A bizarre situation has been created in the lives of individuals across the globe due to coronavirus disease (COVID-19)’s uncertain time and the severity of its consequences. Since December 2019, health care workers are endeavoring on effective treatment plans and implementing strategies to control the spread of the virus. Clinical symptoms of the disease vary from mild respiratory depression to severe organ failure. 1 A recently published global survey assessed the level of fear and practice modifications by dental practitioners worldwide, while it further emphasized on following guidelines by health policy departments. 2 Respiratory droplets generated during human-to-human interaction are acknowledged as the source of its transmission, hence creating an alarming situation for the health care workers as they are frontline workers, exposed to the highest viral load. 3 Excessive viral load found in the nasal cavity, oropharynx, nasopharynx, and saliva is the reason behind the highest transmission risk in a dental care. 4 5 Saliva can be an important diagnostic tool for rapid mass detection of patients based on the fact that it is an essential biomarker, used for diagnosing several viral and bacterial infections. 6
Adversity in our dental setting during this pandemic is not an exception, thus creating an immense need to adopt precautionary measures during dental practices. 3 A virus concentration of 10 /mL is found in the saliva during the early infectious period, thus augmenting the risk of cross-infection and instrument contamination. 7 In contrast, asymptomatic person makes the spread even more challenging since they carry and shed millions of virus particles.
Harrel and Molinari proposed the use of three protective coatings for health care workers which include personal protective equipment, mouthwashes, and high-speed suction instruments. 8 Preprocedural decontamination of the oral cavity is essential. The Centers for Disease Control (CDC) and Prevention guidelines acknowledged the utilization of chlorhexidine oral rinses to reduce aerosol production ( https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm ).
However, preliminary in vitro investigations spotlighted the effectiveness of chlorhexidine only against bacterial particles while it showed negligible antiviral activity. 9 Regrettably for us, little is covered in the literature regarding the antiviral properties of different available oral rinses, and the utilization of these mouthwashes is not considered in our dental practice. 10
Antecedent in vitro investigations on the severe acute respiratory syndrome coronavirus (SARS-CoV) (2002–2003) and the Middle East respiratory syndrome coronavirus (MERS-CoV) (2012–2013), the causative agents accountable for the previous pandemics in history, revealed significantly higher antiviral properties of povidone-iodine (PVP-I) mouthwashes in contrast to other oral rinses which include chlorhexidine and benzalkonium. 11 All these coronaviruses strains are coated with a lipid membrane, thus having the same structure as SARS-CoV-2. Hence, PVP-I can serve as a potential candidate to destroy the virus membrane, thus limiting its transmission. Bidra et al, in a recently conducted in vitro investigation, concluded that a 0.5% lowest concentration of PVP-I was required with a contact time of 15 seconds to eradicate SARS-CoV-2 virus successfully. 10 Eggers et al evaluated the efficacy of PVP-I formulation at 1% concentration against MERS-CoV and modified Vaccinia virus Ankara and concluded its excellent virucidal activity within 15 to 60 seconds. 12 In another investigation, they evaluated a reduction in the viral titers after 15 to 30 seconds of exposure to 0.7 and 0.23% concentration of PVP-I. 13
Earlier in June 2020, Martínez Lamas et al conducted an in vivo investigation which aimed to determine the influence of PVP-I on COVID-19 positive patients. 14 They evaluated and compared the viral loads through polymerase chain reaction testing before and after PVP-I mouth rinse. The results signified a decline in the viral load of the saliva of these COVID-19 patients after 1-minute use of PVP-I and the effects persisted for 3 hours. However, the study had limitations such as small sample size; second, there was no elimination of confounding factors which include determination of the immune response of the patient or the concentration of viral load. Hence, these factors need to be studied to evaluate a specific concentration which could be related to its clinical efficacy. Nonetheless, this study supports the fact that PVP-I can significantly aid in reducing the viral load of COVID-19 patients. 14 Sarfaraz et al, lately in a cross-sectional study, concluded that majority of dental practitioners utilized chlorhexidine oral rinses in contrast to other mouthwashes during this pandemic, thus revealing a lack of knowledge regarding the antiviral properties of PVP-I oral rinses. 15
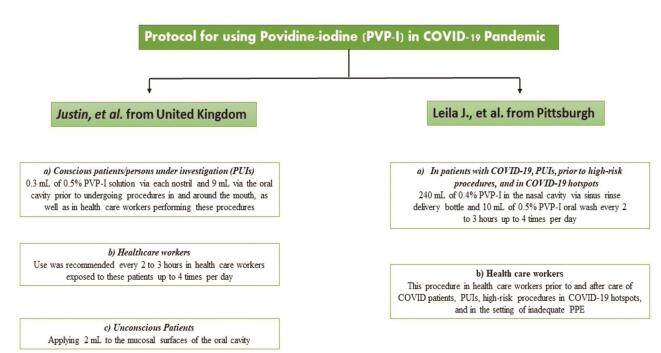
Representation of reported protocols for the use of PVP-I is illustrated in Fig. 1 so that their use can practically be implemented in a dental setting. 16 17 The American Dental Association (ADA) advised preprocedural utilization of 0.2% PVP-I to reduce transmission. Based on the literature search by Frank et al, 2.5% of PVP-I formulation can be used to decontaminate the oral cavity, keeping in mind the toxic adverse effects. 18 However, care should be taken for unconscious patients as cases of aspiration pneumonia have been reported; thus, a small amount is recommended. Second, it should also be spotlighted that PVP-I is not recommended for pregnant women or patients undergoing radioactive therapy or suffering from thyroid problems. 18
Fig. 1.
Protocols for running dental practice in the COVID-19 pandemic. 16 17
Based on these studies, we propose and urge the dental staff for preprocedural use of 0.2% PVP-I mouthwashes for 30 seconds. PVP-I is available with trade name “Betadine,” a small quantity of the mouthwash needs to be introduced and distributed into the mouth for 30 seconds, and gargles for further 30 seconds are recommended in the throat and spit after 1 minute.
PVP-I oral antiseptic rinses may offer promising results as a decontaminating agent in present COVID-19 era because of their supercilious efficacy against SARS-CoV-2 virus as indicated in the literature. Their preprocedural use is highly recommended. However, its dose-dependent toxic effects and contraindications should be evaluated before the prescription. Along with this opinion, we hope to get a translational step toward clinical practice for the use of PVP-I oral rinses.
Footnotes
Conflict of Interest None declared.
References
- 1.Wang D, Hu B, Hu C et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed M A, Jouhar R, Ahmed N et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(08):2821. doi: 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(01):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zou L, Ruan F, Huang M et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khurshid Z, Asiri F YI, Al Wadaani H. Human saliva: non-invasive fluid for detecting novel coronavirus (2019-nCoV) Int J Environ Res Public Health. 2020;17(07):2225. doi: 10.3390/ijerph17072225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamid H, Khurshid Z, Adanir N, Zafar MS, Zohaib S. COVID-19 pandemic and role of human saliva as a testing biofluid in point-of-care technology 2020. Eur J Dent 2020;14(suppl S1):S123–S129 doi:10.1055/s-0040-1713020 [DOI] [PMC free article] [PubMed]
- 7.To K K, Tsang O TY, Yip C C et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71(15):841–843. doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrel S K, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(04):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marui V C, Souto M LS, Rovai E S, Romito G A, Chambrone L, Pannuti C M. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: a systematic review. J Am Dent Assoc. 2019;150(12):1015–10260. doi: 10.1016/j.adaj.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 10.Bidra A S, Pelletier J S, Westover J B, Frank S, Brown S M, Tessema B. Rapid in-vitro inactivation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using povidone-iodine oral antiseptic rinse. J Prosthodont. 2020;29(06):529–533. doi: 10.1111/jopr.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kariwa H, Fujii N, Takashima I.Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents Dermatology 2006212(1, suppl 1)119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eggers M, Eickmann M, Zorn J. Rapid and effective virucidal activity of povidone-iodine products against Middle East respiratory syndrome coronavirus (MERS-CoV) and modified vaccinia virus Ankara (MVA) Infect Dis Ther. 2015;4(04):491–501. doi: 10.1007/s40121-015-0091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther. 2018;7(02):249–259. doi: 10.1007/s40121-018-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.
- 15.Sarfaraz S, Shabbir J, Mudasser M A et al. Knowledge and attitude of dental practitioners related to disinfection during the COVID-19 pandemic. Healthcare (Basel) 2020;8(03):232. doi: 10.3390/healthcare8030232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirk-Bayley J, Challacombe S, Sunkaraneni V, Combes J. The use of povidone iodine nasal spray and mouthwash during the current COVID-19 pandemic may protect healthcare workers and reduce cross infection. SSRN Electron J. 2020 doi: 10.2139/ssrn.3563092. [DOI] [Google Scholar]
- 17.Mady L J, Kubik M W, Baddour K, Snyderman C H, Rowan N R. Consideration of povidone-iodine as a public health intervention for COVID-19: utilization as “Personal Protective Equipment” for frontline providers exposed in high-risk head and neck and skull base oncology care. Oral Oncol. 2020;105:104724. doi: 10.1016/j.oraloncology.2020.104724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frank S, Capriotti J, Brown S M, Tessema B.Povidone-iodine use in sinonasal and oral cavities: a review of safety in the COVID-19 era Ear Nose Throat J 2020(June)1.45561320932318E14. [DOI] [PubMed] [Google Scholar]