Abstract
Barosinusitis, or sinus barotrauma, is a well-described condition associated with changes in barometric pressure during flight and diving that can result in sinonasal mucosal injury. In this case report, we present an adolescent who experienced barosinusitis during scuba diving and subsequently developed Pott's puffy tumor (PPT), characterized by frontal sinusitis, frontal bone osteomyelitis, and overlying subperiosteal abscess. This unique case of PPT following scuba diving provides the opportunity to review the pathophysiology of both barotrauma-induced sinus disease and PPT, a rare and unreported serious complication of barosinusitis. Furthermore, we discuss how scuba diving and associated barosinusitis can be considered a risk factor in the development of PPT.
Key Words: barosinusitis, Pott's puffy tumor, scuba diving
Barosinusitis, or sinus barotrauma, is a well-described condition associated with changes in barometric pressure during flight and diving that can result in sinonasal mucosal injury. In this case report, we present an adolescent who experienced barosinusitis during scuba diving and subsequently developed Pott's puffy tumor (PPT), characterized by frontal sinusitis, frontal bone osteomyelitis, and overlying subperiosteal abscess. This unique case of PPT following scuba diving provides the opportunity to review the pathophysiology of both barotrauma-induced sinus disease and PPT, a rare and unreported serious complication of barosinusitis. Furthermore, we discuss how scuba diving and associated barosinusitis can be considered a risk factor in the development of PPT.
CASE
A 13-year-old white boy with no significant medical history presented to our emergency department with 4 days of severe frontal headache and left-sided forehead swelling and was diagnosed with PPT. The patient is a resident of England and was returning home from a family vacation in Aruba, where he had been scuba diving, when he presented to our New York City institution during a layover. The patient was a novice diver obtaining his initial certification during the trip. He completed 9 total dives over an 8-day period with maximum depth of 65 ft and cumulative diving time of 6 hours. He had notable difficulty equalizing inner ear pressure throughout descent during all of his dives. He experienced pain in his ears and sinuses, although not his forehead, which he reported made the descents very uncomfortable.
Two days after his last dive, the patient began developing symptoms, initially with unilateral eye tearing. He subsequently developed severe frontal headache, which worsened over the next 2 days with associated periorbital edema, malaise, and nonbloody emesis. At this time (4 days after his last dive), he sought treatment at a local clinic where he was prescribed nonsteroidal anti-inflammatory drugs with mild relief. The following day, the child and his family began their journey home on a flight from Aruba to New York City. Over the next 2 days, the patient experienced worsening swelling of his forehead spreading past midline and affecting both periorbital areas with continued severe headaches. Five days after initiation of symptoms and 7 days after his last dive, the patient presented to our hospital.
During this illness, the patient did not experience fevers, chills, diaphoresis, upper respiratory symptoms, abdominal pain, diarrhea, or rash. He had no history of headaches, migraines, allergic rhinitis, or sinusitis prior to this acute illness. He also had no history of prior otorhinolaryngology procedures, recurrent otitis media, or snoring during sleep.
Upon admission, pertinent findings on physical examination include normal vital signs, significant swelling of his forehead (left greater than right), marked bilateral periorbital edema, and nonpainful extraocular movements. Notable laboratory findings include a leukocyte count of 12.0 × 109/L with 77% neutrophils and a C-reactive protein of 74 mg/L. Magnetic resonance imaging (MRI) scan of the head with and without contrast was obtained on day of admission and revealed a heterogeneous T2 hyperintense, peripherally enhancing opacification of bilateral frontal sinuses extending to left anterior ethmoid air cells; a 2.0 × 0.3-cm subperiosteal abscess of the frontal bone; and dural enhancement, likely reactive, without brain parenchymal involvement (Fig. 1). The patient's clinical and radiological findings were consistent with PPT. Computed tomography scan without contrast of brain and sinuses demonstrated severe frontal sinus opacification (left greater than right), anterior ethmoid opacification, mucosal obstruction of the left ostiomeatal complex, mucosal thickening, and retention cysts throughout the sinuses. Of note, there was no evidence of intracranial involvement (Fig. 2).
FIGURE 1.
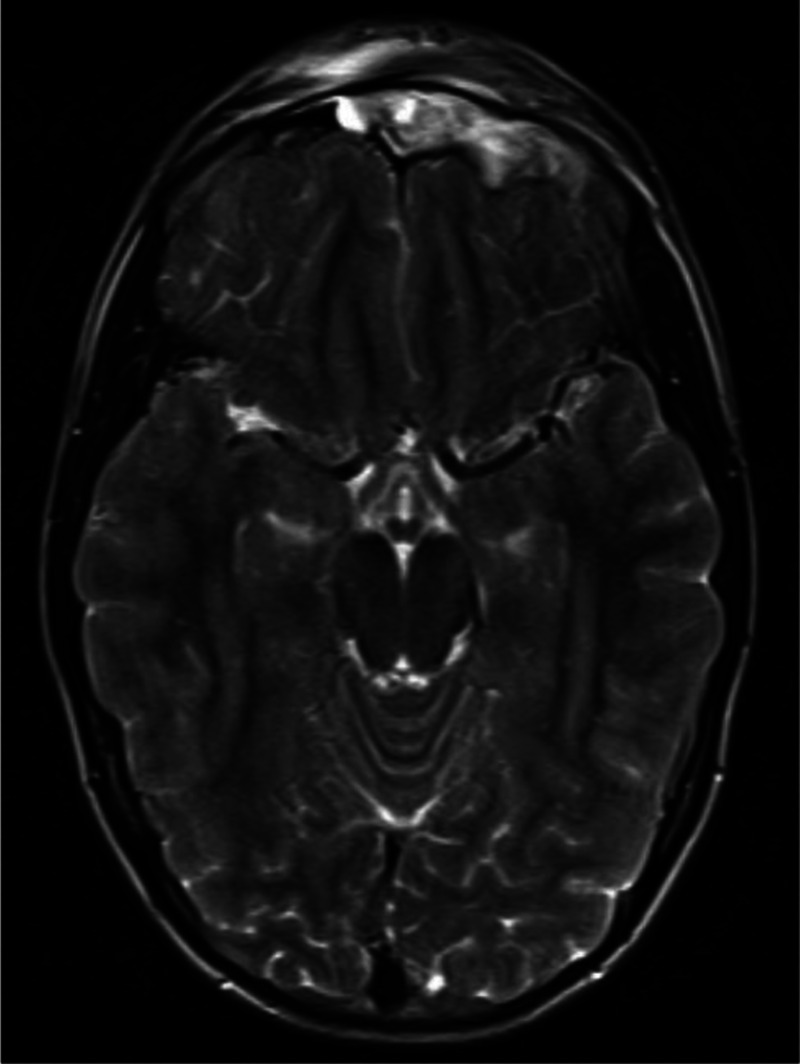
Magnetic resonance imaging scan of the brain with and without contrast: T2 hyperintense, peripherally enhancing opacification of bilateral frontal sinuses; 2.0 × 0.3-cm subperiosteal abscess of the frontal bone; and dural enhancement, likely reactive, without brain parenchymal involvement. Findings consistent with PPT.
FIGURE 2.
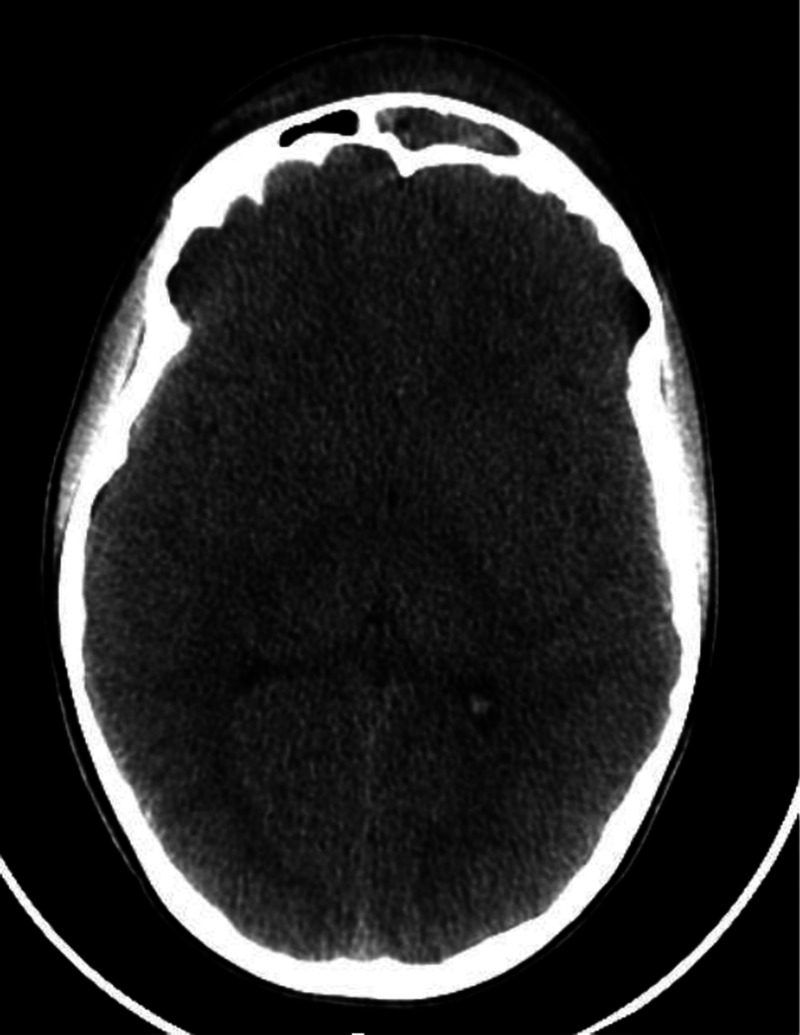
Computed tomography scan of the head without contrast showing severe opacification of the frontal sinuses, left greater than right with associated frontal scalp edema.
Ceftriaxone, vancomycin, and metronidazole were initiated empirically, and the patient underwent computed tomography (CT)–guided incision and drainage of the left frontal subperiosteal abscess, bilateral endoscopic frontal sinusotomy, bilateral endoscopic anterior ethmoidectomy, bilateral maxillary antrostomy, and endoscopic submucosal resection for deviated nasal septum. Intraoperative cultures from abscess drainage were negative for growth of organisms. The patient was hospitalized for 11 days during which his swelling improved, and his inflammatory markers down trended. On hospital day 11, his C-reactive protein normalized, minimal left forehead edema above his eyebrow remained, and he reported no tenderness. He was discharged on amoxicillin/clavulanate for an additional 4 weeks of therapy. Upon follow-up through 18 months after hospitalization, the patient had full recovery without any further complications.
DISCUSSION
Barosinusitis
Scuba diving is one of the fastest-growing “high-risk” recreational sports with an estimated 9 million certified divers in the United States alone.1 Barotrauma is common and is estimated to be experienced by 30% to 50% of divers.1–3 Novice scuba divers are more vulnerable to barotrauma and middle ear disorders because of their inexperience in equalization techniques. Furthermore, children may be more at risk of middle ear pressure equalization problems because of immature Eustachian tube function.
The pathophysiology of diving-induced sinus barotrauma is well described and referred to in the scuba vernacular as “sinus squeeze.” Boyle's Law, which states that the volume of gas is inversely proportional to its pressure at a given temperature, is fundamental in describing the pathogenesis of sinus barotrauma. Barosinusitis is often caused when sudden changes in ambient pressure are not compensated for by force equalization mechanisms within the sinuses.2 Normally, air pressure within the sinus cavities equilibrates with that of the surrounding nasal passages via openings in the sinuses called ostia. Blocked ostia or difficulty with equilibration can lead to uncompensated changes in the intrasinus pressure, which can result in varying degrees of sinonasal mucosal injury and inflammation.3 Divers experience great pressure variation over a short interval, which can lead to a cascade of changes directly impacting the ears and sinuses, as they are rigid air-filled cavities.
The physiology of sinus barotrauma is different during descent and ascent. During descent, the gas volume in the sinuses decreases up to 50% because of increased pressure from the effects of gravity and water mass.4 This decreased gaseous volume causes a decompression or sinus squeeze, which can result in pulling forces and lead to mucosal edema, submucosal hematoma formation, and subsequent tissue, fluid, and blood accumulation.3 The reduction in gas volume has to be equilibrated through the Eustachian tube and the sinus ostia to avoid barotrauma of the ear and sinuses. During ascent, this accumulated tissue and blood may be expelled because of gaseous expansion against the sinuses walls with decrease in pressure, resulting in epistaxis in a “reverse squeeze.” Any remaining tissue and blood products, in combination with necrotic or inflamed mucosa (secondary to allergies, upper respiratory tract infections, or preceding sinus inflammation), act as a medium for the propagation of bacteria, setting the patient up for the development of bacterial sinusitis.4 Decompression barosinusitis associated with descent is more common than injury related to ascent and reverse squeeze.
In our patient, we suspect scuba diving–induced sinus barotrauma led to the development of a pan-sinusitis, complicated by a frontal abscess and PPT. Although flying is also associated with barosinusitis and certainly may have exacerbated symptoms in this patient, we believe his sinusitis was initially triggered by the scuba diving as his symptoms began after diving and prior to air travel.
Eliciting a good history with attention to symptoms can be the most useful aid in diagnosing barotrauma-induced sinusitis. Clinical manifestations and complications from barosinusitis may be difficult to differentiate from other forms of sinusitis and include sinus pain, headache, epistaxis, and rarely meningitis or septal abscess.2,5 The most common symptom is pain referred to the frontal area, with the frontal sinus being the most commonly effected sinus resulting from barotrauma.3,5 In addition, excessive lacrimation from eye on the side most involved may be present.2 In our case, intensive and progressive headache, which was inadequately treated with nonsteroidal anti-inflammatory drugs, was the prominent symptom preceded by unilateral tearing. Although our patient did not have severe pain during his dives, he did experience discomfort, and the difficulty with ear pressure equalization is a crucial piece of the history. This uncompensated change in intrasinus pressure can result in the mucosal injuries observed in barosinusitis.
Case reports of barotrauma-induced sinus disease secondary to scuba diving range from acute sinusitis, sphenoidal mucocele formation, and sinusitis complicated by cerebral empyema.6,7 However, PPT as a sequela to scuba diving–related barotrauma has not been described in the literature. Each case had headache as a common presentation, although other symptoms such as fever and epistaxis were described. Antibiotics, corticosteroids, and surgical management were used in the management of these cases, either alone or in combination. Bacteriologic data were not reported in any of the case reports.
Pott's Puffy Tumor
Pott's puffy tumor, a rare but serious complication of frontal sinusitis, is characterized by osteomyelitis of the frontal bone associated with subperiosteal abscess and the pathognomonic sign of forehead swelling. It classically presents as a puffy swelling and edema over the forehead. Anterior spread of infection from the frontal sinus occurs most frequently via the avalvular diploic veins to the bone, but can also occur from direct extension.8 Risk factors associated with PPT include trauma, intranasal cocaine abuse, dental infections, or complications of neurosurgery.9
Intracranial complications occur in more than half of patients with PPT.10 Extension of the infection may occur in any of 3 directions. Infection may spread posteriorly either by direct extension or septic thrombosis to the dura leading to a subdural, epidural, and frontal brain abscess, meningitis, or cavernous sinus thrombosis.9,11,12 Infection could also extend anteriorly, resulting in subperiosteal abscess. If infection spread inferiorly through the frontal sinus, orbital complications such as preseptal and orbital cellulitis can occur.
Pott's puffy tumor is commonly seen in adolescent males due to the increase vascularity to the frontal bone as it actively grows during adolescence.11 Often patients have preceding symptoms of fever, headache, nasal or eye drainage, periorbital swelling, vomiting, and sinus tenderness.13 Patients usually present for medical attention with the classic sign of a well-circumscribed scalp swelling overlying the area of the osteomyelitis. An important diagnostic modality to diagnose PPT is a contrast-enhanced computed tomography scan, which provides better bone detail than MRI.14 Intracranial involvement is, however, best revealed from an MRI with gadolinium.15 Therefore, both radiological studies are recommended.15 Intracranial complications are usually associated with leukocytosis, elevated erythrocyte sedimentation rate, and raised C-reactive protein levels. However, PPT can also present without any typical laboratory findings.
Surgical sinus drainage is both diagnostic and therapeutic. Often drainage reveals polymicrobial infection. Common etiological organisms include Streptococcus species, Staphylococcus aureus, nontypeable Haemophilus influenzae, and anaerobes (including Bacteroides, Fusobacterium necrophorum). Streptococcus anginosus in particular has been described to cause aggressive intracranial infection in children.9,13,16 Early and definitive diagnosis of PPT is important to avoid intracranial and extracranial complications. Aggressive medical and surgical treatments are essential for optimal outcome. A multidisciplinary approach is important in the management of PPT, including involvement from the otolaryngology, neurosurgery, and infectious diseases teams, as management includes both surgical intervention as well as long-term antibiotic coverage, usually for 4 to 6 weeks.16 The most commonly reported surgical interventions include abscess evacuation, debridement, frontal craniotomy, and sinus lavage.15 The choice of antibiotics should initially be broad and have good central nervous system penetration if there is intracranial involvement, with the consideration of coverage for methicillin-resistant S. aureus.16
CONCLUSIONS
Despite the prevalence of sinus barotrauma in patients, barosinusitis and its complications may be unfamiliar among pediatricians and pediatric emergency medicine physicians. Providers should have a high index of suspicion for signs and symptoms of barosinusitis including sinus pain, headaches, excessive lacrimation, or purulent nasal discharge in patients who recently participated in scuba diving or flying. Frontal sinusitis, blunt facial trauma, maxillofacial surgery, and intranasal substance abuse are known risk factors that can lead to PPT; however, scuba diving as a possible pathophysiology should also be considered a risk factor in the development of PPT. Because barosinusitis can be associated with potentially dangerous intracranial complications, early recognition, diagnosis, and appropriate treatment are of vital importance to reduce morbidity and mortality.
Footnotes
Disclosure: The authors declare no conflict of interest.
Contributor Information
Ami Patel, Email: ami.patel@nyumc.org.
Sharon Vuppula, Email: sharonvuppula@hotmail.com.
Harrison Hayward, Email: harrison.hayward@yale.edu.
Anisa Lakhani, Email: anisa.lakhani@mail.mcgill.ca.
REFERENCES
- 1.Taylor DM, O'Toole KS, Ryan CM. Experienced Scuba Divers in Australia and the United States Suffer Considerable Injury and Morbidity. Wilderness Environ Med. 2003;14:83–88. [DOI] [PubMed] [Google Scholar]
- 2.Battisti AS, Lark JD. Sinusitis, Barosinutis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2017. [Google Scholar]
- 3.Vaezeafshar R Psaltis AJ Rao VK, et al. Barosinusitis: comprehensive review and proposed new classification system. Allergy Rhinol (Providence). 2017;8:109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klingmann C Praetorius M Baumann I, et al. Otorhinolaryngologic disorders and diving accidents: an analysis of 306 divers. Eur Arch Otorhinolaryngol. 2007;264:1243–1251. [DOI] [PubMed] [Google Scholar]
- 5.Lynch JH, Deaton TG. Barotrauma with extreme pressures in sport: from scuba to skydiving. Curr Sports Med Rep. 2014;13:107–112. [DOI] [PubMed] [Google Scholar]
- 6.Mowatt L, Foster T. Sphenoidal sinus mucocele presenting with acute visual loss in a scuba diver. BMJ Case Rep. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buisson P, Darsonval V, Dubin J. Sinus infection and diving (a case of cerebral empyema) [in French]. Rev Laryngol Otol Rhinol (Bord). 1990;111:141–143. [PubMed] [Google Scholar]
- 8.Shemesh AJ, Panebianco NL, Chen AE. An uncommon complication of sinusitis in a young adolescent. Pediatr Emerg Care. 2015;31:531–532. [DOI] [PubMed] [Google Scholar]
- 9.Tsai BY Lin KL Lin TY, et al. Pott's puffy tumor in children. Childs Nerv Syst. 2010;26:53–60. [DOI] [PubMed] [Google Scholar]
- 10.Kombogiorgas D, Solanki GA. The Pott puffy tumor revisited: neurosurgical implications of this unforgotten entity. Case report and review of the literature. J Neurosurg. 2006;105(suppl 2):143–149. [DOI] [PubMed] [Google Scholar]
- 11.Ketenci I Unlü Y Tucer B, et al. The Pott's puffy tumor: a dangerous sign for intracranial complications. Eur Arch Otorhinolaryngol. 2011;268:1755–1763. [DOI] [PubMed] [Google Scholar]
- 12.Bambakidis NC, Cohen AR. Intracranial complications of frontal sinusitis in children: Pott's puffy tumor revisited. Pediatr Neurosurg. 2001;35:82–89. [DOI] [PubMed] [Google Scholar]
- 13.Forgie SE, Marrie TJ. Pott's puffy tumor. Am J Med. 2008;121:1041–1042. [DOI] [PubMed] [Google Scholar]
- 14.Grewal HS, Dangaych NS, Esposito A. A tumor that is not a tumor but it sure can kill! Am J Case Rep. 2012;13:133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bannon PD, McCormack RF. Pott's puffy tumor and epidural abscess arising from pansinusitis. J Emerg Med. 2011;41:616–622. [DOI] [PubMed] [Google Scholar]
- 16.Liu A Powers AK Whigham AS, et al. A child with fever and swelling of the forehead. Pott's puffy tumor and epidural abscess complicating frontal sinusitis. Clin Pediatr (Phila). 2015;54:803–805. [DOI] [PubMed] [Google Scholar]


