Abstract
Diabetic foot ulcers (DFUs) are a common complication of diabetes that impacts on the health-related quality of life (HRQOL). Foot care is an important factor in the self-care management of patients with DFUs. The objective of this study was to investigate the HRQOL and foot care management of people with DFUs. A cross-sectional study involving 41 people with DFUs was conducted at a large tertiary hospital in Northern Thailand. The Diabetic Foot Ulcer Scale-Short Form and the VA-Diabetes Foot Care Survey were used to assess the HRQOL and foot care management among people with DFUs. The majority of the participants were female (n = 24, 58.5%), and the mean age was 62.13 years. The scores for HRQOL in the six domains were as follows: leisure (66.95 ± 28.03), physical health (68.93 ± 28.51), dependence or daily life (80.08 ± 25.23), negative emotions (71.23 ± 29.48), worried about ulcers (62.20 ± 31.97), and bothered by ulcer care (69.36 ± 25.20). High scores indicate a high (good) HRQOL. Less than a third of the participants reported that they had received education about foot care management. Almost all participants reported that they washed their feet daily; however, a large proportion did not test the water temperature or use lubricants on their feet. Most of the participants did not have a mirror for checking under their feet (48.8%), and there was a lack of knowledge about how to use a mirror for foot inspections (51.2%). This study provides guidance for clinicians on the content and delivery of diabetes education programs for people with diabetes (and DFUs) in Northern Thailand. The findings provide guidance on existing knowledge and the need for programs to address barriers to foot self-care management both in terms of skills and attitudes.
Keywords: health-related quality of life, self-care management, diabetic foot ulcer, nurse, Northern Thailand
Introduction
Diabetic foot ulcers (DFUs) are a common complication estimated to affect up to 25% of people with diabetes mellitus globally (Boulton, 2010). DFUs are associated with increased mortality (Walsh, Hoffstad, Sullivan, & Margolis, 2016) with a 5-year mortality rate in people with newly diagnosed DFUs estimated to be 40% (Walsh et al., 2016). Evidence obtained from cross-sectional studies (Goodridge et al., 2006; Nabuurs-Franssen, Huijberts, Nieuwenhuijzen Kruseman, Willems, & Schaper, 2005; Ribu, Hanestad, Moum, Birkeland, & Rustoen, 2007b) and systematic reviews (Khunkaew, Fernandez, & Sim, 2017) have reported decreased HRQOL among people with DFUs. Studies using the SF-36 have reported poor HRQOL in people with DFUs (Meijer et al., 2001; Nabuurs-Franssen et al., 2005; Ribu, Birkeland, Hanestad, Moum, & Rustoen, 2008) when compared with people without DFUs.
Review of Literature
People with DFUs have a poorer HRQOL in the physical, financial, and psychological domains (Boutoille, Feraille, Maulaz, & Krempf, 2008; Garcia-Morales et al., 2011; Ikem, Ikem, & Ola, 2009; Jaksa & Mahoney, 2010; Ribu, Hanestad, Moum, Birkeland, & Rustoen, 2007a; Sanjari et al., 2011; Valensi, Girod, Baron, Moreau-Defarges, & Guillon, 2005; Yekta, Pourali, & Ghasemi-Rad, 2011). People with DFUs who experience poor healing have poorer HRQOL in the mental health, social, and physical domains (Löndahl, 2012). In addition, a large multicenter study that included 10 different countries demonstrated that low HRQOL in patients with DFUs was a predictor of amputation and mortality (Siersma et al., 2014).
Poor HRQOL can be attributed to various factors including pain, fatigue, wound infections, frequent dressing changes, restricted mobility, and social isolation. People with DFUs experience severe pain related to diabetic peripheral neuropathy. A large multicenter study conducted in Norway reported that 75% of people with DFUs experienced pain while walking or standing and also during the night (Ribu et al., 2006). However, there is controversy in the literature about the impact of pain on HRQOL with some studies indicating that pain is not a determinant of HRQOL (Ribu et al., 2007a; Ribu et al., 2006).
Lack of sleep due to pain, altered life circumstances, or anxiety leading to fatigue have all been reported to contribute to poor HRQOL (Castro-Sánchez et al., 2011). These factors may be exacerbated by attending clinic visits, hospitalization, and dressing changes (Khalid, 2014). Presence of wound infection has been reported as a predictor of poor HRQOL in patients with DFUs (Ribu et al., 2007a). Restricted mobility due to difficulties in functioning, problems with footwear, and amputations are reported to cause depression and anxiety and social isolation among people with DFUs (Abetz, Sutton, Brady, McNulty, & Gagnon, 2002; Ashford, McGee, & Kinmond, 2000; Carrington et al., 2001; Meijer et al., 2001). Poor psychosocial adjustment and low self-perceptions have also been reported (Bann, Fehnel, & Gagnon, 2003).
Foot self-care management is a key to reducing mortality for people with DFUs (Aljasem, Peyrot, Wissow, & Rubin, 2001). Self-care knowledge can assist people with diabetes to assess their feet, seek help when needed, and collaborate with health-care providers to reduce the risk of foot ulcers (Glasgow et al., 2001). Foot self-care practices among people with DFUs have been found to be poor (Chellan et al., 2012). In a cross-sectional survey of 352 patients in Nigeria, only a third had good knowledge of foot care, and of these, more than 60% were not aware of the importance of checking the inside of their footwear or what action to take if they found redness or bleeding between their toes (Desalu et al., 2011).
The prevalence of DFUs among Thai people is rapidly increasing. In a large comprehensive foot examination survey undertaken in Thailand of people with diabetes, 15% to 26% had foot problems (Reutrakul & Deerochanawong, 2016). In a study of amputees conducted in Thailand, 32% of amputations were related to type 2 diabetes mellitus (Settakorn et al., 2005). In addition, 2.2% of people with DFUs have been reported to have had a history of amputation, and 10.6% were identified as high risk to develop further foot ulcers (Sarinnapakorn, Sunthorntepwarakul, Deerochanawong, Niramitmahapanya, & Napartivaumnuay, 2016). Despite the increasing prevalence of DFUs in Thailand, there is a dearth of research relating to HRQOL and foot care practices among Thai people with DFUs. A better understanding of the impact of a DFU on the person’s HRQOL will enable clinicians to provide better care for these patients. In addition, identifying gaps in knowledge relating to foot self-care management will enable clinicians to provide patient education to reduce DFUs and the impact they have on HRQOL.
This study is part of a larger research project assessing the HRQOL, diabetes knowledge, and self-care management among Thai people with diabetes mellitus. The objective of this study was to investigate the HRQOL and the self-care management behaviors among people with DFUs using a DFU-specific instrument in a tertiary-level hospital in Northern Thailand.
Methods
Design
A cross-sectional study was undertaken of people with DFUs attending a diabetic foot clinic.
Research Question
What is the HRQOL and the self-care management behaviors among people with DFUs in a tertiary-level hospital in Northern Thailand?
Sample
Consecutive sampling was used to recruit people attending the outpatient diabetes and foot clinic in Northern Thailand. Data were collected between September 13 and November 13 in 2016.
Inclusion or Exclusion Criteria
Participants were recruited if they were over 18 years, had one or more DFUs, attended the diabetic outpatient clinic, were willing to participate, and able to read or understand the Thai language. People who had cognitive impairment or communication difficulties could not understand the Thai language were excluded. All potential participants were given a participant information sheet, and informed consent was obtained prior to recruitment. Participation was voluntary.
Data Collection
Information about the research was provided to eligible participants using a standardized script. Participants were invited to complete the survey by self-administration or interview. Participants who were unable to read or write had a 1:1 interview with the researcher to complete the survey. Self-administration took approximately 15 minutes, and interviews took approximately 25 minutes to complete.
Data Collection Instruments
Data were collected relating to demographic and clinical characteristics, HRQOL, and self-management behaviors relating to foot care. The demographic and clinical characteristics are included in Table 1.
Table 1.
Demographic and Clinical Characteristics.
| Variables | Percentage of people with DFUs (n = 41) |
|---|---|
| Gender | |
| Female | 58.5 |
| Male | 41.5 |
| Smoker | 7.3 |
| Age (mean ± SD) | 62.1 ± 9.5 |
| Marital status | |
| Living with partner | 68.2 |
| Not living with partner | 31.7 |
| Highest qualification | |
| Elementary school (primary school) | 73.2 |
| Secondary school (high school) | 17.1 |
| Diploma and over | 7.3 |
| Employment status | |
| Unemployed | 14.7 |
| Employed | 85.3 |
| Earnings per month | |
| 0–10,000 Baht/month | 82.9 |
| More than 10,001 Baht/month | 17 |
| Occupation | |
| Farmer | 19.5 |
| Government worker | 0 |
| Housewives or husbands | 31.7 |
| Private employee | 4.9 |
| Business | 12.2 |
| Diabetes therapy | |
| Insulin | 12.2 |
| Oral medication | 48.8 |
| Combination of insulin and oral medication | 34.1 |
| Nonpharmacologic treatment | 4.9 |
| Clinical characteristics, mean (SD) | |
| Diabetes duration (years) | 12.0 ± 8.5 |
| HbA1c (in mg%) | 8.1 ± 2.1 |
| BMI | 27.9 ± 7.9 |
| Wagner’s grade | |
| Grade 1 | 82.9 |
| Grade 2 | 17.1 |
Note. DFU = diabetic foot ulcer; HbA1c = glycosylated hemoglobin A1c; BMI = body mass index; SD = standard deviation.
Health-Related Quality of Life
Health-related quality of life (HRQOL) was measured using the disease-specific Diabetic Foot Ulcer Scale-Short Form (DFS-SF; Bann et al., 2003). The DFS-SF was validated previously against the DFS and was reduced from 64 items to 29 items (Abetz et al., 2002). The 29-item DFS-SF comprises six subscales: leisure (5 items), physical health (5 items), dependence or daily life (5 items), negative emotions (6 items), worries about ulcers or feet (4 items), and bothered by ulcer care (4 items; Bann et al., 2003). Responses to each item are rated on a 5-point Likert-type scale ranging from 1 not at all or none of the time to 5 a great deal or all of the time or extremely. Individual items on the DFS-SF are reverse coded, and high scores on the DFS-SF indicate a high (good) HRQOL. The reliability of the DFS-SF has been reported to be greater than .7 (Bann et al., 2003). The DFS-SF has been reported to be acceptable for use in clinical settings (Hogg, Peach, Price, Thompson, & Hinchliffe, 2012). A Thai version of the survey was not available, so permission to translate the DFS-SF into Thai was granted from the Mapi Research Trust™ (Lyon, France). The standard process for forward and back translation was undertaken using a panel of bilingual nutritionists, nurses, and clinicians (Polit & Beck, 2012; Van Nes, Abma, Jonsson, & Deeg, 2010).
Self-Management Relating to Foot Care
Self-management relating to foot care was assessed using the VA-Diabetes Foot Care Survey (Olson et al., 2009), which included subscales on education received about foot care, foot care practices, and barriers to foot care. Education received about foot care comprised of 13 items that were scored on a 4-point scale that classified amount of knowledge (see Table 2). Practices relating to foot care were measured using 14 items and were scored on a 5-point scale that classified the frequency of the practices. Barriers to foot care were measured using 14 items, and patients had to select the items that they considered were a barrier. Permission to translate the VA-Diabetes Foot Care Survey was granted by Olson et al. (2009). The VA-Diabetes Foot Care Survey was translated into Thai, and standard translation methods were followed using a panel of bilingual nutritionists, nurses, and clinicians (Polit & Beck, 2012; Van Nes et al., 2010).
Table 2.
Education Received on Foot Care Using the VA-Diabetes Foot Care Survey (n = 41).
| Item (item number) | Nothing at all (%) | A little bit (%) | Some, but would like to know more (%) | Enough (%) |
|---|---|---|---|---|
| Using a special mirror (6) | 51.2 | 2.4 | 39.0 | 7.3 |
| Gently filing calluses (8) | 46.3 | 4.9 | 34.1 | 14.6 |
| Not cutting corns or calluses with scissors (10) | 43.9 | 4.9 | 46.3 | 4.9 |
| Cutting nails (9) | 41.5 | 2.4 | 39.0 | 17.1 |
| Avoiding hot or cold (7) | 34.1 | 12.2 | 36.6 | 17.1 |
| Always wearing shoes (4) | 22.0 | 14.6 | 51.2 | 12.2 |
| Keep skin moist (5) | 19.5 | 12.2 | 48.8 | 19.5 |
| Check feet regularly (1) | 14.6 | 26.8 | 34.1 | 24.4 |
| Not using drugstore chemicals or other remedies not ordered by health-care providers (11) | 14.6 | 19.5 | 39.0 | 26.8 |
| Choosing proper shoes (3) | 12.2 | 19.5 | 39.0 | 29.3 |
| Whom to call for foot problems (13) | 12.2 | 19.5 | 46.3 | 22.0 |
| Keeping feet clean (2) | 7.3 | 19.5 | 34.1 | 39.0 |
| When to call for foot problems (12) | 7.3 | 19.5 | 48.8 | 24.4 |
Ethical Approval
All procedures performed in this research were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (Rickham, 1964). The study was approved by the Human Research Ethics Committee, University of Wollongong (HE 16/209) and Uttaradit Hospital, Thailand (21/2016).
Statistical Analysis
All data were entered into SurveyMonkey© and then exported into SPSS version 21.0 (SPSS Inc., Chicago, IL) for analysis. The scoring of the DFS-SF was based on the sum of all items; the raw items were reverse coded according to author guidelines. The scores for each dimension were transformed on a scale from 0 to 100, with high score indicating better HRQOL (Bann et al., 2003). Descriptive statistics were used to summarize the demographic and clinical characteristics: HRQOL scores and self-care management relating to foot care.
Results
Sample Characteristics
Data were obtained from 41 patients with DFUs who attended the foot clinic. The majority of the participants were female (n = 24, 58.5%). The mean age of the participants was 62.1 years, 68.2% of participants were living with a partner, 85.3% were employed, and 82.9% were earning 0 to 10,000 Baht/month. Approximately half (48.8%) of participants were using oral diabetic medications. The mean duration of diabetes was 12.0 ± 8.5 years, the mean hemoglobin A1c (%) was 8.1 ± 2.1, and the mean body mass index was 28.0 ± 7.9 (see Table 1). All participants had DFUs that were Wagner’s Grade 1 (82.9%) or Grade 2 (17.1%).
Health-Related Quality of Life
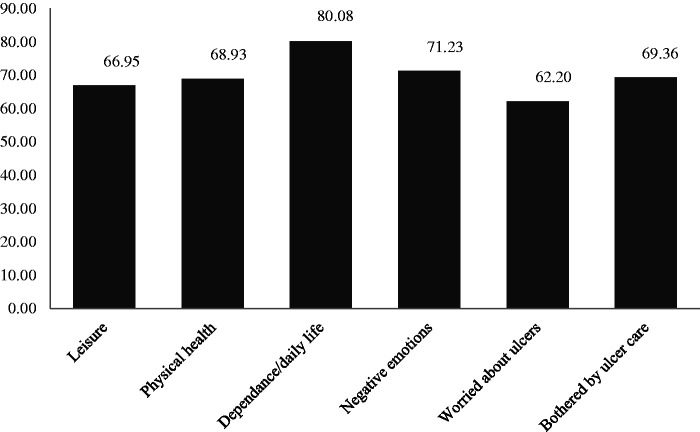
The scores for HRQOL for the six domains were as follows: leisure (66.95 ± 28.03), physical health (68.93 ± 28.51), dependence or daily life (80.08 ± 25.23), negative emotions (71.23 ± 29.48), worried about ulcers (62.20 ± 31.97), and bothered by ulcer care (69.36 ± 25.20; Figure 1). High scores on the DFS-SF indicate a high (good) HRQOL.
Figure 1.
Diabetic Foot Scale-Short Form subscale scores for HRQOL among people with DFUs (n = 41). High scores indicate a high (good) HRQOL.
Education Received About Foot Care (VA-Diabetes Foot Care Survey)
The findings provide a summary of the participants’ recollection of the education they received about foot care and self-care management of their feet (see Table 2). A large percentage of participants reported that they received no education at all about using a special mirror to check under their feet (51.2%), gently filing calluses (46.3%), not cutting corns or calluses with scissors (43.9%), cutting their toe nails (41.5%), and avoiding extremes in temperature (either hot or cold; 34.1%). Only 39.0% of participants reported that they had received enough education about keeping their feet clean. Wearing shoes at all times is an important self-care management strategy for preventing DFUs. Only 12.2% of participants reported that they received enough education on always wearing shoes, and a further 51.2% received some education but would like to know more.
Barriers to Foot Care (VA-Diabetes Foot Care Survey)
The findings summarize the perceived barriers by participants to undertaking self-care management of their feet (see Table 3). The most significant barriers to good foot care were not having a mirror to check their feet (48.8%), not having the correct shoe inserts (41.5%), and either knowing what to do but not knowing how to care for their feet (36.6%) or not knowing how to care for their feet (34.1%). Some of the items assessed attitudes and actions as barriers such as “I couldn’t remember to do it” (26.8%), “I didn’t have time” (14.6%), and “I didn’t think it was important” (12.2%). These items show that participants understanding about why they were conducted self-care of their feet may have been missing.
Table 3.
Perceived Barriers to Foot Care Using VA-Diabetes Foot Care Survey (n = 41).
| Item (item number) | Total n = 41 (%) |
|---|---|
| I didn’t have a mirror (7) | 48.8 |
| I didn’t have the right shoe inserts (6) | 41.5 |
| I know what to do, but I didn’t know how to do it (2) | 36.6 |
| I didn’t know what to do (1) | 34.1 |
| I couldn’t remember to do it (9) | 26.8 |
| I didn’t have the right shoes (5) | 24.4 |
| I needed professional help (10) | 17.1 |
| I needed help from family and friends (11) | 17.1 |
| I didn’t have time (3) | 14.6 |
| I couldn’t see well enough to do it (13) | 14.6 |
| I couldn’t comfortably reach my feet to do it (14) | 14.6 |
| I didn’t think it was important (12) | 12.2 |
| I couldn’t afford it (4) | 7.3 |
| I didn’t have a foot stool (8) | 4.9 |
Foot Care Practices
These results summarize participants self-reported foot care practices (see Table 4). Nearly all participants reported that they washed their feet every day (97.6%), and most never walked barefoot outside (78.9%). However, 70.7% of participants indicated that they walked barefoot inside their house. The activities which were not conducted by participants were not testing the water temperature (87.8%), not soaking feet for 10 minutes (85.4%), not using lubricants (61.0%), and not looking at the bottom of their feet (24.4%). Trimming their toe nails once a week was performed by 75.6% of participants. Drying between their toes was completed by 63.4% of participants every day and 68.3% of participants checked their shoes every day.
Table 4.
Self-Reported Foot Care Practices Using VA-Diabetes Foot Care Survey (n = 41).
| Items (item number) | Not at all (%) | Daily (%) | Several times a week (%) | Once a week (%) | Once or twice a month (%) |
|---|---|---|---|---|---|
| Tested the water temperature (5) | 87.8 | 2.4 | 2.4 | 7.3 | 0.0 |
| Soaked feet for 10 minutes (4) | 85.4 | 0.0 | 4.9 | 4.9 | 4.9 |
| Walked barefoot outside (14) | 78.9 | 17.1 | 0.0 | 0.0 | 4.9 |
| Filed calluses (8) | 75.6 | 2.4 | 4.9 | 4.9 | 12.2 |
| Used lubricants (7) | 61.0 | 22.0 | 0.0 | 9.8 | 7.3 |
| Changed shoes (12) | 56.1 | 22.0 | 9.8 | 2.4 | 9.8 |
| Wore stocking (11) | 43.9 | 36.6 | 9.8 | 7.3 | 2.4 |
| Looked at the bottom feet (1) | 24.4 | 53.7 | 9.8 | 7.3 | 4.9 |
| Walked barefoot inside (13) | 24.4 | 70.7 | 0.0 | 0.0 | 4.9 |
| Checked between toes (2) | 19.5 | 65.9 | 4.9 | 4.9 | 4.9 |
| Dried between toes (6) | 19.5 | 63.4 | 9.8 | 4.9 | 2.4 |
| Checked shoes (10) | 12.2 | 68.3 | 7.3 | 7.3 | 4.9 |
| Washed feet (3) | 0.0 | 97.6 | 0.0 | 0.0 | 2.4 |
| Trimmed nails (9) | 0.0 | 4.9 | 0.0 | 70.7 | 24.4 |
Discussion
To the best of our knowledge, this is the first study undertaken to investigate the HRQOL, self-reported knowledge on foot care, and actual foot care practices and barriers to foot care in people living with DFUs in Northern Thailand. For participants in this study, scores in all HRQOL domains were high. This result is contradictory to that reported in a cross-sectional study conducted in South India where patients with DFUs had poor HRQOL on all six domains (mean scores ranging between 33.6 and 44.3; Sekhar, Thomas, Unnikrishnan, Vijayanarayana, & Rodrigues, 2015). This result may relate to the fact that participants in our study had less severe DFUs with Wagner’s Grade 1 and Grade 2 DFUs only.
This study used the disease-specific instrument, DFS-SF for assessing the HRQOL among people with DFUs. The DFS-SF captures the specific problems relating to diabetes complications. In our study, participants reported high HRQOL in the domains relating to leisure, physical health, and dependence or daily life, which is similar to other published studies (Hui, Yee-Tak Fong, Yam, & Yuk Ip, 2008; Macioch et al., 2017; Valensi et al., 2005). This result is interesting as the high HRQOL in the domain relating to dependence or daily life could be due to the fact that the participants had family or social support to assist with daily living activities. In addition, most of the participants have lived with DFUs for an average of 2 years, which could mean that over time they learnt to adapt and promote their independence in tasks such as cooking, dressing, and organizing their daily life.
Low scores indicating poor HRQOL were observed in the domain “worried about ulcers,” which is congruent with the literature (Hui et al., 2008; Valensi et al., 2005). It could be postulated that the poor HRQOL in this domain may be due to people being concerned about the development of further ulcers, the existing ulcers not healing, the development of wound infection, and the fear of amputation. Care of a foot ulcer can require multiple visits to foot clinics over a long period of time before the ulcer heals. Finding time to attend the clinics might also be a cause of concern as the majority of the participants were employed.
Education About Foot Care
Only a third of the participants indicated that they had received education about the various aspects of foot care. Nearly half the participants indicated that they did not know about using mirrors to check the toes, cutting toenails, and not using scissors to cut corns or calluses. This lack of knowledge is reflected in the poor practices relating to foot care with just over half the participants indicating that they checked and dried between the toes and trimmed their toenails. The low rates relating to checking the feet and toes regularly could be due to the lack of resources such as mirrors and foot stools and lack of assistance to undertake foot care. Furthermore, participants indicated that they were unaware of what to do or who to call if they did find a foot problem. This provides insight into the nature of education that participants had received and the need for education and behavior change to achieve good self-care management practices among people with DFUs.
A large proportion of participants indicated that they walked barefoot inside the house but not outside the house. This could be due to the fact that walking barefoot inside the house is culturally appropriate for Thai people (Rerkasem, 2011). Almost all participants indicated that they washed their feet every day; this could be due to the habitual rituals for Thai people to wash their feet. The majority of the participants reported that they did not test the water temperature. This question may have been misinterpreted as formally testing the water temperature with a thermometer. Testing the water temperature with an elbow is a practical way to test the water temperature prior to bathing or soaking. The results from this study indicate that strategies that are culturally appropriate to improve knowledge relating to foot care are required. This would include knowing when and who to call for foot problems, the process of checking feet regularly and keeping skin moist. Including information on why this is important may assist with behavior change.
Barriers to Foot Care
Surprisingly, the biggest barrier to foot care was not having a mirror to check the base of the feet. Other studies have found that people with DFUs who did not practice foot self-care were 2.52 times more likely to develop DFUs (Mariam et al., 2017). The process of regularly checking the feet is important for prevention and early recognition of problems. Many people with DFUs cannot reach and see under their feet, so a mirror is an important piece of equipment for foot self-care practices.
The importance of good knowledge relating to foot care is vital for the management of DFUs. In this study, low knowledge of foot care was reported by more than a third of the participants. These results are significantly poor when compared with that reported in the literature. The poor knowledge could be due to the fact that nearly three quarters of participants in the study had only primary school education. Low levels of education and health literacy have previously been associated with poor foot self-care practices (Chiwanga & Njelekela, 2015). In addition, it is possible that participants did not receive appropriate education when they visited health professionals. This may be due to lack of time for the patient and the health professional or lack of resources. Usual care in Thailand involves people who are newly diagnosed with diabetes mellitus attending an outpatient appointment to receive follow-up care related to knowledge of diabetes, self-care management, and treatment of DFUs (if present). Diabetes outpatient clinics are usually very busy and overcrowded (Tantitharanukul & Throngjai, 2018). In addition, specialist positions such as Podiatrists and Diabetes Educators are often fulfilled by nurses in rural areas where such specialists are not available. The American Diabetes Association recommends providing Diabetes Self-Management education and training to those people who are diagnosed with diabetes mellitus (Powers et al., 2017). It is not clear whether these recommendations are always fulfilled in all outpatient clinics in Thailand. In addition to not having adequate knowledge, not having the right shoes and a mirror to check the feet were identified as barriers by nearly half of the participants. Improving education and providing advice for selecting shoes and providing appropriate resources (such as mirrors) should be implemented so that participants can ensure they have the equipment they need to protect their feet. The provision of education about good self-care management of the feet is an important strategy for preventing DFUs and assisting healing of DFUs.
Strengths and Limitations
The strength of the study was the rigor in which it was conducted. First, the use of a validated disease-specific instrument to measure HRQOL enabled data to be captured that is specific to DFUs. In most studies examining HRQOL in people with DFUs, generic tools such as the SF-36 are used (Boutoille et al., 2008; Carlos De Meneses, Blanes, Francescato Veiga, Gomes, & Ferreirai, 2011; Garcia-Morales et al., 2011; Ribu et al., 2007b; Sanjari et al., 2011; Yao et al., 2012). Second, the questionnaire was available for self-report and as an interview so that participants with literacy issues were also included. The limitations of this study relate to sampling. Although the sample size is small (41), 100% of people with a DFU who attended the Outpatient Diabetes Clinic at Uttaradit Hospital over the study period agreed to participate in the survey. The small sample size means that the findings may not be representative of all people with DFUs in Thailand. Moreover, this study was undertaken in one hospital in Northern Thailand, and the majority of the participants had low-grade DFUs (Grades 1 and 2) as measured by the Wagner’s Classification Scale. Finally, the data were obtained through a survey, which was cross-sectional in nature and only enabled those receiving treatment at the foot clinic during the recruitment period to participate. Future research should focus on large, well-designed multicenter trials to investigate the HRQOL and foot self-management practices of Thai people with DFUs of varying severities.
Implications for Practice
The findings have implications for health-care professionals who provide education to people with diabetes mellitus, to health-care professionals who provide education to people with DFUs, and to policy makers and funding bodies. This study underlines the significance of foot self-care management practices on HRQOL among people who have diabetes (both with and without DFUs). The findings from this study can be used to develop diabetes education programs for people with diabetes in Northern Thailand. Education programs must provide practical skills and education about why activities are important so that participants understand the need for the self-care management and the impact it has on preventing or healing DFUs.
Conclusions
This is the first study that has investigated HRQOL and foot self-care practices of people with DFUs in Northern Thailand. The results indicate the need for individualized and focused foot care education that includes self-care management practices to improve HRQOL.
Acknowledgments
The authors wish to thank all participants who took part in this study and all the research assistants who helped to gather data from participants. The authors would like to thank Gayle Netto for her help with SurveyMonkey. The authors would also like to thank Mr. Denis Bristow for his assistance in editing the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Abetz L., Sutton M., Brady L., McNulty P., Gagnon D. D. (2002) The Diabetic Foot Ulcer Scale (DFS): A quality of life instrument for use in clinical trials. Practical Diabetes International 19(6): 167–175. [Google Scholar]
- Aljasem L. I., Peyrot M., Wissow L., Rubin R. R. (2001) The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. The Diabetes Educator 27(3): 393–404. [DOI] [PubMed] [Google Scholar]
- Ashford R. L., McGee P., Kinmond K. (2000) Perception of quality of life by patients with diabetic foot ulcers. Diabetic Foot Journal 3(4): 150–155. [Google Scholar]
- Bann C. M., Fehnel S. E., Gagnon D. D. (2003) Development and validation of the Diabetic Foot Ulcer Scale-short form (DFS-SF). Pharmacoeconomics 21(17): 1277–1290. [DOI] [PubMed] [Google Scholar]
- Boulton A. J. (2010) What you can’t feel can hurt you. Journal of Vascular Surgery 52(3): 28S–30S. [DOI] [PubMed] [Google Scholar]
- Boutoille D., Feraille A., Maulaz D., Krempf M. (2008) Quality of life with diabetes-associated foot complications: Comparison between lower-limb amputation and chronic foot ulceration. Foot & Ankle International 29(11): 1074–1078. doi:10.3113/FAI.2008.1074. [DOI] [PubMed] [Google Scholar]
- Carlos De Meneses L., Blanes L., Francescato Veiga D., Gomes H. C., Ferreirai L. M. (2011) Health-related quality of life and self-esteem in patients with diabetic foot ulcers: Results of a cross-sectional comparative study. Ostomy Wound Management 57(3): 36–43. [PubMed] [Google Scholar]
- Carrington A. L., Abbott C. A., Griffiths J., Jackson N., Johnson S. R., Kulkarni J., Boulton A. J. M. (2001) A foot care program for diabetic unilateral lower-limb amputees. Diabetes Care 24(2): 216–221. [DOI] [PubMed] [Google Scholar]
- Castro-Sánchez A. M., Matarán-Peñarrocha G. A., Granero-Molina J., Aguilera-Manrique G., Quesada-Rubio J. M., Moreno-Lorenzo C. (2011) Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evidence-Based Complementary and Alternative Medicine 2011: 561753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chellan G., Srikumar S., Varma A. K., Mangalanandan T. S., Sundaram K. R., Jayakumar R. V., Kumar H. (2012) Foot care practice—The key to prevent diabetic foot ulcers in India. Foot 22(4): 298–302. doi:10.1016/j.foot.2012.08.007. [DOI] [PubMed] [Google Scholar]
- Chiwanga F. S., Njelekela M. A. (2015) Diabetic foot: Prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania—A cross-sectional study. Journal of Foot & Ankle Research 8(1): 1–7. doi:10.1186/s13047-015-0080-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desalu O. O., Salawu F. K., Jimoh A. K., Adekoya A. O., Busari O. A., Olokoba A. B. (2011) Diabetic foot care: Self reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Medical Journal 45(2): 60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Morales E., Lazaro-Martinez J. L., Martinez-Hernandez D., Aragon-Sanchez J., Beneit-Montesinos J. V., Gonzalez-Jurado M. A. (2011) Impact of diabetic foot related complications on the Health Related Quality of Life (HRQol) of patients—A regional study in Spain. International Journal of Lower Extremity Wounds 10(1): 6–11. doi:10.1177/1534734611400257. [DOI] [PubMed] [Google Scholar]
- Glasgow R. E., Hiss R. G., Anderson R. M., Friedman N. M., Hayward R. A., Marrero D. G., Vinicor F. (2001) Report of the health care delivery work group: Behavioral research related to the establishment of a chronic disease model for diabetes care. Diabetes Care 24(1): 124–130. [DOI] [PubMed] [Google Scholar]
- Goodridge, D., Trepman, E., Sloan, J., Guse, L., Strain, L. A., McIntyre, J., & Embil, J. M. (2006). Quality of life of adults with unhealed and healed diabetic foot ulcers. Foot & Ankle International, 27(4), 274–280. [DOI] [PubMed]
- Hogg F. R., Peach G., Price P., Thompson M. M., Hinchliffe R. J. (2012) Measures of health-related quality of life in diabetes-related foot disease: A systematic review. Diabetologia 55(3): 552–565. doi:10.1007/s00125-011-2372-5. [DOI] [PubMed] [Google Scholar]
- Hui L. F., Yee-Tak Fong D., Yam M., Yuk Ip W. (2008) Translation and validation of the Chinese diabetic foot ulcer scale-short form. Patient 1(2): 137–145. [DOI] [PubMed] [Google Scholar]
- Ikem R. T., Ikem I. C., Ola B. A. (2009) Relationship between depression, cognitive function and quality of life of Nigerians with diabetic foot ulcers. A preliminary controlled study. Acta Endocrinologica 5(1): 75–83. doi:10.4183/aeb.2009.75. [Google Scholar]
- Jaksa P. J., Mahoney J. L. (2010) Quality of life in patients with diabetic foot ulcers: Validation of the Cardiff Wound Impact Schedule in a Canadian population. International Wound Journal 7(6): 502–507. doi:10.1111/j.1742-481X.2010.00733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid J. M. (2014) Rates and risk of hospitalisation among patients with type 2 diabetes: Retrospective cohort study using the UK General Practice Research Database linked to English Hospital Episode Statistics. International Journal of Clinical Practice (Esher) 68(1): 40–48. doi:10.1111/ijcp.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khunkaew, S., Fernandez, R., & Sim, J. (2017). The factors determining the low health related quality of life among people living with diabetic foot ulcers: A systematic review. Paper presented at the International Conference on Diabetes and Diabetic Nursing Care, Charlotte, NC.
- Löndahl M. (2012) Hyperbaric oxygen therapy as treatment of diabetic foot ulcers. Diabetes/Metabolism Research and Reviews 28(Suppl. 1): 78–84. doi:10.1002/dmrr.2256. [DOI] [PubMed] [Google Scholar]
- Macioch T., Sobol E., Krakowiecki A., Mrozikiewicz-Rakowska B., Kasprowicz M., Hermanowski T. (2017) Health related quality of life in patients with diabetic foot ulceration—Translation and Polish adaptation of Diabetic Foot Ulcer Scale short form. Health and Quality of Life Outcomes 15(1): 15–15. doi:10.1186/s12955-017-0587-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariam, T. G., Alemayehu, A., Tesfaye, E., Mequannt, W., Temesgen, K., Yetwale, F., & Limenih, M. A. (2017). Prevalence of diabetic foot ulcer and associated factors among adult diabetic patients who attend the diabetic follow-up clinic at the University of Gondar Referral Hospital, North West Ethiopia, 2016: Institutional-based cross-sectional study. Journal of Diabetes Research2017, 2879249. [DOI] [PMC free article] [PubMed]
- Meijer, J. W., Trip, J., Jaegers, S. M., Links, T. P., Smits, A. J., Groothoff, J. W., & Eisma, W. H. (2001). Quality of life in patients with diabetic foot ulcers. Disability and Rehabilitation, 23(8), 336–340. [DOI] [PubMed]
- Nabuurs-Franssen M. H., Huijberts M. S. P., Nieuwenhuijzen Kruseman A. C., Willems J., Schaper N. C. (2005) Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia 48(9): 1906–1910. [DOI] [PubMed] [Google Scholar]
- Olson J. M., Hogan M. T., Pogach L. M., Rajan M., Raugi G. J., Reiber G. E. (2009) Foot care education and self management behaviors in diverse veterans with diabetes. Patient Preference and Adherence 3: 45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polit D. F., Beck C. T. (2012) Nursing research: Generating and assessing evidence for nursing practice, 9th ed Sydney, Australia: Wolters Kluwer Health/Lippincott Williams & Wilkins. [Google Scholar]
- Powers M. A., Bardsley J., Cypress M., Duker P., Funnell M. M., Fischl A. H., Vivian E. (2017) Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diabetes Educator 43(1): 40–53.28118121 [Google Scholar]
- Rerkasem K. (2011) Seminar review: Sociocultural practices and epidemiology of diabetic foot problem: Lessons from a study in Chiang Mai University Hospital, Thailand. The International Journal of Lower Extremity Wounds 10(2): 86–90. doi:10.1177/1534734611406102. [DOI] [PubMed] [Google Scholar]
- Reutrakul S., Deerochanawong C. (2016) Diabetes in Thailand: Status and policy. Current Diabetes Reports 16(3): 1–10. [DOI] [PubMed] [Google Scholar]
- Rickham, P. P. (1964). HUMAN EXPERIMENTATION. CODE OF ETHICS OF THE WORLD MEDICAL ASSOCIATION. DECLARATION OF HELSINKI. British Medical Journal, 2(5402), 177–177. [DOI] [PMC free article] [PubMed]
- Ribu L., Birkeland K., Hanestad B. R., Moum T., Rustoen T. (2008) A longitudinal study of patients with diabetes and foot ulcers and their health-related quality of life: Wound healing and quality-of-life changes. Journal of Diabetes and Its Complications 22(6): 400–407. doi:10.1016/j.jdiacomp.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Ribu L., Hanestad B. R., Moum T., Birkeland K., Rustoen T. (2007. a) A comparison of the health-related quality of life in patients with diabetic foot ulcers, with a diabetes group and a nondiabetes group from the general population. Quality of Life Research 16(2): 179–189. doi:10.1007/s11136-006-0031-y. [DOI] [PubMed] [Google Scholar]
- Ribu L., Hanestad B. R., Moum T., Birkeland K., Rustoen T. (2007. b) Health-related quality of life among patients with diabetes and foot ulcers: Association with demographic and clinical characteristics. Journal of Diabetes and Its Complications 21(4): 227–236. doi:10.1016/j.jdiacomp.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Ribu L., Rustøen T., Birkeland K., Hanestad B. R., Paul S. M., Miaskowski C. (2006) The prevalence and occurrence of diabetic foot ulcer pain and its impact on health-related quality of life. The Journal of Pain: Official Journal of the American Pain Society 7(4): 290–299. [DOI] [PubMed] [Google Scholar]
- Sanjari, M., Safari, S., Shokoohi, M., Safizade, H., Rashidinezhad, H., Mashrouteh, M., & Alavi, A. (2011). A cross-sectional study in Kerman, Iran, on the effect of diabetic foot ulcer on health-related quality of life. International Journal of Low Extremity Wounds, 10(4), 200–206. doi:10.1177/1534734611428728. [DOI] [PubMed]
- Sarinnapakorn V., Sunthorntepwarakul T., Deerochanawong C., Niramitmahapanya S., Napartivaumnuay N. (2016) Prevalence of diabetic foot ulcers and risk classifications in type 2 diabetes mellitus patients at Rajavithi Hospital. Journal of the Medical Association of Thailand 99(2): S99–S105. [PubMed] [Google Scholar]
- Sekhar, M. S., Thomas, R. R., Unnikrishnan, M., Vijayanarayana, K., & Rodrigues, G. S. (2015). Impact of diabetic foot ulcer on health-related quality of life: A cross-sectional study. Seminars in Vascular Surgery, 28(3-4), 165–171. [DOI] [PubMed]
- Settakorn J., Rangdaeng S., Arpornchayanon O., Lekawanvijit S., Bhoopat L., Attia J. (2005) Why were limbs amputated? An evaluation of 216 surgical specimens from Chiang Mai University Hospital, Thailand. Archives of Orthopaedic and Trauma Surgery 125(10): 701–705. doi:10.1007/s00402-005-0060-y. [DOI] [PubMed] [Google Scholar]
- Siersma V., Thorsen H., Holstein P. E., Kars M., Apelqvist J., Jude E. B., Schaper N. C. (2014) Health-related quality of life predicts major amputation and death, but not healing, in people with diabetes presenting with foot ulcers: The Eurodiale study. Diabetes Care 37(3): 694–700. doi:10.2337/dc13-1212. [DOI] [PubMed] [Google Scholar]
- Tantitharanukul, N., & Throngjai, T. (2018). Waiting time estimation system for outpatient's arrival planning. Paper presented at the Digital Arts, Media and Technology (ICDAMT), 2018 International Conference on, Phayao, Thailand.
- Valensi P., Girod I., Baron F., Moreau-Defarges T., Guillon P. (2005) Quality of life and clinical correlates in patients with diabetic foot ulcers. Diabetes & Metabolism 31(3 Pt 1): 263–271. [DOI] [PubMed] [Google Scholar]
- Van Nes F., Abma T., Jonsson H., Deeg D. (2010) Language differences in qualitative research: Is meaning lost in translation? European Journal of Ageing 7(4): 313–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh J., Hoffstad O., Sullivan M., Margolis D. (2016) Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabetic Medicine 33(11): 1493–1498. [DOI] [PubMed] [Google Scholar]
- Yao H., Ting X., Minjie W., Yemin C., Xiqiao W., Yuzhi J., Shuliang L. (2012) The investigation of demographic characteristics and the health-related quality of life in patients with diabetic foot ulcers at first presentation. International Journal of Lower Extremity Wounds 11(3): 187–193. doi:10.1177/1534734612457034. [DOI] [PubMed] [Google Scholar]
- Yekta Z., Pourali R., Ghasemi-Rad M. (2011) Comparison of demographic and clinical characteristics influencing health-related quality of life in patients with diabetic foot ulcers and those without foot ulcers. Diabetes, Metabolic Syndrome and Obesity 4: 393–399. doi:10.2147/DMSO.S27050. [DOI] [PMC free article] [PubMed] [Google Scholar]