Abstract
Telemedicine or tele-health is increasingly used to help meet challenges in health care linked to demographic changes and an aging population. This study aimed to investigate whether a tele-health solution, an “app” presented on a tablet, can assist patients in their recovery following a hip fracture and accommodate individual learning and health literacy needs to support them in self-care and empowerment. Twenty patients with a hip fracture were informed and educated using an app during hospital admission and for 3 to 4 weeks after discharge. A qualitative approach employed field observation and individual interviews with patients and their relatives. Data were analyzed using qualitative content analysis. Patients found that the app supported their ability to perform self-care and their desire for autonomy. They would not have downloaded the app by themselves but found the use of the app presented on a tablet very supportive in their everyday life while rehabilitating after a hip fracture. Findings indicate that health-care professionals can support information and education for patients with a hip fracture using an app that accommodates different learning styles. This demonstrates that apps used for the dissemination of health knowledge can be used by elderly hip fracture patients even if they are not used to technology.
Keywords: tele-health, hip fracture, fragility fracture, self-care, empowerment, “app”, application, tablet computer, tablet
Introduction
Aging is a universal phenomenon, and it is estimated that, by 2050, the proportion of the population aged 60 years and older will increase in every country (World Health Organization, 2015). The risk of fracture increases with age due to osteoporosis and tendency to fall, with significant consequences (Harvey et al., 2017). The main consequence of osteoporosis is that bone density decreases and the skeleton becomes fragile and prone to fractures, with hip fractures being the most serious of these. Hip fracture is one of the greatest challenges facing health-care systems globally (Kanis et al., 2001), as the impacts of fractures are multiple: both for society from a health economics perspective but primarily for the individual in the form of functional decline and early death (Wiktorowicz, Goeree, Papaioannou, Adachi, & Papadimitropoulos, 2001). Sustaining a fragility fracture at least doubles the risk of future fractures. Models of care have been developed in many countries to prevent subsequent fractures including both osteoporosis management and interventions to prevent falls (Akesson et al., 2013; Ambrose, Cruz, & Paul, 2015; British Orthopaedic Association, 2007).
In future health-care systems, it is expected that individuals will have a more dominant role in taking care of their own health and rehabilitation (Clemensen, Rothmann, Smith, Caffery, & Danbjorg, 2017; Ministry of Health, 2017). At the same time, development is focused on improving patient pathways by making them systematized with the aim of reducing inefficiency and delivering best clinical practice (Egerod et al., 2010; Husted, 2012; Kehlet & Dahl, 2003). These systematized programs for improving efficiency in the hospital setting also mean that patients’ hospitalization times are reduced. Shorter length of hospital stay (LOS) provides health-care professionals with fewer opportunities to deliver patient information and education (Jensen, Smith, Overgaard, Wiil, & Clemensen, 2017), so a new way of providing patients with information and education is needed so that they can be empowered to perform self-care after hospital discharge.
One way of supporting individuals is by the use of tele-health. Tele-health is a way of using technology to support the delivery of tailored health care (Choi, Wilson, Sirrianni, Marinucci, & Hegel, 2014). It has been shown to facilitate occupational and physical therapy programs as well as improving management of chronic conditions (Lee, Greenfield, & Pappas, 2018; Tenforde, Hefner, Kodish-Wachs, Iaccarino, & Paganoni, 2017) and has the potential to improve patient satisfaction. Several studies concerned with improving pathways using tele-health have shown one approach to successfully creating effective technological solutions is by working with users through participatory design (Clemensen, Larsen, Kyng, & Kirkevold, 2007; Danbjorg, Wagner, & Clemensen, 2014; Garne Holm, Brodsgaard, Zachariassen, Smith, & Clemensen, 2017). Likewise, studies have demonstrated that innovative information and communication technology can play a significant role in providing care for elderly patients in their own homes (Changizi & Kaveh, 2017).
This study is part of a participatory design research project exploring whether the care of patients with osteoporotic hip fracture can be promoted by tele-health. In the first phase of the overall research project, patients’ needs were identified (Jensen et al., 2017). We found a gap between patient-needs and what was provided by the health-care system. In the second phase, a tele-health solution was created in collaborative workshops with the participation of patients, health-care professionals, and software designers (Jensen, Overgaard, Wiil, Smith, & Clemensen, 2018). The tele-health solution created was an “app” (smart phone application) designed to support the needs of patients following a hip fracture by empowering them to self-care. This article reports on the third phase of the project, the testing of the app in a clinical setting. The aim of the study was to examine whether a tele-health solution in the form of an app can support self-care and empowerment of patients following a fragility fracture of the hip and a short LOS.
Methods and Materials
Setting and Sample
The study took place in the orthopedic department of a university hospital in Denmark. We included patients who were discharged to their own homes and who had been independent prior to the hip fracture. A convenience sample was selected of patients who were 65 years or older. The inclusion criteria were as follows: (a) All participants had to be able to walk around and perform activities of daily living without significant assistance from other individuals or agencies (locally, this applies to approximately 60% of patients treated for a hip fracture at the study hospital; Danish Regions, 2017) and (b) the fracture was caused by low-energy trauma, that is fall from standing height or less, indicating osteoporosis. Clinical staff initially identified eligible patients and asked if they were willing to participate in a study about new ways to provide information. On the first postoperative day, included patients were given an iPad™ (from this point forward, the equipment will be referred to as a “tablet”) with the app “My Hip Fracture Journey” installed. The clinical staff introduced patients to the contents of the app. The tablet was meant for patients to take home during the test phase. The tablet and app aimed to support clinical staff in the daily provision of oral and written information and education of patients in accordance with local clinical guidelines. Patients participating in the test phase were given bothoral and written information concerning the hip fracture treatment and according to local guidelines—andthe tablet. The app was also downloadable from an online application store. Participants were contacted by the first author (C. M. J.) before discharge to plan a postdischarge interview. The test phase commenced in December 2017 and ended in May 2018.
The “My Hip Fracture Journey” App
The design of the app was based on the identified needs of patients with a hip fracture, and its development is reported in depth in a previous article (Jensen et al., 2017). The “My Hip Fracture Journey” app aimed to accommodate individual needs and learning styles and contained four main features:
pictographs,
video clips,
illustrated exercises, and
written information.
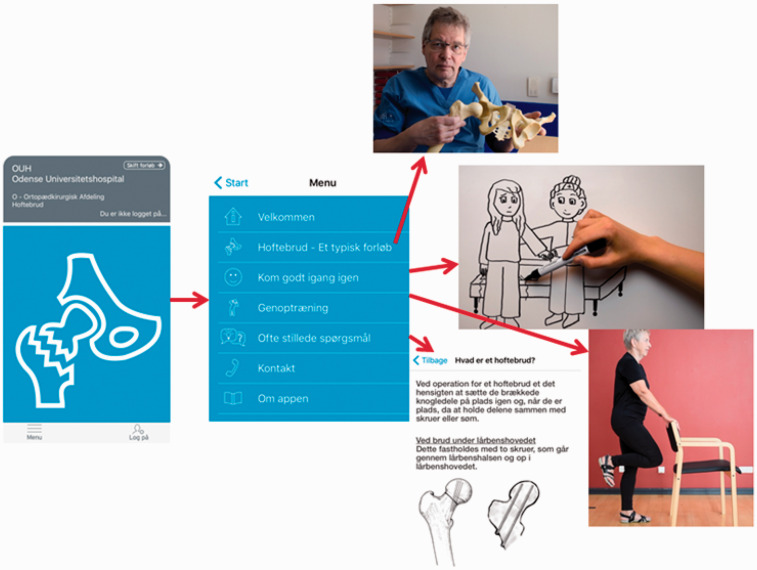
The app was introduced with a recognizable logo representing a fractured hip. Pictographs were used to illustrate a typical treatment pathway, including tips and tricks for individuals to get back on their feet again after the operation. Video clips provided narratives from other patients. Information or education concerning the LOS and rehabilitation was provided through short video clips featuring different health professionals. Eight exercise videos were presented by an older woman and narrated by a physiotherapist. Short, factual, and written information (FAQs) were also provided based on questions agreed on by health-care professionals over a period of 2 months. The font of the written material was made larger to accommodate potential visual impairment (Figure 1).
Figure 1.
The recognizable logo introducing the app and some of the features included in the app.
The tablet had only this one app installed to make it easier to use for individuals not familiar with the device. The tablet was fitted with an outer cover to prevent damage and to accommodate infection prevention guidelines as the tablet had to be returned to the hospital after having been used in patients’ homes. Not all individuals have access to WIFI Internet at home, so a SIM card was installed. To improve ease of use, a green dot marked the on or off button, and stylus pens were provided to accommodate arthritic fingers.
Definition of Key Concepts
For the purposes of this study, empowerment was defined as “a process through which people gain greater control over decisions and actions affecting their health” (World Health Organization, 1998, p. 6) and measured by the following underlying questions:
Did the patients know what health services were available and the possibility of using these in relation to rehabilitation?
Were the patients able to cope with parts of or the full rehabilitative treatment?
Were the patients able to take responsibility for their lives and did they seek to modify and maintain changes in life habits, that is, to prevent new fractures?
Were the patients able to handle negative emotions either by themselves or in cooperation with their network or, for instance, with other patients with similar problems?
Self-care was defined according to the Orem’s (2001)model of nursing as: “… practice of activities that individuals initiate and perform on their own behalf in maintaining life, health and well-being” (p. 117).
Data Collection
Participant observation was performed by the first author for an average of 8 hours per week at the hospital during the test phase. Field notes were taken concurrently in accordance with Spradley’s (1980)recommendations. The observations were made through moderate participation while trying to maintain a balance between “insider” and “outsider” roles (Spradley, 1980). Informal conversations and interviews were conducted with staff with a focus on the objectives of the study. These observations and informal interviews were conducted to generate data on the usability of the app and the tablet.
The aim was primarily to uncover patients’ experiences of using the app and how they felt supported by the app. Narrative interviews are a means of creating an informal atmosphere and collecting individuals’ own stories about their experiences (Anderson & Kirkpatrick, 2016; Kvale, 1996). Individual interviews were conducted by the first author with patients in their homes as a conversation but with an underlying interview guide. For those patients with a spouse, the spouse also participated in the interview. One patient chose to have her son-in-law present. Field notes were taken after each interview. The interviews lasted between 29 and 86 minutes. An interview guide had been compiled according to the recommendations of Spradley (1979)and Kvale (1996), reflecting the key concepts and aims of the study. Interviews were audio recorded and transcribed verbatim by the first author and conferred with the last author. The transcribed data were in Danish and have been translated to English for the purposes of this article. Patients were included until apparent saturation of data was reached, and no new themes emerged in the interviews.
Ethical Considerations
Ensuring that participants were not harmed by taking part in the research preceded the objective to create new knowledge. The voluntary nature of participation was repeatedly stressed. Oral and written information about the study was provided to the patients during hospital stay and, again, at the time of interview. Written consent was obtained at the time of interview as a prior study (Jensen et al., 2017) had shown that patients were in a shock like state of mind and therefore more vulnerable during the hospital stay.
Approval was obtained from the Regional Health Service and University Research Ethics Committee and the Danish Data Protection Agency (case approval no. 15/11860).
Data Analysis
Data analysis focused on the participants’ experiences of use of the app presented on the tablet and the impact on how they experienced life after a hip fracture while considering the aims of the study and the research questions. The transcribed text was gradually reduced and analyzed using qualitative content analysis (Elo & Kyngas, 2008) and included the following phases:
All transcripts and written data from observations and informal interviews were repeatedly read to achieve a sense of the whole and become immersed in the data.
Open coding was conducted; thoughts and headings identified were noted in the text while reading each interview transcript and notes were subsequently organized into a preliminary analysis.
The transcripts were divided into units of meaning and connected to each other and to the aim of the study.
Initial labels for codes and subcategories were created and organized.
This primary coding was conducted by the first and last author in collaboration and, subsequently, the process of analysis was appraised and debated by all authors to increase validity. Likewise, selected quotes and associated coding were discussed.
Finally, categories were produced from subcategories to give a general description of the content and association with use of the app and the tablet.
Results
A total of 25 patients who met the inclusion criteria were included in the test period. Five participants dropped out due to changing their mind about participation. The test phase ended in May 2018 with 20 patients having tested the app using the tablet in hospital and at home. Five of these patients had only used the tablet at the hospital, and, of these, only two were able to recall the contents. The same five patients also did not remember being introduced to how to use the tablet. These five patients were primarily in the first part of the test phase. One of these five patients (P2, as presented in Table 1) had been shown some of the contents of the app by clinical staff during their hospital stay, but the patient had not independently initiated its use. Eight of the participants had relatives who had also used the app. Participants’ ages ranged from 65 years to 91 years. Seven men and 13 women participated. A summary of participant characteristics and their use of the tablet and app is provided in Table 1.
Table 1.
Participant Characteristics.
| Gender | Age | Living Circumstances | Prior Occupation | IT skills | Use of Test Tablet and App: at the Hospital/ at Home/Relatives | |
|---|---|---|---|---|---|---|
| P1 | Female | 70 | With spouse | Secretary | CCT | −/+/+ |
| P2* | Female | 84 | Alone | Cleaning lady | CC | −/−/− |
| P3* | Female | 78 | With spouse | Shop assistant | CC | (+)/−/− |
| P4 | Male | 68 | With spouse | Blacksmith | CC | −/+/+ |
| P5 | Female | 74 | Alone | Farm assistant | CCT | −/+/− |
| P6 | Male | 78 | With spouse | Carpenter | CC | (+)/−/− |
| P7 | Female | 89 | With spouse | Restaurant employee | C | (+)/−/− |
| P8* | Male | 82 | Alone | Janitor | CC | +/+/− |
| P9 | Male | 65 | Alone | IT technician | CC | (+)/−/− |
| P10 | Female | 81 | With spouse | Shop assistant | CC | +/+/+ |
| P11 | Male | 90 | With spouse | Chauffeur | CC | +/+/+ |
| P12 | Female | 70 | Alone | Teacher | CCT | (+)/+/− |
| P13* | Female | 72 | Alone | Optician | CC | +/+/− |
| P14 | Male | 84 | Alone | Farm manager | CC | +/(+)/− |
| P15 | Male | 79 | Alone | Electrician | CC | (+)/+/− |
| P16 | Female | 81 | With spouse | Secretary | CC | +/+/+ |
| P17 | Female | 91 | Alone | House wife | CT | (+)/(+)/+ |
| P18 | Female | 68 | With spouse | Childminder | CC | (+)/(+)/+ |
| P19 | Female | 74 | With spouse | Translator | CC | (+)/+/− |
| P20 | Female | 81 | Alone | Nursing assistant | CC | +/+/+ |
Note.Participants’ IT skills: C = use of cell phone; CC = use of cell-phone and computer; CCT = use of cell-phone, computer, and tablet. Use of test tablet: − = none; (+) = only together with health-care professionals or other persons; + = often.
Participants who suffered from other illnesses.
Following analysis, two overall themes emerged; whether, or not, participants felt supported by the technological solution. These themes are described by five categories relating to the impact of the hip fracture on individuals’ lives and the usability of the app or tablet: (a) regaining physical ability, (b) support of autonomy, (c) the issue of getting old, (d) usability of the tablet and app, and (e) uncertainty about the future and general attitude toward life. Quotations are used to illustrate the findings. Findings are based solely on participants’ descriptions. We did not log the participants’ activity with the app.
Regaining Physical Ability
Mobility and the consequences of physical impairment on individuals’ everyday lives were the most prominent subject for all participants. They had been worried about how to cope at home following discharge but were positively surprised by their daily improvements. Rehabilitation toward better physical capacity was an ongoing and very highly valued issue for all participants whether they had used the tablet or not. All the participants who used the tablet at home felt positive about the exercises shown in the app. They found them easy to perform and very instructive and helpful in their rehabilitation. This enabled them to do the exercises at their own convenience and gave them a feeling of being in control of their own life:
… I was able to do the exercises from that (points at the tablet) before the therapist from the municipality came … so we could carry on with a new set … but I still do the ones from the tablet in the morning and at night … that suits me fine … (P10)
To be able to, for instance, drive a car if they had done so prior to the hip fracture, was also an important goal connected with both independence and the maintaining social contact. Setting short-term goals, as discussed in the examples in the app, was seen as valuable and useful. A long-term goal for all participants was to regain their prior level of physical mobility, although they all suspected that this was almost impossible. The general opinion was that the clinical staff in the hospital was very busy, but kind and they presented a positive attitude toward patients. They were supportive in a “help to self-help kind of way” (P20). This was seen as positive, as it prepared them for being at home. The participants did not use the exercises in the app much during their hospital stay, finding the written and illustrated information more useful at that time. At home, participants’ practice shifted from using the written information sheets to greater engagement with the app:
Every morning, before getting out of bed, I do five of the exercises presented there (pointing at the tablet) … now I soon know them by heart … later I do the rest [of the exercises] here beside the chair … they show me exactly how to do them. (P11)
Supporting Autonomy
“We are all unique individuals” was explained as the reason why some of the participants did not feel supported by the stories from their peers presented in the app, although it seemed that some of the advice provided in the videos was remembered positively. Nevertheless, when they were asked if they preferred to receive the information from the clinical staff, they all agreed that information from their peers was paramount. Having information readily available at their own convenience was very much appreciated. Many of the participants had varying levels of not being able to remember their time in hospital, and they were pleased that the information provided in the app filled some of the gaps.
Apart from the fact that all participants felt motivated toward the exercises, they all favored different features in the app and found them meaningful in diverse ways. They stated that these features supported their primary wish for autonomy and they were pleased with the “pick and choose” opportunity for information. Similarly, all of the participants who had used the app presented on the tablet declared that it supported them in remembering information given during their stay in hospital. Many of the features had some overlap with each other, but patients only found this promoting individual needs: “we all need it [information] in different ways” (P1).
The Issue of Getting Old
“It is not modern to be old,” was a remark made by a 74-year-old woman (P5) and illustrated how some participants felt disregarded the older they got. Only one participant saw age as a personal hindrance for using the app and answered: “No … we are old” (P3), when asked if she and her husband had used the tablet after discharge. Table 1illustrates that use of the app and the tablet was not connected with age. For other participants, age, or being older, was not given as a reason for not using the app and the tablet, but advice given by peers was sometimes received with caution if it was given by someone older than themselves:
… I did not feel that his story hit me … I could not use it for so much … maybe it would have been more meaningful for me if it was someone who was 30-40-50-60 years old … because, of course, there is a difference in how things proceed the younger you are …(P5)
According to national guidelines (Danish Regions, 2014), patients were offered a dual-energy X-ray absorptiometry (DXA) scan to assess need of treatment for osteoporosis. Consent was also sought for patients to be invited for an outpatient fall assessment. All participants had, in one way or another, taken a stance concerning osteoporosis assessment, and 14 of the 20 participants had accepted the invitation from the hospital for a DXA scan:
… my bones have always been strong, so I do not think I have osteoporosis, but now I have said yes to the assessment … you never know what age does to you now do youT … I mean, how can I just stand and break my hip without having done anything? (P6)
At the time of the interview, all participants had received two or three letters from the hospital inviting them to different clinical outpatient clinics, but very few could overlook what these letters implied. Two of the women had, prior to the hip fracture, been taking anti-osteoporotic treatment. One said:
Hmm … if I have to be totally honest, then I haven’t been taking those pills … I thought: well what will it do for a woman of my age [91 years] … now I think maybe I should have done so … (P18)
Usability of the App and the Tablet
The reasons for not using the app and the tablet originated in lack of prior technology knowledge or lack of interest in technology. However, some also labeled tablets as “just a modern way [of communication]” (P2, P3, and P6), and they did not need this. The son-in-law of one of the participants (P2) was present at the interview. The participant had not used the tablet, only seen the exercises at the hospital:
“… I am not all that much into computers and that kind of thing …” (P2) … “ … maybe you should have had something visual like … they should have shown it to you in real life … a lot of people think that everybody has a computer, but not all do” (son-in-law)—[P2 interrupts] “well, I have no problems with using the computer … it’s just not my focus … I do other things!”
We also found that participants with concurrent illnesses considered those health needs to be of higher significance in their lives and they often did not have surplus energy to concentrate on or use the tablet. Features of the app providing information about the patient pathway and time in hospital were generally only used during hospitalization. Participants were content with the advice that was offered by their peers in the app, but two (P13 and P14) mentioned that they would have liked more videos of previous patients, reflecting patient stories from a more positive approach. The majority found that the stories available in the app helped them to have realistic expectations. Three of the female participants’ spouses were very interested in acquiring information via the app. Several participants stated that their children or grandchildren or children-in-law had been very interested in the information provided in the app.
Findings from field observations and interviews indicated a learning curve for clinical staff in achieving confidence in using the tablet and the app. Challenges included difficulties in learning how to handle the tablet both for the clinical staff and for the patients. The tablet had been equipped with a protective shell that the clinical staff had not previously experienced, so they were unsure how to properly manage this at the beginning of the test phase. Minor issues such as where to adjust the sound and where to connect the charger were additional challenges. Using the app demanded considerable time to achieve confidence with its use, but once clinical staff were familiar with the tablet and the app they found it was a good supplement to their normal routines and that it increased their contact with patients and their needs overall. Participants who had not used the tablet and thus not used the app were in the first third of the test phase.
When participants were asked if they would have used the app if it had not been introduced to it already installed on the tablet provided, they generally said: probably not. Only the husbands of P18 and P11 said that they would probably have downloaded the app or consulted the webpage where the app was also available. There was no pattern in how patients’ relatives were involved in using the app and the tablet and this seemed to be an individual decision.
Uncertainty of the Future and General Attitude Toward Life
This category covers participants’ uncertainty about managing their individual situation, despite having been given oral, written and virtual information, and education. One participant (P19) would have liked a feature in the app informing patients about restrictions following surgery for the hip fracture. She was very uncertain of the dos and the don’ts because her neighbor and a friend, who was a doctor, had given her opposing advice. Even though the app was considered supportive and instructive, it was not able to remove all individuals’ worries and uncertainties about the future. Several of the participants still expressed a need of more individual knowledge, exemplified in the following quote: “what about me—when will I be myself again?” (P6). Having a positive approach to life and characteristics such as stubbornness and patience were seen as contributing to a positive recovery:
I am not born a pessimist I am born an optimist … before the opposite has been proven right then I do not think negatively about different things. (P14)
If patients were concerned about something, they sought advice from their own doctor.
In summary, whether or not participants felt supported by the technological solution was subject to whether they had actually used the app or tablet. Some declared that, although they had not personally needed the app, they were certain that other patients would appreciate it. Likewise, the features of the app were used in different ways by different participants. Videos of health-care professionals explaining a typical pathway were used during the hospital stay, but then were only reviewed if the app and tablet were shown to friends and family members. The exercises were not viewed much during hospitalization, but this feature was revisited several times after discharge by all 15 participants who used the app after discharge. In general, patients’ chronological age was not a barrier to use, although some individuals did describe the concept of “being old” as a barrier to using the app or tablet. Neither was gender an indication of use, although female participants who used the app or tablet and were married tended to be introduced to the app by their spouses. Participants with concurrent illnesses often did not have surplus energy to concentrate on using the app.
Patients and their family members who used the app used it for information on what to expect during hospital treatment and how to rehabilitate after discharge.
Discussion
This study focused on whether a tele-health solution in the form of an app can support self-care and empowerment of patients following a hip fracture and a short stay in hospital. We established that patients found the app and the exercises in the app supportive in promoting their everyday physical function. Our findings relating to the importance of regaining prior physical ability echo other studies in demonstrating that mobility and the physical effects of a hip fracture are the most prominent consequences influencing individuals’ lives (Gesar, Baath, Hedin, & Hommel, 2017; Gorman et al., 2013; Zidén, Scherman, & Wenestam, 2010). Consistent with other research regarding patient perspectives on recovery after hip fracture, we found that a barrier to engaging in physical activity was a feeling of lack of information about what they could physically do without hindering their recovery (McBride, Panrucker, & Clothier, 2011; Sims-Gould, Stott-Eveneshen, Fleig, McAllister, & Ashe, 2017).
A Canadian study aimed to understand recovery after a hip fracture from the patient perspective and identified the value of specific messages such as being positive and that patients needed to be integrated into future education to support recovery (Schiller et al., 2015). In our study, we found that these messages could be integrated into case stories told by former patients and integrated into the app. Stories provided by patients’ peers were found to be instructive and supportive. However, patients had a pronounced view that “we are all unique” (P20), explaining why these stories were not always perceived to be transferable to their own everyday lives.
A Swedish study demonstrated that, although older healthy patients are convinced that they will regain prefracture function, they become insecure during hospitalization because they had to adapt to the situation on a ward where they were passive and dependent on clinical staff (Gesar, Hommel, Hedin, & Baath, 2017). We found that an app with a “pick and choose” solution could be a means of mitigating this dependency and support patients to have greater influence. The app could provide patients with a platform to help them gain greater control over decisions and actions affecting their health and, thereby, support patient empowerment. All participants in our study declared their individual uniqueness and that “one size doesn’t fit all” (P18). Our findings that participants believe they are unique and behave in a manner pertinent to them echoes findings of other studies on patient perspectives (Healee, McCallin, & Jones, 2011, 2017; Jensen et al., 2017). This supports the fact that, for successful information or education of patients, this must be done using a variety of approaches. One study (Healee et al., 2017) concluded that nurses need to understand that older adults will recover in their own way following discharge, often reinterpreting health information to fit their own situations. This supports adult learning theory that implies that adults are self-directed learners, and they need educational materials complementing individuals’ different learning styles (Knowles, Holton, & Swanson, 1973). Participants in our study stated that information in the app supported them and that it felt individually relevant by being presented as a “pick and choose” solution. The app presented on the tablet, thereby, provides an option for educating patients and their relatives in order to meet individual needs and increase health literacy (Gardner, 2015), thus increasing individuals’ ability to perform self-care. We also found that an app providing patients with information about the importance of secondary prevention of fragility fractures after a hip fracture aroused their interest in participation in osteoporosis investigations. As in other studies (Gesar, Baath, et al., 2017; Zidén et al., 2010), participants in our study described the hip fracture as an accident. They found that strategies mediated via the app regarding how to make self-determined subtargets were applicable in their everyday lives. They viewed the hip fracture as a temporary condition as opposed to, for instance, osteoporosis, and they were not inclined to believe they had osteoporosis. Nevertheless, patients demonstrated an interest in having the DXA scan. In comparison with a previous qualitative study of patient perspectives following hip fracture treatment (Jensen et al., 2017), it seemed that their ability to take responsibility for their lives and to prevent new fractures increased. This could be a positive indication that communicating health-care knowledge by using new technology that accommodates different learning styles is more adaptable for end users than the conventional oral and written information.
Acquiring a hip fracture is a violent disruption to individuals’ lives, leading to shock and stress (Gesar, Baath, et al., 2017; Jensen et al., 2017; Zidén et al., 2010). Many of the participants explained this state of mind as being in a bubble during hospital admission or having gaps in their memory. Introducing unknown technology such as a tablet to individuals in a stressful situation may be considered neither optimal nor ethical. Nevertheless, the individuals who participated in the test phase and who had these gaps in their memory felt supported by the app presented on the tablet. A study of the prevalence of health-app-use among older adults in Germany found that they have become an integral part of the self-management of chronic disease (Rasche et al., 2018). This is not in accordance with our findings, as the elderly individuals in our study did not have apps nor tablets integrated into their everyday lives. The use of the Internet, computers, and mobile devices by the elderly population is increasing but not yet widespread. The accessibility of the app through a customized tablet (in the form of an iPad™) to take home with them supported its use but accessing the technology and having to download the app by themselves would probably be a barrier that is difficult to overcome. This issue must be taken into consideration when introducing apps in the acute care of the current cohort of older people.
In a review of promises and pit falls of the use telemedicine-based care for older people, Bujnowska-Fedak and Grata-Borkowska (2015)found that a barrier to introducing new technologies is often the older person themselves. In our study, we also found barriers because of age and age-related cognitive function. Nevertheless, we found that, with extra educational effort by clinical staff or others assisting with the technology, some of these barriers can be overcome. However, functionality of the device used to present the app has to be optimized; otherwise, this “new” way of communication will not fit into elderly individuals’ lives. We found that an app can be a means of increasing the effect of information or education for patients with a hip fracture and, thus, supporting them in their everyday lives after discharge.
Limitations
Participants in our study cannot be viewed as representing average individuals acquiring a hip fracture. They are representatives of individuals having the wish to engage in something new, even though in a stressful situation. In the period when the test phase was conducted, approximately 280 patients were treated and operated for a fragility hip fracture at the hospital in focus. According to the annual report from The Danish Clinical Registries on hip fractures in 2017 (Danish Regions, 2017), 76% of patients came from their own homes prior to the hip fracture incidence. We estimated that around 60% were discharged again to their own homes. This equals to 168 persons in this period. Out of this group, only 25 tested the iPad™ or app. This means that patient participants testing the app could be representing an exclusive group and, feasibly, also a resourceful group. That is, despite their stressful situation, they had the capacity to test the app.
The data were collected in the Danish language. In the process of translation into English, differences in language use and cultural context could mean that the nuances have been altered. Likewise, the findings of this study are contextual and reflect a Danish context.
Implications for Practice
Apps used for dissemination of health-care knowledge can be used by elderly hip fracture patients even if they are not accustomed to technology, but a thorough introduction secures user ability. Clinical staff should be able to assist with accessing the app, as none of the participants who tested the app in our study would have downloaded it by themselves and used it because it was accessible through a tablet taken home with them.
Conclusion
We found that an app can support patients with a hip fracture to perform self-care. The app should feature contents accommodating different learning styles. Patients and their relatives find a “pick and choose” solution such as an app meaningful and supportive in their rehabilitation. Likewise, the app supports patients’ wish for autonomy and being provided with timely information. Similarly, this solution increases individuals’ feeling of having control over decisions and actions affecting their health. This approach to informing or educating patients can support their empowerment as well as that of their relatives, along with the possibility of supporting prevention of further fragility fractures.
The app tested in this study is not a stand-alone solution to support self-care and empowerment of patients following a fragility fracture of the hip, but it can facilitate oral and written information and education.
Future Study
The contents and usability of the app and its impact on clinical staff’s work life will be evaluated in a future study using focus group discussions.
Acknowledgments
The authors wish to thank all participants in the study—both patients and their relatives for testing the app and the tablet and subsequently sharing their experiences—and the clinical staff for their positive participation in the study.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Region of Southern Denmark, the University of Southern Denmark, and the Orthopaedic Department at Odense University Hospital have funded the overall research project.
References
- Akesson K., Marsh D., Mitchell P. J., McLellan A. R., Stenmark J., Pierroz D. D., IOF Fracture Working Group(2013) Capture the Fracture: A Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporosis International 24(8): 2135–2152. doi:10.1007/s00198-013-2348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrose A. F., Cruz L., Paul G.(2015) Falls and Fractures: A systematic approach to screening and prevention. Maturitas 82(1): 85–93. doi:10.1016/j.maturitas.2015.06.035. [DOI] [PubMed] [Google Scholar]
- Anderson C., Kirkpatrick S.(2016) Narrative interviewing. International Journal of Clinical Pharmacy 38(3): 631–634. doi:10.1007/s11096-015-0222-0. [DOI] [PubMed] [Google Scholar]
- British Orthopaedic Association(2007) Blue book on fragility fracture care, London, England: Great Britain Chandlers Printers Ltd. [Google Scholar]
- Bujnowska-Fedak M., Grata-Borkowska U.(2015) Use of telemedicine-based care for the aging and elderly: Promises and pitfalls. Smart Homecare Technology and TeleHealth 3: 91–105. doi:10.2147/SHTT.S59498. [Google Scholar]
- Changizi M., Kaveh M. H.(2017) Effectiveness of the mHealth technology in improvement of healthy behaviors in an elderly population—A systematic review. mHealth 3: 51.doi:10.21037/mhealth.2017.08.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi N. G., Wilson N. L., Sirrianni L., Marinucci M. L., Hegel M. T.(2014) Acceptance of home-based telehealth problem-solving therapy for depressed, low-income homebound older adults: Qualitative interviews with the participants and aging-service case managers. Gerontologist 54(4): 704–713. doi:10.1093/geront/gnt083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemensen J., Larsen S. B., Kyng M., Kirkevold M.(2007) Participatory design in health sciences: Using cooperative experimental methods in developing health services and computer technology. Qualitative Health Research 17(1): 122–130. doi:10.1177/1049732306293664. [DOI] [PubMed] [Google Scholar]
- Clemensen J., Rothmann M. J., Smith A. C., Caffery L. J., Danbjorg D. B.(2017) Participatory design methods in telemedicine research. Journal of Telemedicine and Telecare 23(9): 780–785. doi:10.1177/1357633x16686747. [DOI] [PubMed] [Google Scholar]
- Danbjorg D. B., Wagner L., Clemensen J.(2014) Do families after early postnatal discharge need new ways to communicate with the hospital? A feasibilility study. Midwifery 30(6): 725–732. doi:10.1016/j.midw.2013.06.006. [DOI] [PubMed] [Google Scholar]
- Danish Regions. (2014). DrHoftebrud. In: RKKP (ed.) DrHOFTEBRUD—Annual report(pp. 136). Denmark. Dansih Regions. Retrieved from https://docplayer.dk/12094286-Drhoftebrud-dansk-tvaerfagligt-register-for-hoftenaere-laarbensbrud.html.
- Danish Regions. (2017). DrHoftebrud. Retrieved from Denmark: https://www.sundhed.dk/content/cms/62/4662_hofte-fraktur-%C3%A5rsrapport_2017.pdf.
- Egerod I., Rud K., Specht K., Jensen P. S., Trangbaek A., Ronfelt I., Kehlet H.(2010) Room for improvement in the treatment of hip fractures in Denmark. Danish Medical Bulletin 57(12): A4199. [PubMed] [Google Scholar]
- Elo S., Kyngas H.(2008) The qualitative content analysis process. Journal of Advanced Nursing 62(1): 107–115. doi:10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Gardner K. O.(2015) Hip fractures: What information does the evidence show that patients and families need to decrease 30-day readmission? Orthopedic Nursing 34(6): 324–331. quiz 332-323. doi:10.1097/nor.0000000000000190. [DOI] [PubMed] [Google Scholar]
- Garne Holm K., Brodsgaard A., Zachariassen G., Smith A. C., Clemensen J.(2017) Participatory design methods for the development of a clinical telehealth service for neonatal homecare. SAGE Open Medicine 5: 2050312117731252.doi:10.1177/2050312117731252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gesar B., Baath C., Hedin H., Hommel A.(2017) Hip fracture; an interruption that has consequences four months later. A qualitative study. International Journal of Orthopaedic and Trauma Nursing 26: 43–48. doi:10.1016/j.ijotn.2017.04.002. [DOI] [PubMed] [Google Scholar]
- Gesar B., Hommel A., Hedin H., Baath C.(2017) Older patients’ perception of their own capacity to regain pre-fracture function after hip fracture surgery—An explorative qualitative study. International Journal of Orthopaedic and Trauma Nursing 24: 50–58. doi:10.1016/j.ijotn.2016.04.005. [DOI] [PubMed] [Google Scholar]
- Gorman E., Chudyk A. M., Hoppmann C. A., Hanson H. M., Guy P., Sims-Gould J., Ashe M. C.(2013) Exploring older adults’ patterns and perceptions of exercise after hip fracture. Physiotherapy Canada 65(1): 86–93. doi:10.3138/ptc.2012-01BH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey N. C., McCloskey E. V., Mitchell P. J., Dawson-Hughes B., Pierroz D. D., Reginster J. Y., Kanis J. A.(2017) Mind the (treatment) gap: A global perspective on current and future strategies for prevention of fragility fractures. Osteoporosis International 28(5): 1507–1529. doi:10.1007/s00198-016-3894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healee D. J., McCallin A., Jones M.(2011) Older adult’s recovery from hip fracture: A literature review. International Journal of Orthopaedic and Trauma Nursing 15(1): 18–28. doi:10.1016/j.ijotn.2010.06.010. [DOI] [PubMed] [Google Scholar]
- Healee D. J., McCallin A., Jones M.(2017) Restoring: How older adults manage their recovery from hip fracture. International Journal of Orthopaedic and Trauma Nursing 26: 30–35. doi:10.1016/j.ijotn.2017.03.001. [DOI] [PubMed] [Google Scholar]
- Husted H.(2012) Fast-track hip and knee arthroplasty: Clinical and organizational aspects. Acta Orthopedica Supplementum 83(346): 1–39. doi:10.3109/17453674.2012.700593. [DOI] [PubMed] [Google Scholar]
- Jensen C. M., Overgaard S., Wiil U. K., Smith A. C., Clemensen J.(2018) Bridging the gap: A user-driven study on new ways to support self-care and empowerment for patients with hip fracture. SAGE Open Medicine 6: 2050312118799121.doi:10.1177/2050312118799121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen C. M., Smith A. C., Overgaard S., Wiil U. K., Clemensen J.(2017) “If only had I known”: A qualitative study investigating a treatment of patients with a hip fracture with short time stay in hospital. International Journal of Qualitative Studies on Health and Well-being 12(1): 1307061.doi:10.1080/17482631.2017.1307061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanis J. A., Oden A., Johnell O., Jonsson B., de Laet C., Dawson A.(2001) The burden of osteoporotic fractures: A method for setting intervention thresholds. Osteoporosis International 12(5): 417–427. doi:10.1007/s001980170112. [DOI] [PubMed] [Google Scholar]
- Kehlet H., Dahl J. B.(2003) Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 362(9399): 1921–1928. doi:10.1016/s0140-6736(03)14966-5. [DOI] [PubMed] [Google Scholar]
- Knowles, M. S., Holton, E. F., & Swanson, R. A. (1973). The adult learner: The definitive classic in adult education and human resource development(pp. xiv, 387 s., illustreret). Retrieved from http://proxy1-bib.sdu.dk:2048/login?url=http://www.tandfebooks.com/isbn/9781315816951.
- Kvale S.(1996) InterViews: An introduction to qualitative research interviewing, Thousand Oaks, CA: SAGE. [Google Scholar]
- Lee P. A., Greenfield G., Pappas Y.(2018) Patients’ perception of using telehealth for type 2 diabetes management: A phenomenological study. BMC Health Services Research 18(1): 549.doi:10.1186/s12913-018-3353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride T. J., Panrucker S., Clothier J. C.(2011) Hip fractures: Public perceptions. Annals of the Royal College of Surgeons of England 93(1): 67–70. doi:10.1308/003588411X12851639107034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health. (2017). Healthcare in Denmark. Retrieved from http://www.sum.dk/English/Healthcare-in-Denmark-An-Overview.aspx.
- Orem D.(2001) Nursing: Concepts of practice, 6th ed Louis, MO: Mosby. [Google Scholar]
- Rasche P., Wille M., Brohl C., Theis S., Schafer K., Knobe M., Mertens A.(2018) Prevalence of health app use among older adults in Germany: National survey. JMIR Mhealth Uhealth 6(1): e26.doi:10.2196/mhealth.8619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller C., Franke T., Belle J., Sims-Gould J., Sale J., Ashe M. C.(2015) Words of wisdom–patient perspectives to guide recovery for older adults after hip fracture: A qualitative study. Patient Prefer Adherence 9: 57–64. doi:10.2147/PPA.S75657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims-Gould J., Stott-Eveneshen S., Fleig L., McAllister M., Ashe M. C.(2017) Patient perspectives on engagement in recovery after hip fracture: A qualitative study. Journal of Aging Research 2017: 2171865.doi:10.1155/2017/2171865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spradley J. P.(1979) The ethnographic interview, Belmont, CA: Wadsworth Cengage Learning. [Google Scholar]
- Spradley J. P.(1980) Participant observation, Belmont, CA: Wadsworth Cengage Learning. [Google Scholar]
- Tenforde A. S., Hefner J. E., Kodish-Wachs J. E., Iaccarino M. A., Paganoni S.(2017) Telehealth in physical medicine and rehabilitation: A narrative review. PM & R 9(5s): S51–s58. doi:10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1998). Health promotion glossary.Geneva, Switzerland: Division of Health Promotion, Education and Communication World Health Organization.
- World Health Organization. (2015). World report on ageing and health 2015. Retrieved from http://www.who.int/ageing/events/world-report-2015-launch/en/.
- Wiktorowicz M. E., Goeree R., Papaioannou A., Adachi J. D., Papadimitropoulos E.(2001) Economic implications of hip fracture: Health service use, institutional care and cost in Canada. Osteoporosis International 12(4): 271–278. doi:10.1007/s001980170116. [DOI] [PubMed] [Google Scholar]
- Zidén L., Scherman M. H., Wenestam C.-G.(2010) The break remains—Elderly people’s experiences of a hip fracture 1 year after discharge. Disability and Rehabilitation 32(2): 103–113. doi:10.3109/09638280903009263. [DOI] [PubMed] [Google Scholar]