Abstract
In recent years, virtual reality (VR) has become an interesting alternative to traditional exposure-based therapies for many symptoms. VR involves immersion in a computer-generated virtual environment that minimizes avoidance and facilitates emotional processing. The objective of this systematic review is to evaluate evidence on the intervention effect of VR on anxiety, depression, fatigue, and pain. The research strategy of this systematic review included three electronic databases (MEDLINE/PubMed, Cochrane Library, and ScienceDirect) based on predetermined inclusion and exclusion criteria. Published quantitative studies from 2000 to 2020 were identified, which examined the effect of VR intervention on four different symptoms related to symptoms experienced by cancer patients. Quality assessments, data extractions, and analysis were completed on all included studies. A total of 882 titles and abstracts were screened, and 23 studies were included in the review. The studies were grouped according to the symptoms: anxiety and depression, fatigue, and pain. The review showed that VR intervention is more effective compared with the control (i.e., standard care) for anxiety, depression, fatigue, and pain. VR can reduce effectively these symptoms in different contexts and diseases, including cancer. The evidence suggests that there is value in exploring this intervention as a potential crossover treatment for these symptoms in patients. This study contributes to evidence that distraction is an effective symptom management mechanism. The findings are congruent with the theoretical framework, supporting the premise that VR, as an emotion-focused distraction intervention, decreases the severity of these symptoms.
Keywords: virtual reality, anxiety, depression, fatigue, pain
What Is Already Known About the Topic?
Nurses use a variety of different strategies to accommodate management of physical and psychological symptoms in patients.
Symptoms such as anxiety, depression, pain, and fatigue represent four of the most commonly reported symptoms in individuals across many diseases.
Clinical studies provided evidence that virtual reality (VR) is a promising tool for clinical assessment and management of many symptoms.
What This Article Adds?
VR is more effective compared with the control (i.e., standard care) for anxiety, depression, fatigue, and pain.
Using VR decreases significantly the levels of anxiety, depression, fatigue, and pain.
The review provided evidence on the feasibility for using VR in various inpatient medical settings.
Introduction
For many years, nurses have used a variety of different strategies to accommodate management of physical and psychological symptoms in patients. To address all the needs of the patient, clinicians must consider not only the biological impact of illness but also the psychosocial one (Humphreys et al., 2014).
It was as early as the 90s that VR has had promising applications in science and medicine, including intervention delivery (Medling, 2005; Riener & Harders, 2012; Riva et al., 2007). In more recent years, VR technology has become increasingly affordable, immersive, flexible, and portable, enabling its use in a broader range of environments, including the inpatient medical setting (Ferrer-García & Gutiérrez-Maldonado, 2012; Parsons et al., 2009).
VR is one of the strategies that have been identified as cognitive-behavioral intervention. These interventions are thought to affect symptoms by changing symptom-related thoughts, diminishing those beliefs that exacerbate symptoms, and increasing personal perceptions of control over symptoms (Anderson et al., 2006; Kwekkeboom et al., 2003, 2010; Malloy & Milling, 2010).Use of VR interventions has been studied in a wide range of medical conditions, including anxiety, depression, pain, and fatigue that represent four of the most common symptoms present in individuals in many diseases (Chirico et al., 2016; Indovina et al., 2018; Llobera et al., 2013; McCann et al., 2014; Wiederhold, 2006).
To date, there is scarcity of systematic reviews on the use of VR in the inpatient medical setting and related to symptom management. Herein, we review controlled studies evaluating the utility and efficacy of VR-based treatments for patients suffering from these four symptoms. The overall objective of study selection was to collect published peer-reviewed articles that evaluated anxiety and depression, fatigue, and pain symptoms before and after VR exposure therapy.
Virtual Reality
The term VR was used for the first time in 1989 by Jaron Lamier. The most popular definition of VR refers to a particular technological system, which includes a computer capable of providing interactive three-dimensional visualization, a controller for interaction with the animations, a position tracker, and a head-mounted display (HMD) to deliver the visual output. The trackers monitor the position and orientation of the user in space and provide the information to the computer that updates in real time the images for display (Biocca, 1992; Wiederhold & Wiederhold, 2007). VR is immersive and interactive, engaging several senses simultaneously. This technology allows an individual to hear and feel stimuli that correspond with a visual image and can interact with the virtual environment and the virtual world’s response in real time to those actions (Liszio et al., 2018; Yu et al., 2018).
Methods
Study Selection: Search Strategy, Data Sources, and Screening
A systematical literature search was conducted in the following databases: MEDLINE/PubMed, Cochrane Library, and ScienceDirect. The aim was to retrieve experimental studies of VR in inpatient medical settings and symptoms management of the four symptoms. Standard searches were performed, with keywords containing affective domains, as well as references to virtual reality exposure therapy (VRET) and the field of interest. Keywords used for the search included “Virtual Reality,” “Anxiety,” “Depression,” “Fatigue,” “Pain,” and “Symptoms Management” to identify studies published between 2000 and 2020.
Study Eligibility Criteria
Inclusion/Exclusion Criteria
All studies selected for inclusion were English-language publications, which reported original empirical findings and were published in a peer-reviewed journal, between 2000 and 2020. Studies were required to have used an experimental design and focused on the efficiency or effectiveness or process of VRET on the four symptoms. The researchers excluded trials with no control or comparison group, case studies, outpatient studies, theses, or dissertations. The samples of the studies were human participants from all ages having one or more of the symptoms that were the focus of this review.
Screening
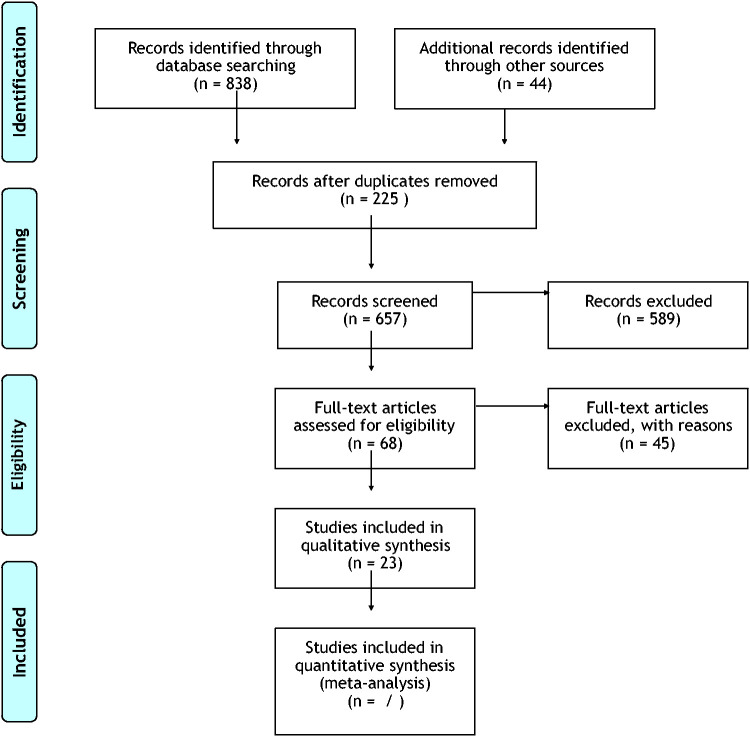
As displayed in Figure 1 (PRISMA flow diagram), the initial first search yielded 882 citations of journal articles written over the past 20 years.Two-hundred and twenty-five citations were discarded after identifying they were duplicates, and 657 more were discarded after reviewing the abstract. The researchers reviewed the remaining 68 in more detail and excluded 45 because they did not meet all the inclusion criteria, the full text was not available, or they were duplicates. The final eligible for the review 23 studies were grouped based on the application of VR on the four symptoms: (a) anxiety, (b) depression, (c) fatigue, and (d) pain. These studies are described in detail in Table 1.
Figure 1.
PRISMA 2009 Flow Diagram.
Table 1.
Studies Characteristics.
| Study | Symptom | Type of study | Study population | N | Intervention | Tools | Main results |
|---|---|---|---|---|---|---|---|
| Dehghan et al. (2019) | Anxiety | Solomon four-group randomized clinical trial | Children undergoing abdominal surgery | 40 (6–12 years) | VR immersive and audio 5-minute exposure to the operating room | Yale Preoperative Anxiety Scale questionnaire (four domains including activity, vocalization, emotional expressivity, and state of apparent arousal) | The comparison of pre- and postscores in the interventional groups by Wilcoxon test indicated a significant statistical difference in all domains except for arousals domain. Comparison of pre- and postscores among control groups showed a significant statistical difference in all domains except for emotional expressivity. |
| Ryu et al. (2018) | Anxiety | Prospective RCT | Children undergoing elective day surgery and general anesthesia | 70 (5–8 years) | - VR gaming – a 5-minute VR game experiencing the preoperative experience - Conventional education regarding the preoperative process | - m-YPAS-Preoperative anxiety, ICC- Procedural behavior rating scale | Preoperative anxiety (28.3 [23.3–36.7] vs. 46.7 [31.7–51.7]; p < .001) and intraoperative compliance measured using ICC (p = .038) were lower in the gamification group than in the control group. The changes of m-YPAS scores before and after the intervention were also significantly different between the two groups (–22.5 [–29.6–14.2] vs. 0 [–20–4.2]; p = .002). |
| Shah et al. (2015) | Anxiety, depression | Quasi-experimental research (a single-group, pretest–posttest) | Inpatients diagnosed with major depressive disorder and bipolar disorder | 22 (21–60 years) | VR DE-STRESS Program: The program comprised three daily 1-hour sessions incorporating psychoeducation and VR-based relaxation practice. | DASS-21 | 3-day program intervention the participants had significantly lowered subjective stress (X difference = 7.62, SD = 5.17, t = 6.91, p < .001), depression (X difference = 8.09, SD = 6.75, t = 5.62, p < .001), and anxiety (X difference = 5.64, SD = 4.77, t = 5.54, p < .001). |
| Lee et al. (2015) | Depression | RCT | Parkinson’s disease patients | 20 (65–75 years) | - Virtual reality dance exercises – control group | BDI | The depressive disorder status significantly improved in the experimental group (20.4 ± 0.9 to 18.2 ± 2.0; p < .05), while the depressive disorder status of the control group showed no significant improvement (21.2 ± 1.3 to 20.6 ± 1.5; p>.05). Compared with the control group, the depressive disorder status of the experimental group was significantly improved (p < .05). |
| Kampmann et al. (2016) | Anxiety (social) | RCT | Patients diagnosed with social anxiety disorder | 60 (18–65 years) | - VRET (immersive)- iVET – waiting list | SIASDASS-21 | A significant decrease of social anxiety from pre- to post assessment for both VRET (p = .014; d = 0.55) and iVET (p < .001; d = 1.14) compared with the waiting-list control group. A significant decrease on the anxiety subscale (p = .043; d = 0.47) was observed for iVET compared with the waiting-list control group. No significant differences were found between VRET and waiting list on the anxiety subscale (p = .135) and depression subscale (p = .401) or between iVET and waiting list on the depression subscale. Participants receiving iVET, but not VRET, improved on fear of negative evaluation, speech performance, general anxiety, depression, and quality of life relative to waiting list. |
| Song and Park (2015) | Depression | RCT | Stroke patients | 40 (40–60 years) | - VR group – ergometer training group | BDI | Both the VRG and ETG patients showed significant improvements in BDI scores after the intervention (p < .05). The comparison of the postintervention improvements of the two groups revealed that the VRG showed a more significant increase in BDI than the ETG. |
| Krijn et al. (2004) | Anxiety (acrophobia) | Prospective RCT | Patients diagnosed with acrophobia | 37 (22) (40–60 years) | - VRET with an HMD (immersive) - VRET – a computer automatic virtual environment- No intervention | Acrophobia Questionnaire (Anxiety in height situations) | VRET was more effective than no treatment on patient with acrophobia. Univariate analysis showed that there was not a significant time-effect: AQ-Anxiety: F(1, 20) = 0.346; p = .563, but there was significant interaction effect between time and condition, F(4, 23) = 7,304; p = .012, to anxiety related to height. They also experienced less presence and anxiety in the virtual environment used in Session 1 when compared with patients who completed VRET. |
| Riva et al. (2003) | Anxiety, depression | RCT | Patients with eating disorders | 36 (women, 18–50 years) | ECT: 15 sessions of Virtual Reality for Eating Disorders Modification—(immersive virtual environment), 14 virtual environments used by the therapist during a 50-minute sessionCBT: 15 sessions of group sessions aimed at improving assertiveness and motivation to change and 10 biweekly individual sessions whose target behaviors for change were eating behavior (dietary restraint and binge eating) as well as self-esteem and related problems. | STAI (Italian version)BDI II | State Anxiety (STAI X2) significantly decreased in both ECT (mean score before treatment, 49.44; after, 36.77; p = .018) and nutritional groups conditions (before: 49.77; after: 38.77; p = .013), while no significant changes were evidenced in CBT and in the waiting-list conditions. Depression levels (BDI) significantly decreased in both ECT (before: 22.23; after: 8.11; p = .008) and CBT (before: 20.55; after: 12.11; p = .050); however, complete remission of depressive symptoms was observed only in the ECT group. |
| Schneider et al. (2003) | Anxiety, fatigue | RCT – crossover design | Breast cancer women | 16 (50–77 years) | - Virtual reality distraction (immersive) | Revised PFSSAI | There was a significant difference in the SAI for Adults (p = .10, 15 df) scores immediately following the chemotherapy treatment when subjects used the VR intervention. There were no significant changes in any of the measures of symptom fatigue, or anxiety 2 days later. There was a trend toward lower scores with the VR condition. |
| Schneider et al. (2004) | Anxiety, fatigue | RCT – crossover design | Breast cancer women | 20 (27–55 years) | VR as a distraction intervention during one session of chemotherapy (immersive) | The SAI for Adults The Revised PFS | Mean state anxiety scores were lower following the use of the virtual reality, but no significant differences were found (p = .230). Highest level of fatigue occurring 2 days after chemotherapy treatments and the lowest level of fatigue (X score = 1.85) immediately following chemotherapy treatment when the participants used the VR. No significant changes in any of the measures of fatigue, or anxiety 2 days later, but a trend toward lower scores existed with the VR condition. |
| Schneider & Hood (2007) | Anxiety, fatigue | RCT – crossover design | Breast, colon, or lung cancer patients | 123 (32–78 years) | VR headset during an IV chemotherapy treatment (immersive) | -Revised PFS-SAI | Significant (p < .01) Pearson correlations were found between Presence Questionnaire and Revised PFS (−0.296) and SAI for Adults (−0.308), suggesting that higher levels of interaction with VR were related to lower levels of symptom distress. Individuals who received the VR during their first chemotherapy treatment had significantly less anxiety, compared with the control condition during the second chemotherapy treatment. |
| Cho & Sohng (2014) | Fatigue | Nonequivalent control group pretest–posttest design | Hemodialysis patients with end-stage renal failure | 46 (45–70 years) | - Virtual reality exercise program (nonimmersive) | Visual Analogue Scale for Fatigue (0–10) | The level of fatigue in the exercise group showed a dramatic decrease, from 6.7 points to 4.9 points (p> .001), while almost no changes were noted in the control group. |
| Gerçeker et al (2018) | Pain | Prospective RCT | Children during phlebotomy | 121 (7–12 years) | Group 1: VR (cartoon videos)Group 2: external cold and vibrationGroup 3: control | - Wong–Baker FACES scale (0–10) | Pain scores were determined to be lower in Groups 1 and 2. Although there was no difference between the Groups 1 and 2, a statistically significant difference was found between Groups 1 or 2 and Group 3 based on all pain scores. |
| JahaniShoorab et al. (2015) | Pain | RCT | Primiparous parturient women having labor for episiotomy repair | 32 (18–43 years) | - VR (video glasses and local infiltration; 5 ml solution of lidocaine 2%)- Local infiltration (5 ml solution of lidocaine 2%) control group | Numeric Pain Rating Scale (0–100 scale) | There were statistically significant differences between the pain score during episiotomy repair in both groups (p = .038). |
| Aminabadi et al. (2012) | Pain, anxiety | Single-blind crossover clinical trial study | Children during dental procedures | 120 (4–6 years) | -VR (cartoon video) immersive -No VR | Wong–Baker FACES Pain Rating ScaleFaces version of the Modified Child Dental Anxiety Scale Screen for Child Anxiety Related Disorders questionnaire | There was a significant decrease in pain perception (p < .001) and state anxiety scores (p < .001) with the use of virtual reality eyeglasses during dental treatment. |
| Schmitt et al. (2011) | Pain | RCT – within-subjects (crossover design) | Hospitalized pediatric burn inpatients undergoing painful physical therapy | 54 (6–19 years) | Virtual reality exposure (immersive) SnowWorld game for 5 days | GRS assessing separate components of pain (cognitive, affective, sensory) | On Study Day 1, subjects reported significant decreases (27%–44%) in pain ratings during virtual reality. GRS assessments on Study Day 1 of cognitive pain (44% reduction), affective pain (32% reduction), and sensory pain (27% reduction) were significantly lower (p < .05 for each paired comparison) in the adjunctive virtual reality condition than in the control condition. The analgesia and affect improvements were maintained with repeated virtual reality use over multiple therapy sessions. |
| Maani et al. (2011) | Pain | Within-subject experimental design | U.S. soldiers burned in combat attacks involving explosive devices in Iraq or Afghanistan | 12 (20–29 years) | - Immersive VR SnowWorld- No VR intervention | Questions and rating scales(0–10) | Patients reported significantly less pain when distracted with VR. Worst pain (pain intensity) dropped from 6.25 of 10 to 4.50 of 10. Pain unpleasantness ratings dropped from moderate (6.25 of 10) to mild (2.83 of 10). “Time spent thinking about pain” dropped from 76% during no VR to 22% during VR. |
| Kipping et al (2012) | Pain | Prospective RCT with a parallel group design | Adolescents undergoing burn wound care and nursing staff | 41 (11–17 years) | -VR immersive- Distraction (TV, stories, music, caregivers) or no distraction | VAS | For adolescent self-report of pain, mean pain scores were higher for the SDG compared with the VRG in both dressing removal and application; however, these differences were not statistically significant. Nursing staff reported a statistically significant reduction in pain scores during dressing removal and significantly less rescue doses of Entonox given to those receiving VR, compared with those receiving standard distraction. For all other pain outcomes and length of treatment, there was a trend for lower pain scores and treatment times for those receiving VR, but these differences were not statistically significant. |
| Carrougher et al.(2009) | Pain | RCT – crossover design | Inpatient with a mean total burn surface area burn of 18% | 39 (21–57 years) | Virtual reality exposure (immersive) | GRS (0–100) | Observed reductions in all GRS in pain unpleasantness (31%), time spent thinking about pain (37%), and worst pain experienced (27%) in VR conditions. |
| van Twillert et al. (2007) | Pain, anxiety | Experimental within-subject design | Burn patients | 19 (8–65 years) | -Immersive VR SnowWorld game -Distraction television, music, nonmedical conversation, and distraction by a childcare worker | Pain: visual analog thermometer, Anxiety: STAI (Dutch edition) | Thirteen of 19 patients reported clinically meaningful (33% or greater) reductions in pain during VR distraction. No side effects were reported. No correlations were found between the reduction in pain ratings and patient variables such as age, sex, duration of hospital stay, or percentage of (deep) burns. There was no significant reduction of anxiety ratings. |
| Gold et al. (2006) | Pain, anxiety | RCT | Children, their parents, and nurses during MRI or CT and IV placement | 20 (8–12 years) | -VR distraction using Street Luge Immersive- Standard of care (topical anesthetic) with no distraction | Wong–Baker FACES Pain Rating ScaleFaces Pain Scale–Revised | Responses from the Faces Pain Scale–Revised indicated a fourfold increase in affective pain within the control condition; by contrast, no significant differences were detected within the VR condition. Significant associations between multiple measures of anticipatory anxiety, affective pain, IV pain intensity, and measures of past procedural pain provided support for the complex interplay of a multimodal assessment of pain perception. |
| Das et al. (2005) | Pain | RCT – crossover design | Children undergoing burn dressing changes | 9 (5–18 years) | Virtual reality game (immersive) | Faces Pain Scale | The average pain scores (from the Faces Scale) for pharmacological analgesia only was 4.1 (SD = 2.9), while VR coupled with pharmacological analgesia, the average pain score was 1.3 (SD = 1.8) |
| Wint et al. (2002) | Pain | RCT | Adolescents with cancer undergoing LPs | 30 (10–19 years) | - VR glasses and watched a video | VAS (0–100) | Although VAS pain scores were not statistically different between the two groups (p = .77), VAS scores tended to be lower in the VR group (median VAS of 7.0, range 0–48) than in the control group (median VAS of 9.0, range: 0–59). Seventy-seven percent of subjects in the experimental group said the VR glasses helped to distract them from the LP. |
Note. VR = virtual reality; RCT = randomized control trial; m-YPAS = Modified Yale Preoperative Anxiety Scale; ICC = induction compliance checklist; DASS = Depression Anxiety Stress Scale; BDI = Beck Depression Inventory; VRET = virtual reality exposure therapy; iVET = in vivo exposure therapy; SIAS = Social Interaction Anxiety Scale; HMD = head-mounted display; STAI = State-Trait Anxiety Inventory; PFS = Piper Fatigue Scale; SAI = State Anxiety Inventory; GRS = graphic rating scale; VAS = Virtual Analog Score; MRI = magnetic resonance imaging; CT = computerized tomography; IV = intravenous; LP = lumbar puncture; CBT = Cognitive Behavioral Therapy; AQ = Acrophobia Questionnaire; VRG = Virtual Reality Group; SDG = Standard Distraction Group; ETG = Ergometer Training Group.
Data Extraction
The following data were extracted from the included studies: author, journal, country, research purpose and questions, theoretical framework, design, setting, subjects, sampling method, measurements instruments, reliability and validity, analysis, symptoms measures (anxiety, depression, fatigue, pain), outcomes of VR, and significant and nonsignificant results.
Quality Review
Each published article was reviewed for methodological quality by the research team members using the Cochrane Collaboration’s tool (Table 2). The selected tool was used to assess risk of bias for randomized control trials. Although the methodological quality of the reviewed studies has been undertaken as part of this review, it was not considered as an eligibility criterion for inclusion in the review.
Table 2.
Quality Assessment of Selected Researches.
| Study | Selection bias Random sequence generation | Selection bias Allocation concealment | Performance bias Blinding of participants and personnela | Detection bias Blinding of outcome assessmenta | Attrition bias Incomplete outcome dataa | Reporting bias Selective reporting | Other bias Anything else, ideally prespecified |
|---|---|---|---|---|---|---|---|
| Dehghan et al. (2019) | – | + | ? | ? | + | + | + |
| Ryu et al. (2018) | + | + | + | + | + | + | + |
| Shah et al. (2015) | + | + | – (informed about the study aim) | – (informed about the study aim) | + | + | + |
| Lee et al. (2015) | + | – | + | ? | + | + | – |
| Kampmann et al. (2016) | + | + | + | + | + | + | + |
| Song and Park (2015) | – | + | – (informed about the study aim) | – (informed about the study aim) | + | ? | – |
| Krijn et al. (2004) | – | ? | ? | ? | – | + | – |
| Riva et al. (2003) | + | + | + – | + | ? | + | – |
| Schneider et al. (2003) | + | + | – (informed about the study aim) | – (informed about the study aim) | + | + | + |
| Schneider et al. (2004) | + | + | – (informed about the study aim) | – (informed about the study aim) | + | + | + |
| Schneider & Hood (2007) | + | + | ? | – (informed about the study aim) | – | – | – |
| Cho & Sohng (2014) | – | – | + | – | + | + | + |
| Gerçeker et al (2018) | + | + | + | + | + | + | – |
| JahaniShoorab et al. (2015) | – | + | – ? (informed about VR) | + | + | + | – |
| Aminabadi et al. (2012) | + | + | – | + | + | + | – |
| Schmitt et al. (2011) | + | ? | + | + | – | + | – |
| Maani et al. (2011) | – | + | – | – | + | + | – |
| Kipping et al (2012) | + | + | – | – | + | + | – |
| Carrougher et al.(2009) | + | + | – | – | + | + | + |
| van Twillert et al. (2007) | + | + | – | – | – | + | – |
| Gold et al. (2006) | + | + | + | + | + | + | – |
| Das et al. (2005) | + | + | – (informed about the study aim) | – (informed about the study aim) | + | + | – |
| Wint et al. (2002) | + | + | + | + | + | + | – |
Note. VR = virtual reality.
aAssessments should be made for each main outcome or class of outcomes.
+ indicates low risk of bias; – indicates high risk of bias; ? indicates unclear risk of bias.
Results
Search Outcome
The search yielded 23 original studies that were included in the systematic review according to the predetermined inclusion criteria. Studies randomized patients to VR conditions, or randomized order of delivery of VR or standard interventions, using crossover designs. We observed that studies were heterogeneous with regard to targeted disease, VR equipment, and intervention materials. Thus, we categorized results within each of the following symptoms: anxiety and depression, fatigue, and pain management.
Overview of VR Intervention to Relieve Symptom Anxiety and Depression
Fourteen studies in total (Aminabadi et al., 2012; Dehghan et al., 2019; Gold et al., 2006; Kampmann et al., 2016; Krijn et al., 2004; Lee et al., 2015; Riva et al., 2003; Ryu et al., 2018; Schneider et al., 2003, 2004; Schneider & Hood, 2007; Shah et al., 2015; Song & Park, 2015; van Twillert et al., 2007) evaluated the efficiency of a VR intervention on relieving anxiety and depression. All of these studies found a statistically significant reduction on patients’ anxiety with the exception of the study by van Twillert et al. (2007), who evaluate anxiety before and after burn wound change after the use of VR. Four of the studies (Lee et al., 2015; Riva et al., 2003; Shah et al., 2015; Song & Park, 2015) had a decrease in the depression level of patients following the use of the VR intervention. In particular, in the study by Ryu et al. (2018), where they used a gaming VR intervention in children undergoing elective day surgery and general anesthesia, findings showed that children who used VR gaming had lower pretreating anxiety than those who did not use VR. Krijn et al. (2004) explored that VR was more effective compared with control in patients with acrophobia, while Aminabadi et al. (2012) explored whether VR can help children reduce their anxiety during dental procedures. Song and Park (2015) demonstrated that the group with the intervention showed more significant improvement in their depression state after the intervention than the group without VR intervention. Moreover, Schneider et al. (2003, 2004) and Schneider & Hood 2007) found that VR decreased the mean state of anxiety in cancer patients during the chemotherapy session.
Overview of VR Intervention to Relieve Symptom Fatigue
Of the 23 studies selected for this overview, 4 studies (Cho & Sohng, 2014; Schneider et al., 2003, 2004; Schneider & Hood, 2007) evaluated the efficiency of VR on fatigue.Three of these studies (Cho & Sohng, 2014; Schneider et al., 2004; Schneider & Hood, 2007) found a statistically significant reduction in symptom fatigue during VR assisted procedure, while the study by Schneider et al. (2003) did not report any statistically significant change of fatigue. Two studies (Schneider et al., 2004; Schneider & Hood, 2007) with cancer patients demonstrated a statistically significant difference in fatigue (i.e., reduction) immediately after chemotherapy treatment when subjects used the VR intervention. Cho and Sohng (2014) in their study with hemodialysis patients with end-stage renal failure found a statistically significant decrease of fatigue at the intervention group with VR exercise program, while almost no changes were noted in the control group.
Overview of VR Intervention Effects of Pain
As shown in Table 1, VR is used for acute pain management in inpatient populations more commonly than for chronic pain. The review yielded 11 studies (Aminabadi et al., 2012; Carrougher et al., 2009; Das et al., 2005; Gerçeker et al., 2018; Gold et al., 2006; JahaniShoorab et al., 2015; Kipping et al., 2012; Maani et al., 2011; Schmitt et al., 2011; van Twillert et al., 2007; Wint et al., 2002) that evaluated efficacy of VR on painful procedures. Six studies (Carrougher et al., 2009; Das et al., 2005; Kipping et al., 2012; Maani et al., 2011; Schmitt et al., 2011; van Twillert et al., 2007) used VR as a distraction intervention during wound changes of burn injuries in children and adults, while the others used VR during or after painful procedures. All studies found statistically significant reductions of pain rates during and after using VR procedure, with the exception of the study by Kipping et al. (2012) where no statistically significant changes between VR group and control group were found. In the other studies using VR for other painful procedures, such as dental procedures, intravenous placement, and lumbar puncture, the results showed that pain scores were lower in the VR groups compared with the control groups (Aminabadi et al., 2012; Gerçeker et al., 2018; Gold et al.,2006; Wint et al., 2002). Furthermore, many positive changes were recorded on secondary end point measurements such as emotional unpleasantness, time spent thinking about pain, and worst pain experience (Carrougher et al., 2009; Maani et al., 2011).
Discussion
In contrast with previous reviews of case reports and observational evidence, the present review focused on experimental studies that describe applications of VR technology on symptom management. Data from 23 eligible studies provided insights into four current medical applications of the VR system: anxiety, depression, fatigue, and pain management. These studies have contributed to our better understanding of the efficiency of VR in reducing these symptoms in different contexts and diseases, such as neurophysiological (Motl et al., 2009) or especially on cancer (Brown & Kroenke, 2009; So et al., 2009). The findings of this systematic review are congruent with those of previous researches, and reviews that suggest that VR can be used to effectively manage symptoms (Chirico et al., 2016; Dascal et al., 2017; Hoffman et al., 2000; Wint et al., 2002). Although studies varied greatly in terms of the contextual setting and the method of intervention, this review identified some overarching themes in addressing the research questions presented in the Introduction section.
Anxiety and Depression
The use of VRET for clinical purpose on anxiety and depression has been investigated empirically for many years. The VR has been used as a tool to deliver exposure therapy, psychoeducation, and relaxation therapy in people suffering from one or both of these symptoms. The results of four independent meta-analyses enhance the conclusion that such interventions lead to significant decreases in anxiety- and depression-related symptoms (Morina et al., 2015; Opriş et al., 2012; Parsons & Rizzo, 2008; Powers & Emmelkamp, 2008). All the studies with a primary focus on anxiety and depression that were included in this review demonstrated an important decrease on the anxiety and depression levels in patients. These results contributed to the preceding evidence showing that the use of VR as an intervention in clinical settings has important positive effects on depression and anxiety level.
Fatigue
Fatigue is a major problem and concern for many patients with diseases such as cancer, stroke, renal failure, autoimmune disorders, and lung disease (chronic obstructive pulmonary disease) to name a few. In a cross-sectional descriptive study with 148 randomly recruited prostate cancer patients in active treatment, the aim was to explore cancer-related fatigue and its impact on quality of life (Charalambous & Kouta, 2016). The results demonstrated that fatigue is a common symptom among patients with advance prostate cancer undergoing treatment. This was supported by the high levels of fatigue reported in this sample with almost two thirds of the patients (66.9%) reporting fatigue as a problem. Findings from this study show that VR could be a potential tool to secure better fatigue levels for all patients. Moreover, findings also identified a relationship between higher levels of presence in the virtual environment and lower levels of fatigue and anxiety. However, there are limited number of studies that have been undertaken to measure VR effectiveness on fatigue. This stresses the need for additional longitudinal studies in this context.
Pain
The findings of experimental studies within the context of pain experience showed that VR distraction is an effective nonpharmacologic intervention for reducing pain from undergoing unpleasant medical procedures (acute or chronic), as well as the pain associated with burn injury care in adult and pediatric patients. According to the theory of pain management, decreased pain can be achieved by blocking the information of pain via analgesics drugs or by creating some sort of distraction that deviates the focus of the brain on pain (Gershon et al., 2004; Parsons et al., 2009).Many side effects can be caused by the medical analgesics such as nausea, increased length of hospitalizations, and inadequate pain alleviation (Teeley et al., 2012). These traditional pharmacotherapies can be supplemented (or even replaced in some cases) by VR as a particularly useful pain distraction intervention. Furthermore, our results coincide with those of preceding studies that VR has been reported to be an effective modality to decrease pain during burn care (Gershon et al., 2004). A systematic review of nine studies by Morris et al. (2009) found that VR coupled with standard analgesia was effective in reducing pain during burn care in eight of the nine studies. Last, but not least, Indovina et al. (2018) in their systematic review using Virtual Reality as a Distraction Intervention to Relieve Pain and Distress During Medical Procedures stated that VR has proven to be effective in reducing procedural pain, as almost invariably observed even in patients subjected to extremely painful procedures, such as patients with burn injuries undergoing wound care, and physical therapy. Moreover, VR seemed to decrease cancer-related symptoms in different settings, including during chemotherapy. VR could promise a useful alternative way of reducing the pain with minimal side effects or one that could enhance standard pain management.
Although the use of VR in the majority of the studies included in this review showed a very positive effect on the specific symptoms of interest, it is possible that some confounding factors might have affected the effectiveness of VR. The researches therefore completed a thorough check of the included studies based on the quality assessment tool. Variables that have been considered included the type of images on VR that seems to work better, the best type of the devices, the interaction with the environment, and finally considering the differentiating of the sense of presence between immersive and nonimmersive VR. This assessment highlighted the fact that the tools utilized in these studies for evaluating the symptoms were different. However, all tools were valid and reliable to measure the symptoms and have previously used in clinical studies. According to the assessment, VR interventions that were game based were found more effective in children as a means to distract them from the hospital environment and the medical procedures. Adults showed a preference toward more natural and relaxing environments and requested to have variety of choices in terms of the virtual environments they could experience (sea, mountains, and adventures). Furthermore, the duration of the intervention varied from study to study, and this variation appeared to be related to the target symptom. For example, Dehghan et al. (2019) used VR for 5 minutes only to reduce anxiety in children scheduled for operation, and in Shah et al. (2015), the intervention lasted 1 hour over 3-day period to reduce anxiety and depression. Both studies demonstrated a positive effect of VR on reducing anxiety and depression. Therefore, further studies are needed to validate the effective time of the VR intervention. Furthermore, the devices that were used in the studies were also different. In the more recent studies where the latest technology of VR was used, participants mentioned that the images and the sense of presence were very realistic, and the interaction was more efficient by using more advance special controllers (e.g., gloves, remote control). Finally, participants did not report any motion sickness or any unusual symptoms during the use of VR, which means VR it is safe and does not cause any side effects.
The studies we reviewed have several strengths. The majority of the studies reviewed employed a randomized control trial’s design, offering the highest level of evidence on the effectiveness of the VR interventions tested. The specific content of interventions was fairly consistent within each category. Moreover, a wide variety of patients were studied, including inpatients and outpatients, patients receiving treatment and those who had completed it, as well as individuals with various diagnoses and stages of disease.
This review included studies that were very heterogeneous in study design as well as theoretical background and the way the intervention was conducted. The principal differences between studies were the use of different disease, instruments, and analysis. Some of the studies required the presence of symptoms as an inclusion criterion, reducing the possibility of floor effects in these trials. Furthermore, sample sizes used in most trials were small to moderate (N < 50). Specific types (immersive, nonimmersive) and doses (duration, frequency, virtual environment) of VR intervention varied across studies.
Future Research
As the results of this review showed, future studies of VR should be undertaken in the context of medical inpatients with larger samples and assessed over time to investigate long-term effects. This intervention has the potential to be effective for patients with a variety of diagnoses and across a wide range of ages. However, although most VR studies are done only in hospital settings, some health professionals point out that VR should also be promoted as a home-based technique. Another issue that needs to be considered is the sense of independence and self-improvement promoted by VR at the home setting for users to be able to implement the VR intervention without supervision and on demand, allowing a sense of control over the symptoms and on the overall disease.
Conclusion
As VR technology expands and becomes more usable, effective, and safe, budget concerns give way to ability for greater impact. The majority of patients were very satisfied, and in most cases, patients state that experience with VR was fun, immersive, and enjoyable, with not a lot of side effects, considering that they would definitely use VR again. Studies varied in terms of quality, but we observed no relationship between study quality and key findings. The findings of this study agree with those of previous research that suggest that VR can be used to manage symptoms. The use of VR in medical fields is relatively novel and promising. It is highly interactive, flexible, tailored to the individual, and applicable to people varying in age, sex, and medical disorders. As technology improves and costs are reduced, VR will play a major role in the future of health care.
Authors’ Note
Dr. Marios Avraamides is also affiliated to Research Centre on Interactive Media, Smart System and Emerging Technologies (RISE).
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Androniki Ioannou https://orcid.org/0000-0002-3343-8768
Andreas Charalambous https://orcid.org/0000-0003-4050-031X
References
- Aminabadi N. A., Erfanparast L., Sohrabi A., Ghertasi Oskouei S., Naghili A. (2012). The impact of virtual reality distraction on pain and anxiety during dental treatment in 4-6 year-old children: A randomized controlled clinical trial. Journal of Dental Research, Dental Clinics, Dental Prospects, 6(4), 117–124. 10.5681/joddd.2012.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K. O., Cohen M. Z., Mendoza T. R., Guo H., Harle M. T., Cleeland C. S. (2006). Brief cognitive‐behavioral audiotape interventions for cancer related pain: Immediate but not long‐term effectiveness. Cancer: Interdisciplinary International Journal of the American Cancer Society, 107(1), 207–214. [DOI] [PubMed] [Google Scholar]
- Biocca F. (1992). Virtual reality technology: A tutorial. Journal of Communication, 42(4), 23–72. [Google Scholar]
- Brown L. F., Kroenke K. (2009). Cancer-related fatigue and its associations with depression and anxiety: A systematic review. Psychosomatics, 50(5), 440–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrougher G. J., Hoffman H. G., Nakamura D., Lezotte D., Soltani M., Leahy L., Engrav L.H., Patterson D. R. (2009). The effect of virtual reality on pain and range of motion in adults with burn injuries. Journal of Burn Care & Research, 30(5), 785–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charalambous A., Kouta C. (2016). Cancer related fatigue and quality of life in patients with advanced prostate cancer undergoing chemotherapy. BioMed Research International, 2016, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico A., Lucidi F., De Laurentiis M., Milanese C., Napoli A., Giordano A. (2016). Virtual reality in health system: Beyond entertainment. A mini‐review on the efficacy of VR during cancer treatment. Journal of Cellular Physiology, 231(2), 275–287. [DOI] [PubMed] [Google Scholar]
- Cho, H., & Sohng, K. (2014). The effect of a virtual reality exercise program on physical fitness, body composition, and fatigue in hemodialysis patients. Journal of Physical Therapy Science, 26(10), 1661–1665. [DOI] [PMC free article] [PubMed]
- Das D. A., Grimmer K. A., Sparnon A. L., McRae S. E., Thomas B. H. (2005). The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: A randomized controlled trial [ISRCTN87413556]. BMC Pediatrics, 5(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dascal J., Reid M., IsHak W. W., Spiegel B., Recacho J., Rosen B., Danovitch I. (2017). Virtual reality and medical inpatients: A systematic review of randomized, controlled trials. Innovations in Clinical Neuroscience, 14(1–2), 14–21. [PMC free article] [PubMed] [Google Scholar]
- Dehghan F., Jalali R., Bashiri H. (2019). The effect of virtual reality technology on preoperative anxiety in children: A Solomon four-group randomized clinical trial. Perioperative Medicine, 8(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer-García M., Gutiérrez-Maldonado J. (2012). The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: A review of the literature. Body Image, 9(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Gerçeker G. Ö., Binay Ş., Bilsin E., Kahraman A., Yılmaz H. B. (2018). Effects of virtual reality and external cold and vibration on pain in 7-to 12-year-old children during phlebotomy: A randomized controlled trial. Journal of PeriAnesthesia Nursing, 33(6), 981–989. [DOI] [PubMed] [Google Scholar]
- Gershon J., Zimand E., Pickering M., Rothbaum B. O., Hodges L. (2004). A pilot and feasibility study of virtual reality as a distraction for children with cancer. Journal of the American Academy of Child & Adolescent Psychiatry, 43(10), 1243–1249. [DOI] [PubMed] [Google Scholar]
- Gold J. I., Kim S. H., Kant A. J., Joseph M. H., Rizzo A. S. (2006). Effectiveness of virtual reality for pediatric pain distraction during IV placement. CyberPsychology & Behavior, 9(2), 207–212. [DOI] [PubMed] [Google Scholar]
- Hoffman H. G., Patterson D. R., Carrougher G. J. (2000). Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: A controlled study. The Clinical Journal of Pain, 16(3), 244–250. [DOI] [PubMed] [Google Scholar]
- Humphreys J., Janson S., Donesky D. A., Dracup K., Lee K. A., Puntillo K., Faucett, J. A., Aouizerat, B., Miaskowski, C., Baggott, C., Carrieri-Kohlman, V., Barger, M., Franck, L., Kennedy, C., & University of California, San Francisco, School of Nursing, Symptom Management Faculty Group. (2014). Theory of symptom management. In M. J. Smith & P. R. Liehr (Eds.), Middle range theory for nursing (pp. 141–164). Springer Publishing Company.
- Indovina P., Barone D., Gallo L., Chirico A., De Pietro G., Giordano A. (2018). Virtual reality as a distraction intervention to relieve pain and distress during medical procedures. The Clinical Journal of Pain, 34(9), 858–877. [DOI] [PubMed] [Google Scholar]
- JahaniShoorab N., Ebrahimzadeh Zagami S., Nahvi A., Mazluom S. R., Golmakani N., Talebi M., Pabarja F. (2015). The effect of virtual reality on pain in primiparity women during episiotomy repair: A randomize clinical trial. Iranian Journal of Medical Sciences, 40(3), 219–224. [PMC free article] [PubMed] [Google Scholar]
- Kampmann I. L., Emmelkamp P. M., Hartanto D., Brinkman W., Zijlstra B. J., Morina N. (2016). Exposure to virtual social interactions in the treatment of social anxiety disorder: A randomized controlled trial. Behaviour Research and Therapy, 77, 147–156. [DOI] [PubMed] [Google Scholar]
- Kipping B., Rodger S., Miller K., Kimble R. M. (2012). Virtual reality for acute pain reduction in adolescents undergoing burn wound care: A prospective randomized controlled trial. Burns, 38(5), 650–657. [DOI] [PubMed] [Google Scholar]
- Krijn M., Emmelkamp P. M. G., Biemond R., de Wilde de Ligny C., Schuemie M. J., van der Mast C. A. P. G. (2004). Treatment of acrophobia in virtual reality: The role of immersion and presence. Behaviour Research and Therapy, 42(2), 229–239. [DOI] [PubMed] [Google Scholar]
- Kwekkeboom K. L., Abbott-Anderson K., Wanta B. (2010). Feasibility of a patient-controlled cognitive-behavioral intervention for pain, fatigue, and sleep disturbance in cancer. Oncology Nursing Forum, 37(3), E151–E159 10.1188/10.ONF.E151-E159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwekkeboom K. L., Kneip J., Pearson L. (2003). A pilot study to predict success with guided imagery for cancer pain. Pain Management Nursing, 4(3), 112–123. [DOI] [PubMed] [Google Scholar]
- Lee N., Lee D., Song H. (2015). Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson’s disease patients. Journal of Physical Therapy Science, 27(1), 145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liszio S., Graf L., Masuch M. (2018). The relaxing effect of virtual nature: Immersive technology provides relief in acute stress situations. Annual Review of Cybertherapy and Telemedicine, 2018, 87. [Google Scholar]
- Llobera J., González-Franco M., Perez-Marcos D., Valls-Solé J., Slater M., Sanchez-Vives M. V. (2013). Virtual reality for assessment of patients suffering chronic pain: A case study. Experimental Brain Research, 225(1), 105–117. [DOI] [PubMed] [Google Scholar]
- Maani C. V., Hoffman H. G., Morrow M., Maiers A., Gaylord K., McGhee L. L., DeSocio P. A. (2011). Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. The Journal of Trauma, 71(1 Suppl), S125– S130 10.1097/TA.0b013e31822192e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malloy K. M., Milling L. S. (2010). The effectiveness of virtual reality distraction for pain reduction: A systematic review. Clinical Psychology Review, 30(8), 1011–1018. [DOI] [PubMed] [Google Scholar]
- McCann R. A., Armstrong C. M., Skopp N. A., Edwards-Stewart A., Smolenski D. J., June J. D., . . . Reger G. M. (2014). Virtual reality exposure therapy for the treatment of anxiety disorders: An evaluation of research quality. Journal of Anxiety Disorders, 28(6), 625–631. [DOI] [PubMed] [Google Scholar]
- Medling B. (2005). Virtual reality utilization in health care: It’s virtually done. Biomedical Instrumentation & Technology, 16(8). [PubMed] [Google Scholar]
- Morina N., Ijntema H., Meyerbröker K., Emmelkamp P. M. (2015). Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behaviour Research and Therapy, 74, 18–24. [DOI] [PubMed] [Google Scholar]
- Morris L. D., Louw Q. A., Grimmer-Somers K. (2009). The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: A systematic review. The Clinical Journal of Pain, 25(9), 815–826. [DOI] [PubMed] [Google Scholar]
- Motl R. W., McAuley E., Snook E. M., Gliottoni R. C. (2009). Physical activity and quality of life in multiple sclerosis: Intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychology, Health & Medicine, 14(1), 111–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opriş D., Pintea S., García-Palacios A., Botella C., Szamosközi Ş., David D. (2012). Virtual reality exposure therapy in anxiety disorders: A quantitative meta‐analysis. Depression and Anxiety, 29(2), 85–93. [DOI] [PubMed] [Google Scholar]
- Parsons T. D., Rizzo A. A. (2008). Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis. Journal of Behavior Therapy and Experimental Psychiatry, 39(3), 250–261. [DOI] [PubMed] [Google Scholar]
- Parsons T. D., Rizzo A. A., Rogers S., York P. (2009). Virtual reality in paediatric rehabilitation: A review. Developmental Neurorehabilitation, 12(4), 224–238. [DOI] [PubMed] [Google Scholar]
- Powers M. B., Emmelkamp P. M. (2008). Virtual reality exposure therapy for anxiety disorders: A meta-analysis. Journal of Anxiety Disorders, 22(3), 561–569. [DOI] [PubMed] [Google Scholar]
- Riener R., Harders M. (2012). Virtual reality in medicine. Springer Science & Business Media. [Google Scholar]
- Riva G., Bacchetta M., Cesa G., Conti S., Molinari E. (2003). Six-month follow-up of in-patient experiential cognitive therapy for binge eating disorders. Cyberpsychology & Behavior, 6(3), 251–258. [DOI] [PubMed] [Google Scholar]
- Riva G., Gaggioli A., Villani D., Preziosa A., Morganti F., Corsi R., . . . Vezzadini L. (2007). NeuroVR: An open source virtual reality platform for clinical psychology and behavioral neurosciences. Studies in Health Technology and Informatics, 125, 394–399. [PubMed] [Google Scholar]
- Ryu J., Park J., Nahm F. S., Jeon Y., Oh A., Lee H. J., . . . Han S. (2018). The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: A prospective, randomized, and controlled trial. Journal of Clinical Medicine, 7(9), 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt Y. S., Hoffman H. G., Blough D. K., Patterson D. R., Jensen M. P., Soltani M., . . . Sharar S. R. (2011). A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns, 37(1), 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S. M., Ellis M., Coombs W. T., Shonkwiler E. L., Folsom L. C. (2003). Virtual reality intervention for older women with breast cancer. CyberPsychology & Behavior, 6(3), 301–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S. M., Hood L. E. (2007). Virtual reality: A distraction intervention for chemotherapy. Oncology Nursing Forum, 34(1), 39–46. 10.1188/07.ONF.39-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S. M., Prince-Paul M., Allen M. J., Silverman P., Talaba D. (2004). Virtual reality as a distraction intervention for women receiving chemotherapy. Oncology Nursing Forum, 31(1), 81–88. [DOI] [PubMed] [Google Scholar]
- Shah L. B. I., Torres S., Kannusamy P., Chng C. M. L., He H., Klainin-Yobas P. (2015). Efficacy of the virtual reality-based stress management program on stress-related variables in people with mood disorders: The feasibility study. Archives of Psychiatric Nursing, 29(1), 6–13. [DOI] [PubMed] [Google Scholar]
- So W. K., Marsh G., Ling W., Leung F., Lo J. C., Yeung M., Li G. K. (2009). The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: A multicenter study. Oncology Nursing Forum, 36(4), E205–E214. [DOI] [PubMed] [Google Scholar]
- Song G. B., Park E. C. (2015). Effect of virtual reality games on stroke patients’ balance, gait, depression, and interpersonal relationships. Journal of Physical Therapy Science, 27(7), 2057–2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeley A. M., Soltani M., Wiechman S. A., Jensen M. P., Sharar S. R., Patterson D. R. (2012). Virtual reality hypnosis pain control in the treatment of multiple fractures: A case series. American Journal of Clinical Hypnosis, 54(3), 184–194. [DOI] [PubMed] [Google Scholar]
- van Twillert B., Bremer M., Faber A. W. (2007). Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. Journal of Burn Care & Research, 28(5), 694–702. [DOI] [PubMed] [Google Scholar]
- Wiederhold B. K. (2006). The potential for virtual reality to improve health care. The Virtual Reality Medical Center.
- Wiederhold M. D., Wiederhold B. K. (2007). Virtual reality and interactive simulation for pain distraction Pain Medicine, 8, S182–S188.
- Wint S. S., Eshelman D., Steele J., Guzzetta C. E. (2002). Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncology Nursing Forum, 29(1), E8–E15. [DOI] [PubMed] [Google Scholar]
- Yu C., Lee H., Luo X. (2018). The effect of virtual reality forest and urban environments on physiological and psychological responses. Urban Forestry & Urban Greening, 35, 106–114. [Google Scholar]