Abstract
BACKGROUND:
Adherence to treatment is one of the major challenges in patients with HIV/ADIS. If the patients do not adhere, they will face recurrent consequences, such as disease progression. The aim of this study was to investigate the effect of information, motivation, and behavioral Skills (IMB) model on medication adherence, diet adherence, and physical activity in HIV/ADIS patients.
MATERIALS AND METHODS:
This interventional study was conducted on 122 patients with 20 years of age and over with HIV/AIDS in Kerman City, Iran, in 2018. A total of patients were selected by census method and categorized into the intervention and control groups. Later, a researcher-made questionnaire on IMB was used before and 3 months after the intervention to assess medication adherence, diet adherence, and physical activity .The intervention study consisted of at least 8 training sessions (90 min) over a 12-week period.
RESULTS:
In adherence to medication, information (P = 0.034) and personal motivation (P = 0.003) constructs and in adherence to diet, information (P = 0.025), personal motivation (P = 0.001), self-efficacy (P = 0.010), and skills (P = 0.011) were significantly different between the two groups after the intervention (P = 0.011). However, regarding the adherence to physical activity, no significant difference was found between the two groups after the intervention.
CONCLUSIONS:
The IMB model can be effective in promoting the diet adherence in HIV/AIDS patients. In this regard, more qualitative and quantitative studies are recommended on the adherence to medication and physical activity.
Keywords: Adherence, AIDS, HIV, model
Introduction
According to the World Health Organization (WHO), AIDS is the second leading cause of death in adolescents and young people worldwide.[1] By 2030, HIV is predicted to have the highest disease burden worldwide.[2] Currently, HIV is considered a chronic disease[3] and adherence to treatment is one of the major challenges in patients with chronic diseases. In the case that these patients do not adhere to treatment plans, they will suffer from severe consequences, such as disease recurrence and progression.[4,5] Based on the WHO definition, behavior performance of individuals, such as medication intake, diet observance, and physical activity in accordance with the recommendations made by the health-care providers is called treatment adherence.[5]
Medication adherence, diet adherence, and physical activity are examples of the treatment adherence.[6] A study in Kenya showed that <10% of HIV-positive people received medication treatment.[7] In Iranian cities of Tehran and Kerman, lack of adherence to medication treatment was 40.5% and 24.5% in HIV-positive patients, respectively.[8] Moreover, HIV/AIDS is associated with biological and social factors and changes people's ability to consume and receive food. These biological and social factors lead to inadequate food intake, malnutrition, and poor adherence to diet, which are among the major causes of mortality in HIV patients.[9] For many developing countries, incidence of HIV and malnutrition hampers the progress towards achieving the UN Millennium Development Goals.[10] In the United States, 15.4% of the HIV-positive population did not follow an appropriate diet.[11] The results of a study by Nzeagwu et al. showed that 44.3% of the HIV-positive people did not have good nutritional habits.[12] The association between diet and physical activity[13] as well as among physical activity, health, and quality of life were reported in the literature.[14] Morowatisharifabad and Mostafavi et al. indicated that physical activity was lower than the average level in HIV-positive individuals and other people.[15,16] Therefore, close attention should be paid to these patients’ physical activity along with their diet and medication diet.
To increase the effectiveness of behavioral interventions, behavioral theories have been developed on the importance of behavior change. One of the models widely considered in the field of adherence to medication is the information, motivation, and behavioral (IMB) model.[17,18] In IMB, information is a prerequisite for personal motivation. Personal motivation, social motivation, and risk perception are considered as the motivational prerequisites for learning the skills [Figure 1].[19] Alexander et al. found that behavioral skills significantly influenced the treatment adherence considering the mediated effects of information and motivation on treatment adherence.[17] High levels of information, motivation, and behavioral skills are among the strong predictors of treatment adherence among the HIV-positive patients.[20] The IMB model has been applied in changing the health behaviors,[21,22] adherence to medications in HIV-positive individuals,[17] antiretroviral therapy (ART) adherence based on information, motivation, and behavioral skills model among HIV-positive patients.[23] However, no study has ever evaluated treatment adherence status in HIV-positive patients using the IMB model in Iran. Hence, this study was conducted to answer this question: Can the IMB model promote treatment adherence among the HIV-positive patients?
Figure 1.
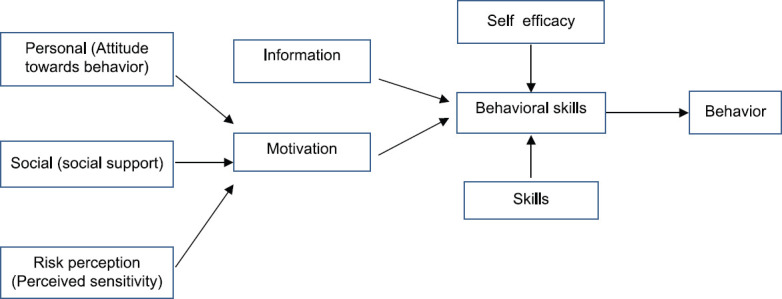
Schematic overview of the information, motivation, and behavioral model
Materials and Methods
This interventional study was carried out on HIV/AIDS patients with 18 years of age and over, who referred to the Behavioral Disease Counseling Center in Kerman City, Iran, in 2018.
Participants and sampling
The available sampling method was used and 183 eligible individuals with active records were selected. A total of 122 people participated in the study. In order to select the participants, questionnaires were distributed among the patients who referred to the Behavioral Disease Counseling Center for receiving counseling and medication services in different days of the week. The exclusion criteria were under 18 years and no medication. These individuals were categorized into the intervention and control groups randomly. The intervention group members attended the educational sessions conducted based on the IMB model, while the control group members received the routine services. After 3 months, the same questionnaire was administered as the follow-up. To determine the sample size, pre- and post-intervention adherence ratios of 5% and 75% reported in similar studies[24,25,26] were considered, respectively. Furthermore, 80% test power, 5% Type I error, and coverage of all study objectives were considered and the sample size was calculated as 61 individuals per group. Through the intervention process, four males due to addiction and two females due to family dissatisfaction did not continue the study. Hence, the research was conducted over the other participants after obtaining informed consent forms. Inclusion criteria were having 18 years and over, consuming antiviral medications for 6 months, and having willingness to participate in the study. The participants’ response rate was 66.67%.
Intervention
The intervention consisted of at least 8 training sessions (90 min per se ssion according to the participants) over a 12-week period on behavioral adherence to medication, nutrition, and physical activity using the IMB model for the intervention group. Every 2 weeks, phone calls were made to remind participants about adherence to the educational contents.
The first and second sessions were conducted using collaborative teaching method by patient friends, question-and-answer method, lecture-guided method, and using the Clinical Exercise Physiology 3rdEdition, ART-Adult, Medical Nutrition Therapy for HIV and AIDS guidelines. These two sessions were implemented within 1 week to raise the participants’ awareness. The third and fourth sessions were held to increase the participants’ motivation for 3 weeks. The motivational construct consisted of three parts: personal motivation, social motivation, and perceived sensitivity (perceived risk). In personal motivation, encouragement, determination of appropriate goals, SMS technology, and accuracy in sending messages at the right time (message timing control) were applied. In social motivation, participants were asked to mention the name of a supportive partner or good friend, who can solve their adherence problem. Given the low level of literacy of the target group in the risk perception construct, the scenario method was used by presenting statistics. The fifth, sixth, and seventh sessions were used to increase the behavioral skills over a period of 3 weeks including self-efficacy and objective behavioral skills. Regarding the self-efficacy section, the practical demonstration, group discussion (6–8 people), and group problem-solving methods were used. In the objective skill section, healthier role models and ability to tackle barriers to correct behavior were covered through MMS video message technology and development of stretch-and-flexibility training videos for HIV patients. Furthermore, we tried to use the self-monitoring method, in which each patient in the intervention group was provided with a daily calendar and asked to list the events leading to adherence and nonadherence. Later, the participants discussed about these factors and events with each other in the training sessions. The eighth session was conducted 1 month after the seventh session to follow-up the participants, review the covered issues, and solve patients’ possible problems in the adherence process.
Tools
To collect the required information, a researcher-made questionnaire was used, containing four parts. The first part consisted of the patients’ demographic and clinical information, including age, gender, marital status, education level, occupation, income level, number of children, housing, disease transmission type, CD4 level, disease stage, virus load, risk factors, disease history, and body mass index (BMI). The second was medication adherence, the next was diet adherence, and the final was physical activity.
Medication adherence questionnaire based on the information, motivation, and behavioral model
The IMB-based medication adherence questionnaire was designed by the researcher after conducting qualitative research and reviewing the related scientific articles and books to meet the research goals. The questionnaire consisted of six IMB model constructs based on a five-point Likert scale; information (6 items), personal motivation (9 items), social motivation (7 items), risk perception (5 items), self-efficacy (7 items), and skills (6 items). With regard to the information, personal motivation, social motivation, and risk perception constructs, selecting the options “totally agree” and “totally disagree” received 5 and 1 scores, respectively. In the self-efficacy and skills constructs, selecting the “always” and “never” options received 5 and 1 scores, respectively. Considering the information dimension, questions 5 and 6, the individual motivation dimension, questions 6, 7, 8, 9, the social motivation dimension, questions 3, 4, 5, 6, 7, and the skills dimension, question 6 were inversely scored. To determine the scientific validity of this tool, the experts’ professional opinions were collected and the questionnaire was revised accordingly. Validity of the questionnaire was higher than 85%. Cronbach's alpha test was also used to determine the scientific reliability of the data collection tool. Reliability of the questionnaire was confirmed in its all dimensions of information (82%), personal motivation (83%), social motivation (83%), risk perception (81%), self-efficacy (81%), and skills (81%).
Diet adherence questionnaire based on the information, motivation, and behavioral Model
This questionnaire consisted of six constructs based on a five-point Likert scale: information (7 questions), personal motivation (6 questions), social motivation (7 questions), risk perception (4 questions), self-efficacy (5 questions), and skills (6 questions). The options were “totally agree” and “totally disagree” received 5 and 1 scores, respectively. In the self-efficacy and skills constructs, selecting the “always” and “never” options received 5 and 1 scores, respectively. The reverse questions were also scored reversely in the IMB Model constructs. Validity of the questionnaire was higher than 76%. Cronbach's alpha test was also run to determine the scientific reliability of the data collection tools. Questionnaire reliability was confirmed with regard to its constructs: information (81%), personal motivation (82%), social motivation (81%), risk perception (82%), self-efficacy (81%), and skills (82%).
Physical activity adherence questionnaire based on the information, motivation, and behavioral model
The questionnaire consisted of six constructs based on a five-point Likert scale: information (6 questions), personal motivation (6 questions), social motivation (6 questions), risk perception (4 questions), self-efficacy (6 questions), and skills (6 questions). The options were “totally agree” and “totally disagree” received 5 and 1 scores, respectively. In the self-efficacy and skills constructs, selecting the “always” and “never” options received 5 and 1 scores, respectively. The reverse questions were also scored reversely in the IMB model constructs. Validity of the questionnaire was higher than 80%. Cronbach's alpha test was run to determine the scientific reliability of the data collection tools. The questionnaire reliability was confirmed with regard to all its constructs: information (76%), personal motivation (76%), social motivation (77%), risk perception (76%), self-efficacy (77%), and skills (77%).
Data collection and ethical consideration
After obtaining the code of ethics from the Ethics Committee of Yazd University of Medical Sciences (IR. SSU. SPH. REC 1396.83), it is also has been approved in the Iranian Registry of Clinical Trials with number IRCT20181112041616N1. Researchers obtained the list of eligible individuals by referring to the Behavioral Diseases Counseling Center, Kerman, Iran. Prior to sampling, participants were provided with explanations about the study purpose and informed consent forms were obtained from them. Furthermore, they were ensured about confidentially of information. In order to achieve the patients’ higher satisfaction, female and male colleagues were asked to complete the questionnaires for female and male patients, respectively. Due to the high stigma of the disease, those who did not wish to complete the questionnaires at the counseling center were allowed to complete the questionnaire at home and deliver the complete questionnaire to the center head or researcher after 1 week. In order to have more precise answers in completing the questionnaires, each participant was paid $3. Finally, all questionnaires were returned. Sampling lasted from August 23, 2017, to March 11, 2018.
Statistical analysis
Descriptive statistics (frequency, percentage, mean, and standard deviation) were used to describe the study population with regard to general characteristics, medication adherence, diet adherence, and physical activity. Independent t-test was run to compare the mean and standard deviation of adherence to medication, adherence to diet, and physical activity according to the parametric conditions. Finally, SPSS version 25 made by SPSS Company in Stanford University of Chicago, USA was run for data analysis.
Results
A total of 122 HIV/ADIS patients with a mean age of 41.88 ± 9.46 years participated in the study. Of all participants, 53.3% were male, 46.7% were married, 36.9% had diploma or higher education levels, 54.1% were unemployed, 33.6% had no children, and the rest had at least one child. Furthermore, 41.8% of the participants had an income of more than 48 $. As shown in Table 1, the disease was transmitted by sex in 37.7% of individuals, BMI was normal in 46.7% of patients, and the CD4 level was higher than 350 in 59% of participants. According to the findings, 93.4% of the participants had HIV, the viral load was < 100 in 63.9% of patients, and 41.8% of them did not mention risk factors such as substance use. The mean BMI was also calculated as 23.5 ± 5.49 [Table 1].
Table 1.
Clinical information of the participants
| Variable | n (%) |
|---|---|
| Disease transmission from | |
| Sexual intercourse | 46 (37.7) |
| Injection | 29 (23.8) |
| I do not know | 27 (22.1) |
| Others | 20 (16.4) |
| BMI | |
| Normal (18.5-24.9) | 57 (46.7) |
| Less than normal (<18.5) | 13 (10.7) |
| More than normal (more than 24.9) | 52 (42.6) |
| CD4 count | |
| <100 | 11 (9) |
| 101-200 | 16 (13.1) |
| 201-350 | 23 (18.9) |
| Higher than 350 | 72 (59) |
| Disease stage | |
| HIV | 114 (93.4) |
| AIDS | 8 (6.6) |
| Viral load | |
| <100 | 78 (63.9) |
| 100 and higher | 44 (36.1) |
| Risk factor | |
| No | 51 (41.8) |
| Yes | 71 (58.2) |
| Disease history | |
| <5 years | 37 (30.3) |
| 5-10 | 37 (30.3) |
| 10-15 | 20 (16.4) |
| 15 and higher | 28 (23) |
HIV=Human immunodeficiency viruses, BMI=Body mass index
The mean adherence to medication diet in all constructs was higher in the intervention than the control groups. However, significant difference was observed between the two groups considering their medication information and personal motivation after the intervention [Table 2].
Table 2.
Mean and standard deviation of medication adherence in the two study groups based on information, motivation, and behavioral skills model
| Stage | Variable | Mean (SD) | F | Test statistics | P | |
|---|---|---|---|---|---|---|
| Intervention group | Control group | |||||
| Preintervention | Information | 20 (0.64) | 20.93 (0.63) | 0.005 | −1.02 | 0.306 |
| Personal motivation | 22.85 (0.54) | 21.90 (0.58) | 1.37 | 1.19 | 0.236 | |
| Social motivation | 24.42 (0.58) | 24.85 (0.53) | 0.50 | −0.539 | 0.591 | |
| Risk perception | 16 (0.41) | 16.93 (0.40) | 0.42 | −1.61 | 0.109 | |
| Self-efficacy | 24.27 (0.80) | 24.37 (0.72) | 0.38 | −0.091 | 0.928 | |
| Behavioral skills | 23.80 (0.57) | 24.37 (0.54) | 0.006 | −0.723 | 0.471 | |
| Postintervention | Information | 24.20 (0.52) | 22.64 (0.50) | 0.01 | 2.15 | 0.034 |
| Personal motivation | 24.71 (0.62) | 22.16 (0.57) | 0.03 | 2.99 | 0.003 | |
| Social motivation | 25.57 (0.41) | 24.60 (0.48) | 1.08 | 1.53 | 0.128 | |
| Risk perception | 17.10 (0.39) | 16.39 (0.45) | 2.44 | 1.19 | 0.237 | |
| Self-efficacy | 27.11 (0.54) | 25.89 (0.73) | 4.24 | 1.35 | 0.179 | |
| Behavioral skills | 25.23 (0.35) | 24.21 (0.50) | 5.42 | 1.66 | 0.099 | |
The mean of diet adherence in all constructs was higher in the intervention than the control group. However, a significant difference was found between the two groups in terms of information, personal motivation, self-efficacy, and skills after intervention [Table 3].
Table 3.
Mean and standard deviation of diet adherence in the two study groups based on the information, motivation, and behavioral skills model
| Stage | Variable | Mean (SD) | F | Test statistics | P | |
|---|---|---|---|---|---|---|
| Intervention group | Control group | |||||
| Preintervention | Information | 19.16 (0.77) | 17.26 (0.86) | 0.13 | 1.62 | 0.106 |
| Personal motivation | 19.44 (0.57) | 18.44 (0.48) | 0.48 | 1.32 | 0.188 | |
| Social motivation | 18.49 (0.60) | 18.54 (0.45) | 0.58 | −0.065 | 0.948 | |
| Risk perception | 14.16 (0.47) | 14.36 (0.43) | 0.49 | −0.305 | 0.761 | |
| Self-efficacy | 15.22 (0.69) | 15.52 (0.67) | 0.21 | −0.306 | 0.760 | |
| Behavioral skills | 11.81 (0.57) | 11.49 (0.60) | 0.03 | 0.392 | 0.696 | |
| Pos intervention | Information | 21.50 (0.53) | 19.25 (0.85) | 3 | 2.26 | 0.025 |
| Personal motivation | 22.25 (0.53) | 19.57 (0.48) | 0.02 | 3.72 | 0.001 | |
| Social motivation | 18.83 (0.48) | 19.05 (0.50) | 2.88 | −0.31 | 0.752 | |
| Risk perception | 15.37 (0.50) | 14.85 (0.44) | 2.39 | 0.760 | 0.449 | |
| Self-efficacy | 18.71 (0.71) | 16.07 (0.71) | 0.04 | 2.60 | 0.011 | |
| Behavioral skills | 14.52 (0.65) | 12.08 (0.67) | 2.01 | 2.58 | 0.011 | |
The mean adherence to physical activity in all constructs was higher in the intervention than the control group. However, no significant difference was observed between the two groups in terms of the model constructs after intervention [Table 4].
Table 4.
Mean and standard deviation of adherence to physical activity in the two study groups based on the information, motivation, and behavioral skills model
| Stage | Variable | Mean (SD) | F | Test statistics | P | |
|---|---|---|---|---|---|---|
| Intervention group | Control group | |||||
| Preintervention | Information | 19.42 (0.55) | 18.62 (0.59) | 0.40 | 0.986 | 0.326 |
| Personal motivation | 20.47 (0.43) | 20.18 (0.50) | 3.83 | 0.441 | 0.660 | |
| Social motivation | 22.14 (0.57) | 20.47 (0.51) | 4.80 | 2.16 | 0.032 | |
| Risk perception | 14.16 (0.47) | 14.36 (0.43) | 0.49 | −0.305 | 0.761 | |
| Self-efficacy | 13.43 (0.53) | 13.62 (0.57) | 0.06 | −0.354 | 0.724 | |
| Behavioral skills | 20.18 (0.47) | 18.93 (0.49) | 1.13 | 1.82 | 0.070 | |
| Postintervention | Information | 27.33 (0.58) | 26.01 (0.77) | 2.58 | 1.37 | 0.173 |
| Personal motivation | 22.15 (0.49) | 20.71 (0.54) | 1.62 | 1.95 | 0.053 | |
| Social motivation | 22.40 (0.70) | 21.33 (0.62) | 0.003 | 1.13 | 0.260 | |
| Risk perception | 16.49 (0.43) | 15.60 (0.48) | 0.59 | 0.125 | 0.176 | |
| Self-efficacy | 16.62 (0.53) | 16.07 (0.65) | 0.01 | 0.834 | 0.508 | |
| Behavioral skills | 20.22 (0.38) | 19.35 (0.52) | 0.11 | 0.159 | 0.185 | |
Discussion
The results of our study revealed inconsistencies in efficacy of the IMB model on adherence; the IMB model was effective on diet adherence, but did not function well in adherence to medication and physical activity. The nonsignificant change in adherence to medication diet after intervention in both the groups could be due to the follow-up and special attention of the Behavioral Disease Counseling Center to medication status of all patients.
In the present study, the level of information and personal motivation increased after intervention regarding both diet and medication adherence. However, in the study by Gavgani et al., increase of information enhanced personal and social motivations.[27] Results of the studies conducted by Shirley et al.,[28] Karimi et al.,[29] Rongkavilit et al.,[18] and Khorsandi et al.[30] were consistent with the present research, so that adherence to the treatment recommendations was accompanied by increase of information. Thus, recent findings provide an opportunity for the health-care providers to render in-depth training services to the population with poor treatment adherence. We found that the IMB model was not effective on adherence to physical activity in the present study. However, Webel et al.[31] and Aweto et al.[32] reported that the personal motivation increased in HIV-positive patients after exercise intervention, so that exhaustion reduced by 17% in the intervention group. The application of self-assessment questionnaire and differences in the administered questionnaires can justify the discrepancies in the results.
Although social motivation is the most common stimulus for continuing a behavior,[33] social motivation did not increase in any components of the treatment adherence after intervention in the present research. Shirley et al.[33] noted that many participants emphasized the influence of social motivation as the most important stimulus for smoking, but HIV-positive patients had to deal with many problems such as stigma, discrimination, and shame.[34,35] In other words, the Iranian culture of silence about HIV requires the individuals to avoid talking about HIV with regard to the context of religious issues in the community.[36]
Therefore, as other studies emphasized the importance of stigma and discrimination in HIV-positive patients, our results can provide a platform for health policy makers to adopt effective interventions in eliminating stigma and discrimination in these patients. In addition, having the behavior motivation and risk perception can affect the behavioral skills and preventive behaviors.[37] In our study, risk perception did not increase in any of the adherence constructs. Given the high importance of risk perception in different studies[38,39,40] and their emphasis on the great impact of risk perception on the adherence to treatment, risk perception seems to be one of the effective factors on adherence. Therefore, health care providers to patients with HIV should be provided with specific information about the risks caused by nonadherence to treatment. Consequently, care providers should inform the patients about the involved risks.
In the present study, self-efficacy and behavioral skills were identified as the strongest predictors of adherence to behavior only in the diet adherence section, which is consistent with the studies carried out by other researchers.[41,42,43] However, this finding was contrary to the results reported by Barroso and Voss[43] The inconsistency in the findings may be due to the studied model and target population.
Azimi[44] found that information and motivation were identified as strong predictors of self-efficacy and appropriate behavior, but in the present study, information and motivation of the medication use were not identified as drivers of medication adherence behavior. These findings suggest that the IMB model acts differently in each disease, so that adherence to physical activity was effective among patients with diabetes[27] and also effective in predicting use of condom.[45] However, it had no effect on HIV-positive patients in adherence to physical activity. Limitations of the present study included selection of the participants from a specific center and use of a self-assessment questionnaire.
Recommendations for practice and research
We suggest other researchers and health-care providers to use the IMB model in their interventional studies. Policy makers and health-care providers are also recommended to consider social support and adherence to physical activity in HIV-positive patients
Limitation
One of the limitations in the present study was lack of access to patient files that we selected census method.
Conclusions
We found that IMB-based educational interventions that incorporate information, motivation, and behavioral skills enhancement strategies can be effective in helping HIV-positive patients to follow a diet. However, the effect of IMB model was not confirmed on these patients’ adherence to medication and physical activity. Therefore, more qualitative and quantitative studies are required to identify the types of information and effective motivation in forming favorable health behaviors in HIV-positive patients and individuals with other chronic diseases.
Financial support and sponsorship
My article has been derived from a thesis research project in Yazd University of Medical Science.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge authorities of the Behavioral Disease Counseling Center in the southern Iran.
References
- 1.World Health Organization. Health for the World's Adolescents: A Second Chance in the Second. Decade: Summary World Health Organization; 2014. [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao Y, Kraft JC, Yu D, Ho RJY. Recent developments of nanotherapeutics for targeted and long-acting, combination HIV chemotherapy. Eur J Pharm Biopharm. 2019;138:75–91. doi: 10.1016/j.ejpb.2018.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gholamaliei B, Karimi-Shahanjarini A, Roshanaei G, Rezapour-Shahkolaei FJ. Medication adherence and its related factors in patients with type ii diabetes. J Educ Community Health. 2016;2:3–12. [Google Scholar]
- 5.Masror Roudsari D, Dabiri Golchin M, Haghani H. Relationship between adherence to therapeutic regimen and health related quality of life in hypertensive patients. Iran J Nurs. 2013;26:44–54. [Google Scholar]
- 6.Masoudnia E, Foroozannia K, Montazeri M. Relationship between perceived social support and adherence to medical advices among patients with coronary heart disease after by-pass surgery. J Shahid Sadoghi Univ Med Sci Health Serv. 2012;19:798–806. [Google Scholar]
- 7.Elul B, Basinga P, Nuwagaba-Biribonwoha H, Saito S, Horowitz D, Nash D, et al. High levels of adherence and viral suppression in a nationally representative sample of HIV-infected adults on antiretroviral therapy for 6, 12 and 18 months in Rwanda. PLoS One. 2013;8:e53586. doi: 10.1371/journal.pone.0053586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morowatisharifabad MA, Movahed E, Farokhzadian J, Nikooie R, Hosseinzadeh M, Askarishahi M, et al. Antiretroviral therapy adherence and its determinant factors among people living with HIV/AIDS: A case study in Iran. BMC Res Notes. 2019;12:162. doi: 10.1186/s13104-019-4204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colecraft EJ, Pot NS. HIV/AIDS: Nutritional implications and impact on human development. Proc Nutr Soc. 2008;67:109–13. doi: 10.1017/S0029665108006095. [DOI] [PubMed] [Google Scholar]
- 10.Karimi I, Kasaeeian N, Atayi B, Tayeri K, Zare M, Azadbakht LJ. Anthropometric indices and dietary intake in HIV-infected patients. Journal of Isfahan Medical School. 2010;28:1–10. [Google Scholar]
- 11.Coleman-Jensen A, Rabbitt MP, Gregory C, Singh A. Household Food Security in the United States in 2014. Washington, DC: United States Department of Agriculture; 2015. [Google Scholar]
- 12.Nzeagwu OC, Uwaegbute A. Nutrition-Related Behaviors and Nutritional Status of HIV Adult Patients, Advances in Nutrition. 2016;7:41A. doi.org/10.1093/advances/7.1.41A. [Google Scholar]
- 13.Ottevaere C, Huybrechts I, Béghin L, Cuenca-Garcia M, De Bourdeaudhuij I, Gottrand F, et al. Relationship between self-reported dietary intake and physical activity levels among adolescents: The helena study. Int J Behav Nutr Phys Act. 2011;8:8. doi: 10.1186/1479-5868-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tumusiime DK, Stewart A, Venter FWD, Musenge E. The effects of a physiotherapist-led exercise intervention on peripheral neuropathy among people living with HIV on antiretroviral therapy in Kigali, Rwanda. S Afr J Physiother. 2019;75:1328. doi: 10.4102/sajp.v75i1.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morowatisharifabad MA, Movahed E, Nikooie R, Farokhzadian J, Bidaki R, Askarishahi M, et al. Research m: Adherence to medication and physical activity among people living with HIV/AIDS. Iran J Nurs Midwifery Res. 2019;24:397. doi: 10.4103/ijnmr.IJNMR_205_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mostafavi F, Pirzadeh A. Physical activity among employee women based on transtheoretical model. J Educ Health Promot. 2015;4:81. doi: 10.4103/2277-9531.171792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexander DS, Hogan SL, Jordan JM, DeVellis RF, Carpenter DM. Adherence: Examining whether the information-motivation-behavioral skills model predicts medication adherence for patients with a rare disease. 2017;11:75. doi: 10.2147/PPA.S115272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rongkavilit C, Naar-King S, Kaljee LM, Panthong A, Koken JA, Bunupuradah T, Parsons JT. Applying the information-motivation-behavioral skills model in medication adherence among Thai youth living with HIV: A qualitative study. AIDS Patient Care STDs. 2010;24:787–94. doi: 10.1089/apc.2010.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher JD, Fisher WA, Shuper PA. Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass; 2009. The information-motivation-behavioral skills model of HIV preventive behavior; p. 21e63. [Google Scholar]
- 20.Horvath KJ, Smolenski D, Amico KR. An empirical test of the information-motivation-behavioral skills model of ART adherence in a sample of HIV-positive persons primarily in out-of-HIV-care settings. AIDS Care. 2014;26:142–51. doi: 10.1080/09540121.2013.802283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Starks TJ, Millar BM, Lassiter JM, Parsons JT. STDs: Preintervention profiles of information, motivational, and behavioral self-efficacy for methamphetamine use and HIV medication adherence among gay and bisexual men. AIDS Patient Care STDS. 2017;31:78–86. doi: 10.1089/apc.2016.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang SJ, Choi S, Kim SA, Song M. Intervention strategies based on information-motivation-behavioral skills model for health behavior change: A systematic review. Asian Nurs Res. 2014;8:172–81. [Google Scholar]
- 23.Morowatisharifabad MA, Movahed E, Nikooie R, Farokhzadian J, Bidaki R, Askarishahi M, et al. Antiretroviral therapy adherence based on information, motivation, and behavioral skills model and its association with depression among HIV-positive patients: Health promotion strategy towards the 909090 target. J Educ Health Promot. 2019;14:185. doi: 10.4103/jehp.jehp_42_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaihin R, Asatpibal N, Chitreechuer J, Grimes RM. Effect of an empowerment intervention on antiretroviral drug adherence in Thai Youth. Behav Med. 2015;41:186–94. doi: 10.1080/08964289.2014.911717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyon ME, Trexler C, Akpan-Townsend C, Pao M, Selden K, Fletcher J, et al. A family group approach to increasing adherence to therapy in HIV-infected youths: Results of a pilot project. AIDS Patient Care STDS. 2003;17:299–308. doi: 10.1089/108729103322108175. [DOI] [PubMed] [Google Scholar]
- 26.Safren SA, Bedoya CA, O'Cleirigh C, Biello KB, Pinkston MM, Stein MD, et al. Cognitive behavioural therapy for adherence and depression in patients with HIV: A three-arm randomised controlled trial. Lancet HIV. 2016;3:e529–38. doi: 10.1016/S2352-3018(16)30053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gavgani RM, Poursharifi H, Aliasgarzadeh A. Effectiveness of Information-Motivation and Behavioral skill (IMB) model in improving self-care behaviors & Hba1c measure in adults with type 2 diabetes in Iran-Tabriz. Procedia-Social and Behavioral Sciences. 2010;5:1868–1873. [Google Scholar]
- 28.Shirley D, Thibodeau L, Catz SL, McCoy K, Jorenby DE, Safdar N, et al. Cessation-related information, motivation, and behavioral skills in smokers living with HIV. AIDS Care. 2018;30:131–9. doi: 10.1080/09540121.2017.1367088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karimi Z, Majlesi F, Tol A, Rahimi Foroushani A, Sahaf R, Ali Gol M, et al. The Effect of educational intervention on the promotion of physical activities of the elderly men in Qom city. Appl Trans Theor Model. 2015;10:182–91. [Google Scholar]
- 30.Khorsandi M, Fekrizadeh Z, Roozbahani N. Investigation of the effect of education based on the health belief model on the adoption of hypertension-controlling behaviors in the elderly. Clin Interv Aging. 2017;12:233–40. doi: 10.2147/CIA.S117142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Webel AR, Perazzo J, Decker M, Horvat-Davey C, Sattar A, Voss JJ. Physical activity is associated with reduced fatigue in adults living with HIV/AIDS. 2016;72:3104–12. doi: 10.1111/jan.13084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aweto HA, Aiyegbusi AI, Ugonabo AJ, Adeyemo TA. Effects of aerobic exercise on the pulmonary functions, respiratory symptoms and psychological status of people living with HIV. J Res Health Sci. 2016;16:17–21. [PMC free article] [PubMed] [Google Scholar]
- 33.Shirley DK, Kesari RK, Glesby MJ. STDs: Factors associated with smoking in HIV-infected patients and potential barriers to cessation. AIDS Patient Care and STDs. 2013;27:604–12. doi: 10.1089/apc.2013.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moodley A, Kagee AJ. Experiences of social support among persons seeking HIV testing. J Health Psychol. 2019;24:777–86. doi: 10.1177/1359105316685900. [DOI] [PubMed] [Google Scholar]
- 35.Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Ann Behav Med. 2012;43:362–71. doi: 10.1007/s12160-012-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Movahed E, Morowatisharifabad MA, Farokhzadian J, Nikooie R, Hosseinzadeh M, Askarishahi M, et al. Antiretroviral therapy adherence among people living with HIV: Directed content analysis based on information-motivation-behavioral skills model. Int Q Community Health Educ. 2019;40:47–56. doi: 10.1177/0272684X19858029. [DOI] [PubMed] [Google Scholar]
- 37.Cai Y, Ye X, Shi R, Xu G, Shen L, Ren J, et al. Predictors of consistent condom use based on the Information-Motivation-Behavior Skill (IMB) model among senior high school students in three coastal cities in China. BMC Infect Dis. 2013;13:262. doi: 10.1186/1471-2334-13-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jassempour K, Shirazi KK, Fararooei M, Shams M, Shirazi AR. The impact of educational intervention for providing disaster survival kit: Applying precaution adoption process model. Int J Disaster Risk Reduct. 2014;10:374–80. [Google Scholar]
- 39.Esmaili F, Tahmaseb R, Noroozi A, Vahdat K, Kavehie B. Impact of education for adherence to therapy based on health promotion model on the quality of life in HIV-infected Patients. Iran J Health Educ Promot. 2016;4:173–183. [Google Scholar]
- 40.Lee G, Yang SJ, Chee YK. Assessment of healthy behaviors for metabolic syndrome among Korean adults: A modified information-motivation-behavioral skills with psychological distress. BMC Public Health. 2016;16:518. doi: 10.1186/s12889-016-3185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez H, Palar K, Linnemayr S, Smith A, Derose KP, Ramirez B, et al. Tailored nutrition education and food assistance improve adherence to HIV antiretroviral therapy: Evidence from Honduras. AIDS Behav. 2014;18(Suppl 5):S566–577. doi: 10.1007/s10461-014-0786-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pirzadeh A, Mazaheri MA. The effect of education on women's practice based on the health belief model about pap smear test. Int J Prev Med. 2012;3:585–90. [PMC free article] [PubMed] [Google Scholar]
- 43.Barroso J, Voss JG. Fatigue in HIV and AIDS: An analysis of evidence. J Assoc Nurses AIDS Care. 2013;24:S5–14. doi: 10.1016/j.jana.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 44.Azimi H, Hosseini J, Mahmuodi G, Jannati Y. Mental Health Nursing. 2th ed. Tehran: Jameenegar Inc; 2014. [Google Scholar]
- 45.Kalichman S, Stein JA, Malow R, Averhart C, Dévieux J, Jennings T, et al. Predicting protected sexual behaviour using the Information-Motivation-Behaviour skills model among adolescent substance abusers in court-ordered treatment. Psychol Health Med. 2002;7:327–38. doi: 10.1080/13548500220139368. [DOI] [PMC free article] [PubMed] [Google Scholar]


