ABSTRACT
Introduction:
The positional relationship between the mandibular canal with impacted mandibular third molar is the main factor of inferior alveolar nerve injury. The purpose of this study was to classify the anatomical three-dimensional relationship between the proximity of impacted mandibular third molars to the inferior alveolar canal.
Methods:
The descriptive cross-sectional study was conducted in the Department of Oral and Maxillofacial Surgery of a tertiary care hospital from July 2020 to August 2020 after obtaining ethical approval from the institutional review committee (Reference number 2506202001). Cone-beam computed tomography images of 200 patients' mandibular third molars were used. A convenient sampling method was used. Data were analyzed using Statistical package for the Social Sciences.
Results:
Mandibular canal relative to the roots of the mandibular third molar was observed on the apical side in 104 (52.0%) and 173 (86.5%) third molars had direct contact with the mandibular canal. About 36 (97.3%) lingually placed mandibular third molars had contact with the mandibular canal.
Conclusions:
The findings of the study conclude that most of the mandibular third molars situated lingually had a higher occurrence of mandibular nerve involvement. The anatomic structures of the mandibular third molar and the mandibular canal may be helpful to draw upon the adequate surgical plan to avoid or reduce nerve involvement.
Keywords: anatomy, cone-beam computed tomography, inferior alveolar nerve, mandible, third molar
INTRODUCTION
The extraction of mandibular third molars is one of the most common surgical procedures done in the hospital. Ascertaining the position of impacted third molars and their contiguity with the inferior alveolar canal is of utmost importance before attempting their surgical removal to prevent the complication of an injury to inferior alveolar nerves and vessels.1
Previously, panoramic radiographs have been recommended as a primary radiographic investigation of choice. However, due to overlapping images on these x-ray films, it is difficult to judge the positional relationship precisely, especially in the buccolingual direction.2–4 With three-dimensional images, a cone-beam computed tomography (CBCT) has been widely applied in clinical work.
The study aimed to classify the three-dimensional anatomical relationship between the contiguity of impacted mandibular third molars to the inferior alveolar canal, which gives a guide to draw up the surgical plan and prevent postoperative complications.
METHODS
A descriptive cross-sectional study was conducted in the Department of Oral and Maxillofacial Surgery, Kathmandu Medical College and Teaching Hospital, Bhaktapur, Nepal from July 2020 to August 2020. The Institutional Review Committee provided ethical clearance before conducting the study (Reference number 2506202001). CBCT imaging having the presence of unilateral or bilateral impacted mandibular third molars with ipsilateral second molars were included in the study. The images having the presence of any pathology (radiolucency that might represent a cyst, tumor, or periapical lesion), and fracture, supernumerary, or impacted teeth in the region of interest (ROI) which obscure visualization of the mandibular canal was excluded. The sample was selected by convenient sampling method. Written informed consent was obtained from all participants whose CBCT images were included in the study. The sample size has been calculated using the formula,
Where,
n = required sample size
Z = 1.96 at 95% Confidence Interval
p = prevalence from previous study, 88.1%5
e = margin of error, 5%
Adding 20% of non-response rate, the sample size becomes 177.20978. However, a total of 200 participants were taken into the study.
The CBCT machine used in this study was Planmeca Promax 3D (Finland) and mandibular third molars were exposed at 90 kV and 12.0 mA for 14 seconds, and field of view (FOV) at 100 mm × 90 mm. Voxel size was 400 μm, and a slice thickness of axial images was 0.20 mm. Images were processed using PlanmecaRomexis software (Planmeca, Finland), to create axial, coronal, and sagittal reformatted images.
An oral and maxillofacial surgeon and oral radiologist under ideal viewing conditions interpreted all the CBCT images. The classification was based on the horizontal relationship between the mandibular third molar and the mandibular canal; the vertical relationship between the mandibular third molar and the mandibular canal and the integrity of the mandibular canal wall.5
Interpretation of radiographs was made cautiously for the following:
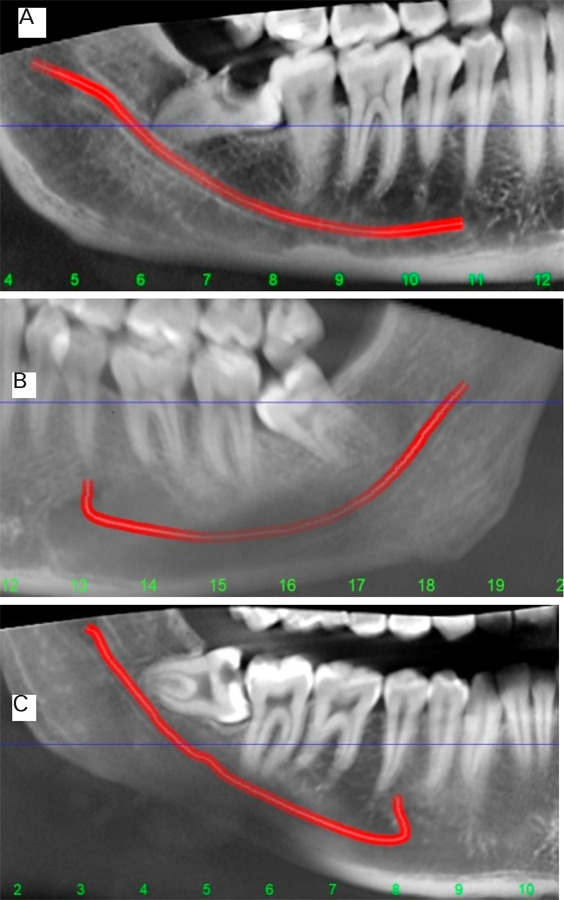
The shape of the canal was observed as;
a) Straight projection: Last part of the mandibular canal was almost at the same level as a mental foramen;
b) Catenary-like configuration: Mandibular canal curled as hanging between two points;
c) Progressive descent: Descent of mandibular canal from posterior to anterior6 (Figure 1).
Figure 1. Variation in the course of mandibular canal: A) Straight projection B) Catenary-like configuration C) Progressive descent.
The position of the mandibular canal relative to the roots of the mandibular third molar was analyzed as:
Class I: The mandibular canal on the apical side;
Class II: The mandibular canal on the buccal side;
Class III: The mandibular canal on the lingual side;
Class IV: The mandibular canal between the roots.5
Based on the mandibular third molar and the mandibular canal's contact relation, the four following conditions are grouped as:
i) Mandibular third molar not in contact with the mandibular canal;
ii) Mandibular third molar does have in contact with the mandibular canal with a complete white line;
iii) Mandibular third molar does have in contact with the mandibular canal with a defective white line;
iv) Mandibular third molar penetrates the mandibular canal.5
Data were entered in a Microsoft Excel sheet and analyzed using Statistical Package for the Social Sciences (SPSS) software version 20. Frequency and percentage were determined for descriptive statistics.
RESULTS
The study sample comprised of 200 patient's CBCT scans including images of 108 (54.0%) females and 92 (46.0%) males, ranging from 18 to 52 years (mean age 35 years).
The most common course of the mandibular canal observed was straight projection 123 (61.5%) followed by the catenary 56 (28.0%), and the remaining 21 (10.52%) had a progressive descent.
The mandibular canal's anatomic position concerning the mandibular third molar in the whole study population. Out of total 200 third molars, the mandibular canal concerning the mandibular third molars root was on the apical side 104 (52.0%) where as none of the third molars were observed between the roots (Table 1).
Table 1. Position of the mandibular canal relative to the mandibular third molar.
| Position of the mandibular canal | No-Contact | Contact | ||
|---|---|---|---|---|
| Contact with a complete white line | Contact with a defective white line | Penetration of the mandibular canal | ||
| Class I: the mandibular canal on the apical side | 14 (13) | 1 (14.4) | (2.9) | 20 (19.2) |
| Class II: the mandibular canal on the buccal side | 12 (20.3) | 22 (37.8) | 20 (33.9) | (8) |
| Class III: themandibularcanal on the lingual side | 1 (2.7) | 0 (0.0) | 14 (37.8) | 22 (9) |
| Class IV: the mandibular canal between the roots | - | - | - | - |
One hundred and seventy-three (86.5%) third molars had direct contact with the mandibular canal. Most of the individuals having mandibular canal in the lingual side had contact with the third molar 36(97.3%)(Table 2).
Table 2. Contact relation of the mandibular third molar and the mandibular canal in each class.
| Position of Mandibular canal | No Contact n (%) | Contact n (%) |
|---|---|---|
| Class I | 14 (13.5) | 90 (86.5) |
| Class II | 12 (20.3) | 47 (79.7) |
| Class III | 1 (2.7) | 36 (97.3) |
The different types of contact in Class II, and Class III. Most of the individuals with penetrating the mandibular canal 22 (81.5) had mandibular teeth located on the lingual side (Table 3).
Table 3. Different types of contact in Class II and Class III.
| Types of contact | Class II n (%) | Class III n (%) |
|---|---|---|
| Contact with a complete white line | 22 (100.0) | 0 (0.0) |
| Contact with a defective white line | 20 (58.8) | 14 (41.2) |
| Penetration of the mandibular canal | 5 (18.5) | 22 (81.5) |
DISCUSSION
The extraction of impacted third molars is the most common procedure in the specialty of oral and maxillofacial surgery. Mandibular third molars exhibit significant differences in size, shape, and path of eruption and are also the most commonly impacted teeth. Impacted teeth could give rise to different complications like pericoronitis, dental caries, resorption, abscess formation, and cellulitis, necessitating their surgical removal. The most common complications after surgery are hemorrhage, infection, edema, trismus, alveolar osteitis, ecchymosis, and nerve damage. Among this, a serious complication of surgical extraction is an injury to inferior alveolar nerve (IAN), which accounts for 0.4 to 6 of the complications.7–9 Damage to the inferior alveolar nerve occurs most frequently when the mandibular third molar and nerve roots are in direct contact.10,11 Several clinicians have suggested a CBCT before mandibular third molar extraction could reduce the prevalence of postoperative complications. Susarla and Dodson, et al.12 suggested that additional information provided by CBCT images could reduce the prevalence of paraesthesia. Pre-operational analysis and evaluation help make reasonable surgical management to avoid or reduce complications.
A panoramic radiograph is done in clinical practice before extracting the mandibular third molar to evaluate the condition and risk of IAN injury.1 However, it can be inaccurate to evaluate the relationship in the buccolingual direction.2–4 Recently, CBCT provides reimaging on axial, coronal, and sagittal sections and shows the three-dimensional structures of the teeth and surrounding tissues.3,13 The absence of cortical integrity of the mandibular canal in CBCT images suggests direct contact of the mandibular third molar with the inferior alveolar nerve and damage or exposure of the nerve after extraction.
In this study, the most common course of the mandibular canal observed was straight projection (61.5), which is less favorable for implant placement posterior to premolars. The distribution of the other two configurations in the present study was favorable for implant placement due to mental foramen was found to be higher than the canal. This finding is in contrast to the study done by Ozturk, et al. study where the most common configuration observed was a catenary-like canal present in almost one-half of the specimens.6
The current study showed that 173 (86.5) third molars had a close relationship with the mandibular canal. Of these cases, a higher percentage was seen when the mandibular canal was on the lingual side. Ghaeminia, etal.14 demonstrated an increasing potential of IAN injury when the mandibular canal is situated lingually. Thus, we may hypothesize that the lingually positioned mandibular canal is more likely to be in contact with the mandibular third molar due to insufficient space. Though the prevalence of IAN injury is low, several operation techniques have been proposed to reduce the in risk of IAN injury.
The technique of coronectomy is one of the possible alternatives to total removal for a third mandibular molar in cases of proximity to the inferior alveolar nerve.15 Orthodontic extraction is another technique that decreases the risk of IAN injury by extrusion and subsequent retrieval of high-risk mandibular third molar.16–18 The sagittal split osteotomy was considered as one of the most common operations of mandibular deformity. It was applied to removal lower third molar close to the mandibular canal.19,20
This study has some limitations. This study was done considering a small sample that might not represent scans of the whole population of Kathmandu.
CONCLUSIONS
The findings of the study conclude that most of the mandibular third molars situated lingually had a higher occurrence of mandibular nerve involvement. In this study, a three-dimensional anatomical relationship between the proximity of impacted mandibular third molars to the inferior alveolar canal and anatomic variability of the course of the mandibular canal to give guidance to draw up the surgical plan to prevent postoperative complications.
ACKNOWLEDGEMENTS
I would like to acknowledge Dr. Rajesh Twyana, Department of Oral and Maxillofacial Surgery, Kathmandu Medical College, and Teaching hospital for providing help in selecting the participants for CBCT.
Conflict of Interest
None.
REFERENCES
- 1.Smith AC, Barry SE, Chiong AY, Hadzakis D. Kha S-L, Mok SC. Inferior alveolar nerve damage following removal of mandibular third molar teeth. A prospective study using panoramic radiography. Aust Dent J. 1997 Jun;42(3):149–52. doi: 10.1111/j.1834-7819.1997.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 2.Maegawa H, Sano K, Kitagawa Y, Ogasawara T, Miyauchi K, Sekine J, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surgery, Oral Medicine, Oral Pathology. Oral Radiol Endod. 2003 Nov;96(5):639–46. doi: 10.1016/S1079-2104(03)00356-1. [DOI] [PubMed] [Google Scholar]
- 3.Monaco G, Montevecchi M, Alessandri BG, Gatto MRA, Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc. 2004;179135:312–8. doi: 10.14219/jada.archive.2004.0179. [DOI] [PubMed] [Google Scholar]
- 4.Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005 Jan;63(1):3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 5.Ozturk A, Potluri A, Vieira AR. Position and course of the mandibular canal in skulls. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Maxillofac Surg. 2012 Apr;113(4):453–8. doi: 10.1016/j.tripleo.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 6.Gu L, Zhu C, Chen K, Liu X, Tang Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone-beam computed tomography images. Surg Radiol Anat. 2018;40(6):609–14. doi: 10.1007/s00276-017-1928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003 Dec;61(12):1379–89. doi: 10.1016/j.joms.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Cheung LK, Leung YY, Chow LK, Wong MCM, Chan EKK, FokYH Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010 Apr;39(4):320–6. doi: 10.1016/j.ijom.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surgery, Oral Medicine, Oral Pathology. Oral Radiol Endodontol. 2001 Oct;92(4):377–83. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]
- 10.Al-Salehi SK, Horner K. Impact of cone beam computed tomography(CBCT) on diagnostic thinking in endodontics of posterior teeth: a before-after study. J Dent. 2016 Oct;53:57–63. doi: 10.1016/j.jdent.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Pohlenz P, Blessmann M, Blake F, Heinrich S, Schmelzle R, Heiland M. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral and maxillofacial surgery. Oral Surgery, Oral Medicine, Oral Pathology. Oral Radiology Endodontics. 2007 Mar;103:412–7. doi: 10.1016/j.tripleo.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Robinson PP, Loescher AR, Yates JM, Smith KG. Current management of damageto the inferior alveolar and lingual nerves as a result of removal of third molars. Br J Oral Maxillofac Surg. 2004 Feb;42:285–92. doi: 10.1016/j.bjoms.2004.02.024. [DOI] [PubMed] [Google Scholar]
- 13.Kipp DP, Goldstein BH, Weiss WW., Jr. Dysesthesia after mandibular third molar surgery: a retrospective study and analysis of 1,377 surgical procedures. J Am Dent Assoc. 1980 Feb;100(2):185–92. doi: 10.14219/jada.archive.1980.0074. [DOI] [PubMed] [Google Scholar]
- 14.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Berge SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg. 2009 Sep;38(9):964–71. doi: 10.1016/j.ijom.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Knutsson K, Lysell L, Rohlin M. Postoperative status after partial removal of the mandibular third molar. Swed Dent J. 1989 Jan;13(1-2):15–22. [PubMed] [Google Scholar]
- 16.Checchi L, Alessandri BG, Pelliccioni G. Removing high-risk impacted mandibular third molars: a surgical-orthodontic approach. J Am Dent Assoc. 1996 Aug;127(8):1214–7. doi: 10.14219/jada.archive.1996.0413. [DOI] [PubMed] [Google Scholar]
- 17.Ma Z-G, Xie Q-Y, Yang C, Cai XY, Li JY. An orthodontic technique for minimally invasive extraction of impacted lower third molar. J Oral Maxillofac Surg. 2013 Jun;71(8):1309–17. doi: 10.1016/j.joms.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 18.Montevecchi M, Checchi V, Bonetti GA. Management of a deeply impacted mandibular third molar and associated large dentigerous cyst to avoid nerve injury and improve periodontal healing: Case report. J Can Dent Assoc. 2012;78:59. [PubMed] [Google Scholar]
- 19.Jones TA, Garg T, Monaghan A. Removal of a deeply impacted mandibular third molar through a sagittal split ramus osteotomy approach. Br J Oral Maxillofac Surg. 2004 Aug;42(4):365–68. doi: 10.1016/j.bjoms.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 20.Kim JW, Cha IH, Kim SJ, Kim MR. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 2012 Aug;70(11):2508–14. doi: 10.1016/j.joms.2012.06.004. [DOI] [PubMed] [Google Scholar]


