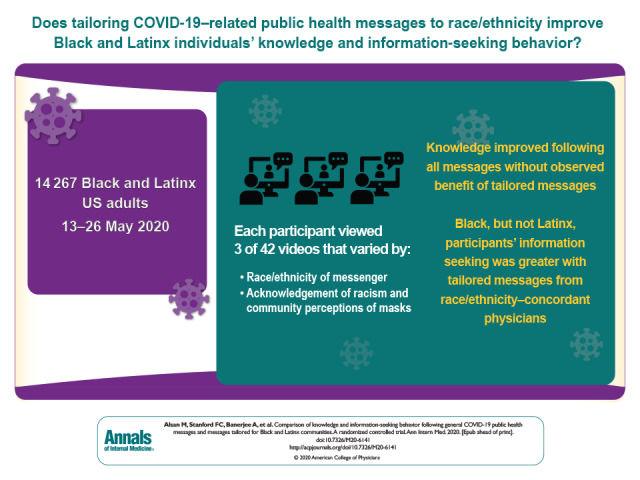
The paucity of public health messages that directly address communities of color might contribute to racial and ethnic disparities in COVID-19–related knowledge and behavior. This randomized trial examined whether physician-delivered prevention messages affect knowledge and information-seeking behavior of Black and Latinx persons and if this differs according to the race/ethnicity of the physician and the tailored content.
Visual Abstract. General and Tailored COVID-19 Health Messaging to U.S. Minorities.
The paucity of public health messages that directly address communities of color might contribute to racial and ethnic disparities in COVID-19–related knowledge and behavior. This randomized trial examined whether physician-delivered prevention messages affect knowledge and information-seeking behavior of Black and Latinx persons and if this differs according to the race/ethnicity of the physician and the tailored content.
Abstract
Background:
The paucity of public health messages that directly address communities of color might contribute to racial and ethnic disparities in knowledge and behavior related to coronavirus disease 2019 (COVID-19).
Objective:
To determine whether physician-delivered prevention messages affect knowledge and information-seeking behavior of Black and Latinx individuals and whether this differs according to the race/ethnicity of the physician and tailored content.
Design:
Randomized controlled trial. (Registration: ClinicalTrials.gov, NCT04371419; American Economic Association RCT Registry, AEARCTR-0005789)
Setting:
United States, 13 May 2020 to 26 May 2020.
Participants:
14 267 self-identified Black or Latinx adults recruited via Lucid survey platform.
Intervention:
Participants viewed 3 video messages regarding COVID-19 that varied by physician race/ethnicity, acknowledgement of racism/inequality, and community perceptions of mask-wearing.
Measurements:
Knowledge gaps (number of errors on 7 facts on COVID-19 symptoms and prevention) and information-seeking behavior (number of Web links demanded out of 10 proposed).
Results:
7174 Black (61.3%) and 4520 Latinx (38.7%) participants were included in the analysis. The intervention reduced the knowledge gap incidence from 0.085 to 0.065 (incidence rate ratio, [IRR], 0.737 [95% CI, 0.600 to 0.874]) but did not significantly change information-seeking incidence. For Black participants, messages from race/ethnic-concordant physicians increased information-seeking incidence from 0.329 (for discordant physicians) to 0.357 (IRR, 1.085 [CI, 1.026 to 1.145]).
Limitations:
Participants' behavior was not directly observed, outcomes were measured immediately postintervention in May 2020, and online recruitment may not be representative.
Conclusion:
Physician-delivered messages increased knowledge of COVID-19 symptoms and prevention methods for Black and Latinx respondents. The desire for additional information increased with race-concordant messages for Black but not Latinx respondents. Other tailoring of the content did not make a significant difference.
Primary Funding Source:
National Science Foundation; Massachusetts General Hospital; and National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Black and Latinx communities have been disproportionately affected by coronavirus disease 2019 (COVID-19) (1, 2). The disparities in prevalence and health outcomes reflect a complex set of factors, including systemic racism, inequality in access to health services, educational opportunities, and occupational differences (3), but they may also partly reflect knowledge gaps. A nationally representative survey found large gaps in knowledge of COVID-19 symptoms and transmission among Black and Latinx respondents (4). While messaging campaigns and public service announcements have been deployed, little attention has been given to how to frame messages for communities of color. In particular, the majority of messaging is delivered by White experts, and messages may not be framed to specifically address these communities' concerns (5). Since the beginning of the pandemic, healthcare professionals have reached out to spread prevention messages using social media (6), yet there is no evidence on the effectiveness of this effort.
Given this lack of evidence, we partnered with the Center for Diversity and Inclusion at Massachusetts General Hospital (MGH) and over 40 physicians from MGH and Lynn Community Health Center to develop COVID-19 health messages that would address the specific concerns of these communities. We dubbed this group of staff, researchers, and clinicians the “COVID-19 Messaging Working Group.” Black and Latinx respondents were randomly assigned to receive video messages on COVID-19 delivered by a study physician.
We sought to identify whether messages delivered by physicians would increase COVID-19 knowledge and improve preventive behaviors for Latinx and Black individuals and to assess whether race or ethnic concordance, acknowledgments of injustice, or information on social perceptions would make the message more effective, as measured by a reduced knowledge gap and change in information-seeking behaviors.
Methods
Trial Design and Oversight
The study flow diagram (Appendix Figures 1 to 3, available at Annals.org) shows the factorial design and the allocation of participants to each intervention arm. The design was approved by the ethical review boards of Massachusetts Institute of Technology and Stanford University, with MGH, Yale University, and Harvard University ceding authority to the Massachusetts Institute of Technology. Messages were produced after several focus groups with physicians and leaders from the Center for Diversity and Inclusion. The trial was registered on ClinicalTrials.gov, which specified the main primary and secondary outcomes. Planned analyses were prespecified and published on the American Economic Association RCT Registry. The main change from preplanned analyses is that we report negative binomial regressions for count outcomes and logistic regression for binary outcomes (rather than ordinary least squares), and we weighted observations to correct for attrition.
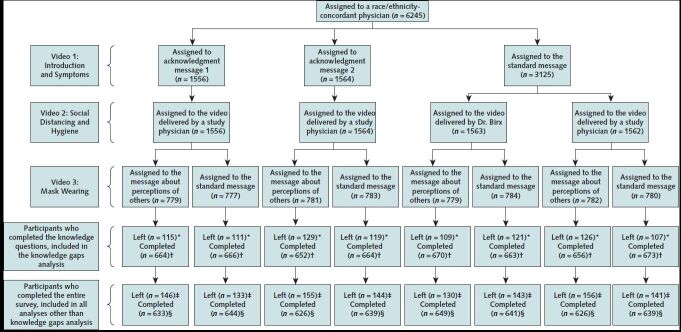
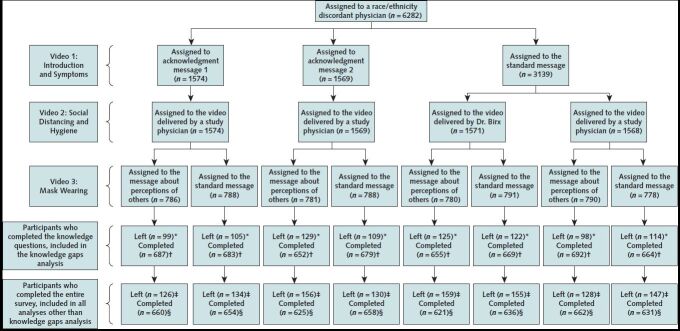
Appendix Figure 1. Enrollment and randomization of participants.
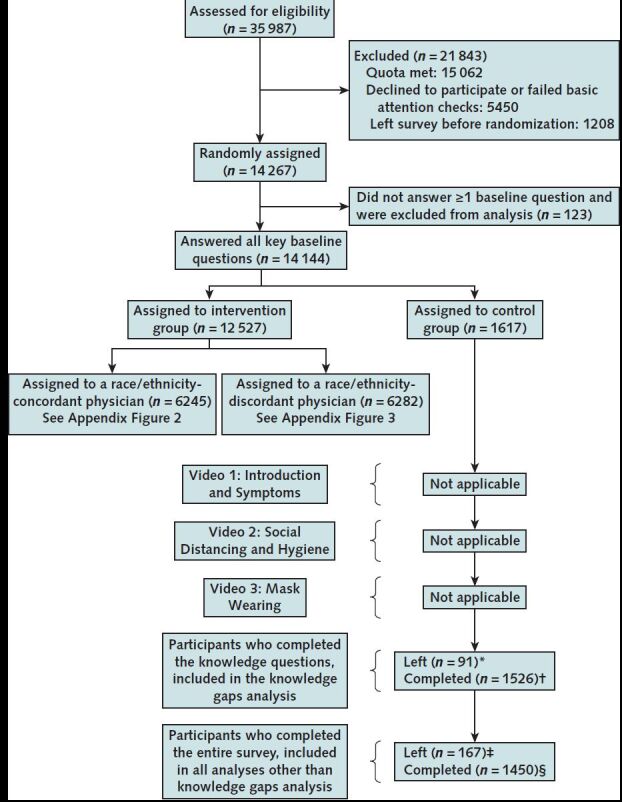
* Participants who left the survey before the knowledge outcome.
† Participants who completed the knowledge questions and were included in the knowledge outcome analysis questions.
‡ Participants left the survey before the links outcome.
§ Participants completed the survey and were included in all analyses.
Appendix Figure 2. Study flow diagram: group assigned to a race/ethnicity-concordant physician.
See Appendix Figure 1 for caption.
Appendix Figure 3. Study flow diagram: group assigned to a race/ethnicity-discordant physician.
See Appendix Figure 1 for caption.
Participants
Individuals were recruited throughout the United States by the survey company Lucid from 13 May to 26 May 2020. Only persons aged 18 years or older and self-identifying as Black or Latinx were eligible. Individuals with a secondary education or less were oversampled because these individuals were considered more likely to have knowledge gaps, by imposing a quota of 5% of our target sample size on individuals with a college degree. We also used quotas to match the 2018 population estimates by age, sex, race and Hispanic origin issued by the U.S. Census Bureau (7). Quotas were implemented to assess eligibility by the survey company Lucid.
Interventions
Messages on COVID-19 developed for the study were read by 42 physicians. Each message was recorded by several physicians, who varied in age, gender, race and ethnicity. Each respondent saw 3 videos, read by 3 different physicians. Section B of the Supplement (available at Annals.org) includes scripts, and the videos are available on the project Web site (8). Participants could elect to receive the messages in English or Spanish.
Video 1 defined COVID-19 as a virus that mainly infects the lungs and stated that although many infected people improve spontaneously, some get very sick and die. It discussed common symptoms associated with COVID-19 and asymptomatic transmission. Video 2 defined and discussed the importance of social distancing and hygiene using the script of a public service announcement featuring Dr. Deborah Birx, lead of the White House Coronavirus Task Force. Video 3 discussed wearing a mask or facial covering and emphasized its importance despite potential uncomfortable reactions by others.
In the intervention group, individuals answered sociodemographic questions, saw 3 videos, and then completed the outcome survey questions. In the control group, respondents answered all survey questions first and then saw the 3 videos.
The video messages were all delivered either by a concordant or discordant study physician. The content of the video varied along the following dimensions.
Video 1
In the baseline condition, physicians delivered information about COVID-19 and its symptoms. In the acknowledgment condition, in addition to the baseline message, the physicians explicitly acknowledged social constraints on access to healthcare. For Black participants, the message either acknowledged unequal treatment in health care or economic hardships that were associated with tight living quarters and working in essential services. For Latinx participants, the message either acknowledged fears about immigration status that made it difficult to seek care or the same economic hardship statement noted for the Black participants.
Video 2
Participants included in the baseline (that is, no acknowledgement) condition in video 1 received a message on social distancing and prevention delivered either by a study physician or by Dr. Deborah Birx. For Dr. Birx, we used an official Public Service Announcement (9), and the study physician read an identical script in their own voice. The rationale was to test whether the same message would be less effective delivered by the White House official spokesperson (who may be viewed as a polarizing figure).
Video 3
All participants received information about the importance of wearing masks. Those assigned to the “social perception” group further received information from study physicians that 8 out of 10 Americans report that an Black/Latinx person wearing a mask is protecting their community (this figure came from a nationally representative survey of 2611 respondents we conducted on 23 April 2020 [Section C of the Supplement]).
Outcomes
All outcomes were measured online immediately after the intervention for the intervention group and immediately after the sociodemographic survey questions for the control group.
The primary outcome prespecified in the registration on ClinicalTrials.gov was knowledge, beliefs, and practices related to COVID-19. The secondary outcome was video ratings. We also collected data on additional outcomes, prespecified in our preanalysis plan. For brevity, in the main text, we only present the results on our primary outcomes: a summary measure of knowledge and beliefs related to COVID-19 and practice. Given the difficulty of observing actual behavior, practice was measured by information-seeking behavior within the survey.
The full set of outcomes (prespecified in the preanalysis plan, page 7) are as follows.
Time spent watching the videos, and video ratings. Results on time spent watching video and video rating are presented in Supplement Table 1 (available at Annals.org).
Knowledge and beliefs. To measure knowledge and beliefs, participants were asked to identify ways to prevent COVID-19 spread, including staying 6 feet away from other people when outside, washing their hands when returning home, and wearing a mask/facial covering when outside. Failure to identify each of these 3 practices added 1 to the knowledge gap count. Participants were then asked whether COVID-19 could be asymptomatically transmitted; those who answered “no” received an additional unit to the knowledge gap count. Finally, participants were asked to select exactly 3 common COVID-19 symptoms from a list of 9 symptoms. Each symptom selected that was not among cough, fever, difficulty breathing, or new loss of taste or smell increased the knowledge gap count by 1. The knowledge gaps outcome is an integer that can take values from 0 (complete knowledge) to 7 (incomplete knowledge). We also define an indicator for “any gap in knowledge,” which is 1 if the knowledge gap is 1 or greater and 0 otherwise.
Trust in the health care system; health information–seeking behavior and interest in information on social distancing and hygiene. Trust in the health care system, health information–seeking behavior, and interest in more information on social distancing and hygiene were measured by asking whether the participant was interested in Web links to Web pages or videos. They could elect to obtain any of 10 weblinks, and if they did, they received the information at the end of the survey. Specifically, the links were presented as more information about Web resources about COVID-19 from MGH; a COVID-19 app from MGH; the respondent's state COVID-19 hotline; telehealth; mental health resources; COVID-19 testing locations; how to make a mask at home without sewing; how to safely disinfect one's home; how to exercise in small spaces; and tips to keep children moving in a small space. Links are provided in Section D of the Supplement.
The information-seeking behavior outcome is the number of links for which participants expressed interest (that is, the click-through rate), a count variable between 0 (lowest information-seeking behavior) and 10 (greatest information-seeking behavior). We also defined an outcome “any link demanded,” which was assigned a value of 1 if the participant demanded any link and 0 otherwise. Click-through rates are a standard metric for gauging the success of advertising campaigns in marketing (10), but a limitation is that they may not be an accurate proxy of behavior.
Views on mask-wearing. To assess whether those assigned to the “social perception” intervention in fact changed participants' views, we presented them with a photo asking them their view on how others would perceive people wearing a mask (Supplement Table 2-Table 3-Table 4, available at Annals.org).
Allocations to organizations supporting mask-wearing. We asked respondents how they would prefer the study allocate a donation between two organization targeted to their community, one that supports masks, and another that supports economic relief (Supplement Table 3 and Table 4).
Randomization
Random assignment into the control group versus to an intervention group and between intervention groups was stratified according to sex, age (> 45 years), and location (by first digit of ZIP code, to proxy for coastal versus noncoastal states: 0, 1, 2, and 9 is one category, and 3, 4, 5, 6, 7, and 8 is another). The study flow diagram (Appendix Figures 1 to 3, available at Annals.org) summarize the randomization. One in 9 respondents was assigned to the control group, and 8 in 9 respondents were assigned to an intervention group.
In the intervention group, participants were randomly assigned to race/ethnicity-concordant encounters and race/ethnicity-discordant encounters with equal probability. Within each discordant and concordant arm, participants were further randomly assigned, with equal probability, into 1 of 4 arms: the original Dr. Birx video about social distancing; the same message read by one of the study physicians; or 2 versions of the same message read by 1 of the study physicians, with additional acknowledgements of specific difficulties faced by Black and Latinx communities, depending on the respondent. Finally, within each of these arms, participants were randomly assigned with equal probability to receive information about perception of people wearing masks. Random assignment to video content was performed using the online survey platform Qualtrics in its May 2020 version. It was implemented in the Survey Flow using a Randomizer block within each stratum with the option to evenly present elements.
Statistical Analysis
We determined that a sample of 15 000 individuals (10 000 Black and 5000 Latinx) would provide 85% power to detect effect sizes of 0.08 SD for any intervention relative to control, and for effects of specific variations in message content.
The analysis was performed by original assigned group and included all the participants who answered all baseline questions and completed the survey up to the knowledge questions (for the knowledge gaps analysis) or up to the Web links question (for all other analyses). For count data, we use negative binomial regression to assess the effectiveness of our randomized messaging interventions. Models include the stratifying variables (age by sex by location dummies), race, and an indicator for preferred video language (English or Spanish).
To address bias stemming from nonrandom attrition, we weight the data using Hainmueller entropy weights (11), which ensures that the observed baseline characteristics of the sample matches the original sample as closely as possible (Section E of the Supplement 1).
To analyze effects of seeing any video message on the knowledge gap and information seeking outcomes, we fit the following negative binomial regression model:
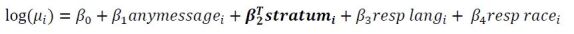
where μi is the estimated mean outcome value (knowledge gap count or count of demanded links); anymessagei is an indicator for receipt of videos before outcome measures (that is, not being in the control group); stratum i is a vector of indicator variables, denoting which stratum was assigned, resp langi is an indicator for participants who chose to receive videos in Spanish; and resp racei is an indicator for the participant's self-identified race or ethnicity.
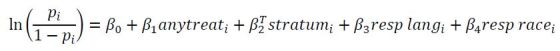
We also fit a logistic regression on the same model using the outcomes any gap in knowledge and any info demanded (section H of the Supplement). Noting pi = P(Any gap = 1), we fit the following logistic regression equation:
To analyze whether the videos have larger effects when they are tailored to the Black or Latinx communities, we consider only participants assigned to the “any intervention group” and fit a negative binomial regression model:
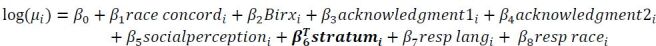
where race concordi is an indicator that equals 1 if the physician and the recipient share the same race or ethnicity and 0 otherwise, Birxi is an indicator for video 2 featuring Dr. Birx, acknowledgment1i is an indicator that equals 1 if video 1 included an acknowledgment of inequality in health care (Black participants) or the immigration-related fears associated with seeking health care (Latinx participants), acknowledgment 2i is an indicator for video 1 acknowledging economic hardships affecting minorities, and socialperceptioni is an indicator that the social perception message is included in video 3.
Finally, we fit the same model for a logistic regression on any gap in knowledge and any info demanded (Supplement; results are shown in Supplement Table 6, Table 7, and Table 8, available at Annals.org).
We performed additional analyses in which we 1) controlled for additional baseline covariates using a double-robust machine learning algorithm (12), 2) used unweighted regression specifications, 3) analyzed effects on secondary outcomes and 4) test for heterogenous effects by prior perceptions about masks (Section F of the Supplement).
Analyses were performed by using R, version 3.6.1, including the following packages (versions): stats (3.6.1), tidyverse (1.3.0), estimatr (0.22), anytime (0.3.9), readr (1.3.1), dplyr (1.0.0), lubridate (1.7.9), stargazer (5.2.2), hdm (0.3.1), fastDummies (1.6.2), mfx (1.2-2), car (3.0.3), MASS (7.3.51.4), cobalt (4.2.3), WeightIt (0.10.2), ebal (0.1.6), pscl (1.5.5). The data and all statistical codes are publicly available on Harvard Dataverse (13).
Role of the Funding Source
The study was funded by the National Science Foundation; Massachusetts General Hospital; and National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. The funding sources had no role in the design or conduct of the trial, interpretation of the data, or preparation of the manuscript.
Results
The trial sample was enrolled from 13 May 2020 through 26 May 2020. Of 35 987 persons screened, 20 925 were eligible for participation (15 062 who would have been eligible were excluded because the demographic quotas were met); 5450 individuals did not consent or failed both basic attention checks, and 1208 left the survey before randomization.
Then, 14 267 persons were randomly assigned, of whom 123 failed to answer at least 1 baseline question. The 123 participants with missing baseline data are excluded from the main analysis because we use baseline data to weight observations and account for attrition. Therefore, the final sample comprises 14 144 individuals with complete baseline data.
Of those, all participants who completed the survey at least up to the knowledge gaps survey questions and did not miss any baseline covariates were included in the analyses for knowledge gaps (12 236 participants, including 7522 Black and 4714 Latinx individuals), and all participants who completed the entire survey and did not have missing baseline covariates were included in the rest of the analysis (11 694 participants, including 7174 Black (61.3%) and 4520 Latinx individuals (38.7%) (Appendix Figures 1 to 3, available at Annals.org). The target sample size of 15 000 was not reached because of difficulty recruiting participants in selected demographic quotas, particularly men older than 65 years.
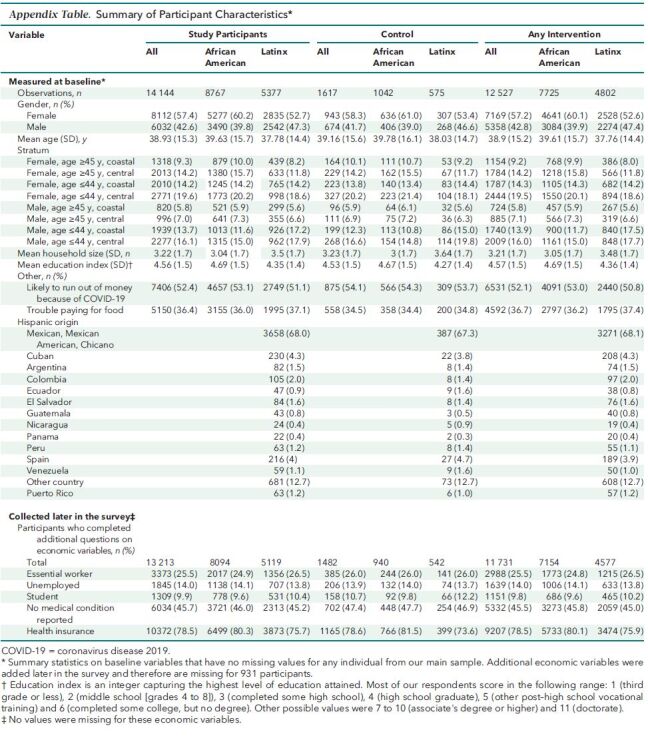
Summary statistics on the sample that was randomized are shown in the Appendix Table (available at Annals.org). Our final sample was 57.4% female (60.1% among Black participants). The mean age was almost 40 years. In total, 52.4% of participants reported being likely to run out of money because of COVID-19 and 36.4% reported difficulty paying for food. In addition, 25.5% were essential workers, 14% were unemployed and looking for work, and 9.9% were students. Finally, 54.3% reported a medical condition which placed them or a person close to them at higher risk from COVID-19 and 78.5% reported having health insurance. Most of the Latinx respondents were of Mexican origin (68%).
Appendix Table. Summary of Participant Characteristics*.
Baseline covariates were balanced across all intervention arms (Section E of the Supplement and Supplement Table 5, available at Annals.org). Similarly, baseline covariates restricting to participants who did complete the study are also balanced across intervention arms (Supplement Table 5).
Attrition
Because of the online nature of the survey, participants could exit at any point after watching the video messages, but without finishing the survey. The knowledge gaps outcome was measured early in the survey. Thus, when analyzing effects of the intervention on knowledge gaps, we include all participants who completed the survey at least up to that outcome. At that stage, 1908 participants included in the initial randomization and who had not missed any baseline question were excluded (5.7% attrition in the control group and 14.5% attrition in any video group). The information seeking behavior outcome was measured at the end of the survey, when attrition was higher, especially in the intervention group which had gone through a longer study (because they watched the videos) so 2450 participants were excluded (10.3% attrition in the control group and 18.2% attrition in the intervention group). However, attrition probability did not differ across arms (Appendix Figures 1 to 3).
Effects of Any Video Message Intervention Versus Control
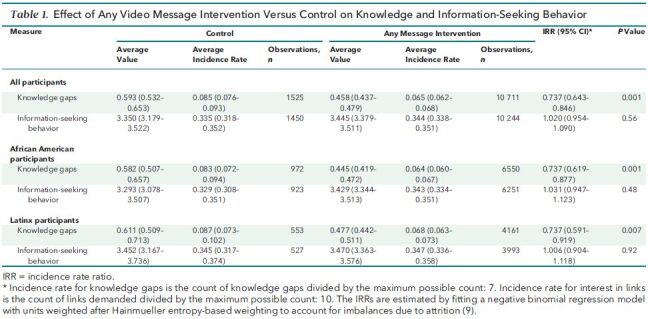
Table 1 shows the effect of receiving any video on knowledge gaps and information seeking behavior. Individuals in the control group had on average 0.6 out of 7 possible knowledge gaps, for a knowledge gap incidence rate of 0.085. Individuals who saw any video had an average 0.5 knowledge gaps (incidence rate, 0.065). Thus, seeing any video had a significant effect on reducing knowledge gaps relative to the control (estimated incidence rate ratio [IRR, 0.737 [95% CI, 0.643 to 0.846]; P < 0.001).
Table 1. Effect of Any Video Message Intervention Versus Control on Knowledge and Information-Seeking Behavior.
The Figure shows the effect of any intervention on the distribution of knowledge gaps. In the control group, 72.7% participants had no gap in knowledge at all (they answered all questions correctly). The proportion increased to 80.3% among participants who received any intervention. Supplement Table 6 (available at Annals.org) reports the result of a logistic regression of “any gap in knowledge” and confirms the significant decline in the fraction of participants with any gap in knowledge.
Figure. Distribution of knowledge gap scores in the control group and among participants who received any intervention.
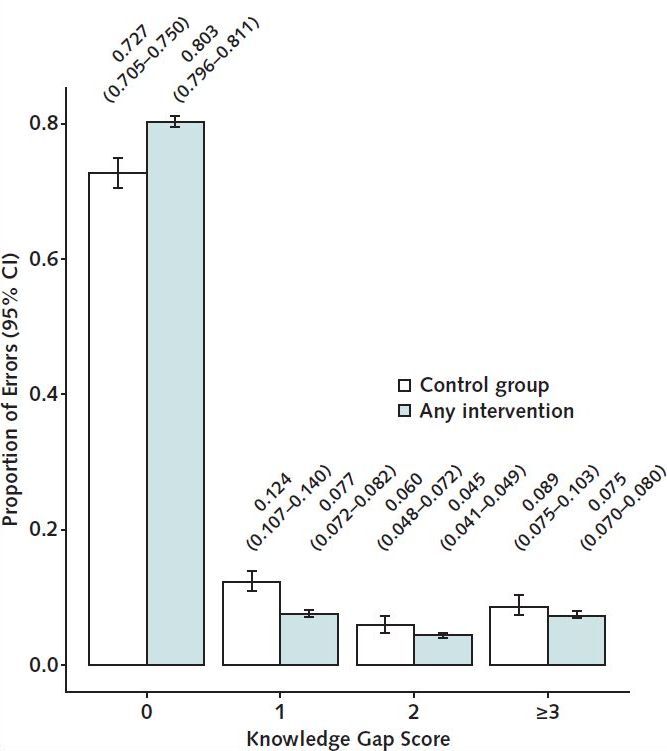
Bars indicate 95% CIs. A Kolmogorov–Smirnov test of the equality of the distribution resulted in a value of 0.07598 (P < 0.001).
The decline in knowledge gap was distributed across all levels. Participants in the intervention group were less likely than those in the control group to have 1 gap (7.7% versus 12.4%, respectively), 2 gaps (4.5% versus 6.4%), or 3 gaps or more (7.5% versus 8.9%). A Kolmogorov-Smirnov test confirmed that the distribution of knowledge gap in the control group first order stochastically dominates the distribution in the intervention group (P < 0.001).
In contrast, information-seeking behavior did not change significantly. The incidence rate of interest in links was 0.335 (that is, 3.35 links demanded out of 10 possible) in the control group and 0.344 in the intervention group. The estimated IRR of link demand is 1.02 (CI, 0.954 to 1.090) (P > 0.56) (Supplement Table 6, available at Annals.org, confirmed with the outcome “any link demanded”).
These results were very similar for Black and Latinx participants.
Effects of Race-Concordant Physicians
Concordance did not affect knowledge retention (Tables 2 and 3 and Supplement Table 7 and Table 8, available at Annals.org). However, assignment to a race-concordant physician increased our measure of information-seeking behavior. In the intervention sample, the incidence rate of link demand was 0.336 with a discordant physician and 0.353 with a concordant physician (IRR, 1.051 [CI, 1.003 to 1.102]; P = 0.037). The effect was significant for Black participants (IRR, 1.085 [CI, 1.022 to 1.153]; P = 0.007), although the absolute difference remained relatively small. There was no statistically significant effect on Latinx participants (IRR, 0.999 [CI, 0.927 to 1.077]; P = 0.98). The same conclusions were reached when the discrete variables for “any gap in knowledge” and “any link” were used.
Table 2. Effects of Tailoring Messages on Knowledge and Information-Seeking Behavior: Average Incidence Rates by Intervention*.
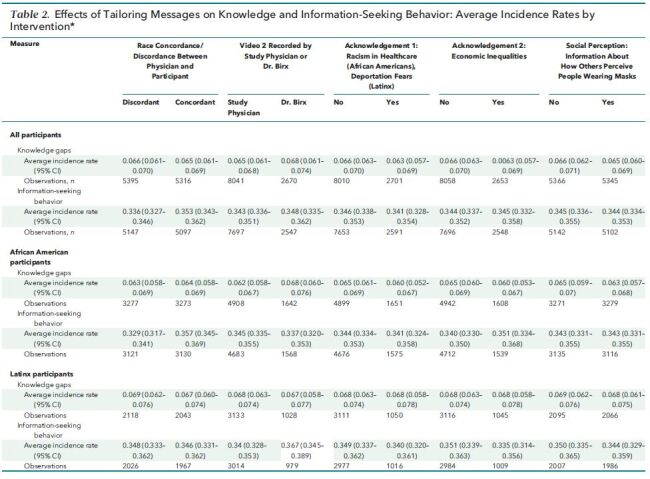
Table 3. Effects of Tailoring Messages on Knowledge and Information-Seeking Behavior: Incidence Rate Ratios Associated With Video Tailoring*.
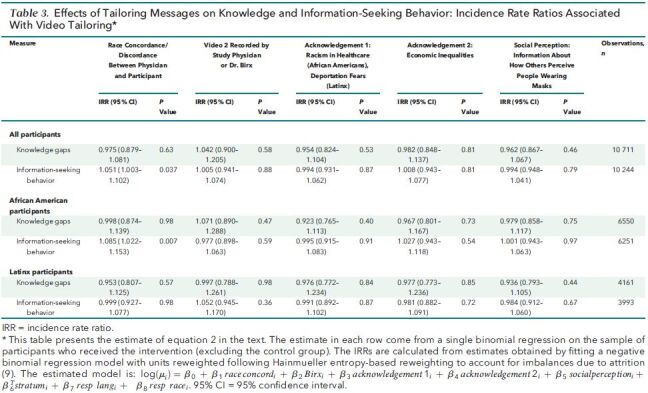
Effects of Acknowledgement of Injustice and Economic Hardship and the Dr. Birx Video
There was no further effect of tailoring the message according to each community for either Black or Latinx participants (Tables 2 and 3 and Supplement Table 7 and Table 8). Random assignment to the message recorded by Dr. Birx, to a message including acknowledgements of racism or deportation fears, or to a message acknowledging economic inequality did not affect knowledge gaps or information-seeking behavior, either overall or for Black or Latinx participants separately. However, Black participants spent less time viewing the video recorded by Dr. Birx than the equivalent video recorded by our study physicians, and they rated it lower.
Effects of Addressing the Fear of Stigma and Racism When Wearing a Mask
In video 3, randomly selected participants were informed that, in a survey, 8 out of 10 respondents believed that an Black (or Latinx) individual wearing a mask was protecting their community. This intervention had no effect on knowledge gaps or information-seeking behavior (Tables 2 and 3 and Supplement Table 7 and Table 8, available at Annals.org). Yet, there is evidence that information was retained and belief about social perception of mask-wearing shifted: Supplement Table 4 (available at Annals.org) shows that this intervention had the predicted effect on beliefs. Those who initially underestimated the proportion of people with a positive image of mask-wearing changed their perception toward believing that more people had a positive image of mask-wearing, and vice versa for those who initially overestimated this proportion. However, this updating of the social norm did not translate into changes in information-seeking behavior, even among those whose perception of mask-wearing became more favorable.
Heterogeneity by Sex and by Education
Across all conditions, there were no statistically significant differences by sex within race/ethnicity (Supplement Table 9, available at Annals.org). The effect of any intervention relative to control on knowledge gaps was more pronounced for participants with more than a high school education (Supplement Table 10, available at Annals.org). The incidence rate of knowledge gaps was reduced from 0.091 to 0.077 among participants with at most high school education (IRR, 0.811 [CI, 0.685 to 0.96]) and from 0.073 to 0.048 among more educated participants (IRR, 0.608 [CI, 0.482 to 0.767]). The difference in IRR between the 2 groups is statistically significant (P = 0.049). There is no significant difference by education in effects on information-seeking behavior.
We replicated the main analysis in 2 sensitivity analyses that controlled for additional baseline covariates (Supplement Table 11 and Table 12, available at Annals.org) and that did not apply weights to address possible bias from nonrandom attrition (Supplement Table 5 and Table 6, available at Annals.org). Results were consistent with those of the primary analyses.
Additional outcomes listed in the preanalysis plan are reported in Supplement Table 1-Table 2-Table 3 (available at Annals.org).
Discussion
Random assignment of Black and Latinx participants to watch public health video messages recorded by a diverse set of physicians decreased knowledge gaps on COVID-19 symptoms, preventive behaviors, and transmission. Although the level of knowledge was already relatively high at baseline (72.7% had no knowledge gap at all and 12.4% had a knowledge gap of 1), the effect on knowledge was modest but very clear (80.3% of participants receiving the intervention have no knowledge gap at all).
Tailoring the message to specific communities; racial/ethnic concordance of the physician; and acknowledgment of racism, fear of deportation, or economic inequality did not further increase the effectiveness of the messages. Replacing one message by doctors by a message from Dr. Birx of the White House COVID-19 Task Force did not change its effectiveness (although Black participants rated it lower).
Increased knowledge is only 1 step in affecting behavior and exposure to the disease, so the final clinical significance of these findings is uncertain. In general, physician-recorded video messages did not affect information-seeking behavior, as measured by interest in learning more about social distancing strategies, hygiene practices, or how to make a mask. Information on the social acceptability of masks also did not affect information-seeking behavior even among those who modified their beliefs. However, for Black participants, assignment to race-concordant physicians increased information-seeking behavior, although the magnitude of that effect was small. Similar results were not found among Latinx participants. Tailoring the content of messages had no statistically significant effect on information-seeking behavior and did not offset the discordance gap for White physicians.
These findings accord with those of studies reporting a positive association between patient–physician racial/ethnic concordance and improved satisfaction or health outcomes (14, 15) and with those of a recent randomized trial performed in Oakland, California (16).
Our study has limitations. First, it was conducted online because field activities were paused for many institutions at the time. Participants thus may have been more likely to have Internet access and be interested in an online study than the average low-income Black or Latinx individual, although recruitment was focused on persons with less than a college education and the final sample appears to be economically disadvantaged.
Second, although information-seeking behavior was objectively measured, participants' preventive health behaviors were not directly observed. Outcomes were collected immediately after the intervention and thus may not be durable. Regarding alternative behavior measures, direct observation of physical distancing and hygiene might have been seen as surveillance and thus was eschewed. Moreover, even if information self-reported behaviors had been collected, it would have been challenging to interpret because immediately after the intervention, nationwide protests occurred following the murder of George Floyd and other unarmed Black persons by police.
Third, outcomes might be subject to social desirability bias. Respondents may have felt compelled to click on links the study provided, for example. However, this was less likely to affect knowledge gaps, and changes in information-seeking behavior change were observed only among Black participants who were randomly assigned to a race-concordant doctor. Furthermore, although the increases in knowledge and information-seeking behavior were statistically significant, the clinical significance of changes remains uncertain.
Finally, findings regarding the acknowledgement intervention may be specific to the period of the analysis (May 2020). Preventive behaviors may be easier to measure when COVID-19 restrictions have eased. The effect of tailoring messages may also vary depending on the political climate.
Despite these limitations, the findings provide evidence that, especially in a moment when a novel human-to-human virus is disproportionately affecting communities of color, a diverse physician workforce can be an effective channel to communicate life-saving information.
Our findings lay out several directions for future work. First, would similar video messages have larger or smaller effects as COVID-19 incidence fluctuates? Second, would tailored messaging be important as awareness of systemic racism is heightened? Might official statements from health organizations identifying systemic racism as a public health concern increase the effectiveness of messages tailored to each community? Might intersectionality (concordance across multiple self-reported identities) matter, and could other professional healthcare staff, not solely physicians, assist in providing trusted messages regarding COVID-19 to underserved communities? Finally, would the effect of physician messages be the same among White persons? Addressing such research questions will be crucial in guiding the policy response to the pandemic and other health conditions.
Supplementary Material
Footnotes
This article was published at Annals.org on 21 December 2020
* Drs. Alsan and Stanford contributed equally.
References
- 1. Garg S , Kim L , Whitaker M , et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458-464. [PMID: ] doi: 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Price-Haywood EG , Burton J , Fort D , et al. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534-43. [PMID: ] doi: 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and Racial/Ethnic disparities. JAMA. 2020;323:2466-7. [PMID: ] doi: 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alsan M , Stantcheva S , Yang D , et al. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw Open. 2020;3:e2012403. [PMID: ] doi: 10.1001/jamanetworkopen.2020.12403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Facher L. As Covid-19 devastates communities of color, the government's minority health experts are conspicuously quiet. Stat. 22 June 2020. Accessed at www.statnews.com/2020/06/22/covid-19-minority-health-experts-conspicuously-quiet/ on 29 July 2020.
- 6. McDonnell Nieto del Rio G. Doctors plead with Americans to take the virus surge seriously New York Times. Accessed at www.nytimes.com/live/2020/11/15/world/covid-19-coronavirus/doctors-plead-with-americans-to-take-the-virus-surge-seriously on 25 November 2020.
- 7. U.S. Census Bureau. 2018 population estimates by age, sex, race and Hispanic origin. 20 June 2019. Accessed at www.census.gov/newsroom/press-kits/2019/detailed-estimates.html on 19 June 2020.
- 8. Abdul Latif Jameel Poverty Action Lab (J-PAL). COVID-19 health messaging in underserved communities. Accessed at www.povertyactionlab.org/project/covid-19-health-messaging-underserved-communities on 22 December 2020.
- 9. Birx D. Dr. Birx: stay 6 feet away. YouTube. 6 April 2020. Accessed at www.youtube.com/watch?v=8p0u-d4f604&feature=youtu.be&ab_channel=TheWhiteHouse on 25 November 2020.
- 10. Directive Consulting. Why is click through rate important? Accessed at https://directiveconsulting.com/resources/glossary/click-through-rate/ on 19 June 2020.
- 11. Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Political Analysis. 2012;20:25-46.
- 12. Chernozhukov V, Chetverikov D, Demirer M, et al. Double/debiased machine learning for treatment and structural parameters. Econometrics Journal. 2018;21:C1-68.
- 13. Alsan M, Stanford FC, Banerjee A, et al. Replication data for: comparison of knowledge and intended behaviors following general COVID-19 public health messages and messages tailored for Black and Latinx communities: a randomized controlled trial. Harvard Dataverse. 2020. doi: 10.7910/DVN/CJPVOD [DOI] [PMC free article] [PubMed]
- 14. Meghani SH , Brooks JM , Gipson-Jones T , et al. Patient-provider race-concordance: does it matter in improving minority patients' health outcomes. Ethn Health. 2009;14:107-30. [PMID: ] doi: 10.1080/13557850802227031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hill AJ, Jones DB, Woodworth L. Physician-patient race-match reduces patient mortality. Posted 31 July 2018; last updated 21 August 2020. Accessed at https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3211276 on 9 December 2020.
- 16. Alsan M, Garrick O, Graziano G. Does diversity matter for health? Experimental evidence from Oakland. American Economic Review. 2019;109:4071-111. doi: 10.1257/aer.20181446
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.