Abstract
Coronavirus disease is now spreading in different countries of the world. The alarmism created through the media also creates confusion in people about virus spreading. The health care environments among which the dental practice could be places of spread of the virus, especially places where patients with systemic pathology could be exposed to this. The purpose of this article is to clarify coronavirus disease 2019 and its management in the dental practice. Only by following the normal guidelines on disinfection and sterilization of environments and operators, with some additional rules on the management of patients in the waiting room, it is possible to limit this risk. Limiting the risk of spreading the virus is one of the keys to its eradication.
Keywords: coronavirus disease 2019, infection risk, public health, dental office, virus
Introduction
Coronavirus disease 2019 (COVID-19) or acute respiratory disease from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an infectious respiratory disease caused by the virus called SARS-CoV-2 belonging to the coronavirus family. The first cases were found during the SARS-CoV-2 epidemic of 2019 to 2020. The responsible virus is believed to be of zoonotic origin, but by February 2020 the predominant mode of transmission results from man to man, generally through infected water and mucus particles (droplets) that people release by sneezing or coughing and which are then inspired by other people. Coronavirus mainly affects the lower respiratory tract and causes several symptoms described as flu-like. 1 2 3 4 5 6 7 It is transmitted mainly through close and prolonged contacts from man to man. The main symptoms are fever, cough, breathing difficulties, muscle pain, and sore throat. It has only been known for a few weeks and scientific reports on its clinical evolution knowledge are constantly updated. Currently, rapid testing is taking place with the help of nasopharyngeal, oropharyngeal swab, bronchoalveolar lavage, sputum, urine, and blood. 8 The purpose of this study is to summarize all the necessary information concerning the diffusion methods of COVID-19 and clarify the behaviors to be used.
Materials and Methods
The term personal protective equipment (PPE) refers to products that have the function of protecting the person who wears them from risks to health and safety. These devices are used in many areas, including in the workplace, home, sports, and recreation. PPE to protect the respiratory tract are used to protect against potentially harmful aeriform substances (gas, dust, and vapors) and to allow normal breathing when the oxygen level is in any case higher than the limit value of 17%. They are classified as following 9 10 11 :
Filter: as masks
Insulators: open or closed circuit.
The filters can also be classified as dustproof, antigas, or combined ( Figs. 1 2 ).
Fig. 1.
Filter mask ( http://fotoedukacja.edu.pl , CC BY-SA 3.0).
Fig. 2.
Common dental office surgical mask (CC0).
Eye protection devices are also different. The eyes are subject to various risks: splinters, hot or caustic or corrosive materials, and radiation, which can lead to three types of injuries: mechanical, optical, and thermal. To protect these delicate organs, the types of PPE are used:
Glasses
Masks
Visors
Screens
They too may or may not be equipped with a filter.
The devices for the protection of the upper limbs, particularly the hands are most exposed to risks, which can be of various kinds:
Gloves
Mechanical and electrostatic risks
Electrical risks/electrocution
Chemical and microbiological risks
Cold risks
Risks from heat and fire
Risks from vibrations
Security personal digital assistants
Paramanic and super-sleeved
The gloves can be of different materials: latex, nitrile, and vinyl. 12 13
Results
From the research performed in the literature, it is possible to summarize the guidelines for limiting and avoiding the risk of COVID-19 contagion in dental office. Here are some rules to be applied to patients to limit the risks of contagion once they arrive in the dentist’s office:
Before the patient has access to the dental office, it is mandatory to carry out a telephone triage to verify the total absence of symptoms potentially attributable to the infection by coronavirus SARS-CoV-2 such as cough, conjunctivitis, fever (even modest), sneezing, rhinitis, diarrhea, etc., and to ask for any transfers, personal trips, and/or contacts with people from areas of maximum contagion (see questionnaire). In the event of a positive answer to these questions, it should be evaluated—depending on the possible severity of the dental problem to be treated—to receive the patient at the end of the working day. Should the patient go to the office without an appointment? The secretarial staff will have to ask these same questions before the person has access to the operating areas of the study. 14 15 16 17 18
Avoid having multiple patients in the waiting room. Mandatory to maintain the recommended distance of at least 1.5 m between a person and the nearest one. Better to arrange appointments to have only one patient at a time in the waiting room.
Before having access to the operating area, the patient should have personal belongings (bags, telephones, and others) with them, the assistance staff or secretary of the office must provide a disposable bag in which to place all the objects they own at the end of the treatment session, and the patient will take care of carrying them without removing them from the container provided. It is preferable to carry out any accounting operations before the patient is invited to put his personal items in the disposable container. Before entering the operating area, the patient should be invited to wash their hands thoroughly for at least 20 seconds with specific soaps. Any further hand treatments with hydroalcoholic or chlorine-based gels are useful.
Make sure that during their stay, patients do not touch anything in the office, including door handles, surfaces, objects, etc. The secretarial accounting operations (payments, scheduling appointments, etc.) must be managed by staff of PPE. The gloves must be changed for each patient.
All study staff must always wear PPE (double pair of gloves, nonwoven headgear, and suitable mask—the type of mask to be used varies according to the patient to be treated, the type of performance, and the geographical area in which the dental office is located), disposable socks, and shirts. Before putting on disposable gloves, wash your hands thoroughly for at least 20 seconds with specific soaps and/or hydroalcoholic or chlorine-based gels. 19 Only FFP2 and 3 masks guarantee real protection from the risk of inhalation of the virus. If you find yourself operating in the red zone or on patients with suspected or confirmed infection, the operator will need to use FFP3 masks; the only ones capable of protecting against the risk of contagion linked to the aerosol that is formed during use of water spray instruments (micromotor, turbine, ultrasound, air flow, etc.). 20 21
Frequently and for a long time to change the air between one patient and another in operational studies and in the waiting room.
Scrupulously clean all study surfaces when changing each patient with hydroalcoholic (70 % ethyl alcohol) or chlorine-based disinfectants (0.1% sodium hypochlorite solutions), with particular attention to the dental unit and all surfaces with whom the patient came into contact (waiting chairs, reception desk, etc.). Surface disinfection could be performed with 0.1% sodium hypochlorite or 62 to 71% ethanol for 1 minute. 22 The most exposed surfaces will be protected with disposable barriers which, at the end of the session, must be replaced, disposing of them in special waste.
Instruct staff on how to wear, remove, and properly dispose of used PPE. The gloves must also be worn double, as can be recommended for masks, if they are normal masks. When the PPE are removed, a precise procedure must be followed: first of all, remove the first pair of gloves, then the gown, the cap, the shoes, and the masks. Finally, the glasses and protective screens, which will be cleaned with specific disinfectants. Finally, remove the second pair of gloves. All disposable personal protective equipment used will be disposed of as potentially infectious special waste.
Rinse the patient’s mouth with a 1% solution of hydrogen peroxide for 30 seconds or with 0.2 to 0.3% chlorhexidine to reduce the bacterial/viral load. It is strongly recommended to apply the rubber dam and use double suction.
Remove all potential contaminants from the waiting room (toys, consoles, newspapers, books, brochures, etc.).
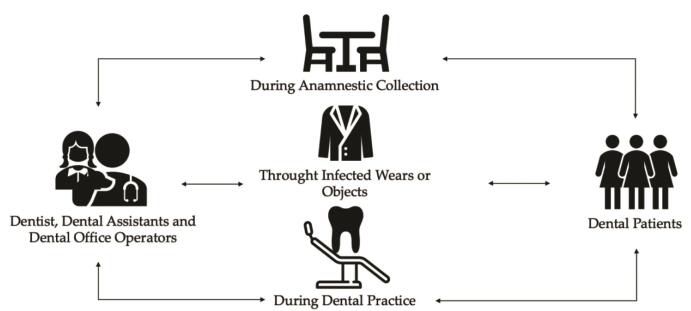
Dental patients and professionals can be exposed to pathogenic microorganisms, including viruses and bacteria that infect the oral cavity and respiratory tract. 23 24 Dental care settings invariably carry the risk of 2019-nCoV infection due to the specificity of its procedures, which involves face-to-face communication with patients, and frequent exposure to saliva, blood, and other body fluids, and the handling of sharp instruments ( Fig. 3 ). 25 Since today patients can no longer attend the dentist with the usual habit (unless urgent needs), it is necessary to maintain a high standard of oral hygiene with the constant use of a toothbrush, toothpaste, and bottle brush. The scientific community is therefore urged to spread this useful message.
Fig. 3.
Common dental office coronavirus disease 2019 transmission routes.
Discussion
Certainly, these guidelines do not represent a novelty in the medical field, and indeed reflect common standards of good conduct to be used in health care facilities. Some of the places most at risk are precisely hospitals, medical, and dental offices. Some effective generic prevention methods in medical structure are 14 26 27 28 29 30 31 :
Always change the air between one patient and another and periodically also in the waiting room.
Constantly use PPE while you are working and demand maximum attention in the use of PPE by medical and health care personnel ( Figs. 1 2 ).
Wash your hands for at least 20 seconds. The washing operation must be preliminary to the use of the disinfectant.
Clean the clinical contact surfaces (the surfaces that touch each other more frequently such as the buttons and handles) always between each patient and protect them with devices to be changed every time between the patients. The virus can reach surfaces in the form of an aerosol. Therefore, following nebulization through people (sneezing or coughing) or electromedical machinery, infection via surfaces should be considered, since the latter could remain viable and infectious for hours or days. 22
Make an alcoholic disinfectant available to patients and careers at the entrance and invite them to clean their hands before sitting down.
These are the indications for the prevention of COVID-2019 infection that are considered “more effective without incurring unnecessary and even dangerous alarms.” 6 7 The common transmission routes of novel coronavirus include direct transmission (cough, sneeze, and droplet inhalation transmission) and contact transmission (contact with oral, nasal, and eye mucous membranes). Although common clinical manifestations of novel coronavirus infection do not include eye symptoms, the analysis of conjunctival samples from confirmed and suspected cases of 2019-nCoV suggests that the transmission of 2019-nCoV is not limited to the respiratory tract, and that eye exposure may provide an effective way for the virus to enter the body ( Fig. 3 ). 12 32 33 34
In some European countries, all industry associations and trade unions suggest the temporary closure of dental practices to limit the spread of the virus. Since the dental practice is a high-risk place, as it is in contact with saliva, and possibly forms of aerosols generated by dental instruments. 35 Furthermore, these forms of aerosol cannot be blocked by the common surgical masks used in dentistry ( Fig. 2 ). The treatments and dental surgeries must be reserved for acute pain, infections such as a gingival abscess, trauma, or the results of accidental events are some examples of clinical conditions which are of an urgent nature and which must be capable of being treated. In addition, if the patient is at a greater risk of contracting infection or has symptoms attributable to COVID-19 infection or is also in quarantine, treatment will need to be postponed to a later period. Attention to coronavirus and the prevention measures adopted in some regions are triggering forms of collective psychosis that could also affect the dental practice, erroneously seen as a possible “place of spread of the virus”. 1 34 36 37 The difficulty to practice physical activity adds to the risks associated with sedentary habits, maintaining exercise routine even at home, are needed to avoid the consequences of inactivity. 38 39
Like all health care facilities, the dental practice is already equipped, the trained staff and the normal sterilization and disinfection protocols protect us operators, and our patients from far more serious infections. 40 41 42 43 44 45 46 47
The test to check coronavirus positivity also does not detect those who came into contact with the virus and who did not manifest the infection. It only detects positivity at the precise moment it is made. This is why II level tests have been performed to evaluate the presence of antibodies, which are evidence of the past presence of the virus. 28
There is still no defined therapy or therapeutic protocol. In cases where the disease is more advanced, the hospital treatment aimed at supporting vital functions, such as artificial ventilation or extra corporeal membrane oxygenation. It is important for the community to be able to contain the number of infected patients as much as possible while avoiding to create alarmism among the population. 36 48 49 50 51 52 53
Conclusion
The dental office could be a place where even debilitated patients are exposed to this risk. For this reason, following the guidelines and the strictest protocols for the disinfection of operators and environments is essential. If the number of infected decreases, hospital facilities will be freed from this excessive workload, and at the same time, the healing and immunization of other individuals may lead to the eradication of this pandemic.
NoteAuthors’ ContributionsConflict of Interest All authors have read and agreed to the published version of the manuscript.
C.D.A. and S.B. dedicated to conceptualization and methodology. R.D.S., F.G., R.M., S.M., and C.S. focused on investigation, resources, data curation, writing—original draft preparation, writing—review, and editing. G.S., G.A., C.S., D.G., and E.M.A supported in visualization. L.F. helped in project administration.
None declared.
Authors contributed equally to this study.
References
- 1.Li J O, Lam D SC, Chen Y, Ting D SW. Novel coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104(03):297–298. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 2.Jalava K. First respiratory transmitted food borne outbreak? Int J Hyg Environ Health. 2020;226:113490. doi: 10.1016/j.ijheh.2020.113490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gostic K, Gomez A CR, Mummah R O, Kucharski A J, Lloyd-Smith J O. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. eLife. 2020;9:e55570. doi: 10.7554/eLife.55570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbert M, Pullano G, Pinotti F.Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study Lancet 2020395(10227)871–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(05):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calisher C, Carroll D, Colwell R.Statement in support of the scientists, public health professionals, and medical professionals of China combatting COVID-19 Lancet 2020395(10226)e42–e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aw J. The non-contact handheld cutaneous infra-red thermometer for fever screening during the COVID-19 global emergency. J Hosp Infect. 2020;104(04):451. doi: 10.1016/j.jhin.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamid H, Khurshid Z, Adanir N, Zafar MS, Zohaib S. COVID-19 pandemic and role of human saliva as a testing biofluid in point-of-care technology 2020. Eur J Dent 2020;14(suppl S1):S123–S129 doi:10.1055/s-0040-1713020 [DOI] [PMC free article] [PubMed]
- 9.McGoldrick M. Personal protective equipment: protecting the eyes. Home Healthc Now. 2019;37(04):234–235. doi: 10.1097/NHH.0000000000000804. [DOI] [PubMed] [Google Scholar]
- 10.McGoldrick M. Personal protective equipment. Home Healthc Now. 2015;33(02):112–113. doi: 10.1097/NHH.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 11.Honda H, Iwata K. Personal protective equipment and improving compliance among healthcare workers in high-risk settings. Curr Opin Infect Dis. 2016;29(04):400–406. doi: 10.1097/QCO.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 12.Wax R S, Christian M D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(05):568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X, Zhang X, He J. Challenges to the system of reserve medical supplies for public health emergencies: reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci Trends. 2020;14(01):3–8. doi: 10.5582/bst.2020.01043. [DOI] [PubMed] [Google Scholar]
- 14.The Lancet COVID-19: fighting panic with information Lancet 2020395(10224)537. 10.1016/S0140-6736(20)30379-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spagnuolo G, De Vito D, Rengo S, Tatullo M. COVID-19 outbreak: an overview on dentistry. Int J Environ Res Public Health. 2020;17(06):2094. doi: 10.3390/ijerph17062094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mascitti M, Campisi G. Dental public health landscape: challenges, technological innovation and opportunities in the 21st century and COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(10):3636. doi: 10.3390/ijerph17103636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giudice A, Barone S, Muraca D et al. Can teledentistry improve the monitoring of patients during the COVID-19 dissemination? A descriptive pilot study. Int J Environ Res Public Health. 2020;17(10):3399. doi: 10.3390/ijerph17103399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cervino G, Oteri G. COVID-19 pandemic and telephone triage before attending medical office: problem or opportunity? Medicina (Kaunas) 2020;56(05):250. doi: 10.3390/medicina56050250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiorillo L. Chlorhexidine gel use in the oral district: a systematic review. Gels. 2019;5(02):31. doi: 10.3390/gels5020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiorillo L, Leanza T. Worldwide 3D printers against the new coronavirus. Prosthesis. 2020;2(02):87–90. doi: 10.3390/prosthesis2020009. [DOI] [Google Scholar]
- 21.Cavallo L, Marcianò A, Cicciù M, Oteri G. 3D printing beyond dentistry during COVID 19 epidemic: a technical note for producing connectors to breathing devices. Prosthesis. 2020;2(02):46–52. [Google Scholar]
- 22.Fiorillo L, Cervino G, Matarese M et al. COVID-19 surface persistence: a recent data summary and its importance for medical and dental settings. Int J Environ Res Public Health. 2020;17(09):3132. doi: 10.3390/ijerph17093132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yildirim S, Yildiz E, Kubar A. TaqMan real-time quantification of Epstein-Barr Virus in severe early childhood caries. Eur J Dent. 2010;4(01):28–33. [PMC free article] [PubMed] [Google Scholar]
- 24.Muralidharan S, Acharya A, Margabandhu S. Dentition status and treatment needs of human immunodeficiency virus-positive patients on anti retro viral therapy in Raichur taluk, Karnataka, India: a cross sectional study. Eur J Dent. 2017;11(02):238–241. doi: 10.4103/ejd.ejd_290_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health O. Infection prevention and control during health care for probable or confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: interim guidance: updated October 2019. Available at: https://extranet.who.int/iris/restricted/handle/10665/174652. Accessed 2019
- 26.Tetro J A. Is COVID-19 receiving ADE from other coronaviruses? Microbes Infect. 2020;22(02):72–73. doi: 10.1016/j.micinf.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song P, Karako T. COVID-19: real-time dissemination of scientific information to fight a public health emergency of international concern. Biosci Trends. 2020;14(01):1–2. doi: 10.5582/bst.2020.01056. [DOI] [PubMed] [Google Scholar]
- 28.Qin C, Liu F, Yen T C, Lan X. 18F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. Eur J Nucl Med Mol Imaging. 2020;47(05):1281–1286. doi: 10.1007/s00259-020-04734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phan T. Genetic diversity and evolution of SARS-CoV-2. Infect Genet Evol. 2020;81:104260. doi: 10.1016/j.meegid.2020.104260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.
- 31.Ling L, Joynt G M, Lipman J, Constantin J M, Joannes-Boyau O. COVID-19: a critical care perspective informed by lessons learnt from other viral epidemics. Anaesth Crit Care Pain Med. 2020;39(02):163–166. doi: 10.1016/j.accpm.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(01):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nastro E, Musolino C, Allegra A et al. Bisphosphonate-associated osteonecrosis of the jaw in patients with multiple myeloma and breast cancer. Acta Haematol. 2007;117(03):181–187. doi: 10.1159/000097876. [DOI] [PubMed] [Google Scholar]
- 34.Cicciù M, Risitano G, Lo Giudice G, Bramanti E. Periodontal health and caries prevalence evaluation in patients affected by Parkinson’s disease. Parkinsons Dis. 2012;2012:541908. doi: 10.1155/2012/541908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.36 signatories Alwan N A, Bhopal R, Burgess R A.Evidence informing the UK’s COVID-19 public health response must be transparent Lancet 2020395(10229)1036–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Open COVID-19 Data Curation Group . Xu B, Kraemer M UG. Open access epidemiological data from the COVID-19 outbreak. Lancet Infect Dis. 2020;20(05):534. doi: 10.1016/S1473-3099(20)30119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cervino G, Fiorillo L, Spagnuolo G et al. Interface between MTA and dental bonding agents: scanning electron microscope evaluation. J Int Soc Prev Community Dent. 2017;7(01):64–68. doi: 10.4103/jispcd.JISPCD_521_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ravalli S, Musumeci G. Coronavirus outbreak in Italy: physiological benefits of home-based exercise during pandemic. J Funct Morphol Kinesiol. 2020;5(02):31. doi: 10.3390/jfmk5020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paoli A, Musumeci G. Elite athletes and COVID-19 lockdown: future health concerns for an entire sector. J Funct Morphol Kinesiol. 2020;5(02):30. doi: 10.3390/jfmk5020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Odontoiatria33. Available at: http://www.odontoiatria33.it/approfondimenti/19017/coronavirus-le-raccomandazioni-per-lo-studio-odontoiatrico.html?xrtd=YSLXXASYSLYARCXACRPLSV&fbclid=IwAR0SpjHpFZRJ0heLDs-344uBk6RktHY6OSiW9PCmR1_imd3zT5TmyplWBmg. Accessed 2020
- 41.Cicciù M, Fiorillo L, Herford A S et al. Bioactive titanium surfaces: Interactions of eukaryotic and prokaryotic cells of nano devices applied to dental practice. Biomedicines. 2019;7(01):12. doi: 10.3390/biomedicines7010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lo Giudice G, Cicciù M, Cervino G, Lizio A, Visco A M. Flowable resin and marginal gap on tooth third medial cavity involving enamel and radicular cementum: a SEM evaluation of two restoration techniques. Indian J Dent Res. 2012;23(06):763–769. doi: 10.4103/0970-9290.111256. [DOI] [PubMed] [Google Scholar]
- 43.Cervino G, Fiorillo L, Laino L et al. Oral health impact profile in celiac patients: analysis of recent findings in a literature review. Gastroenterol Res Pract. 2018;2018:7.848735E6. doi: 10.1155/2018/7848735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cicciù M, Herford A S, Cervino G, Troiano G, Lauritano F, Laino L. Tissue fluorescence imaging (VELscope) for quick non-invasive diagnosis in oral pathology. J Craniofac Surg. 2017;28(02):e112–e115. doi: 10.1097/SCS.0000000000003210. [DOI] [PubMed] [Google Scholar]
- 45.Lo Giudice G, Lipari F, Lizio A, Cervino G, Cicciù M. Tooth fragment reattachment technique on a pluri traumatized tooth. J Conserv Dent. 2012;15(01):80–83. doi: 10.4103/0972-0707.92613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castrogiovanni P, Trovato F M, Szychlinska M A, Nsir H, Imbesi R, Musumeci G. The importance of physical activity in osteoporosis. From the molecular pathways to the clinical evidence. Histol Histopathol. 2016;31(11):1183–1194. doi: 10.14670/HH-11-793. [DOI] [PubMed] [Google Scholar]
- 47.Muscatello M R, Spina E, Bandelow B, Baldwin D S. Clinically relevant drug interactions in anxiety disorders. Hum Psychopharmacol. 2012;27(03):239–253. doi: 10.1002/hup.2217. [DOI] [PubMed] [Google Scholar]
- 48.De Stefano R. Psychological factors in dental patient care: odontophobia. Medicina (Kaunas) 2019;55(10):678. doi: 10.3390/medicina55100678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Y, Xu J, Li H, Cao B. A novel coronavirus (COVID-19) outbreak: A call for action. Chest. 2020;157(04):e99–e101. doi: 10.1016/j.chest.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang Y, Shang W, Rao X. Facing the COVID-19 outbreak: what should we know and what could we do? J Med Virol. 2020;92(06):536–537. doi: 10.1002/jmv.25720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323(13):1239-1242 doi:10.1001/jama.2020.2648 [DOI] [PubMed]
- 52.Wu J, Wu X, Zeng W et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020;55(05):257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tong Z D, Tang A, Li K F et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26(05):1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]