Abstract
Objectives:
In fluoroscopy-guided interventional practices, new dose reduction systems have proved to be efficient in the reduction of patient doses. However, it is not clear whether this reduction in patient dose is proportionally transferred to operators’ doses. This work investigates the secondary radiation fields produced by two kinds of interventional cardiology units from the same manufacturer with and without dose reduction systems.
Methods:
Data collected from a large sample of clinical procedures over a 2-year period (more than 5000 procedures and 340,000 radiation events) and the DICOM radiation dose structured reports were analysed.
Results:
The average cumulative Hp(10) per procedure measured at the C-arm was similar for the standard and the dose reduction systems (452 vs 476 μSv respectively). The events analysis showed that the ratio Hp(10)/KAP at the C-arm was (mean ± SD) 5 ± 2, 10 ± 4, 14 ± 4 and 14 ± 6 μSv·Gy−1·cm−2 for the beams with no added filtration, 0.1, 0.4 and 0.9 mm Cu respectively and suggested that the main cause for the increment of the ratio Hp(10)/KAP vs the “standard system” is the use of higher beam filtration in the “dose reduction” system.
Conclusion:
Dose reduction systems are beneficial to reduce KAP in patients and their use should be encouraged, but they may not be equally effective to reduce occupational doses. Interventionalists should not overlook their own personal protection when using new technologies with dose reduction systems.
Advances in knowledge:
Dose reduction technology in interventional systems may increase scatter dose for operators. Personal protection should not be overlooked with dose reduction systems.
Introduction
Interventional procedures are among the diagnostic medical practices with highest radiation doses. That is why, following the recommendations of the International Commission on Radiological Protection (ICRP),1,2 the European directive and national regulations stress the importance of optimization in interventional practices.3 Optimization, which means enough diagnostic information for the clinical task but with the smallest possible radiation dose for patients and operators, is especially challenging for fluoroscopically guided procedures. Interventionists should therefore know the “price in dose” they are paying for each minute of fluoroscopy, each run of cine, of digital subtraction angiography (DSA) or of cone beam computed tomography (CBCT). The ICRP recommends adopting an integral approach for radiation protection during interventional procedures and auditing not only patient doses but also occupational doses,2 while never losing sight of the clinical outcome in any medical procedure.
In the last years, there has been considerable progress in the patient dose monitoring technology thanks to the Digital Imaging and Communication in Medicine (DICOM) standard and the radiation dose structured reports (RDSR). Most of the patient dose information at radiation event level is currently available in these RDSR and the possibility of managing all information through new automatic patient dose registries opened up a new era for the optimization of imaging procedures that would have been unthinkable only a few years ago.
The conventional personal dosimeter for interventionists (and other health professionals working in catheterization rooms) was traditionally the “passive dosimeter” that would give the total cumulative occupational dose for 1 month without any possibility of discriminating the occupational dose for each individual procedure. Today, electronic “active dosimeters” allow the level of occupational dose for each radiation event to be measured, archived and analyzed in an “occupational dose structured report” - in a similar way as with RDSR for patients - and the secondary radiation level (and the occupational doses) to be correlated with the patient doses.4,5
Manufacturers of X-ray and imaging systems have also made efforts to optimize their products by improving the post-processing of the images and achieving a reduction of more than 50% in patient doses while maintaining or improving the image quality.6–13 These dose reduction systems may require increasing the X-ray spectral filters to increase the mean beam energy in order to reduce the patient entrance dose. They also require the use of image post-processing algorithms to maintain image contrast at an acceptable level. A reduction in patient dose that keeps image quality and clinical information acceptable is always welcome. It is in general assumed that a reduction in patient dose leads to a reduction in occupational dose: this would be true if the radiation quality did not change but, in such dose reduction systems, the quantity of primary radiation is reduced but the quality (mean energy of the spectra) is increased. Then, how does the level of secondary radiation around the patients change for the operators? Do occupational doses also decrease in the same way as patient doses do?
There is an agreement among physicists that the secondary radiation level also increases when the primary beam quality is increased.14–17 Perisnakis et al18 reported an increment of a factor ≈1,5 at interventionalist location when the total beam filtration moved from 5 to 11 mm. Al. Sutton et al19 showed increments in a factor of ≈2.5 when the additional filtration is increased from 0 to 0.99 mm Cu. Using dose reduction systems, among other adjustments beam filtration is likely to increase. However, since the different fluoroscopy systems have different logics of automatic dose rate control and as their application in clinical practice may vary, their impact is difficult to predict. As a consequence, different or even conflicting results are found in the literature. Schueler et al20 reported a reduction in patient and operator doses when the spectral beam filtration was increased from 0.2 to 0.5 mm Cu, and at the same time a reduction in occupational dose half that of the patient dose. Buytaert et al21 reported a patient and occupational reduction (at feet level) of more than 60% using a patient dose reduction system which increased the primary beam filtration, but they also said that secondary radiation increases with higher beam filtration. Salinas et al22 have recently analyzed a series of percutaneous interventions on chronic total occlusions performed with and without dose reduction system and reached a patient dose reduction of 36%, but no significant difference in occupational dose.
The aim of this work is to quantify the effect of one of these dose reduction systems on the secondary radiation measured by a reference dosimeter at the C-arm using a large sample of clinical procedures.
Methods and materials
Occupational and patient doses are routinely supervised by the medical physicists in the three interventional laboratories of the Interventional Cardiology Department at the Hospital Clínico San Carlos (Madrid, Spain). Two of the interventional laboratories are Allura Xper models and the third one is an Allura Clarity (all from Philips Healthcare). All three have the same image detector and X-ray tube and quite a similar generator. The main difference between the Allura Xper model and the Allura Clarity is that the latter has an additional functionality (hardware and software) that can provide an important patient dose reduction.6–13,21,22 This dose reduction functionality requires the use of higher beam filtration, that has a default value of 0.4 mm Cu +1 mm Al for fluoroscopy and cine. In the Xper model, the cine is delivered with no additional filtration and the fluoroscopy has ( in Hospital Clínico San Carlos) a default value of 0.9 mm Cu +1 mm Al. The operator can change the beam filtration if necessary, which very rarely happens, and the most frequent operation modes are in general the default modes. When comparing these two different systems, we shall refer from now on to the Xper model with no added filtration in cine as the “standard” system and to Clarity with a patient dose reduction capability and with 0.4 mm Cu +1 mm Al of added filtration in cine as the “dose reduction” system. Both systems use pulsed radiation beams with a frequency ranging from 7.5 to 25 pulses/s and a pulse width from 3 to 15 ms. The pulse frequency is fixed for each mode and selected by the user, 7.5 and 15 being the most used, but the pulse width is set by the automatic exposure control according to patient thickness.
Using the dose management system DoseWise Portal coupled with the DoseAware Xtend system (both from Philips HealthCare), the patient dose records from the RDSR are archived along with the occupational dose measurements from the ODSR from all the electronic personal dosimeters model i3 (RaySafe, Sweden) used in the room (Figure 1). The dose information is recorded at event level and includes detailed data relative to beam quality (kV and filtration), beam angle, KAP, etc. as well as the quantity Hp(10) for those electronic dosimeters present in the room. An analysis of Hp(10)/KAP can therefore be made at room, procedure or event level.
Figure 1.
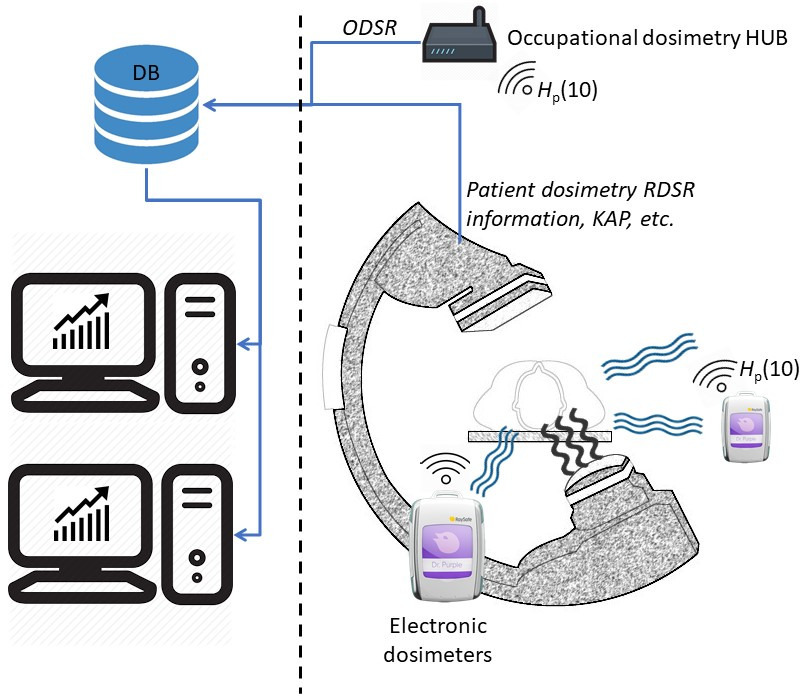
Dose management system used in this experiment, managing occupational and patient dose. The dosimeter located at the C-arm used in this experiment is shown bigger. ODSR, occupational dose structured report.
The personal dosimeter used for this study is the one located at a point of the C-arm (Figure 1). This point is defined by the intersection of a straight line with the C-arm from the isocentre, forming a 45° angle with C-arm rotation axis. It receives high secondary radiation dose rate from patient backscatter and describes the dose rate in the worst cases, e.g. in those radiation events where the tube and the professional are on the same side of the patient.23 Depending on the protection level, in particular if a protection screen is being used, the cumulative dose per procedure over the apron at chest level is expected to under 2% of the secondary radiation dose measured by the C-arm reference dosimeter.24 For the model of dosimeters used in this work, the manufacturer declares an energy dependence of less than 25%1(N40-N150), a dose rate uncertainty of 10% for dose rates between 40 and 150 mSv/h and of 20% for dose rates between 150 and 300 mSv/h. Regarding angular dependence, their response can drop to less than 20% for incidence angles under 60°. He also warns that the dosimeters may have temperature dependence of 5% between 15 and 26°C but this dependence could reach 20% for temperatures over 26°C. Some authors25–29 have brought up an issue regarding the response of electronic personal dosimeters with pulsed radiation fields and the high instantaneous dose rates present during these radiation pulses. That is why the Medical Physics Service in our hospital routinely tests (at least once a year) the performance of their electronic personal dosimeters with pulsed radiation beams and a reference personal dosimeter (EPD Mk2 from Thermo-Fisher Scientific, Walltman, Massachusetts, USA) calibrated in a secondary laboratory. This reference dosimeter was tested26,29 with acceptable results in cumulative dose measurements for dose rates under 1.8 Sv/h and pulsed frequencies under 20 s−1. In the in-house verification performed by the Medical Physics Service, dosimeters are irradiated with the scatter radiation produced by a PMMA phantom located over the examination couch on an interventional C-arm, with beams typically used in interventional radiology and cardiology on several kVs and filtrations (60–120 kV), and pulse frequencies from 3 to 25 p/s. The Medical Physics Service routinely also tests the accuracy of the KAP meter integrated in the C-arms: to this end, a calibrated semiconductor detector is used to measure the incident air kerma and a computed radiography (CR) plate to measure the radiation field size, as recommended by national and international protocols.30,31 The DoseWise portal allows the user to introduce a correction factor for the KAP, and this factor is rounded to the first decimal figure by the system. Based on this information and considering the energy dependence of the KAP meters as the main source of uncertainty, 10% was considered to be the uncertainty for the KAP provided by the modality in this experiment.
Considering the uncertainty of both measurement quantities, Hp(10) at the C-arm and KAP, the global uncertainty will be dominated by the measurement of Hp(10) whose uncertainty depends on several factors as described previously and could be estimated (with the square root of the quadratic sum) from 27 to 37% in the worst case. The uncertainty of the ratio Hp(10)/KAP would then range between 30 and 40%.
A statistical analysis was carried out with SPSS 25 (IBM, USA). The Student’s t and two-way ANOVA tests were used as hypothesis tests when distributions could be considered normal and variance homogeneity could be assumed, otherwise Mann–Whitney U and Kruskal–Wallis tests were used.
The ethics committee of the Hospital Clínico San Carlos gave a favourable opinion on this work (C.I.19/377E).
Results
First, results at event level are presented to investigate how the scatter radiation changes with the beam quality (spectral filters and kV). Secondly, results at procedure level are presented showing the impact in clinical practice.
Table 1 shows the sample sizes managed in this study in the three interventional rooms and the percentage of KAP delivered with the different beam filtrations (ΣKAPfilter/ΣKAPtotal).
Table 1.
Sample sizes for the “standard” systems (rooms 1 and 2) and the “dose reduction” system (room 3)
| Room 1 | Room 2 | Room 3 | ||
|---|---|---|---|---|
| X-ray system | Standard | Standard | Dose reduction | |
| No. clinical procedures | 1659 | 2683 | 667 | |
| No. total radiation events | 110,676 | 159,849 | 70,522 | |
| % of total KAP with | No added filtration | 74% | 72% | 10% |
| 0.1 mm Cu +1 mm Al | 2% | 2% | 20% | |
| 0.4 mm Cu +1 mm Al | 4% | 4% | 70% | |
| 0.9 mm Cu +1 mm Al | 20% | 22% | 0% | |
The use of the different filtrations in the three rooms in this sample is shown as the % of the total KAP delivered.
Analysis at event level
Figure 2 shows the average and the standard deviation of the sample for Hp(10)/KAP measured at the C-arm for events from clinical procedures performed in the three rooms, with 75 < kV < 85, C-arm angles between −10 and 10 degrees and the four different beam filtrations used in clinics. Differences resulted statistically significant under Kruskal–Wallis (p < 0.001), even in the two last groups (0.4 mm Cu +1 Al and 0.9 mm Cu +1 Al) that resulted with p < 0.001 under Mann–Whitney U test, probably as a consequence of the high sample sizes (n1 = 6241 and n2 = 3882 radiation events).
Figure 2.
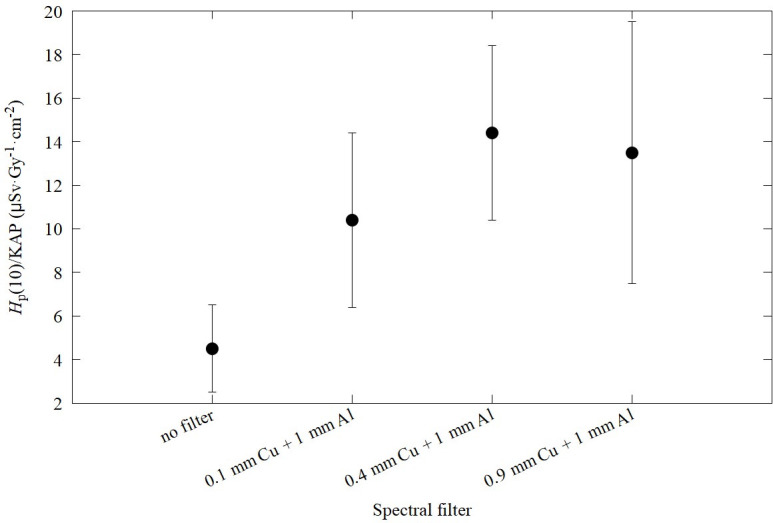
Hp(10) at C-arm/KAP vs beam filtration for the sample of events with restricted kV and C-arm close to PA projection (±10°). Each point represents the mean value and the standard deviation of the sample for radiation events with 75 < kV < 85 and −10° < C arm angles < 10°. Sample sizes ranged from a minimum of 223 to 6241 radiation events.
Figure 3 shows the average and standard deviation of the sample for Hp(10)/KAP measured at the C-arm vs the kV, for the events with C-arm angles between −10 and 10 degrees. For simplicity’s sake, only the most frequent spectral filtrations (Table 1) are shown. All differences can be considered statistically significant (p ≤ 0.004 under Kruskal–Wallis and Mann–Whitney tests) with the exception of groups (60,70), (70–80) and (80–90) kV for no filter and groups (60–70) and >100 for 0.4 mm Cu +1 mm Al.
Figure 3.
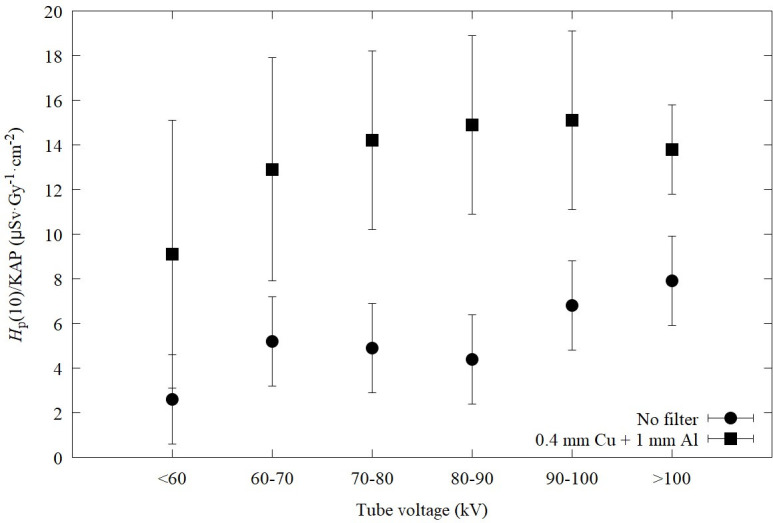
The ratio Hp(10) at C-arm/KAP vs kV for a sample of events for C-arm angles close to PA projection. Each point represents the average and standard deviation (of the sample) for radiation events with −10°< C arm angles < 10°. Minimum sample sizes were of 5 events (for no filter, kV > 100), 17 events (for no filter 90–100 kV) and 56 events (for no filter, kV <60). The rest of the points had sample sizes greater than 100 up to 7474 radiation events.
Analysis at procedure level
Figure 4 shows the ratio Hp(10)/KAP per cardiac procedure, graphed with boxes, for the two types of systems discussed in this investigation: the “dose reduction” system with high filtration (with a default added filtration of 0.4 mm Cu in cine) and the “standard” system with low filtration (with no added filtration in cine). The boxes represent the percentiles 5, 25, 50, 75 and 95%. The cross-point is the average. The sample sizes were the ones shown in Table 1. Both distributions are quite symmetric and present similarities with normal distribution at Q-Q graphs (not shown in this paper). The average ± standard deviation resulted in 7 ± 2 μSv·Gy−1cm−2 for the “standard” and 13 ± 3 μSv·Gy−1cm−2 for the “dose reduction” system (p < 0.001 under Student’s t test).
Figure 4.
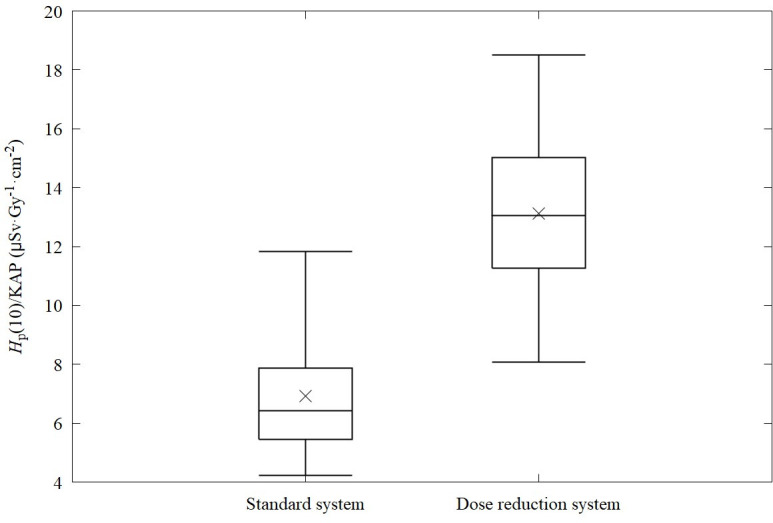
Ratios of Hp(10) at C-arm/KAP for interventional procedures performed with the two X-ray systems used in this survey. The standard system has a cine mode with no added filtration. The “dose reduction” X-ray unit has patient dose reduction system that uses a cine X-ray beam with 0.4 mm Cu +1 mm Al added filtration (default filtration).
Figure 5 shows the cumulative KAP and Hp(10) at the C-arm per procedure for both models of X-ray systems. Student t test resulted in significant differences (p < 0.001) even for Figure 5b because of the high sample size.
Figure 5.
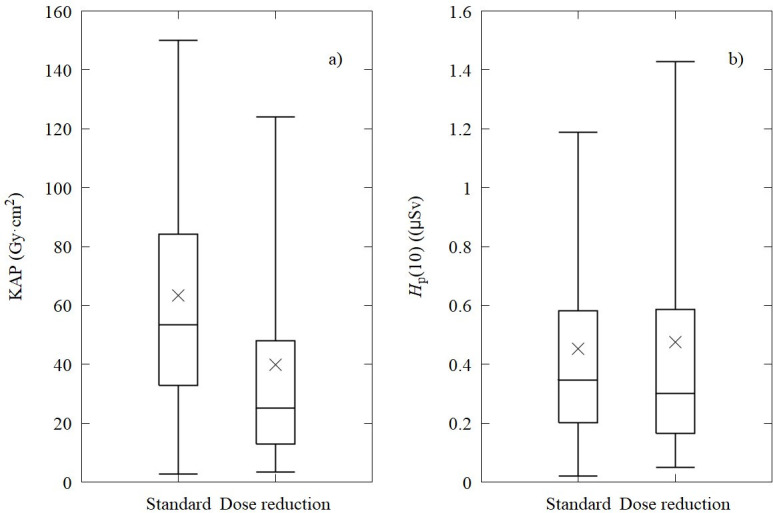
The KAP per procedure and the Hp(10) per procedure measured at the C-arm. Box graph shows the percentiles 5, 25, 50, 75 and 95%. The cross-point shows the average. As shown in Table 1, in the “dose reduction” system, 70% of the KAP was delivered with 0.4 mm Cu + 1 mm Al of added filtration. In the standard system, 70% of the KAP was delivered with no added filtration.
Discussion
Our results show (Figure 2) an increase of the scatter dose to patient dose ratio Hp(10)/KAP by a factor of up to 2.6 when increasing the spectral filtration from 0 to 0.4 mm Cu +1 mm Al. This result is consistent with those phantom measurements published in the literature.19 Similarly, Figure 3 shows an increase of Hp(10) to KAP ratio with a factor of 2.5 when changing the tube voltage from below 60 kV to above 100 kV, and a similar variation when the beam filtration is increased from no filter to 0.4 mm Cu +1 mm Al. This is consistent with previous publications.14,15
Therefore, the factor that affects the most the ratio Hp(10)/KAP measured at the C-arm is the beam quality, in particular when using higher beam filtration: a higher Hp(10)/KAP ratio is then produced.
In Figure 4, the analysis of Hp(10)/KAP is made at procedure level for the two systems investigated. The samples corresponding to rooms 1 and 2 are treated as the “standard” system. As seen from Table 1, the standard system used in rooms 1 and 2 delivers 70% of the KAP with no filtration. In the case of the “dose reduction” system used in room 3, the 70% of the KAP was delivered with 0.4 mm Cu +1 mm Al, which permits to reduce the patient KAP by 50–75% as shown in literature.6–13,21,22 But this leads to an increment of the ratio of Hp(10)/KAP by a factor of almost two as shown in Figure 4. Therefore, the important reduction in patient dose obtained by the “dose reduction” system is not directly transferred to the scatter radiation dose to the operators as the reduction in KAP is compensated with the increase in Hp(10). In fact, in this sample, the average for the cumulative Hp(10) per procedure measured at the C-arm was quite similar in both systems: for the standard and dose reduction system, the average was 452 and 476 μSv respectively, while the average KAP was higher in the standard system, 63 vs 40 Gy·cm2 (Figure 5a and b).
In the analysis of the cumulative Hp(10) at procedure level, the complexity of the procedures, that has not been considered here, might be different in different rooms and can affect the results. Salinas et al22 presented an analysis using the same X-ray systems considering the complexity of the procedures: in a sample of chronic total occlusions, a reduction by almost 36% in patient dose was observed, but no reduction in occupational dose was found, neither at the C-arm, nor at operators.
Our study has limitations, the most important of which is that the measurement of secondary radiation was based at a particular point at the C-arm. It certainly gives a general idea of the secondary radiation level present in an interventional laboratory, but the results in operators can behave differently depending on the distance to the source of secondary radiation, the C-arm orientation and the proper use of suspended protection screens during all the procedures.
Conclusion
In interventional practices, “dose reduction” systems using high filtration X-ray beams can provide an important reduction in patient dose indicators. Their use should be encouraged in interventional rooms whenever the image quality provided gives enough clinical information. But it is also important to note that they may not provide the same reduction in scatter radiation dose for operators. Therefore, interventionalists must not overlook personal protection even when working with patient dose reduction systems.
Acknowledgements: This work has been partially founded by the Spanish Ministry of Economy and Competitiveness (Instituto de Salud Carlos III) and European Regional Development Fund (ERDF) under the project MEDICI number PI16/01413 and the Spanish National Safety Council under the project EDOCI.
https://www.raysafe.com/products/real-time-dosimetry-systems/raysafe-i3-real-time-radiation-dosimeter
Contributor Information
Roberto M Sanchez, Email: robertomariano.sanchez@salud.madrid.org.
Eliseo Vano, Email: eliseov@ucm.es.
Pablo Salinas, Email: salinas.pablo@gmail.com.
Nieves Gonzalo, Email: nieves_gonzalo@yahoo.es.
Javier Escaned, Email: javier.escaned@salud.madrid.org.
Jose M Fernández, Email: josemiguel.fernandez@salud.madrid.org.
REFERENCES
- 1.Valentin J. Avoidance of radiation injuries from medical interventional procedures. Ann ICRP 2000; 30: 7–67. doi: 10.1016/S0146-6453(01)00004-5 [DOI] [PubMed] [Google Scholar]
- 2.Cousins C, Miller DL, Bernardi G, Rehani MM, Schofield P, Vañó E, et al. ICRP publication 120: radiological protection in cardiology. Ann ICRP 2013; 42: 1–125. doi: 10.1016/j.icrp.2012.09.001 [DOI] [PubMed] [Google Scholar]
- 3. Council Directive 2013/59/Euratom of 5 December 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation, and repealing directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom. 73. [Google Scholar]
- 4.Sanchez R, Vano E, Fernandez JM, Gallego JJ. Staff radiation doses in a real-time display inside the angiography room. Cardiovasc Intervent Radiol 2010; 33: 1210–4. doi: 10.1007/s00270-010-9945-4 [DOI] [PubMed] [Google Scholar]
- 5.Vano E, Sanchez RM, Fernandez JM. Strategies to optimise occupational radiation protection in interventional cardiology using simultaneous registration of patient and staff doses. J Radiol Prot 2018; 38: 1077–88. doi: 10.1088/1361-6498/aad429 [DOI] [PubMed] [Google Scholar]
- 6.Söderman M, Holmin S, Andersson T, Palmgren C, Babić D, Hoornaert B. Image noise reduction algorithm for digital subtraction angiography: clinical results. Radiology 2013; 269: 553–60. doi: 10.1148/radiol.13121262 [DOI] [PubMed] [Google Scholar]
- 7.Söderman M, Mauti M, Boon S, Omar A, Marteinsdóttir M, Andersson T, et al. Radiation dose in neuroangiography using image noise reduction technology: a population study based on 614 patients. Neuroradiology 2013; 55: 1365–72. doi: 10.1007/s00234-013-1276-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balter S, Brinkman M, Kalra S, Nazif T, Parikh M, Kirtane AJ, et al. Novel radiation dose reduction fluoroscopic technology facilitates chronic total occlusion percutaneous coronary interventions. EuroIntervention 2017; 13: e1468–74. doi: 10.4244/EIJ-D-16-00216 [DOI] [PubMed] [Google Scholar]
- 9.Gislason-Lee AJ, Keeble C, Malkin CJ, Egleston D, Bexon J, Kengyelics SM, et al. Impact of latest generation cardiac interventional X-ray equipment on patient image quality and radiation dose for trans-catheter aortic valve implantations. Br J Radiol 2016; 89: 20160269. doi: 10.1259/bjr.20160269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gislason-Lee AJ, Keeble C, Egleston D, Bexon J, Kengyelics SM, Davies AG. Comprehensive assessment of patient image quality and radiation dose in latest generation cardiac X-ray equipment for percutaneous coronary interventions. J Med Imaging 2017; 4: 025501. doi: 10.1117/1.JMI.4.2.025501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastrati M, Langenbrink L, Piatkowski M, Michaelsen J, Reimann D, Hoffmann R. Reducing radiation dose in coronary angiography and angioplasty using image noise reduction technology. Am J Cardiol 2016; 118: 353–6. doi: 10.1016/j.amjcard.2016.05.011 [DOI] [PubMed] [Google Scholar]
- 12.Sullivan PM, Harrison D, Badran S, Takao CM, Ing FF. Reduction in radiation dose in a pediatric cardiac catheterization lab using the Philips AlluraClarity X-ray system. Pediatr Cardiol 2017; 38: 1583–91. doi: 10.1007/s00246-017-1700-z [DOI] [PubMed] [Google Scholar]
- 13.Dekker LRC, van der Voort PH, Simmers TA, Verbeek XAAM, Bullens RWM, Veer Marcel Van't, van’t VM, et al. New image processing and noise reduction technology allows reduction of radiation exposure in complex electrophysiologic interventions while maintaining optimal image quality: a randomized clinical trial. Heart Rhythm 2013; 10: 1678–82. doi: 10.1016/j.hrthm.2013.08.018 [DOI] [PubMed] [Google Scholar]
- 14.Boone JM, Levin DC. Radiation exposure to angiographers under different fluoroscopic imaging conditions. Radiology 1991; 180: 861–5. doi: 10.1148/radiology.180.3.1871307 [DOI] [PubMed] [Google Scholar]
- 15.Marshall NW, Faulkner K. The dependence of the scattered radiation dose to personnel on technique factors in diagnostic radiology. Br J Radiol 1992; 65: 44–9. doi: 10.1259/0007-1285-65-769-44 [DOI] [PubMed] [Google Scholar]
- 16.Marshall NW, Faulkner K, Warren H. Measured scattered X-ray energy spectra for simulated irradiation geometries in diagnostic radiology. Med Phys 1996; 23: 1271–6. doi: 10.1118/1.597690 [DOI] [PubMed] [Google Scholar]
- 17.Williams JR. Scatter dose estimation based on dose–area product and the specification of radiation barriers. Br J Radiol 1996; 69: 1032–7. doi: 10.1259/0007-1285-69-827-1032 [DOI] [PubMed] [Google Scholar]
- 18.Perisinakis K, Solomou G, Stratakis J, Damilakis J. Data and methods to assess occupational exposure to personnel involved in cardiac catheterization procedures. Phys Med 2016; 32: 386–92. doi: 10.1016/j.ejmp.2016.02.006 [DOI] [PubMed] [Google Scholar]
- 19.Sutton DG, Martin CJ, Peet D, Williams JR. The characterization and transmission of scattered radiation resulting from X-ray beams filtered with zero to 0.99 MM copper. J Radiol Prot 2012; 32: 117–29. doi: 10.1088/0952-4746/32/2/117 [DOI] [PubMed] [Google Scholar]
- 20.Schueler BA, Vrieze TJ, Bjarnason H, Stanson AW. An investigation of operator exposure in interventional radiology. Radiographics 2006; 26: 1533–41. doi: 10.1148/rg.265055127 [DOI] [PubMed] [Google Scholar]
- 21.Buytaert D, Eloot L, Mauti M, Drieghe B, Gheeraert P, Taeymans Y, et al. Evaluation of patient and staff exposure with state of the art X-ray technology in cardiac catheterization: a randomized controlled trial. J Interv Cardiol 2018; 31: 807–14. doi: 10.1111/joic.12553 [DOI] [PubMed] [Google Scholar]
- 22.Salinas P, Sanchez‐Casanueva RM, Gonzalo N, Gil J, Salazar CH, Jimenez‐Quevedo P, et al. Dose‐reducing fluoroscopic system decreases patient but not occupational radiation exposure in chronic total occlusion intervention. Catheter Cardiovasc Interv 2020; 13: ccd.29253. doi: 10.1002/ccd.29253 [DOI] [PubMed] [Google Scholar]
- 23.Vano E, Sanchez RM, Fernandez JM, Bartal G, Canevaro L, Lykawka R, et al. A set of patient and staff dose data for validation of Monte Carlo calculations in interventional cardiology. Radiat Prot Dosimetry 2015; 165(1-4): 235–9. doi: 10.1093/rpd/ncv032 [DOI] [PubMed] [Google Scholar]
- 24.Vano E, Sanchez RM, Fernandez JM. Estimation of staff lens doses during interventional procedures. comparing cardiology, neuroradiology and interventional radiology. Radiat Prot Dosimetry 2015; 165(1-4): 279–83. doi: 10.1093/rpd/ncv049 [DOI] [PubMed] [Google Scholar]
- 25.Ciraj-Bjelac O, Carinou E, Vanhavere F. Use of active personal dosimeters in hospitals: EURADOS survey. J Radiol Prot 2018; 38: 702–15. doi: 10.1088/1361-6498/aabce1 [DOI] [PubMed] [Google Scholar]
- 26.Clairand I, Bordy J-M, Daures J, Debroas J, Denozière M, Donadille L, et al. Active personal dosemeters in interventional radiology: tests in laboratory conditions and in hospitals. Radiat Prot Dosimetry 2011; 144(1-4): 453–8. doi: 10.1093/rpd/ncq556 [DOI] [PubMed] [Google Scholar]
- 27.Ankerhold U, Hupe O, Ambrosi P. Deficiencies of active electronic radiation protection dosemeters in pulsed fields. Radiat Prot Dosimetry 2009; 135: 149–53. doi: 10.1093/rpd/ncp099 [DOI] [PubMed] [Google Scholar]
- 28.Kržanović N, Živanović M, Ciraj-Bjelac O, Lazarević Đorđe, Ćeklić S, Stanković S. Performance testing of selected types of electronic personal dosimeters in X- and gamma radiation fields. Health Phys 2017; 113: 252–61. doi: 10.1097/HP.0000000000000704 [DOI] [PubMed] [Google Scholar]
- 29.Ambrosi P, Borowski M, Iwatschenko M. Considerations concerning the use of counting active personal dosimeters in pulsed fields of ionising radiation. Radiat Prot Dosimetry 2010; 139: 483–93. doi: 10.1093/rpd/ncp286 [DOI] [PubMed] [Google Scholar]
- 30.Lin P-JP, Schueler BA, Balter S, Strauss KJ, Wunderle KA, LaFrance MT, et al. Accuracy and calibration of integrated radiation output indicators in diagnostic radiology: a report of the AAPM imaging physics Committee task group 190. Med Phys 2015; 42: 6815–29. doi: 10.1118/1.4934831 [DOI] [PubMed] [Google Scholar]
- 31.Alonso Diaz M, Torres Cabrera R. Protocolo español de control de calidad en radiodiagnóstico. Revisión 2011. Madrid: Senda Editorial; 2012. https://www.seram.es/images/site/protocolo_2011.pdf. [Google Scholar]


