Abstract
Background
Simulation is the most adopted teaching methodology in nursing education.
Objectives
This article investigated the outcome of repeated simulation experience on self-confidence, critical thinking, knowledge, competence, and satisfaction of nurses and nursing students.
Methods
The Scholarly literature published in English for the period of 2011 to 2019 was reviewed.
Results
Repeated simulation enhances students’ self-confidence, knowledge, competence, critical thinking, and satisfaction.
Conclusions
Repetitive simulation experience is valued by the nurse educators as a valuable teaching methodology to reinforce the student's learning outcomes.
Keywords: nursing faculty; nursing students; undergraduate nursing programs; nursing theory, nursing simulation
During the past 20 years, simulation has become an important part in nursing education, providing practical training on nursing care for nursing students (Aebersold & Tschannen, 2013). Beginning in the 1960s, simulation has been used for educating health professionals and has evolved over time due to the demand to provide high-quality care, increased complexity of patients, and need to minimize risks of care delivery for patients (Hall & Tori, 2017).
The National council of State Boards of Nursing defines clinical simulation as a computer-based event or activity imitating real clinical practice using medium fidelity manikins, high-fidelity manikins, clinical scenarios, standardized patients, skill stations, role playing, and critical thinking components (Kim et al., 2016). The International Nursing Association for Clinical Simulation and Learning Simulation defines simulation as a pedagogy using one or more typologies to improve, promote, and validate a participant’s progression from novice to expert. International Nursing Association for Clinical Simulation and Learning Simulation designated three parts of simulation as prebriefing, scenario, and debriefing (Meakim et al., 2013).
In clinical nursing education, the theoretical knowledge is integrated into practical knowledge in real-life situations and the students are taught to develop problem-solving skills. The opportunities to provide direct patient care and to handle problem-based clinical situations have diminished due to rapid changes in clinical placements, patient safety issues, and ethical concerns (Kim et al., 2016). As the opportunities are decreased for the nursing students to practice the clinical and decision-making skills, there are mounting concerns that graduate nurses are not competent in basic psychomotor skills. This requires the nurse educators to reevaluate the methods that they use to teach these skills. Simulation in clinical nursing education allows the nursing students to integrate the knowledge while practicing the skills (Ross, 2012). Nursing students get the opportunity to practice their clinical and decision-making skills through varied real-life situational experiences without compromising the patient’s safety through simulation-based clinical education (Kim et al., 2016).
Simulation-based clinical education is an experiential learning technique, which involves placing the learners in patient care situations created by instructors in order to maximize the learning in real situations that learners may encounter. This involves an active preparation by the educators where the degree of realistic situation ranges from completely artificial to an actual real-life like situation. This includes many delivery methods that involve actors trained as standardized patients who play out specific situation, and artificial modes, which include basic low-fidelity simulators (LFS), mid-fidelity simulators (MFS), and high-fidelity simulators (HFS). With LFS, mannequin parts that simulate patient situations such as wounds, fractures, and arms for intravenous calculations are used. The MFS allows simulations that use mannequins with some, but not all features of human beings (Hicks et al., 2009). High-fidelity simulation refers to a simulation activity that integrates the use of a full body manikin that can be programmed to deliver the response which is physiological in nature to the actions of students (Blakeslee, 2019).
The use of simulation in health care has various benefits. It is well documented that simulation improves the psychomotor skills, assessment skills, communication, and management skills (Nestel & Bearman, 2015; Yuan et al., 2012). The simulation scenarios are created according to the knowledge and experience level of the participants (Motola et al., 2013). The skills are rehearsed and practiced by the participants in simulation for a better application in the real clinical practice (Dieckmann, 2009; Westwood, 2014).
The practice of skills in the simulation laboratory provides a safe and effective environment for undergraduate students to acquire the clinical skills (Lynagh et al., 2007). This training improves the knowledge, skills, and behavior of students as compared with the direct clinical training. The training of the skills in the simulation laboratory enables the students to perform the skills faster and in an accurate manner (Lund et al., 2012).
The practice of skills deliberately in the simulation laboratory using LFS, MFS, and HFS results in an improvement of procedural skill acquisition of students. The practice of skills in the laboratory along with intermittent feedback results in better and smoother performance. Furthermore, the training of the students in the skills laboratory leads to higher scores in Objective Structured Clinical Examination (Bradley & Bligh, 1999; Herrmann-Werner et al., 2013; Junger et al., 2005).
Simulation-based nursing education increases the clinical competency of nursing students. However, the repetitive practice of skills through simulation results in long-term retention of both low- and high-complexity skills (Ericsson, 2007; Lammers, 2008). Repeated simulation experience also enhances the technical skills and critical thinking skills (Abe et al., 2013). Similar findings are reported by many authors across the world (Boling & Hardin-Pierce, 2016; Bowling & Underwood, 2016; Lubbers & Rossman, 2016; Cummings & Connelly, 2016; Kaddoura et al., 2016; Shin et al., 2015; Ko & Kim, 2014; Abe et al., 2013; Mould et al., 2011; Brewer, 2011; Guhde, 2011).This makes it very evident that repetitive simulation enhances the clinical competence of nursing students.
Having the evidence that repetitive simulation enhances the clinical competence of nurses and nursing students, the authors of this article reviewed the existing literature on the effect of repeated simulation experience on nurses and nursing students’ competence, self-confidence, knowledge, critical thinking, and satisfaction with learning. Delivery methods and type of fidelity are also included to add more relevance to the article. Findings could help nurses, nursing students, and nurse educators to be aware of the potential impact of simulation and may imply that simulation education is a best practice. Furthermore, conclusions could help educators to value or adopt simulation experiences as an effective teaching methodology in nursing education.
Methods
Integrative review of literature was done through a systematic process in an attempt to understand the effect of repeated simulation experience on nurses’ and nursing students’ competence, self-confidence, knowledge, critical thinking, and satisfaction with learning of nurses and nursing students. With the existing available qualitative and quantitative literature, an integrative review method was utilized. The CINAHL, Medline, and ProQuest data base were searched using combination of keywords such as nursing education, simulation experience, debriefing, effect, self-confidence, undergraduate nursing students, and nursing. The peer-reviewed literature published in English between January 1, 2011 and December 30, 2019 was used for the review to find the most updated literature.
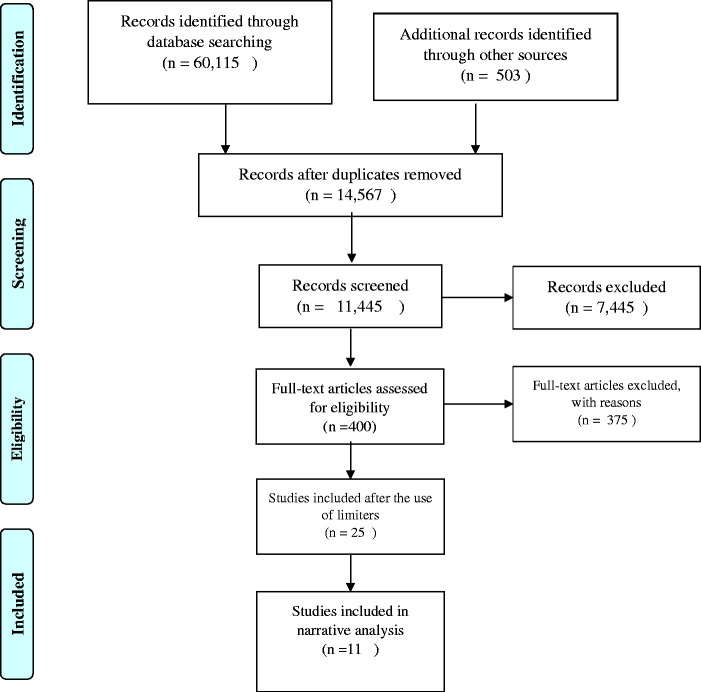
Initially, 60,618 results were obtained with the use of simulation experience and its related keywords. After this, the search was narrowed down to nursing (Figure 1). A total of 11,445 articles were retrieved. Thereafter 400 articles were obtained when the keywords were further limited to repeated simulation experience. Although single simulation experiences were studied in many articles, those were rejected to conserve the main focus of repeated simulation experience. These articles were hand searched and those with general information, commentary, speech/lecture, biography, and instructional material/guideline were excluded. The use of limiters such as timeframe from January 1, 2011 to December 30, 2019, English language, peer-reviewed journals, and nursing and ProQuest data base reduced the number to 25. All 25 articles were further analyzed based on the availability of keywords repeated simulation experience and nurses and nursing students’ competence, self-confidence, knowledge, critical thinking, and satisfaction with learning. This resulted in 11 articles for the analysis.
The rigor and bias were addressed as follows: the authors screened the titles and abstracts of each relevant article in the first step after the elimination of duplicates. In the second step, the authors independently evaluated each relevant full texted article for eligibility and disagreement was settled by consensus. The authors independently carried out data extraction. In the third step, the authors collected relevant data from the articles and consolidated it into an article review matrix.
The narrative analysis was done to interpret the text in this article as only limited literature was available to generate the evidence of effect of repetitive simulation on nurses and nursing students’ competence, self-confidence, knowledge, critical thinking, and satisfaction with learning.
Results
The detailed information of the articles analyzed through narrative analysis is appended in online Appendix A, Article Review Matrix. The outcome variables analyzed in this article included nurses and nursing students’ competence, self-confidence, knowledge, critical thinking, and satisfaction with learning. However, the authors have included the findings of two other variables which are delivery of simulation and type of fidelity. The authors felt that these variables would add more value to the article as these are more relevant to the simulation experience.
Delivery of Simulation
Across studies, there are variations in timing and design of simulations. In terms of the total time of simulation experience, a period of 7 to 9 weeks is sufficient to achieve desired outcomes for undergraduate nursing students (Bowling & Underwood, 2016; Cummings & Connelly, 2016; Kaddoura et al., 2016; Smith & Roehrs, 2009).In contrast, Abe et al. (2013) required 6 months to conduct simulation training for cardiovascular nurses in a hospital. These nurses participated in two to three case scenarios during the 6-month training. These data inform us that a minimum of 7 to 9 weeks of simulation experience is adequate to achieve the desired outcome among nursing students.
Type of Fidelity
Some studies were conducted to compare the effects of LFS versus HFS experiences. For instance, Bowling and Underwood (2016) examined the difference in the simulation outcome between MFS and LFS. They found that the knowledge, self-confidence, and skill performance outcomes improved following simulation, but there was no difference in the outcomes between the two types of simulation. In addition, Guhde (2011) found that all participants scored high means on critical thinking, assessment, and satisfaction with teaching following the simple and complex case scenario simulations (M = 4.74, SD = 0.50), and there were no significant differences between the simple and complex in improving the learner’s knowledge (p > .05). It appears that simulation, ranging from low to high fidelity, is considered a good strategy for enhancing student outcomes.
Competence, Self-Confidence, and Knowledge of Nurses and Nursing Students
Several studies examined the effect of repeated simulation scenarios on nursing students’ competence and self-confidence. For example, in a survey of 54 baccalaureate students, Cummings and Connelly (2016) found that the students reported that their mastery of skills and critical thinking improved after repeated simulation experience. Students reported that they experience active learning and active participation during simulation, which enhanced their competence.
In addition, in a classic experimental study by Mould et al. (2011), students were evaluated on perceived confidence and competence after repeated simulation scenarios. The tested intervention was a series of 27 case scenarios delivered over 9 weeks; each student experienced 17 to 18 simulations. The authors found a statically significant increase from baseline in perceived level of student confidence (63% increase) and perceived competence (48% increase).
Ko and Kim (2014) evaluated the effectiveness of multimode simulation learning on 65 junior nursing students’ problem-solving, critical thinking, and clinical competence. Authors found that multimode simulation learning improved the clinical competence and problem-solving process of nursing students. The problem-solving process in the experimental group who participated in multimode simulation increased by 0.32 points, whereas the scores of control group increased by 0.03 points which indicates a statistically significant difference between the groups (t = –2.39, p = .020). The clinical competence scores of experimental group increased by 0.29 points and the scores of control group decreased by 0.03. This shows a significant difference between both the groups (F = 12.76, p = .001). There was no significant effect on critical thinking disposition.
In a nonequivalent control group pretest–posttest study, Bowling and Underwood (2016) compared the effects of MFS and LFS simulation on self-confidence, knowledge, and skill performance in 77 baccalaureate students enrolled in pediatric nursing course. Skill performance was measured with a mini Objective Structured Clinical Examination; self-confidence was measured by a self-reported questionnaire and knowledge was measured by 15 items knowledge questionnaire. The MFS simulation experience lasted 30 minutes, followed by 20-minute group debriefing; the LFS was a paper and pencil case study. The LFS group scored higher on self-confidence (t = 2.213, df = 71, p = .03) than the MFS group. Both groups exhibited significantly increased postsimulation skill performance (p < .0001), with no difference between the LFS and HFS groups (p = .123).
Using a quasi-experimental pretest/posttest design, Lubbers and Rossman (2016) studied the effects of a pediatric community simulation experience on self-confidence among 54 senior baccalaureate students. The study took place in a private institution in the Midwestern, United States. The simulation experience was given once a week for approximately 3.5 hours each week for 7 weeks. The intervention involved approximately 1 hour spent in simulation and debriefing which was preceded by presimulation and followed with postsimulation exercises included within the Simulation Learning System. Self-confidence was measured using a survey developed for the study to measure self-confidence and the author included four subcategories as a part of the students’ self-confidence which included students’ knowledge, skill, communication, and documentation. The study showed significant increase in overall self-confidence (t = 20.70, p < .001).
Repeated simulation has also been evaluated among practicing registered nurses. Abe et al. (2013) evaluated repeated simulation scenarios during a 6-month training program for 27 cardiovascular critical care nurses working in a Tokyo hospital. The baseline scores after the first simulation showed low levels of self-reported self-confidence and competence. As the number of simulation scenarios increased, rubric scores of competence and confidence increased.
In a systematic review to examine the effect of HFS training among critical care providers, Boling and Hardin-Pierce (2016) did a meta-analysis for self-confidence and knowledge of critical care providers. Of the 17 studies included in the review, 13 examined the effect of simulation on provider self-confidence. In most articles, self-confidence was measured by self-rated survey. All studies showed that repeated simulation training improved self-confidence of nurses. It had been found that, confidence level was consistently higher in the experimental groups who participated in the simulation exercise. Seven studies focused on participant’s knowledge as an outcome. In all seven studies, participants rated their knowledge as greater following the simulation intervention. The researchers concluded that HFS is a valuable means for improving knowledge and confidence among critical care workers and advised inclusion of simulation in critical care training curricula.
Critical Thinking
The effect of simulation on Critical Thinking (CT) has also been studied. Shin et al. (2015) studied the effect of repeated simulation scenarios on 237 baccalaureate students’ CT level (N = 237). In this experimental study, a control group of students experienced one scenario, an experimental group of students had two different simulation sessions, and another experimental group had three different simulation sessions. Yoon’s Critical Thinking Disposition tool (2008) was used in this study to measure the CT of the students. The authors found that CT scores varied according to the number of exposures to simulation experiences. The results showed that students who had three simulations showed more CT gains in the subcategories of prudence and intellectual eagerness. The students who were exposed to two simulation scenarios also had improved scores in CT when compared with students who underwent one simulation.
To compare the effect of complex versus simple human patient simulation scenarios on CT and learner satisfaction, Guhde (2011) conducted a quasi-experimental, quantitative study among134 junior nursing students. Simulation scenarios were delivered over 6 weeks. During the first 4 weeks, a simple one-event scenario was implemented. On Week 5, the students were evaluated. On the last 2 weeks, students were doing a complex role-playing scenario. On Week 7, students’ responses showed a high mean CT scores (M = 4.69, SD = 0.53). The means were slightly, but not significantly, higher on the complex scenarios compared with the simple case scenario. The researchers concluded that HFS can heighten CT.
Student Satisfaction With Learning
Student’s learning satisfaction also were investigated by many researchers. For example, in a qualitative study, Kaddoura et al. (2016) interviewed nursing students (N = 107) to explore the perception of first-degree Bachelor of Science in Nursing (BSN) students about their perceived benefits and challenges of repeated exposure to HFS in the first medical-surgical nursing course.The exposure of students to seven different health scenarios were evaluated consecutively in a single experimental session. They found that most of participating students were satisfied with the knowledge; they gained post simulation confidence and perceived HFS as an active teaching pedagogy that contributes to their CT, clinical competence, self-confidence, and integration of knowledge by bridging the theory-practice gap.
Using a quasi-experimental design, Lubbers and Rossman (2016) also studied student satisfaction with learning. Student satisfaction with the learning experience was measured by a 1 to 5 point Likert-type scale with 5 indicating very satisfied. Students also reported a high level of satisfaction with their simulation experience (M = 4.36, SD = 0.50). Their finding is consistent with others (Abe et al. 2013; Kaddoura et al., 2016; Smith & Roehrs, 2009). For example, Smith and Roehrs (2009) reported that all nursing students were satisfied (M = 4.5; SD = 0.5) with the knowledge they gained because of simulation, concluding that students were satisfied with teaching pedagogy. The mean satisfaction with learning knowledge score for students with clinical experience was 4.5 (SD = 0.5) compared with 4.6 (SD = 0.4) for students without any clinical experience, that was found to be insignificant (p = .05).
Figure 1.
PRISMA Flow Diagram.
Discussion
In the evidence, participants were junior and senior undergraduate BSN students or staff nurses. The level of confidence, competence, CT, satisfaction with learning, and knowledge were measured before and after the simulation training. Sample sizes, which varied, involved either convenience or random sampling. The students were exposed to multiple different simulation experiences throughout semesters and were provided with experiential sessions and simulation debriefing sessions. Open-ended question surveys and Likert-type scales were used to evaluate self-confidence, competence, knowledge, learning satisfaction, and CT. The objective measurement tools reported were self-efficacy assessment tools (Boling & Hardin-Pierce, 2016), Simulation Learning System (Lubbers & Rossman, 2016), and Yoon’s Critical Thinking Scale (Shin et al., 2015). However, most of the outcomes were self-reported measures. This indicates the need to develop objective measurement tools to assess the competence, self-confidence, knowledge, CT, and satisfaction with learning.
None of the investigators measured the practice of the nurses and nursing students on their direct clinical practice after the exposure to repetitive clinical simulation. Therefore, future research is needed to determine the competence, critical thinking, and self-confidence of nurses and nursing students to indicate that simulation enhanced the skills and confidence level of the nurses for a better practice in the actual clinical setting. Investment in terms of simulation in nursing curriculum will improve the clinical practice of nurses; therefore, the quality of patient care will be improved.
Most of the evidence shows that simulation using different case scenarios each time over a semester of a course enhanced students’ self-confidence, competence, and CT. Moreover, students were satisfied with their learning and believed that the simulation experiences enhanced their knowledge. In addition, evidence showed that a range of simulation fidelity enhanced students’ self-confidence, competence, knowledge, and critical thinking. The use of LFS, MFS, and HFS with repeated simulation experiences is found to be the best teaching practices until now. Therefore, the authors highly recommend integrating the use of LFS, MFS, and HFS with repeated simulation experiences in nursing curriculum to enhance the nursing students’ self-confidence, competence, knowledge, and critical thinking. Also, the nurse’s competence will definitely be improved with the use of repeated simulation experiences.
Limitations
The authors have reviewed and summarized the literature pertaining to both nurses and nursing students although the knowledge, skills, attitudes, and behaviors vastly differ across these groups as very limited literature is available. However, the authors intended to convey that repeated simulation enhances both the nursing students and nurses’ self-confidence, competence, knowledge, and critical thinking. Despite the abundance of literature available about simulation in undergraduate nursing students, researchers have yet to study the effect of repeating the similar simulation experience after debriefing with facilitators. This aspect merits investigation because there are two possible outcomes from practicing the same experience after debriefing with instructors. First, students may be more confident because they will be able to correct their mistakes done during the first simulation experience while improving their skills. A second possible outcome is that immediate repetition of the same simulation experience will be a waste of time because students could benefit more from practicing in different experience.
Priorities for Future Research
Therefore, the authors would recommend a study to evaluate the effect of repeating same simulation practice post debriefing on students’ learning outcomes. Future research could be directed toward determining the competence, critical thinking, knowledge, and self-confidence of nursing students and nurses in the real clinical setting after exposure to repetitive simulation experience. Moreover, future studies are required to develop objective tools to measure the competence, critical thinking, knowledge, and self-confidence of nursing students and nurses.
Highlights
The review concluded that simulation enhances nursing students’ and nurse’s self-confidence, competence, knowledge, critical thinking, and satisfaction.
Repetitive simulation experience shall be valued and adopted as an effective teaching methodology in nursing education by the nurse educators.
Repetitive simulation enhances the nurse’s competence and knowledge while providing nursing care.
Supplemental Material
Supplemental material, sj-pdf-1-son-10.1177_2377960820927377 for Repeated Simulation Experience on Self-Confidence, Critical Thinking, and Competence of Nurses and Nursing Students—An Integrative Review by Koukab Abdullah Al Gharibi, MSN and Judie Arulappan, MSc(N), PhD, DNSc in SAGE Open Nursing
Author contributions
Koukab Abdullah Al Gharibi conceived, designed, and performed the study. He also analyzed and interpreted the data and wrote the initial draft of the article. Judie Arulappan reviewed, edited, and finalized the article.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Koukab Abdullah Al Gharibi https://orcid.org/0000-0003-2773-8067
Judie Arulappan https://orcid.org/0000-0003-2788-2755
Supplemental Material
Supplemental material for this article is available online.
References
- Abe Y., Kawahara C., Yamashina A., Tsuboi R. (2013). Repeated scenario simulation to improve competency in critical care: A new approach for nursing education. American Journal of Critical Care, 22 (1), 33–40. 10.4037/ajcc2013229 [DOI] [PubMed] [Google Scholar]
- Aebersold M., Tschannen D. (2013). Simulation in nursing practice: The impact on patient care. The Online Journal of Issues in Nursing, 18(2), 6 10.3912/OJIN.Vol18No02Man06 [DOI] [PubMed] [Google Scholar]
- Blakeslee J. R. (2019). Effects of high-fidelity simulation on the critical thinking skills of Baccalaureate nursing students. Walden University. [DOI] [PubMed]
- Boling B., Hardin-Pierce M. (2016). The effect of high-fidelity simulation on knowledge and confidence in critical care training: An integrative review. Nurse Education in Practice, 16(1), 287–293. 10.1016/j.nepr.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Bowling A., Underwood P. (2016). Effect of simulation on knowledge, self-confidence, and skill performance in the USA: A quasi-experimental study. Nursing & Health Sciences, 18(3), 292–298. 10.1111/nhs.12267 [DOI] [PubMed] [Google Scholar]
- Bradley P., Bligh J. (1999). One year’s experience with a clinical skill resource centre. Medical Education, 33(2), 114–120. [DOI] [PubMed] [Google Scholar]
- Brewer E. P. (2011). Successful techniques for using human patient simulation in nursing education. Journal of Nursing Scholarship, 43(3), 311–317. 10.1111/j.1547-5069.2011.01405.x [DOI] [PubMed] [Google Scholar]
- Cummings, C. L., & Connelly, L. K. (2016). Can nursing students' confidence levels increase with repeated simulation activities?. Nurse education today, 36, 419--421. [DOI] [PubMed]
- Dieckmann P. (2009). Using simulations for education, training and research. Pabst Science Publ.
- Ericsson K. A. (2007). An expert‐performance perspective of research on medical expertise: The study of clinical performance. Medical Education, 41(12), 1124–1130. [DOI] [PubMed] [Google Scholar]
- Guhde J. (2011). Nursing students’ perceptions of the effect on critical thinking, assessment, and learner satisfaction in simple versus complex high-fidelity simulation scenarios. Journal of Nursing Education, 50(2), 73–78. 10.3928/01484834-20101130-03 [DOI] [PubMed] [Google Scholar]
- Hall K., Tori K. (2017). Best practice recommendations for debriefing in simulation based education for Australian undergraduate nursing students: An integrative review. Clinical Simulation in Nursing, 13(1), 39–50. 10.1016/j.ecns.2016.10.006 [DOI] [Google Scholar]
- Herrmann-Werner A., Nikendei C., Keifenheim K., Bosse H. M., Lund F., Wagner R., Celebi, N., Zipfel, S., & Weyrich P. (2013). “Best practice” skills lab training vs. a “see one, do one” approach in undergraduate medical education: An RCT on students’ long-term ability to perform procedural clinical skills. PLoS One, 8(9), e76354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks F., Coke L., Li S. (2009). The effect of high-fidelity simulation on nursing students’ knowledge and performance National Council of State Boards of Nursing. https://www.ncsbn.org/09_SimulationStudy_Vol40_web_with_cover.pdf
- Junger J., Schäfer S., Roth C., Schellberg D., Friedman Ben-David M., Nikendei C. (2005). Effects of basic clinical skills training on objective structured clinical examination performance. Medical Education, 39(10), 1015–1020. [DOI] [PubMed] [Google Scholar]
- Kaddoura, M., Vandyke, O., Smallwood, C., & Gonzalez, K. M. (2016). Perceived benefits and challenges of repeated exposure to high fidelity simulation experiences of first degree accelerated bachelor nursing students. Nurse education today, 36, 298--303. [DOI] [PubMed] [Google Scholar]
- Kim J., Park J. H., Shin S. (2016). Effectiveness of simulation-based nursing education depending on fidelity: A meta-analysis. BMC Medical Education, 16, 152 10.1186/s12909-016-0672-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko E., Kim H. Y. (2014). Effects of multi-mode simulation learning on nursing students’ critical thinking disposition, problem solving process, and clinical competence. Korean Journal of Adult Nursing, 26(1), 107–116. [Google Scholar]
- Lammers R. L. (2008). Learning and retention rates after training in posterior epistaxis management. Academic Emergency Medicine, 15(11), 1181–1189. [DOI] [PubMed] [Google Scholar]
- Lubbers J., Rossman C. (2016). The effects of pediatric community simulation experience on the self-confidence and satisfaction of baccalaureate nursing students: A quasi-experimental study. Nurse Education Today, 39, 93–98. 10.1016/j.nedt.2016.0 [DOI] [PubMed] [Google Scholar]
- Lund F., Schultz J. H., Maatouk I., Krautter M., Möltner A., Werner A., Weyrich P., Jünger J., Nikendei C. (2012). Effectiveness of IV cannulation skills laboratory training and its transfer into clinical practice: A randomized, controlled trial. PLoS One, 7(3), e32831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynagh M., Burton R., Sanson-Fisher R. (2007). A systematic review of medical skills laboratory training: where to from here? Medical Education, 41(9), 879–887. [DOI] [PubMed] [Google Scholar]
- Meakim C., Boese T., Decker S., Franklin A. E., Gloe D., Lioce L., Sando C. R., Borum J. C. (2013). Standards of best practice: Simulation standard I: Terminology. Clinical Simulation in Nursing, 9(6), S3–S11. [Google Scholar]
- Motola I., Devine L. A., Chung H. S., Sullivan J. E., Issenberg S. B. (2013). Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Medical Teacher, 35(10), e1511–e1530. [DOI] [PubMed] [Google Scholar]
- Mould J., White H., Gallagher R. (2011). Evaluation of a critical care simulation series for undergraduate nursing students. A Journal for the Australian Nursing Profession, 38(12), 180–190. 10.5172/conu.2011.38.1-2.180 [DOI] [PubMed] [Google Scholar]
- Nestel D., Bearman M. (2015). Theory and simulation-based education: Definitions, worldviews and applications. Clinical Simulation in Nursing, 11(8), 349–354. [Google Scholar]
- Ross J. G. (2012). Simulation and psychomotor skill acquisition: A review of the literature. Clinical Simulation in Nursing, 8(9), e429–e435. [Google Scholar]
- Shin H., Ma H., Park J., Ji E. S., Kim D. H. (2015). The effect of simulation courseware on critical thinking in undergraduate nursing students: Multi-site pre-post study. Nursing Education Today, 35(4), 537–542. [DOI] [PubMed] [Google Scholar]
- Smith S., Roehrs C. (2009). High-fidelity simulation: Factors correlated with nursing student satisfaction and self-confidence. Nursing Education Perspectives, 30(2), 74–78. [PubMed] [Google Scholar]
- Westwood J. D. (2014). Simulation fidelity: More than experience and mere repetition? Medicine Meets Virtual Reality 21: NextMed/MMVR21, 196, 128. [PubMed]
- Yuan H. B., Williams B. A., Fang J. B. (2012). The contribution of high‐fidelity simulation to nursing students’ confidence and competence: A systematic review. International Nursing Review, 59(1), 26–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-son-10.1177_2377960820927377 for Repeated Simulation Experience on Self-Confidence, Critical Thinking, and Competence of Nurses and Nursing Students—An Integrative Review by Koukab Abdullah Al Gharibi, MSN and Judie Arulappan, MSc(N), PhD, DNSc in SAGE Open Nursing