholar]
- 8.Shah C, Gabriel R, Kedhar S, Kuppermann B, Mehta M. Subclinical foveal vasculopathy in patients with systemic lupus erythematosus using optical coherence tomography angiography? J Vitreo Retinal Dis. 2019;3:283–8. doi: 10.1177/2474126419850758. [Google Scholar]
- 9.Weinberg DV, Covert DJ. Amaurosis fugax captured during fluorescein angiography. Retina. 2015;35:2669–71. doi: 10.1097/IAE.0000000000000607. [DOI] [PubMed] [Google Scholar]
- 10.Heimovski FE, Simioni JA, Skare TL. Systemic lupus erythematosus and Raynaud's phenomenon. An Bras Dermatol. 2015;90:837–40. doi: 10.1590/abd1806-4841.20153881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winterkorn JM, Kupersmith MJ, Wirtschafter JD, Forman S. Brief report: Treatment of vasospastic amaurosis fugax with calcium-channel blockers. N Engl J Med. 1993;329:396–8. doi: 10.1056/NEJM199308053290604. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


