Abstract
Background:
Asthma disproportionately impacts youth from marginalized minority backgrounds. Aspects of core asthma management (asthma management and medication beliefs) were examined among a cohort of diverse families.
Methods:
Caregiver-youth dyads (N= 92; Mage= 13.8 years; non-Hispanic/Latinx White (NLW) = 40%; Black/African-American = 25%; Hispanic/Latinx= 35%) completed a medication beliefs questionnaire (Medication Necessity, Medication Concerns) and a semi-structured interview (Family Asthma Management System Scale (FAMSS)). FAMSS subscales (Asthma Knowledge, Symptom Assessment, Family Response to Symptoms, Child Response to Symptoms, Environmental Control, Medication Adherence, Family-Provider Collaboration, and Balanced Integration) were used for analyses.
Results:
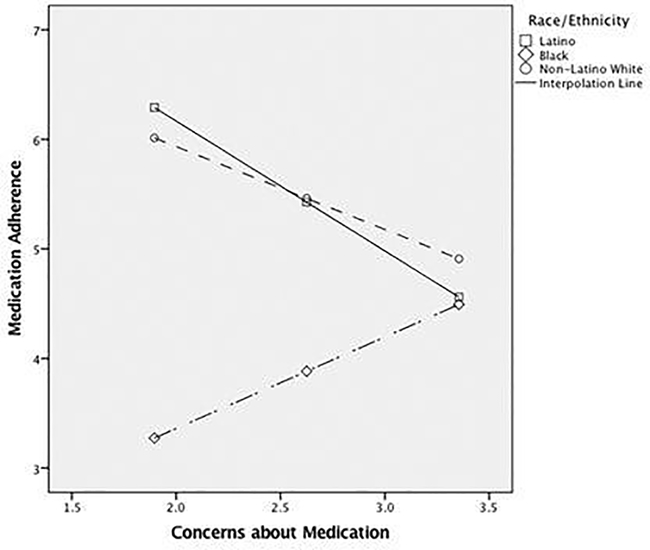
More Hispanic/Latinx families were at or below the poverty line (75%) relative to NLW (22%) and Black/African-American (39%) families (p < .001). Adherence (p< .01), Knowledge (p< .001), and Symptom Assessment (p< .01) were higher for NLW relative to Black/African-American families. Collaboration was higher among NLW (p= .01) and Hispanic/Latinx families (p= .05). Effect sizes were moderate (η2= .10 – .12). Parental race/ethnicity moderated the relationship between adherence and parental perceived medication concern and necessity for NLW and Hispanic/Latinx families. As medication concerns increased, medication adherence decreased, however, only for NLW and Hispanic/Latinx families.
Conclusions:
In this sample, racial/ethnic differences emerged for elements of asthma management. Interview-based ratings of asthma management among Black/African-American families depicted lower asthma knowledge, lower levels of family-provider collaboration, and lower medication adherence. The relationship between medication concerns and adherence appeared to differ by ethnic group. Future research is needed to elucidate cultural factors that influence family-provider relationships and health-related behaviors, like medication use/adherence.
Keywords: Adherence, Asthma, Family-Provider Collaboration, Medication Beliefs
Introduction
Childhood asthma affects 6 million children (23%) in the United States and is the most prevalent childhood chronic illness (1). In the US, asthma disproportionately affects non-Hispanic Black children (15.7%) and children of Puerto Rican descent (12.9%) relative to non-Hispanic/Latinx White (NLW) children (7.1%) (1). Black/African American children experience increased rates of asthma-related hospitalizations (1, 2), asthma morbidity and mortality (2–4), and prevalence (5, 6) when compared to their NLW counterparts. In general, asthma prevalence and asthma-related hospitalizations and missed school days have decreased since 2001, highlighting the important role that asthma education(1) and management (1, 7, 8) play in reducing health care utilization. However, recent data suggest that asthma continues to affect Black children more than their NLW and Hispanic/Latinx counterparts (1, 5) and for all groups adherence to controller medications continues to be suboptimal (~55%) (1, 9, 10). These current data highlight the continued importance of comprehensive, multicomponent education among families of children with asthma (10). While many studies have highlighted racial differences in asthma prevalence, medication beliefs, and management (11–13), the goal of the present study is to extend the current literature in two ways to provide direction for the development of more tailored interventions (14): 1) by assessing family management of asthma more comprehensively through a validated semi-structured interview, and 2) by distinguishing which aspects of asthma management may be associated with adherence and if these differ by race/ethnicity.
The National Asthma Education and Prevention Program (NAEPP) has established four key components associated with effective asthma management: a) management of allergen exposure and asthma triggers, b) assessment and monitoring of symptoms, c) patient and family continued education, and d) asthma medication knowledge and adherence (15). Thus, a number of disease management factors may contribute to racial/ethnic disparities in asthma morbidity; identifying those may pave the way to more tailored interventions. First, management and monitoring exposure to allergens (16), including environmental irritants (e.g., pollution, cigarette smoke, use of cleaning products, air fresheners), and the early identification of asthma symptoms (17) are important to reduce asthma exacerbations (18, 19). Several studies (11, 20–22) have highlighted that low-income, urban minority children have increased exposure and sensitivity to indoor/outdoor irritants relative to their NLW counterparts. Ongoing family-provider discussions of methods to reduce allergen exposure may be salient components in developing effective asthma management (12). However, under-prescription or underutilization of long-term controller medications also continues to be prevalent, particularly among minority families of children with asthma (9, 13, 14, 23). Continued asthma education and asthma medication discussions between the family and provider may establish and maintain more accurate general asthma knowledge (16, 24), medication knowledge, asthma medication beliefs (25), and improve asthma medication adherence (26).
A number of research studies have highlighted the significance of institutional barriers to healthcare on the formulation of medication beliefs, adherence, and illness management beliefs among minority families (7–9). Additionally, caregivers’/patients’ medication beliefs or misperceptions about medications can influence adherence behaviors (7–9). Specifically, concerns regarding long-term medication use (11), medication side effects (8, 12, 13), perceptions of illness (self-monitoring, feeling “okay” (7, 10)), mistrust of healthcare providers/recommendations (15), access to medication/healthcare (5), and informative resources (16) have all been shown to be important factors in developing medication beliefs. These beliefs can often impact adherence to medication and medical regimens. In one study (27), greater medication adherence and lower asthma-related healthcare utilization were associated with corresponding medication beliefs and perceptions between providers and families. Further, two recent interventions found that improved family-provider collaboration increased caregiver asthma knowledge, confidence in managing their child’s asthma, and reduced emergency department utilization (7, 28). Therefore, effective family-provider collaboration appears to be an important element in facilitating effective asthma management. Elucidating if racial/ethnic associations exist within specific asthma management components (i.e., medication adherence, asthma knowledge, asthma symptom assessment, family-provider collaboration with healthcare providers) and how medication beliefs may impact these components is needed to prepare healthcare providers to support the increasingly diverse families they may encounter in clinical practice.
We sought to examine differences in core components of asthma management among a diverse group of families of youth with asthma utilizing the Family Asthma Management System Scale (FAMSS)(26), a well-validated semi-structured interview (26) that assesses how a family integrates the management of asthma into the family system, and the Beliefs About Medications Questionnaire (29). In other studies, utilizing the BMQ, which assesses beliefs about medication necessity and concerns about taking medication, it has been found that concerns about asthma medications were independently associated with poor medication adherence (24). Specifically, NLW caregivers were more likely to have higher necessity scores (e.g., “My child’s health depends on their medication”)(17), whereas Black or Hispanic caregivers were more likely to have higher concern scores (e.g., “I worry about the side effects of my child’s medication”) (17). While all of these components may be interconnected and play a significant role in asthma management, the family-provider relationship may be particularly salient in the development and maintenance of asthma management and knowledge (19). Family-provider clinical encounters often include complex management and medication discussions. The literature has highlighted that 1) adherence is higher when families report inclusion in treatment planning (30), and 2) caregivers often prefer increased physician/healthcare provider support (25) in the adaption of daily living routines, personalized asthma education, care coordination, and medication/management plans (31). All of these studies highlight the value of interactive family-provider collaboration during the clinical encounter and recognize the salient components of an effective provider-patient relationship. Given the disparities highlighted in the literature (14, 24, 32, 33) associated with asthma management among minority families, we anticipated poorer family-provider collaboration, less asthma knowledge, and lower levels of medication adherence. We also hypothesized that caregiver beliefs about medication would vary by race/ethnicity, and more specifically that parental race/ethnicity would moderate the relationship between beliefs about medication (i.e., concern and necessity) and children’s medication adherence.
Methods and Materials
The current study includes baseline data from a prospective, observational, longitudinal study (K24 HD058794) examining asthma management and medication use among families of youth with asthma. Study protocols were approved by the institutional board at the hospital where the study was conducted. All research staff who assisted with this study were either Bachelor, Master’s, or Doctoral level research assistants or trainees who were fluent in English or bilingual (English/Spanish). Research staff were trained to administer and score the study questionnaires, including the FAMSS interview, according to established procedures (26, 34) in either English or Spanish, as applicable. The FAMSS interviews were administered and audio-recorded by a research assistant and rated immediately afterward. The participant catchment area was limited to a small state located in the New England region of the United States, which included both urban and rural areas. This was a single-site study. Participants were recruited from hospital-based ambulatory pediatric clinics, community education programs, and physician referrals. Families who expressed interest in study participation were either screened in person or by phone to confirm eligibility. All enrollees provided parental consent and child assent. Study visits were conducted in the participants’ preferred language and either at the on-site research laboratory or their home, as participants chose the location for their convenience. Study visits typically lasted 60–90 minutes as response length and questionnaire completion time varied by participant.
Participants
Eligible participants were 8th graders at enrollment; had a current mild-, moderate- or severe-persistent asthma diagnosis, and had no conditions that would otherwise prevent successful study completion (e.g., significant developmental delay). Eligible caregivers were either English- or Spanish-speaking. Caregivers and children from NLW, Hispanic/Latinx, or Black/African American racial/ethnic backgrounds were recruited. Of the 222 families screened, 108 (48.7%) did not meet study criteria for the following reasons: no persistent asthma (n = 21) or current symptoms (n = 10), out of age range (n = 67), or other (e.g., no asthma medications prescribed, cognitive delay; n = 10). Fifteen families (6.8%) were deemed eligible but 12 (5.4%) were never enrolled and 3 (1.4%) did not complete study participation. Failure to complete the study, lack of interest in continued participation, or insufficient time to commit to the study were reasons for withdrawal. Our final sample included 99 parent-child dyads. Due to missing or incomplete FAMSS interviews, only 92 were included in the present study.
Measures
Demographics.
Primary caregivers provided key demographic information (e.g., ethnicity, race, age, education, and poverty status). Among participants who identified as Hispanic/Latinx, additional information was obtained about language preferences (Spanish vs. English) and ethnic origin. To determine participant poverty status, family household per capita income was compared to the US federal poverty threshold for a family of that size in the year that the family participated in the study (35).
Asthma Specific Allergens, Barriers to Care and Health Care Utilization.
All participants completed a brief measure of health care utilization (i.e., number of doctor visits, emergency department visits), barriers to healthcare (e.g., buying medications and attending doctor appointments), and asthma specific allergens over the past 12 months. Families also answered questions about common allergies and were asked to check yes or no for which allergens exacerbate their child’s asthma. Summary statistics including means and frequencies were calculated.
Beliefs about Medication Questionnaire (BMQ) (36).
Beliefs about asthma medications were assessed using the BMQ. In the present study, beliefs about medication were defined as the necessity of medication to control asthma symptoms (14) and specific concerns about taking asthma medication (37). This questionnaire includes two five-item scales, one that assesses parental beliefs about the necessity of medication (Medication Necessity) for controlling their child’s asthma, and the other that evaluates parental concerns (Medication Concerns) about the child taking asthma medication. Each individual item is rated via a 5-point Likert scale, with 1 ‘Strongly Agree’ and 5 ‘Strongly Disagree’. High scores on the Necessity subscale indicates a stronger positive belief regarding the necessity of medications, and high scores on the Concerns subscale indicates more parental concerns about their child using asthma medication. The BMQ has been used previously in studies of parents of children with asthma (14, 18, 37). Internal consistency estimates of necessity and concerns scales are good to excellent for both English (α = 0.82 and 0.75, respectively) and Spanish versions (α = 0.82 and 0.74, respectively) (14, 18, 37). In the present study, internal consistency estimates of necessity (α = .80 English and α = .81 Spanish) and concerns (α = .71 English and α = .65 Spanish) were excellent to good, respectively. BMQ questionnaire items and other psychometric proprieties are published elsewhere (29).
Family Asthma Management System Scale (FAMSS; FAMSS; 26).
The FAMSS is a well-established semi-structured interview used to assess several domains of asthma management (34). The interview is rated on seven 9-point subscales that tap various domains of asthma management, with higher scores indicating better management (34). Open-ended questions assess the family’s management of their child’s asthma across seven subscales: 1) Asthma Knowledge, 2) Symptom Assessment, 3) Family and Child Response to Symptoms, 4) Environmental Control, 5) Medication Adherence, 6) Family-Provider Collaboration, and 7) Balanced Integration. In this study, the interview was recorded and coded using a standardized manual. The FAMSS has been well-validated across multiple pediatric asthma samples including racially and culturally diverse children (26).The FAMSS summary score is the mean of the ratings on the constituent subscales. More information about the FAMSS and FAMSS subscale development as well as other psychometric proprieties are published elsewhere (26). Family Asthma Management System Scale (FAMSS; FAMSS; 26). The FAMSS is a well-established semi-structured interview used to assess several domains of asthma management (34). The interview is rated on eight 9-point subscales that tap various domains of asthma management, with higher scores indicating better management (34). Open-ended questions assess the family’s management of their child’s asthma across seven subscales: 1) Asthma Knowledge, 2) Symptom Assessment, 3) Family Response to Symptoms, 4) Child Response to Symptoms, 5) Environmental Control, 6) Medication Adherence, 7) Family-Provider Collaboration, and 8) Balanced Integration. The interview is recorded and coded using a standardized manual. The FAMSS has been well-validated across multiple pediatric asthma samples including racially and culturally diverse children (38).The FAMSS summary score is the mean of the ratings on the constituent subscales. More information about the FAMSS and FAMSS subscale development as well as other psychometric proprieties are published elsewhere (26, 34).
FAMSS Subscales.
The Asthma Knowledge subscale includes items about the family’s/child’s general knowledge of asthma, such as basic understanding of the disease, and knowledge about prescribed asthma medications. The Symptom Assessment subscale evaluates parent and child awareness of asthma exacerbation, specifically noting early warning signs, symptom patterns, and levels of symptom urgency. (e.g., How easy is it for you two [child and parent] to tell when child is having breathing problems). The Family Response to Symptoms subscale includes strategies the family has previously determined to manage asthma symptoms and exacerbations (e.g., What happens when you start to have asthma symptoms and you’re with your family). The Child Response to Symptoms is similar but evaluates how well the child manages asthma when an adult is not available.. The Environmental Control subscale measures the extent to which exposure to environmental tobacco smoke, pets and pests, and other triggers of asthma are controlled (e.g., Does anyone who smokes live in the home?) in the household. The Medication Adherence subscale is a summary of adherence to controller medications and access/use of quick-relief medications when needed (e.g., How do you keep track of what medicine your child needs at what time? How frequently do you realize you don’t have your quick-relief medicine with you when you need to use it?). The Family-Provider Collaboration subscale assesses the family’s relationship with the identified health care provider, including communication and agreement regarding treatment, (e.g., How often do you ask your child’s doctor questions?). Lastly, the Balanced Integration subscale assesses the balance of attention to asthma management and family-related concerns (e.g., school attendance, extracurricular family activities).
Data Analytic Plan
Initial probes examined differences in key study variables by race/ethnicity. First, Chi-square (χ2) analyses were utilized to examine differences in socioeconomic status by ethnic group. Additional Chi-square analyses were conducted to examine racial/ethnic differences in health care utilization and other key asthma management variables. Analyses of variance (ANOVA) models were employed to examine differences in FAMSS subscales across each racial/ethnic group. ANOVA effect sizes are expressed as eta-squared (η2), interpreted as small (η2 =0.2), medium (η2 =0.5), or large (0.26; 0.26; 39). Next, descriptive statistics and intercorrelations of significant variables identified via ANOVA and covariates (age, sex, asthma severity) were examined prior to conducting moderation analyses to further investigate significant ANOVA findings. Lastly, exploratory independent-samples t-tests were conducted to compare potential differences in asthma management among English- vs. Spanish-speaking Hispanic/Latinx families. All analyses were conducted in SPSS version 24.
Results
Demographic Characteristics.
Participant characteristics appear in Table 1. The current sample includes 92 youth with asthma aged 12–14 years, with a mean age of 13.8 (SD=0.6; 60% male). Forty percent of the sample identified as NLW, 25% as Black/African-American, and 35% as Hispanic/Latinx. The majority of Hispanic/Latinx participants were Dominican (n = 14), Puerto Rican (n = 13), or Guatemalan (n = 3). Four families did not wish to provide information about racial/ethnic origin. Forty five percent of the total sample (n=41) were at or below the national poverty threshold. Hispanic/Latinx families were more likely to be living at or below the poverty line (75%) relative to NLW (22%) and Black (39%) families (X2 = 20.16, p < .001).
Table 1.
Demographic, Socioeconomic, and Asthma Management Variables.
| Variable | Racial/Ethnic Group | ||
|---|---|---|---|
| Non-Hispanic/Latinx White | Hispanic/Latinx | Black | |
| n = 39 (39%) | n = 34 (34%) | n = 26 (26%) | |
| Relationship to Child | |||
| Mother | 38 (97%) | 33 (97%) | 23 (89%) |
| Caregiver Education (Mother) | |||
| High School Equilivent or Less | 5 (13%) | 14 (41%) | 10 (39%) |
| Some College | 15 (38%) | 17 (50%) | 11 (42%) |
| College Graduate | 10 (26%) | 2 (6%) | 3 (12%) |
| Graduate or Profressoinal School | 8 (21%) | 0 | 0 |
| Missing/Refused | 1 (3%) | 2 (8%) | |
| Child Age (Years) | M = 13.8 (SD = .5) | M = 13.8 (SD = .6) | M = 13.7 (SD = .6) |
| Child Sex (Male) | 24 (62%) | 21 (62%) | 16 (62%) |
| Language Preference | |||
| English | 39 (100%) | 15 (44%) | 26 (100%) |
| Spanish | ----- | 19 (56%) | ----- |
| Child Asthma Severity | |||
| Mild intermittent | 2 (5%) | 4 (12%) | 2 (8%) |
| Mild Persistent | 15 (39%) | 14 (41%) | 8 (31%) |
| Moderate Persistent | 16 (41%) | 13 (38%) | 11 (42%) |
| Severe | 6 (15%) | 3 (9%) | 5 (19%) |
| Caregiver Marital Status | |||
| Married | 31 (80%) | 11 (32%) | 5 (19%) |
| Separated | 1 (3%) | 2 (6%) | 4 (15%) |
| Divorced | 3 (8%) | 12 (35%) | 6 (23%) |
| Never Married | 3 (8%) | 9 (27%) | 10 (39%) |
| Family Poverty Status | |||
| At or Below Poverty Threshold | 8 (21%) | 24 (71%) | 9 (35%) |
| Above Poverty Threshold | 29 (74%) | 8 (24%) | 14 (54%) |
| Parent Reported Environmental Triggers | |||
| Allergens | 16 (41%) | 19 (56%) | 17 (65%) |
| Pollen | 29 (74%) | 26 (77%) | 22 (85%) |
| Mold | 22 (56%) | 20 (59%) | 18 (69%) |
| Tobacco Smoke | 27 (69%) | 29 (85%) | 22 (85%) |
| Seasonal Weather Changes | 32 (82%) | 26 (77%) | 23 (89%) |
| Strong Odors | 16 (41%) | 22 (65%) | 16 (62%) |
| Home Tobacco Smoke Exposure | 3 (8%) | 3 (9%) | 6 (23%) |
| Barriers to Care | |||
| Buying Perscription Medicines | |||
| Never | 1 (3%) | 3 (9%) | 4 (17%) |
| Sometimes | 5 (14%) | 9 (28%) | 2 (9%) |
| Always | 27 (73%) | 13 (41%) | 12 (52%) |
| Missing | 2 (5%) | 7 (23%) | 4 (17%) |
| Doctor Appointments | |||
| Never | 1 (3%) | 2 (6%) | 2 (9%) |
| Sometimes | 3 (8%) | 6 (19%) | 4 (17%) |
| Always | 29 (78%) | 18 (56%) | 13 (57%) |
| Missing | 2 (5%) | 6 (19%) | 4 (17%) |
| Health Care Utilization | |||
| Number of Hospitalizations | M = .36 (SD =1.0) | M = .24 (SD .66) | M = .27 (SD = .67) |
| Nukber of Emergengy Room Visits | M = 1.3 (SD = 4.8) | M = .79 (SD = 1.1) | M = 1.1 (SD = 2.1) |
| Number of Doctor Sick Visits | M = 4.1 (SD = 9.9) | M = 2.52 (SD = 4.0) | M = 2.9 (SD = 3.5) |
| Missed School Due to Asthma | M = 6.7 (SD = 12.5) | M = 5.5 (SD = 8.1) | M = 2.8 (SD = 3.7) |
Note. M = mean, SD = standard deviation.
Differences in Asthma Management by Racial/Ethnic Group.
Barriers to Care and Health Care Utilization.
No differences were observed by racial/ethnic group related to barriers to care (buying medicines χ2 (2, n = 80) = 4.84, p = .09; attending doctor visits χ2 (2, n = 82) =1.89, p = .39). Interestingly, and regardless of racial/ethnic group, 89% (n = 73) of families indicated difficulties in attending medical visits, and 85% (n = 68) indicated difficulties in buying prescription medications. No differences were observed for any healthcare utilization variables by racial/ethnic group (doctor visits: F (2, 88) = .42, p = .66; emergency department visits: F (2, 88) = 1.81, p = .86; hospitalizations: F (2, 88) = .13, p = .88). Although not significantly different, for all healthcare utilization variables, NLW families indicated the highest frequency of utilization across racial/ethnic groups. Frequencies of all variables are reported in Table 1.
Asthma Specific Allergens and Household Tobacco Exposure.
No ethnic group differences were observed for any parent-reported asthma-specific allergen triggers (pollen χ2 (4, n = 89) = 1.79, p = .77; mold χ2 (4, n = 89) = 4.85, p = .30; seasonal weather changes χ2 (4, n = 89) = 4.59, p = .33; strong odors χ2 (4, n = 89) = 5.79, p = .22). Additionally, no ethnic group differences were observed in tobacco smoke exposure (χ2 (2, n = 90) = 4.78, p = .11), with the majority of families indicating no household tobacco smoke exposure (n = 78, 85%).
FAMSS Subscale Models.
ANOVA models were used to explore potential sociocultural differences in asthma management (Tables 2 and 3 contain descriptive statistics and intercorrelations). Among all racial/ethnic groups in the present study NLW, Hispanic/Latinx, Black/African-American), no differences were observed for FAMSS scales of Family Response to Symptoms, Child Response to Symptoms, Environmental Control, or Balanced Integration. Similarly, there were no differences in BMQ subscales of Medication Necessity and Medication Concerns. Racial/ethnic differences were observed in a number of other management variables, including Asthma Knowledge (F (2, 85) = 4.91, p= .01), Symptom Assessment (F (2, 86) = 5.36, p< .01), Medication Adherence (F (2, 85) = 6.06, p< .01), Family-Provider Collaboration (F (2, 86) = 4.52, p= .01), and the FAMSS Total Score (F (2, 86) = 5.55, p< .01). Post-hoc comparisons indicated Asthma Knowledge, Symptom Assessment and Medication Adherence were higher for NLW families relative to Black/African-American families (Asthma Knowledge, Mdifference = 1.23; p< .001; Symptom Assessment, Mdifference = 1.17; p< .01; Medication Adherence, Mdifference= 1.74; p< .01;). Family-Provider Collaboration was higher for NLW (Mdifference = 1.09; p= .01) and Hispanic/Latinx families (Mdifference = .93; p= .05) relative to Black/African-American families. Lastly, both NLW and Hispanic/Latinx FAMSS Total Scores were higher (NLW, Mdifference = .95, p< .01; Hispanic/Latinx Mdifference = .83, p= .02) relative to Black/African-American families. Effect sizes were moderate across all ANOVA findings (η2= .10 – .12).
Table 2.
ANOVA Summary of Differences in Asthma Management and Medication Beliefs.
| FAMSS Subscale | F | Effect Size | M (SD) | ||
|---|---|---|---|---|---|
| Hispanic/ Latinx | Black | Non-Hispanic/Latinx White | |||
| FAMSS Subscale | |||||
| Asthma Knowledge | 4.91** | .10 | 5.8 (1.6) | 5.2 (1.5) | 6.4 (1.3) |
| Symptom Assessment | 5.36** | .11 | 6.0 (1.3) | 5.1 (1.5) | 6.3 (1.5) |
| Family Response to Symptoms+ | 2.85 | .06 | 5.4 (1.5) | 5.3 (1.9) | 6.2 (1.7) |
| Child Response to Symptoms + | 2.12 | .04 | 4.5 (1.8) | 4.1 (1.7) | 5.1 (2.1) |
| Environmental Control | 1.73 | .04 | 4.5 (2.8) | 3.2 (2.5) | 3.6 (2.4) |
| Medication Adherence | 6.06** | .12 | 5.1 (1.8) | 3.9 (2.0) | 5.7 (1.9) |
| Family-Provider Collaboration | 4.52** | .10 | 5.8 (1.2) | 4.9 (1.5) | 6 (1.5) |
| Balanced Intregration | 0.86 | .02 | 5.4 (1.8) | 4.8 (1.8) | 5.0 (2.0) |
| FAMSS Total Score | 5.55** | .11 | 5.4 (.99) | 4.6 (1.1) | 5.6 (1.2) |
| Beliefs about Medication Questionnaire | |||||
| Medication Necessity | 1.06 | .02 | 3.3 (.96) | 3.1 (.88) | 3.0 (.86) |
| Medication Concerns | 2.34 | .05 | 2.4 (.80) | 2.2 (.70) | 2.0 (.59) |
Note.
Significant at p ≤ .01. NLW = Non-Hispanic/Latinx White. M = mean, SD = standard deviation. ANOVA F = variation between sample means / variation within the samples.
= Family and Child Response to Symptoms are similar subscales but the Child Response to Symptoms evaluates how well the child manages asthma when an adult is not available.
Table 3.
Intercorrelations of Significant ANOVA FAMSS Subscales.
| Variable | 1 | 2 | 3 | 4 | 5 | Child Age | Child Sex | Child Asthma Severity | Poverty Status | Medication Concerns | Medication Necessity |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | (.87) | ||||||||||
| 2 | .70** | (.87) | |||||||||
| 3 | .45** | .44** | .(87) | ||||||||
| 4 | .53** | .45** | .41** | .(87) | |||||||
| 5 | .64** | .68** | .65** | .67** | (.87) | ||||||
| Child Age | −.02 | −.10 | −.10 | −.01 | −.06 | - | |||||
| Child Sex | .11 | .004 | .02 | −.13 | −.05 | −.18 | - | ||||
| Child Asthma Severity | .10 | .07 | .09 | .06 | .05 | .03 | .14 | - | |||
| Poverty Status | .17 | .08 | −.01 | −.01 | −.02 | .20 | −.06 | .23* | - | ||
| Medication Concerns | −.20* | −.17 | −.11 | −.09 | −.10 | .15 | .07 | .31** | .16 | - | |
| Medication Necessity | .06 | .04 | .12 | .11 | −.04 | .11 | .07 | .42** | .16 | .36** | - |
Note. Entries on the main diagonal are standardized Cronbach’s alpha. 1 = Asthma Knowledge; 2 = Symtpom Assessment; 3 = Medication Adherence; 4 = Collaboration with Health Care Providers; 5 = FAMSS Total Score.
p < .05
p < .001.
To test the hypothesis that parental beliefs about medication varied by race/ethnicity, and more specifically that parental race/ethnicity moderated the relationship between beliefs about medication (i.e., BMQ subscales Medication Necessity and Medication Concerns) and Medication Adherence (as rated in the FAMSS), a hierarchical multiple regression analysis was conducted. Conditional process modeling was used as outlined by Hayes (40) via the PROCESS macro and bootstrapped to 5,000 samples. In the first step, two variables were included: Medication Concerns and race/ethnicity. These variables accounted for a significant amount of variance in Medication Adherence to the child’s asthma medications (R2 = .48, F (5, 82) = 4.96, p = .005). Next, the interaction term between Medication Concerns and parental race/ethnicity was added to the regression model, which accounted for a significant proportion of the variance in Medication Adherence to the child’s asthma medications(ΔR2 = .08, ΔF(2, 82) = 4.32, p = .02, b = 2.02, t(82) = 2.82, p = .006). Examination of the interaction plot revealed that as Medication Concerns increased, Medication Adherence decreased for Hispanic/Latinx and NLW (see Figure 1). No significant differences were observed for Black/African-American families. Beliefs about Medication Necessity were not associated with any covariates (age, sex, asthma severity).
Figure 1.
Signficant Moderation of FAMSS Asthma Medication Adherence and Medication Beliefs by Caregiver/Child Ethnicity/Race.
Note. Moderation analyses were bootstrapped to 5,000 samples.
FAMSS English- vs. Spanish- speaking Hispanic/Latinx Participants.
No differences were observed for FAMSS scales of Asthma Knowledge, Symptom Assessment, Family Response to Symptoms, Child Response to Symptoms, Medication Adherence, Family-Provider Collaboration, or the FAMSS Total Score. Similarly, there were no differences in BMQ Medication Concerns. Spanish-speaking families reported higher Environmental Control (M = 5.81, SD = 2.29, t(30) = 3.06, p = .005), and Balanced Integration (M = 6.07, SD = 1.39, t(30) = 2.09, p = .05) than English-speaking families (Environmental Control M = 3.07, SD = 2.71; Balanced Integration (M = 4.80, SD = 1.90). Lastly, English-speaking families indicated higher scores regarding asthma Medication Necessity (M = 3.72, SD = .88) than Spanish-speaking families (M = 2.98, SD = .91, t(30) = 2.36, p = .03).
Discussion
In this sample of families of children with asthma, no significant differences in the child’s asthma allergen exposure, utilization of healthcare services, or barriers to care (medication purchasing, doctor visits) were observed across racial/ethnic groups. Key differences did emerge among several domains of core asthma management. First, Asthma Knowledge, Symptom Assessment, and Medication Adherence were higher for NLW families relative to Black/African-American families. Second, Family-Provider Collaboration was higher for NLW and Hispanic/Latinx families relative to Black/African-American families. Lastly, parental beliefs about medication differed by racial/ethnic group, such that as concerns about medication increased, adherence decreased for Hispanic/Latinx and NLW child participants. These findings are consistent with previous literature highlighting racial/ethnic differences in the management of childhood asthma (14, 33, 41). This study, however, builds on previous literature by disentangling those aspects of core asthma management in children that may be more salient for different racial/ethnic groups. The association between Medication Concerns among Hispanic/Latinx families may reflect cultural or personal perceptions about medication side effects (14, 18) and general medication concerns, which would be similar to other studies utilizing the BMQ in the pediatric asthma literature (8, 14, 18, 42). For example, in one study, Spanish-speaking parents reported a lack of knowledge regarding appropriate responses to their child’s asthma exacerbations and lack of information about how or why it is important to alter the home environment to reduce their child’s exposure to allergens (43). Consistent with the literature, in the present study, Spanish-speaking families reported higher levels of environmental control (e.g., managing child’s exposure to allergens), balanced integration (e.g., the extent to which families were able to integrate illness management into their everyday lives), and lower scores regarding necessity of asthma medications (e.g., perceptions that medications are important to manage/treat their child’s asthma) than English-speaking families. While overall (across all Hispanic/Latinx participants) adherence scores appeared to decline with increased concerns about medication, more research is needed to determine which specific concerns regarding medication (e.g., concerns about long term effects) are predictors of medication adherence, what variables may drive these associations, and if these concerns could be addressed through targeted interventions.
Interestingly, adherence was not associated with medication beliefs for Black/African-American families in this sample, despite similar scores of medication necessity (average score range = 3.0 – 3.3) and concerns (average score range = 2.0 – 2.3) for each racial/ethnic group (see Table 2). One factor that may be driving this association is that Black/African-American families were rated as having significantly lower adherence (M = 3.9) when compared to Hispanic/Latinx (M = 5.1) and NLW families (M = 5.7). Asthma disparities among Black/African-American children are well documented in the literature (44–46) and Black/African-American families may encounter explicit or implicit bias in healthcare settings, which may affect their perception of their healthcare provider and their ability to collaborate with them (13, 47, 48). Previous studies have identified that Black/African-American children were less likely to be seen by a doctor for their asthma, (44, 46), were less likely to receive a written treatment plan (44, 45), and that many parents and physicians of minority children often underestimate the severity of their child’s asthma due to cultural or family-provider communication difficulties (44). Specifically, Haywood and colleagues identified that when patients experience discrimination and report distrust toward their healthcare provider, they are more likely to report nonadherence to physician recommendations (48). Thus, perceptions about medication concerns and the necessity of medication may not be as salient as other family-level variables (e.g., family connectedness, psychosocial stressors) and contextual variables (e.g., neighborhood stress and environment, perceived discrimination in health care) not measured in this study. In order to further substantiate these findings, future studies should incorporate longitudinal designs assessing the core components of asthma management and medication beliefs, with repeated assessments, to determine whether changes in beliefs or asthma management precede and predict medication adherence.
Clinical Implications
The present study observed different domains of asthma management that may be important factors to consider when assessing adherence among families of youth with asthma. In order to reduce racial and ethnic disparities in asthma morbidity, it is important to tailor asthma management strategies and recommendations in a manner that addresses the unique concerns of caregivers and families, particularly among those from diverse cultural and ethnic backgrounds (18). Ongoing asthma education and assessment of the asthma management plan may be an important strategy to improve family-provider collaboration and adherence to asthma management recommendations (28). Our data suggest that medication adherence, asthma knowledge, family-provider collaboration, and symptom assessment may differ across racial/ethnic groups, and when some parents experience concerns about medication, these concerns may impact adherence to their child’s medical regimen. Taken together, our findings highlight the need to develop interventions that target specific aspects of asthma management (for example, providing education to enhance beliefs about medication necessity and dispelling concerns to support improved medication adherence). Similarly, providing culturally responsive training to healthcare providers may work to enhance family-provider collaboration, which in turn could support medication adherence.
The present study is not without limitations. First, the data presented here are cross-sectional and provide only a snapshot of the families’ asthma management behaviors. Second, the data are comprised of a relatively small sample size (N = 92), with small subgroups of each race/ethnicity. Thus, significant findings should be replicated with larger sample sizes and longitudinal data. Third, other influential variables associated with the healthcare system (e.g., healthcare provider role or specialty, healthcare provider ethnicity, cultural competence, health literacy, perceived discrimination) were not assessed in the present study (26, 34), and it is possible that other cultural, interpersonal, familial attitudes or behaviors may drive these identified associations. Future studies that incorporate the use of family, patient, and provider responses are needed to further assess the associations highlighted in the present study. Lastly, this study does not include information about medical providers’ primary language spoken or medical record review of the presence of an asthma action plan. Studies examining the relationship between provider language and families’ perceptions of care as well as the language and presence of a provider-initiated action plan are needed to further examine the associations highlighted in this study. Despite these limitations, the present study provides important insight into the complexity of asthma management and perceptions of medication beliefs with a diverse sample by distinguishing which aspects of asthma management may be associated with adherence.
Conclusions
Families of children with asthma often face a multitude of barriers including adherence to medication (12), multiple clinical appointments, variations in asthma severity due to environmental exposures (49), and access to resources (5, 33). In this study, we highlight the role of family-provider collaboration, asthma knowledge, and medication beliefs on medication adherence in ethnically diverse families. In this sample, interview-based ratings showed that Black/African-American families had lower levels of asthma knowledge, lower levels of family-provider collaboration, and lower medication adherence relative to NLW and Hispanic/Latinx families. Interestingly, for NLW and Hispanic/Latinx families, low medication concerns were associated with higher adherence; however, as medication concerns increased, medication adherence also decreased. Future research is needed to elucidate other factors that influence the relationships between race/ethnicity, family-provider relationships, and health-related beliefs. This includes utilizing state-provided services to elucidate and eliminate environmental triggers(50), more frequent reviews and evaluations of asthma knowledge/education(51), provision of action plans in preferred languages(52), and the inclusion of language-specific asthma clinics.
Acknowledgments
Funding:
Hassenfeld Child Health Innovation Institute and K24HD058794 (McQuaid, PI); F32HL138734 (Tackett, PI)
Footnotes
Conflict of Interest:
The authors report no conflict of interest.
References
- 1.Zahran HS, Bailey CM, Damon SA, Garbe PL, Breysse PN. Vital Signs: Asthma in Children - United States, 2001–2016. MMWR Morb Mortal Wkly Rep 2018; 67: 149–155 10.15585/mmwr.mm6705e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck AF, Huang B, Auger KA, Ryan PH, Chen C, Kahn RS. Explaining racial disparities in child asthma readmission using a causal inference approach. JAMA Pediatr 2016; 170: 695–703 10.1001/jamapediatrics.2016.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health 2005; 26: 89–113 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 4.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief 2012: 1–8 [PubMed] [Google Scholar]
- 5.Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics 2016; 137: 1–7 10.1542/peds.2015-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National Health Statistics Reports 2011: 1–14 [PubMed] [Google Scholar]
- 7.Lou Y, Atherly A, Johnson T, Anderson M, Valdez C, Sabalot S. The impact of care management for high-risk pediatric asthmatics on healthcare utilization. J Asthma 2019: 1–8 10.1080/02770903.2019.1659311. [DOI] [PubMed] [Google Scholar]
- 8.McQuaid EL. Barriers to medication adherence in asthma: The importance of culture and context. Annals of Allergy, Asthma & Immunology 2018; 121: 37–42 10.1016/j.anai.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Lintzenich A, Teufel RJ, Basco WT Jr. Under-utilization of controller medications and poor follow-up rates among hospitalized asthma patients. Hospital pediatrics 2011; 1: 8–14 10.1542/hpeds.2011-0002. [DOI] [PubMed] [Google Scholar]
- 10.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: A multilevel challenge. JACI 2009; 123: 1209–1217 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rastogi D, Reddy M, Neugebauer R. Comparison of patterns of allergen sensitization among innercity Hispanic and African American children with asthma. Ann Allergy Asthma Immunol 2006; 97: 636–642 [DOI] [PubMed] [Google Scholar]
- 12.Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MCJM, Verhamme KMC. : Medication adherence and the risk of severe asthma exacerbationsA systematic review. 2015; 45: 396–407 10.1183/09031936.00075614. [DOI] [PubMed] [Google Scholar]
- 13.McQuaid EL, Landier W. Cultural issues in medication adherence: Disparities and directions. J Gen Intern Med 2018; 33: 200–206 10.1007/s11606-017-4199-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McQuaid EL, Vasquez J, Canino G, Fritz GK, Ortega AN, Colon A, Klein RB, Kopel SJ, Koinis-Mitchell DK, Esteban CA, Seifer R. Beliefs and barriers to medication use in parents of Latino children with asthma. Pediatr Pulmonol 2009; 44: 892–898 10.1002/ppul.21074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. Bethesda MD: US Department of Health and Human Services, National Institutes of Health; 2007. [Google Scholar]
- 16.Asthma and Allergy Foundation in America. Ethnic disparities in the burden and treatment of asthma. Washington, DC; 2005. [Google Scholar]
- 17.Conn KM, Halterman JS, Lynch K, Cabana MD. The impact of parents’ medication beliefs on asthma management. Pediatrics 2007; 120: 521–526 10.1542/peds.2006-3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McQuaid EL, Fedele DA, Adams SK, Koinis-Mitchell D, Mitchell J, Kopel SJ, Seifer R, Jandasek B, Fritz GK, Canino G. Complementary and alternative medicine use and adherence to asthma medications among Latino and non-Latino white families. Acad Pediatr 2014; 14: 192–199 10.1016/j.acap.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halterman JS, Yoos HL, Kaczorowski JM, McConnochie K, Holzhauer RJ, Conn KM, Lauver S, Szilagyi PG. Providers underestimate symptom severity among urban children with asthma. Arch Pediatr Adolesc Med 2002; 156: 141–146 10.1001/archpedi.156.2.141. [DOI] [PubMed] [Google Scholar]
- 20.Kattan M, Mitchell H, Eggleston P, Gergen P, Crain E, Redline S, Weiss K, Evans R 3rd, Kaslow R, Kercsmar C, Leickly F, Malveaux F, Wedner HJ. Characteristics of inner-city children with asthma: The National Cooperative Inner-City Asthma Study. Pediatr Pulmonol 1997; 24: 253–262 10.1002/1099-0496(199710)24. [DOI] [PubMed] [Google Scholar]
- 21.Kitch BT, Chew G, Burge HA, Muilenberg ML, Weiss ST, Platts-Mills T, O’Connor G, Gold DR. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. 2000; 108: 301–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarpong SB, Karrison T. Skin Test Reactivity to Indoor Allergens as a Marker of Asthma Severity in Children with Asthma. Ann Allergy Asthma Immunol 1998; 80: 303–308 10.1016/s1081-1206(10)62973-0. [DOI] [PubMed] [Google Scholar]
- 23.Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, Quesenberry CP, Selby JV, Farber HJ. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. 2002; 109: 857–865. [DOI] [PubMed] [Google Scholar]
- 24.Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr 2005; 5: 306–310 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 25.Mowrer JL, Tapp H, Ludden T, Kuhn L, Taylor Y, Courtlandt C, Alkhazraji T, Reeves K, Steuerwald M, Andrew M, Dulin M. Patients’ and providers’ perceptions of asthma and asthma care: A qualitative study. J Asthma 2015; 52: 949–956 10.3109/02770903.2015.1010731. [DOI] [PubMed] [Google Scholar]
- 26.McQuaid EL, Walders N, Kopel SJ, Fritz GK, Klinnert MD. Pediatric asthma management in the family context: The Family Asthma Management System Scale. J Pediatr Psychol 2005; 30: 492–502 10.1093/jpepsy/jsi074. [DOI] [PubMed] [Google Scholar]
- 27.Yoos HL, Kitzman H, Henderson C, McMullen A, Sidora-Arcoleo K, Halterman JS, Anson E. The impact of the parental illness representation on disease management in childhood asthma. Nurs Res 2007; 56: 167–174 10.1097/01.NNR.0000270023.44618.a7. [DOI] [PubMed] [Google Scholar]
- 28.Janevic MR, Baptist AP, Bryant-Stephens T, Lara M, Persky V, Ramos-Valencia G, Uyeda K, Hazan R, Garrity A, Malveaux FJ. Effects of pediatric asthma care coordination in underserved communities on parent perceptions of care and asthma-management confidence. J Asthma 2017; 54: 514–519 10.1080/02770903.2016.1242136. [DOI] [PubMed] [Google Scholar]
- 29.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology & Health 1999; 14: 1–24 10.1080/08870449908407311. [DOI] [Google Scholar]
- 30.Sleath B, Carpenter DM, Slota C, Williams D, Tudor G, Yeatts K, Davis S, Ayala GX. Communication during pediatric asthma visits and self-reported asthma medication adherence. Pediatr 2012; 130: 627–633 10.1542/peds.2012-0913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riekert KA, Borrelli B, Bilderback A, Rand CS. The development of a motivation interviewing intervention to promote medication adherence among inner-city, African-American adolescents with asthma. Patient Educ Couns 2011; 82: 117–122 10.1016/j.pec.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Canino G, Koinis-Mitchell D, Ortega AN, McQuaid EL, Fritz GK, Alegria M. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Soc Sci Med 2006; 63: 2926–2937 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 33.Koinis-Mitchell D, Kopel SJ, Salcedo L, McCue C, McQuaid EL. Asthma indicators and neighborhood and family stressors related to urban living in children. Am J Health Behav 2014; 38: 22–30 10.5993/AJHB.38.1.3. [DOI] [PubMed] [Google Scholar]
- 34.Klinnert M, McQuaid E, Gavin L. Assessing the Family Asthma Management System. J Asthma 1997; 34: 77–88 10.3109/02770909709071206. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Department of Health and Human Services. The 2005 HHS Poverty Guidelines. Washington, DC: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 36.Horne R, Weinman R. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. 1999; 47: 555–567 10.1016/S0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 37.Friedman D, Masek B, Barreto E, Baer L, Lapey A, Budge E, McQuaid EL. Fathers and asthma care: Paternal involvement, beliefs, and management skills. J Pediatr Psychol 2015; 40: 768–780 10.1093/jpepsy/jsv035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Celano M, Klinnert MD, Holsey CN, McQuaid EL. Validity of the Family Asthma Management System Scale with an urban African-American sample. Journal of pediatric psychology 2011; 36: 576–585 10.1093/jpepsy/jsp083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen J Statistical Power Analyses for the Behavioral Sciences (revised edition). New York: Academic Press; 1977. [Google Scholar]
- 40.Hayes AF. A primer on multilevel modeling. 2006.
- 41.Koinis-Mitchell D, McQuaid EL, Jandasek B, Kopel SJ, Seifer R, Klein RB, Potter C, Fritz GK. Identifying individual, cultural and asthma-related risk and protective factors associated with resilient asthma outcomes in urban children and families. J Pediatr Psychol 2012; 37: 424–437 10.1093/jpepsy/jss002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: Reasoning, responsibility, and behavior. J Pediatr Psychol 2003; 28: 323–333 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 43.McQuaid EL, Koinis-Mitchell D, Canino GJ. Acculturation. Achieving Respiratory Health Equality: Springer; 2017. p. 65–76. [Google Scholar]
- 44.Mitchell SJ, Bilderback AL, Okelo SO. Racial disparities in asthma morbidity among pediatric patients seeking asthma specialist care. Acad Pediatr 2016; 16: 64–67 10.1016/j.acap.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 45.Trivedi M, Fung V, Kharbanda EO, Larkin EK, Butler MG, Horan K, Lieu TA, Wu AC. Racial disparities in family-provider interactions for pediatric asthma care. J Asthma 2018; 55: 424–429 10.1080/02770903.2017.1337790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Utidjian LH, Fiks AG, Localio AR, Song L, Ramos MJ, Keren R, Bell LM, Grundmeier RW. Pediatric asthma hospitalizations among urban minority children and the continuity of primary care. J Asthma 2017; 54: 1051–1058 10.1080/02770903.2017.1294695. [DOI] [PubMed] [Google Scholar]
- 47.Paradies Y, Truong M, Priest N. A systematic review of the extent and measurement of healthcare provider racism. 2014; 29: 364–387 10.1007/s11606-013-2583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haywood C, Lanzkron S, Bediako S, Strouse JJ, Haythornthwaite J, Carroll CP, Diener-West M, Onojobi G, Beach MC, Investigators I. Perceived discrimination, patient trust, and adherence to medical recommendations among persons with sickle cell disease. 2014; 29: 1657–1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jang J, Gary Chan KC, Huang H, Sullivan SD. Trends in cost and outcomes among adult and pediatric patients with asthma: 2000–2009. Ann Allergy Asthma Immunol 2013; 111: 516–522 10.1016/j.anai.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 50.Gold DR, Adamkiewicz G, Arshad SH, Celedón JC, Chapman MD, Chew GL, Cook DN, Custovic A, Gehring U, Gern JE. NIAID, NIEHS, NHLBI, and MCAN Workshop Report: The indoor environment and childhood asthma—implications for home environmental intervention in asthma prevention and management. 2017; 140: 933–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McCallum GB, Morris PS, Brown N, Chang AB. Culture-specific programs for children and adults from minority groups who have asthma. The Cochrane database of systematic reviews 2017; 8: CD006580. 10.1002/14651858.CD006580.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poureslami I, Shum J, Nimmon L, FitzGerald JM. Culturally specific evaluation of inhaler techniques in asthma. 2016; 61: 1588–1596 [DOI] [PubMed] [Google Scholar]