Abstract
Background
COVID-19 has affected the entire world. We aimed to determine the impact of COVID-19 containment measures on the daily life and follow up of patients with inflammatory bowel disease (IBD).
Methods
During May 2020, we evaluated 179 (79.6%) patients with Crohn’s disease (CD) and 46 (20.4%) with ulcerative colitis (UC) by telephone, using a structured questionnaire to gather information on social impact and IBD follow up.
Results
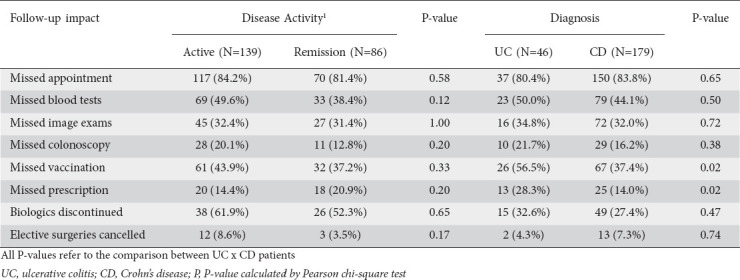
Some kind of social distancing measure was reported by 95.6% of our patients, self-quarantine (64.9%) being the most frequent. Depressive mood was the most prevalent social impact (80.2%), followed by anxiety/fear of death (58.2%), insomnia (51.4%), daily activity impairment (48%), sexual dysfunction (46.2%), and productivity impairment (44%). The results were similar when we compared patients with active disease to those in remission and patients with UC to those with CD. Analysis of IBD follow up showed that 83.1% of all patients missed an IBD medical appointment, 45.5% of the patients missed laboratory tests, 41.3% missed the national flu vaccination program, 31.3% missed any radiologic exam, 17.3% missed colonoscopy, and 16.9% failed to obtain biologic therapy prescriptions. Biologics were discontinued by 28.4% of the patients. UC patients had higher rates of missed vaccination than CD patients (56.5% vs. 37.4%, P=0.02) and more failures to obtain a biologic prescription (28.3% vs. 14.0%, P=0.02).
Conclusions
Our study reveals alarming social impacts and declining follow-up care for IBD patients during the COVID-19 outbreak. These findings may have implications for disease control in the near future.
Keywords: Inflammatory bowel disease, Crohn’s disease, ulcerative colitis, outcome assessment, healthcare
Introduction
In late December 2019, there were reports of pneumonia of unknown etiology by health authorities in Wuhan, China. In early January 2020, the causative agent was identified as a new coronavirus, called SARS-CoV-2 [1-3]. The virus causes COVID-19, a disease with a spectrum of clinical manifestations that range from a mild and self-limited disease of the respiratory tract (in 80-90% of cases) to severe acute pneumonia with dyspnea, hypoxemia and extensive radiological involvement (10% of cases). Up to 5% of severe cases may be complicated by acute respiratory distress syndrome, multiple organ failure, and even death [4-7]. The presence of preexisting comorbidities, such as hypertension, diabetes and cardiovascular diseases, is associated with worse clinical outcomes in patients with COVID-19, especially among elderly and frail patients [7-9].
The outbreak of COVID-19 has spread rapidly and now affects the entire world, with the number of new confirmed cases currently increasing every day [10,11]. COVID-19 may have implications for the management of patients with preexisting digestive diseases, including inflammatory bowel disease (IBD) [12].
A significant number of IBD patients with either Crohn’s disease (CD) or ulcerative colitis (UC) use immunosuppressives, biological therapy, and steroids during the course of their disease [13,14], and the potential risk of infectious complications attributed to these therapies within the context of IBD is well known. Additionally, malnutrition may occur, especially in CD patients [15]. Thus, there is a concern that IBD patients will have a greater risk of developing COVID-19, with an increased risk of progressing to a more severe clinical course or even death when compared to the general population. Nonetheless, despite the potentially greater risk of SARS-CoV-2 infection and COVID-19 complications due to immunosuppressive treatment, global records have shown that the risks of SARS-CoV-2 infection and the development of its severe forms in patients with IBD appear to be similar to those in the general population [16,17].
IBD patients often need to visit health facilities, either for medical appointments and tests or for treatment. This increased movement can definitely be a risk factor for SARS-CoV-2 infection and the development of COVID-19 [12]. Overall, IBD patients represent a challenge in the current pandemic scenario, in which increased exposure may be associated with a higher risk of infection and isolation may compromise rigorous follow-up requirements and predispose patients to IBD flares.
Currently, there is no specific drug treatment for COVID-19, and a vaccine is not available [18,19]. Treatment is based primarily on clinical supportive care. Furthermore, as COVID-19 spreads across the globe, unprecedented measures—such as the imposition of quarantines, travel restrictions, and social distancing, as well as the closure of commercial establishments and schools—to control disease dissemination have been adopted by the governmental authorities of several countries [19,20]. The purpose of these measures is to ensure the isolation of individuals, symptomatic and asymptomatic, and anyone who may have had contact with them to prevent transmission to others, family members and health professionals [18,19].
Data relating COVID-19 quarantine measures and IBD patients are scarce. Thus, the present study aimed to determine the impact of coronavirus containment measures on the daily life and follow up of IBD patients in a tertiary Brazilian IBD center.
Patients and methods
Study design and data collection
We conducted a cross-sectional study during May 18-22, 2020, 2 months after the quarantine decree in the state of Sao Paulo, which was issued on March 23, 2020. A personalized questionnaire was developed in a pilot study with 60 IBD patients 3 weeks after the beginning of the quarantine. An English translation is provided (supplementary data).
The first 4 parts of the questionnaire gather clinical and demographic information from the electronic medical records of IBD patients; the subjects were selected from a prospective database of 570 patients diagnosed with moderate-to-severe IBD who were being followed-up at the IBD unit of Ribeirao Preto Medical School, University of Sao Paulo (Ribeirao Preto, Sao Paulo, Brazil). In order to achieve a more homogeneous group, only adult patients (>18 years of age), receiving small-molecule or biological maintenance therapy, with clinical characterization of the disease in the last 3 months and assessment of the mucosa in the last year, were included in the study. These patients often need to visit health facilities for clinical evaluation or to receive medication. In CD and UC patients, clinical activity was measured with the Harvey-Bradshaw Index (HBI) and partial Mayo score, respectively. Clinical remission was defined as an HBI <5 or partial Mayo <2. Biochemical activity was defined as C-reactive protein (CRP) >5 mg/dL. Mucosal activity was defined by a simple endoscopic score (SES-CD) greater than 3 and/or any sign of luminal or transmural inflammation on magnetic resonance enterography in CD, or an endoscopic Mayo score of 0 or 1.
The last 2 parts were designed to evaluate the impact of the COVID-19 outbreak on IBD patients. First, we assessed whether patients had adopted social distancing measures and whether the outbreak impacted the following aspects of life: productivity, overall activity, sleep cycle, emotional status, sexual activity and anxiety. Finally, we investigated whether regular medical appointments, complementary exams, vaccination, medical therapy, and elective surgeries were compromised.
Statistical analysis
Categorical variables are expressed as absolute and relative frequencies. Continuous variables are expressed as mean ± standard deviation (SD). The Kruskal-Wallis test was used to check for normality of variables. Mean symptom and impact scores were compared among patients with and without deep remission, and statistical significance was calculated by ANOVA. SPSS version 20.0 software (SPSS, Chicago, IL, USA) was used. A P-value <0.05 was considered statistically significant.
Ethics approval
This study was approved by the Institutional Review Board and the Ethics Committee (HCFMRP-USP, CAAE nr. 31115320.4.0000.5440, 13th May 2020). All patients agreed to participate in the study, and informed consent was obtained from each patient included. All procedures were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the 1964 Helsinki declaration and its later amendments, or comparable ethical standards.
Results
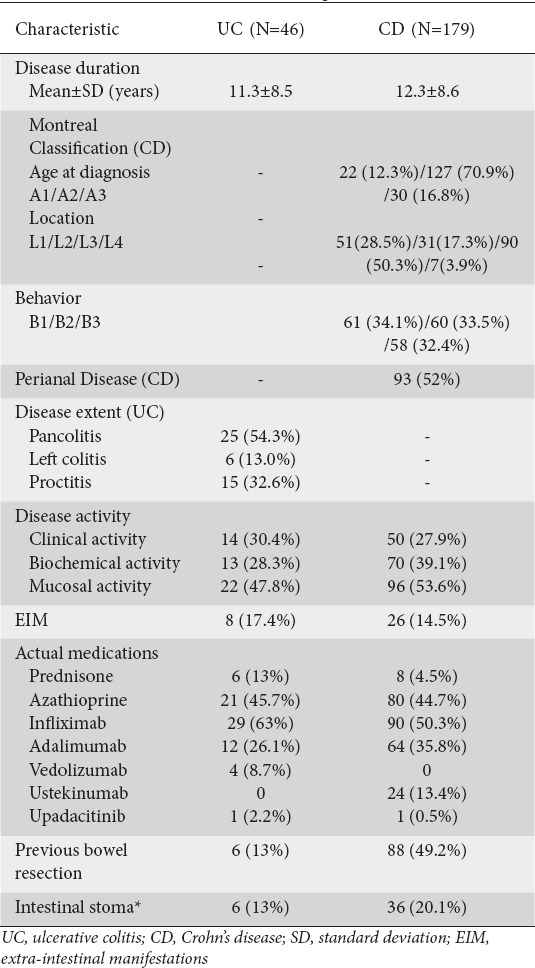
In total, 179 (79.6%) CD and 46 (20.4%) UC patients were included in the study. The baseline demographic and clinical characteristics of the participants are shown in Tables 1 and 2, respectively.
Table 1.
Baseline demographic characteristics of patients
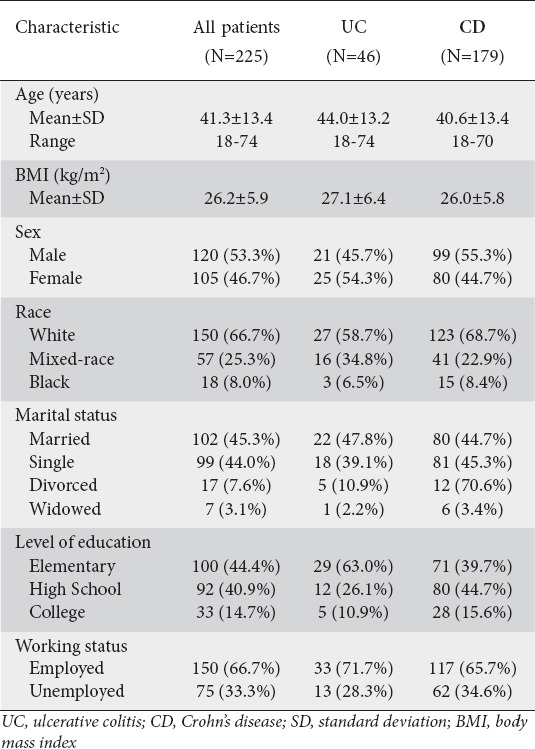
Table 2.
Baseline clinical characteristics of patients
After 1 month of the quarantine period decreed by the government, 4 (8.7%) patients with UC and 13 (7.3%) with CD developed a mild flu syndrome; however, none underwent COVID-19 testing, as they were completely asymptomatic at the time of the interview. A significant decrease in the number of medical appointments for IBD follow up was observed in our institution, as shown in Fig. 1.
Figure 1.
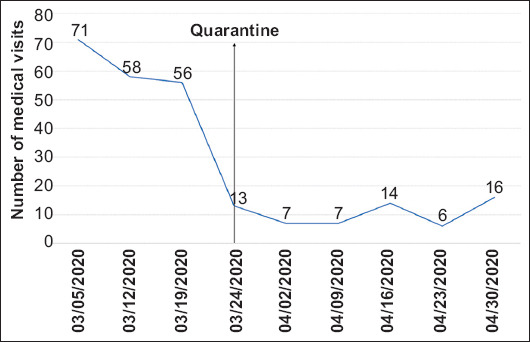
Number of inflammatory bowel disease-related medical appointments in our institution before and after the quarantine began
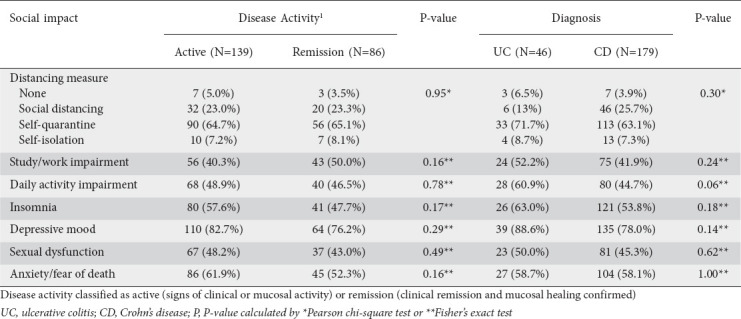
Regarding the impact of the COVID-19 outbreak, we noted that 95.6% of our patients followed some type of social distancing measure, of which self-quarantine was the most frequent (64.9% of all patients). Depressive mood was the most prevalent social impact (80.2%), followed by anxiety/fear of death (58.2%), insomnia (51.4%), daily activity impairment (48%), sexual dysfunction (46.2%) and productivity impairment (44%). The results were similar when we compared patients with active disease to those in remission and patients with UC to those with CD. The results are shown in Table 3.
Table 3.
Social and personal impact of COVID-19 quarantine measures according to disease activity and diagnosis
Analysis of IBD follow up indicate that 83.1% of all patients missed an IBD medical appointment. Specifically, we observed that 45.5% missed laboratory tests, 41.3% missed the national flu vaccination program, 31.3% missed any radiologic exam, 17.3% missed colonoscopy, and 16.9% failed to obtain biologic therapy prescriptions. Medical therapy was discontinued by 28.4% of the patients, who admitted that fear of infection was the main cause. Adalimumab was the most commonly discontinued medication (Table 4). Elective surgeries of 15 patients (6.7%) were canceled. However, the impact on follow up did not differ among patients with or without remission, though higher rates of missed vaccination and failure to obtain a biologic prescription were observed in UC patients. The results are provided in Table 5.
Table 4.
Rates of nonmedical discontinuation of biological or small-molecule therapy
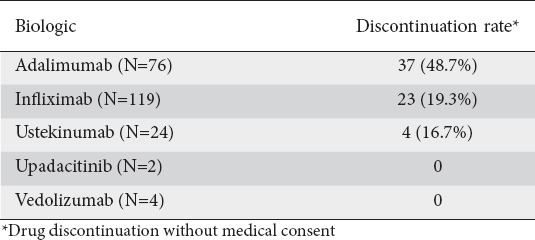
Table 5.
Impact of COVID-19 outbreak on inflammatory bowel disease follow up according to disease activity and diagnosis
Discussion
Our study showed that the COVID-19 outbreak had a negative impact on the quality of care and follow up of patients with IBD. Many patients developed depressive mood, anxiety, fear of death and insomnia, and some patients had daily activity impairment, sexual dysfunction and productivity impairment. We also demonstrated that the majority of patients missed IBD medical appointments; almost 1 in 3 patients discontinued medical therapy.
In São Paulo, the COVID-19 quarantine began on March 23, 2020. IBD patients were advised to stay at home, maintain proper distance from other people, wash hands with soap or alcohol-based sanitizers, and avoid touching facial mucosa, as was the general population [16,21-27]. Like other large institutions, our institute, one of the biggest in the state of São Paulo, with more than 1000 IBD patients, implemented a massive organizational plan to evacuate wards, equip intensive care units and provide sufficient beds for patients diagnosed with SARS-CoV-2 infection [28]. These rearrangements affected our IBD team, which is composed of surgeons, gastroenterologists, endoscopists, pediatricians, nurses, and nutritionists, as only oncologic or urgent procedures were authorized.
As in other IBD units, the great majority of appointments were rescheduled in our outpatient clinic [17,29]. We think that social distance measures are important to halt the spread of the COVID-19, though we attempted to maintain close monitoring in patients with complications or active disease. These measures surely explain the reduction in outpatient IBD visits from 70 to less than 20 per week.
Laboratory tests, radiologic exams and endoscopies were strictly limited as well, in accordance with international recommendations [30]. Although we are a reference center for IBD care, we do not have widely available fecal calprotectin tests. Therefore, unlike in other IBD units [28], ileocolonoscopy could not have been replaced by fecal calprotectin, even if deemed necessary.
During the first month of quarantine, our team called all IBD patients to inquire about clinical manifestations and infectious symptoms. Patients with respiratory symptoms were considered to have suspected COVID-19 and were treated according to international guidelines [29]. For patients in clinical remission, high-cost drug (biological and immunosuppressive therapy) prescriptions were renewed electronically and sent for dispensation at authorized pharmacies. The period for renewal of medical prescriptions was also extended. If IBD flares or complications were suspected, patients were invited to visit our unit for proper evaluation.
Despite a lack of adequate tools for assessing patient-reported outcomes during pandemics, our study showed that the COVID-19 outbreak had a high impact, as most patients were adhering some type of social distance measure, with almost half of the sample reporting impairment of their general activities and sex lives. Psychological distress is common in IBD patients [31]. Nevertheless, most people had psychological symptoms due to the COVID-19 outbreak.
Active IBD, especially among CD patients, is associated with a substantial impact on quality of life [32,33]. Curiously, our findings did not differ according to diagnosis (UC or CD) or disease status (active or remission), leading us to believe that the pandemic and its containment measures had an early and negative impact on patients regardless of their IBD phenotype.
Our study provides evidence for an alarming impact of COVID-19 quarantine measures on the follow up of IBD patients. More than 80% of IBD patients missed medical appointments, and many missed laboratory tests, endoscopies, flu vaccinations and elective surgeries. In addition, up to 1 in 4 patients lost access to their prescribed medication, and almost 1 in 3 patients discontinued medical therapies because of fear of infection and COVID-19 complications.
It is not known whether the lack of close monitoring due to social distancing measures can lead, in the short- or long-term, to higher rates of clinical relapse or loss of response to therapy. In general, there is a need to restructure the IBD unit, use telemonitoring [34,35], or send questionnaires to the patients through emails, mobile communication applications, and text messaging to monitor their progress and detect adverse events that could be missed in those who are not under closer monitoring [36]. This is an important consideration during the COVID-19 outbreak: namely, to detect patients who need immediate medical attention and those who may postpone their appointments.
More than 40% of patients missed flu vaccination. Although the incidence of influenza does not appear greater in IBD patients receiving immunomodulators, immunosuppression is generally considered to enhance the risk of severe or complicated influenza infection, while immunosuppressed patients with a laboratory diagnosis of influenza should receive timely treatment early in the course of the illness [37]. Vaccine utilization remains suboptimal in patients with IBD and can worsen during quarantine. Several reasons explain the low vaccination rates in the IBD population: they include lower education level, younger age or lack of recommendations. Inadequate immunization increases the risk of infectious diseases that might easily be avoided through a more rigorous and standardized vaccination program. Educational interventions may increase vaccination rates, and gastroenterologists can play a more active role in healthcare maintenance in patients with IBD by counseling patients on which vaccines to receive or avoid [38,39].
An important point to be discussed is the high rate of discontinuation of clinical therapy for nonmedical reasons. Several factors are responsible for the suspension of medical therapy during the quarantine period, including fear of immunosuppression, fear of contracting COVID-19 and difficulties in receiving the drug. Approximately half of IBD patients relapse within 2 years after discontinuation of anti-tumor necrosis factor (TNF) therapy [40,41], and even when deep remission is achieved, anti-TNF discontinuation is associated with a significant risk of relapse within 1-2 years [42,43]. More than 50% of the CD patients in our cohort had perianal CD, and approximately half of IBD patients were endoscopically active. The incidence rate of IBD relapse after anti-TNF discontinuation is relevant, especially in a moderate-to-severe IBD population with a high rate of perianal CD and without endoscopic remission [44,45].
Overall, IBD patient management presents a challenge during the current COVID-19 pandemic [46,47]. The primary focus should remain on keeping bowel inflammation controlled and encouraging medication adherence [16]. In our opinion, lack of awareness, the incorrect assumption that small-molecule or biological therapy cannot be safely administered to IBD patients during the COVID-19 outbreak, fear of side effects, and difficulty in consulting with the gastroenterologist might explain the lack of adherence. The overall available evidence suggests that IBD patients do not have an increased risk of developing COVID-19 and should stay on IBD medications. Active IBD, old age and comorbidities are associated with negative COVID-19 outcomes, whereas IBD treatments, except for corticosteroids, are not [48].
Preventing acute IBD flares may help patients avoid unnecessary exposure to possibly lethal COVID-19 [49]. Regardless, patients receiving immunosuppressors should be carefully monitored for the occurrence of symptoms and/or signs suggesting COVID-19 [50].
The vast majority of our patients had moderate-to-severe disease, as demonstrated by the high rates of perianal disease, previous surgeries, stoma presence, and long disease course. Some important questions must be considered regarding the current circumstances. Will there be more recurrence of moderate-to-severe IBD in the coming months or years due to social isolation and reduced patient monitoring? Will patients have higher rates of flu due to a lack of vaccination against influenza? Will the cancellation of elective surgeries and endoscopic exams have negative consequences for IBD patients? Finally, will there be an overcrowding of public health services in the future because most patients are not being seen at this time? We will only have answers to these questions in a few months or even 1-2 years after the follow up of these patients who were isolated during the COVID-19 outbreak. Nevertheless, chronic IBD patients undergoing long-term treatment on the one hand, and physical distancing measures on the other, will likely present a worsening challenge with regard to overcrowding in our outpatient facilities [25].
This study demonstrated the alarming magnitude of changes due to COVID-19 outbreaks in IBD patients at a referral center in Brazil. Nevertheless, limitations must be addressed. First, although a personalized questionnaire was developed in a pilot study after the beginning of the quarantine, we applied a non-validated questionnaire. However, there are currently no validated questionnaires, and the use of telemedicine will increase even during the COVID-19 outbreak; there is a need to adapt the patient treatment units to this new reality. Second, this was a cross-sectional, nonrandomized study and causal relationships could not be established, given the nature of the study, without a follow-up period. Finally, the sample of patients in the study included only those with moderate-to-severe disease receiving small-molecule or biological therapy. Hence, this cohort may not represent the IBD population of our city or state. However, the main purpose of this study was to evaluate patients who require more frequent evaluations and more rigorous care for IBD, and who require consultations or infusions regularly.
In summary, our study reveals alarming social impacts and declining follow-up care for IBD patients during the COVID-19 outbreak. These findings may have implications for disease control in the near future.
Summary Box.
What is already known:
COVID-19 has implications for the management of patients with preexisting digestive diseases, including inflammatory bowel diseases (IBD)
Data collected from IBD patients do not show any particular susceptibility to SARS-CoV-2 infection among patients on immunosuppressants or biologics
During the SARS-CoV-2 pandemic, all elective medical appointments, endoscopic procedures, and surgeries were postponed, and there are no current data regarding the impact of coronavirus containment measures on the daily life and follow up of IBD patients
What the new findings are:
COVID-19 outbreak had a negative impact on the quality of care and follow up of patients with IBD
Many patients developed depressive mood, anxiety, fear of death and insomnia, and some patients experienced daily activity impairment, sexual dysfunction, and productivity impairment
The majority of patients missed IBD medical appointments, and almost 1 in 3 patients discontinued medical therapy
Biography
Ribeirão Preto Medical School, University of São Paulo, Ribeirão Preto, State of São Paulo, Brazil
Footnotes
Conflict of Interest: None
References
- 1.Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure replication, and pathogenesis. J Med Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N, Zhang D, Wang W, et al. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan China. JAMA. 2020;17(323):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He F, Deng Y, Li W. Coronavirus disease 2019:What we know? J Med Virol. 2020;92:719–725. doi: 10.1002/jmv.25766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan Y, Yang Y, Wang F, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. 2020;8:e001343. doi: 10.1136/bmjdrc-2020-001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hulot JS. COVID-19 in patients with cardiovascular diseases. Arch Cardiovasc Dis. 2020;113:225–226. doi: 10.1016/j.acvd.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sohrabi C, Alsafi Z, O'Neill N, et al. World Health Organization declares global emergency:A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak:What we know. Int J Infect Dis. 2020;94:44–48. doi: 10.1016/j.ijid.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magro F, Abreu C, Rahier JF. The daily impact of COVID-19 in gastroenterology. United European Gastroenterol J. 2020;8:520–527. doi: 10.1177/2050640620920157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeong DY, Kim S, Son MJ, et al. Induction and maintenance treatment of inflammatory bowel disease:A comprehensive review. Autoimmun Rev. 2019;18:439–454. doi: 10.1016/j.autrev.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Cholapranee A, Hazlewood GS, Kaplan GG, Peyrin-Biroulet L, Ananthakrishnan AN. Systematic review with meta-analysis:comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn's disease and ulcerative colitis controlled trials. Aliment Pharmacol Ther. 2017;45:1291–1302. doi: 10.1111/apt.14030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirchgesner J, Lemaitre M, Carrat F, Zureik M, Carbonnel F, Dray-Spira R. Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases. Gastroenterology. 2018;155:337–346. doi: 10.1053/j.gastro.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Al-Ani A, Prentice R, Rentsch C, et al. Review article:prevention diagnosis and management of COVID-19 in the inflammatory bowel disease patient. Aliment Pharmacol Ther. 2020;52:54–72. doi: 10.1111/apt.15779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fiorino G, Allocca M, Furfaro F, et al. Inflammatory bowel disease care in the COVID-19 pandemic era:the Humanitas, Milan experience. J Crohns Colitis. 2020;16(14):1330–1333. doi: 10.1093/ecco-jcc/jjaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong:an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures and second-wave scenario planning:a modelling impact assessment. Lancet. 2020;395:1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kavanagh MM. Authoritarianism, outbreaks and information politics. Lancet Public Health. 2020;5:e135–e136. doi: 10.1016/S2468-2667(20)30030-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bodini G, Demarzo MG, Casagrande E, et al. Concerns related to COVID-19 pandemic among patients with inflammatory bowel disease and its influence on patients management. Eur J Clin Invest. 2020;50:e13233. doi: 10.1111/eci.13233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pasha SB, Fatima H, Ghouri YA. Management of inflammatory bowel diseases in the wake of COVID-19 pandemic. J Gastroenterol Hepatol. 2020;35:1449–1450. doi: 10.1111/jgh.15056. [DOI] [PubMed] [Google Scholar]
- 23.Rubin DT, Abreu MT, Rai V, Siegel CA International Organization for the Study of Inflammatory Bowel Disease. Management of patients with Crohn's disease and ulcerative colitis during the COVID-19 pandemic: results of an international meeting. Gastroenterology. 2020;159:6–13. e6. doi: 10.1053/j.gastro.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rubin DT, Feuerstein JD, Wang AY, Cohen RD. AGA Clinical Practice Update on Management of Inflammatory Bowel Disease During the COVID-19 Pandemic:Expert Commentary. Gastroenterology. 2020;159:350–357. doi: 10.1053/j.gastro.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ribaldone DG, Astegiano M, Actis GC, Pellicano R. Management of inflammatory bowel disease during COVID-19 pandemic. Minerva Gastroenterol Dietol. 2020;66:184–186. doi: 10.23736/S1121-421X.20.02707-5. [DOI] [PubMed] [Google Scholar]
- 26.Remzi FH, Panis Y, Spinelli A, et al. International Organization for the Study of Inflammatory Bowel Disease Recommendations for Surgery in Patients with Inflammatory Bowel Disease During the COVID-19 Pandemic. Dis Colon Rectum. 2020;63:870–873. doi: 10.1097/DCR.0000000000001718. [DOI] [PubMed] [Google Scholar]
- 27.Garcia LP, Duarte E. Nonpharmaceutical interventions for tackling the COVID-19 epidemic in Brazil. Epidemiol Serv Saude. 2020;29:e2020222. doi: 10.5123/S1679-49742020000200009. [DOI] [PubMed] [Google Scholar]
- 28.Queiroz NSF, Barros LL, Azevedo MFC, et al. Management of inflammatory bowel disease patients in the COVID-19 pandemic era:a Brazilian tertiary referral center guidance. Clinics (Sao Paulo) 2020;75:e1909. doi: 10.6061/clinics/2020/e1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Danese S, Cecconi M, Spinelli A. Management of IBD during the COVID-19 outbreak:resetting clinical priorities. Nat Rev Gastroenterol Hepatol. 2020;17:253–255. doi: 10.1038/s41575-020-0294-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iacucci M, Cannatelli R, Labarile N, et al. Endoscopy in inflammatory bowel diseases during the COVID-19 pandemic and post-pandemic period. Lancet Gastroenterol Hepatol. 2020;5:598–606. doi: 10.1016/S2468-1253(20)30119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mikocka-Walus A, Massuger W, Knowles SR, et al. Psychological distress is highly prevalent in inflammatory bowel disease:A survey of psychological needs and attitudes. JGH Open. 2020;4:166–171. doi: 10.1002/jgh3.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parra RS, Feitosa MR, Ribeiro LCH, Castro LA, Rocha JJR, Féres O. Infliximab trough levels and quality of life in patients with inflammatory bowel disease in maintenance therapy. Gastroenterol Res Pract. 2018;2018:1952086. doi: 10.1155/2018/1952086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parra RS, Chebli JMF, Amarante HMBS, et al. Quality of life work productivity impairment and healthcare resources in inflammatory bowel diseases in Brazil. World J Gastroenterol. 2019;25:5862–5882. doi: 10.3748/wjg.v25.i38.5862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Del Hoyo J, Nos P, Bastida G, et al. Telemonitoring of Crohn's disease and ulcerative colitis (TECCU):cost-effectiveness analysis. J Med Internet Res. 2019;21:e15505. doi: 10.2196/15505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Occhipinti V, Pastorelli L. Challenges in the care of IBD patients during the CoViD-19 pandemic:report from a “Red Zone”Area in Northern Italy. Inflamm Bowel Dis. 2020;12:793–796. doi: 10.1093/ibd/izaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bai X, Yang H, Qian J. COVID-19 outbreak and inflammatory bowel disease management:a questionnaire survey from realistic practice. J Crohns Colitis. 2020;5:1494–1495. doi: 10.1093/ecco-jcc/jjaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sitte J, Frentiu E, Baumann C, et al. Vaccination for influenza and pneumococcus in patients with gastrointestinal cancer or inflammatory bowel disease:A prospective cohort study of methods for improving coverage. Aliment Pharmacol Ther. 2019;49:84–90. doi: 10.1111/apt.15057. [DOI] [PubMed] [Google Scholar]
- 38.Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014;20:246–250. doi: 10.1097/01.MIB.0000437737.68841.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strasse KLA, Jamur CM, Marques J, Kim MSM, Petterle RR, Amarante HMBDS. Immunization status of patients with inflammatory bowel disease. Arq Gastroenterol. 2019;56:124–130. doi: 10.1590/S0004-2803.201900000-26. [DOI] [PubMed] [Google Scholar]
- 40.Bortlik M, Duricova D, Machkova N, et al. Discontinuation of anti-tumor necrosis factor therapy in inflammatory bowel disease patients: a prospective observation. Scand J Gastroenterol. 2016;51:196–202. doi: 10.3109/00365521.2015.1079924. [DOI] [PubMed] [Google Scholar]
- 41.Bots SJ, Kuin S, Ponsioen CY, et al. Relapse rates and predictors for relapse in a real-life cohort of IBD patients after discontinuation of anti-TNF therapy. Scand J Gastroenterol. 2019;54:281–288. doi: 10.1080/00365521.2019.1582693. [DOI] [PubMed] [Google Scholar]
- 42.Gisbert JP, Marín AC, Chaparro M. The risk of relapse after anti-TNF discontinuation in inflammatory bowel disease:systematic review and meta-analysis. Am J Gastroenterol. 2016;111:632–647. doi: 10.1038/ajg.2016.54. [DOI] [PubMed] [Google Scholar]
- 43.Zhang B, Gulati A, Alipour O, Shao L. Relapse from deep remission after therapeutic de-escalation in inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis. 2020;5:1413–1423. doi: 10.1093/ecco-jcc/jjaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Casanova MJ, Chaparro M, García-Sánchez V, et al. Evolution after anti-TNF discontinuation in patients with inflammatory bowel disease:a multicenter long-term follow-up study. Am J Gastroenterol. 2017;112:120–131. doi: 10.1038/ajg.2016.569. [DOI] [PubMed] [Google Scholar]
- 45.Mak JWY, Tang W, Yip TCF, et al. Stopping anti-tumour necrosis factor therapy in patients with perianal Crohn's disease. Aliment Pharmacol Ther. 2019;50:1195–1203. doi: 10.1111/apt.15547. [DOI] [PubMed] [Google Scholar]
- 46.Allocca M, Fiorino G, Furfaro F, et al. Maintaining the quality standards of care for inflammatory bowel disease patients during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2020;18:1882–1883. doi: 10.1016/j.cgh.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.D'Amico F, Peyrin-Biroulet L, Danese S. Inflammatory bowel diseases and COVID-19:the invisible enemy. Gastroenterology. 2020;158:2302–2304. doi: 10.1053/j.gastro.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brenner EJ, Ungaro RC, Gearry RB, et al. Corticosteroids, but not TNF antagonists are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology. 2020;159:481–491. e3. doi: 10.1053/j.gastro.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bezzio C, Saibeni S, Variola A, et al. Outcomes of COVID-19 in 79 patients with IBD in Italy:an IG-IBD study. Gut. 2020;69:1213–1217. doi: 10.1136/gutjnl-2020-321411. [DOI] [PubMed] [Google Scholar]
- 50.Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J Crohns Colitis. 2020;16(14):1334–1336. doi: 10.1093/ecco-jcc/jjaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]


