Abstract
Purpose
To assess the use of telemedicine with phone-call visits as a practical tool to follow-up with patients affected by urological benign diseases, whose clinic visits had been cancelled during the acute phase of the COVID-19 pandemic.
Methods
Patients were contacted via phone-call and a specific questionnaire was administered to evaluate the health status of these patients and to identify those who needed an “in-person” ambulatory visit due to the worsening of their condition. Secondarily, the patients’ perception of a potential shift towards a “telemedicine” approach to the management of their condition and to indirectly evaluate their desire to return to “in-person” clinic visits.
Results
607 were contacted by phone-call. 87.5% (531/607) of the cases showed stability of the symptoms so no clinic in-person or emergency visits were needed. 81.5% (495/607) of patients were more concerned about the risk of contagion than their urological condition. The median score for phone visit comprehensibility and ease of communication of exams was 5/5; whilst patients’ perception of phone visits’ usefulness was scored 4/5. 53% (322/607) of the interviewees didn’t own the basic supports required to be able to perform a real telemedicine consult according to the required standards.
Conclusion
Telemedicine approach limits the number of unnecessary accesses to medical facilities and represents an important tool for the limitation of the risk of transmission of infectious diseases, such as COVID-19. However, infrastructures, health workers and patients should reach out to a computerization process to allow a wider diffusion of more advanced forms of telemedicine, such as televisit.
Electronic supplementary material
The online version of this article (10.1007/s00345-020-03536-x) contains supplementary material, which is available to authorized users.
Keywords: Telemedicine, Covid-19, BPH, Urology, Telehealth, Phone-counselling
Introduction
In the era of coronavirus disease 2019 (COVID-19) pandemic, one of the first countries to face this viral infection was Italy, with a first outbreak registered on 21st February 2020 [1]. The Italian Government declared quarantine status and was forced to lock all the non-essential businesses starting from 9th March 2020 to 18th May 2020.
The urological daily practice was overwhelmed [2], with a strong reduction both for surgical [3], emergency [4] and outpatients’ activities [5]. In particular, the outpatients’ visits in Italy were admitted only for urgencies or emergencies [6].
In this scenario, telehealth and telemedicine offer useful tools that allow to overcoming current challenges and to optimize resources [2]. Patients’ feedback on the potential use of telemedicine seems to be overwhelmingly positive. In a recent survey, the 72% of the interviewees reported to appreciate the use of telemedicine for outpatients’ visits during the COVID-19 period; however, this percentage decreased to 49.4% when considering a post-pandemic scenario [7].
The aim of this study was to assess the use of a phone call only visits as a practical tool to follow-up with patients affected by urological benign diseases, whose clinic visits had been cancelled during the acute phase of the pandemic.
Materials and methods
Study populations and objectives
Patients presenting a urological benign disease who had a Urology clinic visit scheduled and cancelled because of the COVID-19 outbreak between 9th March and 18th May 2020 at San Luigi Gonzaga University Hospital (Orbassano, Turin, Italy) were contacted via phone call.
During the call, a specific questionnaire was administered to the patients and data were prospectively collected. First study aim was to evaluate the health status of these patients, to identify those who needed an “in-person” ambulatory visit due to the worsening of their condition. Secondary objective was to evaluate the patients’ perception of a potential shift towards a “telemedicine” approach to the management of their condition and to indirectly evaluate their desire to return to “in-person” clinic visits.
Questionnaire
A purpose built 17 items questionnaire was administered to the patients during the phone call (Supplementary Material 1). Demographic variables were collected in terms of age, sex, type of disease (benign prostatic hyperplasia [BPH], urolithiasis, incontinence, infections, andrological issues) and Covid-19 status (affected, not affected). Then, the results of labs or imaging were also recorded. The first section (4 items) of the questionnaire analyzed patients’ health, including the type of disease, its stability, and the onset of a new problem/issue. Patients were recommended to postpone the follow-up or to plan an in-person visit depending on the findings at the phone call. The second section evaluated patients’ appreciation for the phone counselling using a five-point Likert scale (1 extremely disappointed; 5 absolutely appreciated). Last, patients’ attitude for a more advanced telehealth visit (including video consultation with the possibility to transmit radiological or laboratory exams) was assessed.
Statistical analysis
Descriptive statistics included frequencies and proportions for continuous and categorical variables, respectively.
Results
Demographics findings
Six hundred and seven patients with a benign urologic disease were contacted by telephone by the medical staff of the Department of Urology. Median age of this population was 74 years (range 44–89 years), and most patients were male (76.9%). Most common conditions were: BPH (n = 490; 80.7%) and urolithiasis (n = 69; 11.4%) (Table 1).
Table 1.
Demographics variables (BPH: benign prostatic hyperplasia)
| Demographics variables | 607 patients |
|---|---|
| Age, years; median (IQR) | 74 (44–89) |
| Male; no. (%) | 467 (76.9) |
| Disease, no. (%) | |
| BPH | 490 (80.7) |
| Urolithiasis | 69 (11.4) |
| Andrology and others | 48 (7.9) |
Clinical findings
12.5% (76/607) of patients showed a worsening of the urological condition or an onset of new symptoms; thus, a in person consult was scheduled in the following 15 days. On the other hand, 87.5% (531/607) of the cases showed stability of the symptoms at the phone interview, so no clinic or emergency visits were needed (Table 2) and the next follow-up visit was re-scheduled traditionally at after 6, 12 or 18 months in case of worsening, stability or improving of clinical conditions, respectively.
Table 2.
Clinical outcomes of hone-counselling
| Clinical outcomes | |
|---|---|
| Health status, no. (%) | |
| Stable | 531 (87.5) |
| Worsening | 50 (8.2) |
| Onset of new symptoms | 26 (4.3) |
| Exam presented, no. (%) | |
| First level | 303 (49.9) |
| Secondary level | 291 (47.9) |
| Phone-counselling outcomes, no. (%) | |
| Planned FU visit | 531 (87.5) |
| Indicated clinical visit with priority Ba | 76 (12.5) |
| Indicated access to ED | 0 (0) |
FU follow-up, ED emergency department
aAccording to Italian Ministry of Health disposition “priority B” means that the visit should be execute within 2 weeks
Telemedicine evaluation
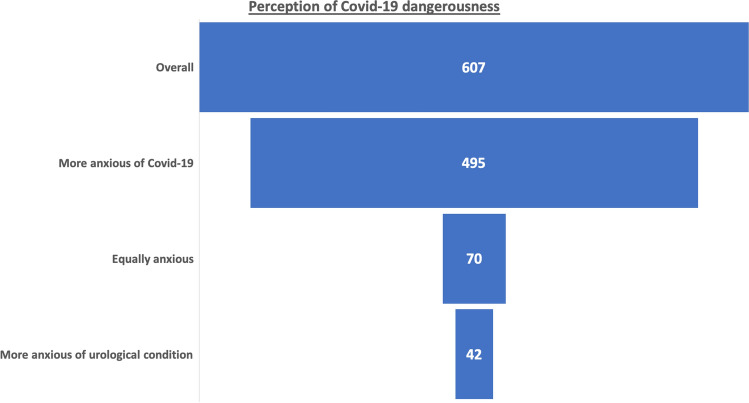
81.5% (495/607) of patients were more concerned about the risk of contagion than their urological condition (Fig. 1). Furthermore, 66% (401/607) stated that they would have postponed an in-person consult, if this had not been canceled, because of the fear of contracting COVID-19.
Fig. 1.
Graphical representation of the patient’s anxious for their urological conditions or Covid-19
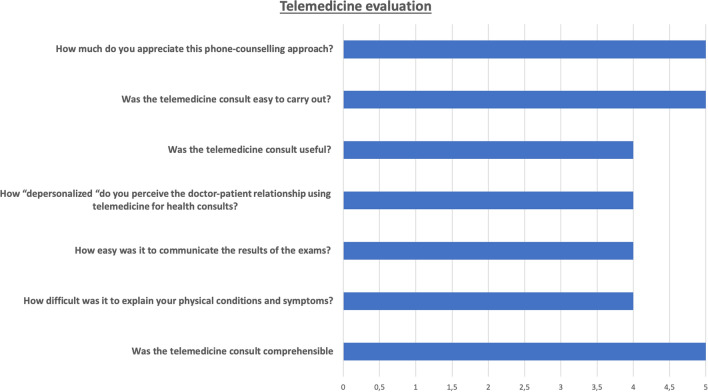
Concerning the evaluation of patients’ opinion on the use of telemedicine, the median score for phone visit comprehensibility and ease of communication of exams was 5/5. The median score for the patients’ perception of phone visits’ usefulness was 4/5 (Table 3). About half (46%; 279/607) of the patients approved being followed up with a telemedicine approach, even after the COVID emergency (Fig. 2).
Table 3.
Telemedicine evaluation
| Telemedicine evaluation | |
|---|---|
| Q.7 Was the telemedicine consult comprehensible? [median (IQR)]a | 5 (4–5) |
| Q.8 How difficult was it to explain your physical conditions and symptoms? [median (IQR)]a | 4 (3–4) |
| Q.9 How easy was it to communicate the results of the exams? [median (IQR)]a | 4 (4–5) |
| Q.10 How “depersonalized” do you perceive the doctor-patient relationship using telemedicine for health consults? [median (IQR)]a | 4 (3–5) |
| Q.11 Was the telemedicine consult useful? [median (IQR)]a | 4 (4–5) |
| Q.12 Was the telemedicine consult easy to carry out? [median (IQR)]a | 5 (4–5) |
| Q.13 How much do you appreciate this phone-counselling approach? [median (IQR)]a | 5 (4–5) |
| Q.14 Is the telemedicine visit more comfortable to carry out, compared to the classic consultation? No. (%) | |
| Yes | 394 |
| No | 213 |
| Q.15 Do you own any IT support? No. (%) | |
| No | 12 (1.9) |
| PC | 182 (29.6) |
| Tablet | 175 (28.8) |
| Smartphone | 578 (95.2) |
| Q.16 Would you have the possibility to carry out this visit with the help of an IT support? N (%) | |
| Yes | 285 (47.0) |
| No | 322 (53.0) |
| Q.17 Having experienced the COVID crisis, would you be willing to be followed-up using telemedicine even in the post-COVID period? | |
| Yes | 194 (32.0) |
| No | 413 (68.0) |
aThese items were assessed by using a 5-point Likert scale, see captions on the questionnaire attached
Fig. 2.
Telemedicine and the phone-counselling approach performed were tested using a five-point Likert scale evaluating the patients’ perception
Lastly, 53% (322/607) of the interviewees did not own the basic supports required to be able to perform a real telemedicine consult (computer, tablet, smartphone, internet connection). Furthermore, 68% (413/607) stated that even if they had had the chance, they would not have been able to carry out an online visit according to the required standards.
Discussion
During the hardest phase of the pandemic, in each single country, the majority of the population encountered restrictions, affecting their daily routines. In particular, the avoidance of physical contact was stressed following the #stayathome trend. Focusing on health services, the follow-up ambulatory visits for benign pathology were postponed or cancelled, also in Italy [8].
In this context, to cope with the COVID-19 pandemic, the use of telemedicine for patients’ health management steps into the limelight, even in urology. Telemedicine represents a peculiar instrument which, when used for selected populations of patients, can be compared to traditional counseling, as stated by Novara et al. [9]. Thanks to this instrument, physicians can offer effective and high-quality clinical consultations.
To fill the blank of official guidelines concerning the correct execution of a telemedicine counseling, Rodriguez Socarrás et al. [10] outlined its main principles and characteristics, highlighting some crucial aspects such the maintenance of professionalism, privacy, confidentiality whilst reaching satisfying levels of data transmission and comprehension.
Our study reported the data of more than 600 phone counselling for urological benign pathology: notwithstanding the simple call may seem an obsolete approach for telemedicine and may even seem inadequate for clinical visits, it perfectly matches the recommendations of the European Association of Urology [10]. In fact, the phone call, performed using hospital phones, can be considered the first and easiest approach for telemedicine, as reported in previously published experiences, for the management of prostate cancer [11], hematuria [12], stones [13, 14], urinary incontinence [15, 16] and urinary tract infections [17].
Focusing on clinical findings of our study, it is worth noticing that all patients presented a benign disease (mostly BPH), and only in 8% of the cases a worsening of the clinical condition was recorded, and in 12.5% of the cases a traditional visit within 2 weeks was recommended. No patients required to go to the ER for an urgent visit. On the contrary, most of the interviewers reported stability of the symptoms. Thus, phone counselling made by medical staff allowed to perform a triage to discriminate the patient’s clinical condition with a subsequent optimization of the hospital resources, allowing access to patients with a real need.
Another important finding was that more than 80% of the patients were more worried about viral infections than their urological diseases. Moreover, 66% of patients stated their intention to postpone their visit due to COVID-19 emergency. These percentage was very high probably because the patients were affected by benign diseases, with a clinical stability in 85% of the cases. On the contrary, in our series for oncological disease, only 20% of the patients would postpone their treatment [18]; whilst in Rodler et al. [19] experience, 56% of the patients were more anxious about their malignant disease than about COVID-19.
However, the most interesting findings of our study concerns the evaluation of patients’ perception of the telemedicine approach. In 88% of the cases, the appreciation for this telematic approach was rated 5/5 (“absolutely appreciated” using the five-point Likert scale). These findings are in line with our previous experiences evaluating the perceptions of patients waiting for urological procedures during COVID-19 lockdown at our center, which reported a high appreciation for telemedicine in 72% of the cases [7]. As expected, this value decreased to 46% when we evaluated its potential application in post-pandemic era, probably due to the scarce knowledge about this kind of approach by the patients.
Notwithstanding these encouraging findings, our analysis showed that the patients are not ready for a more modern telemedicine approach, such as tele-visiting. In fact, the 53% did not have an adequate support (PC, tablet, smartphone); moreover 68% of patients declared that, even if available, they would not have the instruments to perform an online visit. A 2019 survey reported by Cacciamani et al. [20] investigating the popularity of telehealth in the US, showed that lack of access (34.6%) and poor awareness (39.7%) of telehealth options represent the main limitations to the spreading of this instrument, with an estimated 10% of Americans to have experienced a telemedicine visit. In fact, the most popular tools for virtual communication resulted to be, in decreasing order of preference, phone call (76.9%), e-mail (56.7%), patient-reported outcome applications (22.0%), and video call (14.3%), as reported by Rodler et al. [19].
It is important to note that telemedicine represents a new area for both physicians and patients. The latter, particularly when elderly, may be unable to effectively use electronic devices, making an electronic consultation hard to perform. As suggested by Sosnowski et al. [21], the urologist can play an essential role in offering the patient the best option, choosing the most appropriate communication tool, and considering all the variables and the patient’s needs and preferences. The role of caregivers should also be maximized and integrated inside this context since they can be helpful in the communication process. Moreover, in this setting, patients should be able to get in touch with the physician as soon as a new problem arise, to promptly schedule a follow-up visit.
The main limitation of the present study should be mentioned. Phone-counselling allowed to perform a triage visit without the chance to adequately evaluate blood tests or radiological exams, and no change in pharmacological therapy was suggested, intrinsically limiting the in-depth analysis of the clinical investigation of this kind of approach.
Secondarily, lack of blindness of the interviewer (the same clinician that performed the consult) can influence the patient’s answers.
However, taking together all of these findings, one can argue that even if telemedicine is highly appreciated both by doctors and patients, current health care infrastructures remain inadequate and low access to computers of the patients represent the main challenges for a real transition to telemedicine in current daily clinical practice. Therefore, health practitioners should become increasingly familiar with telemedicine and, at the same time, national and regional initiatives to improve patients’ digital “literacy” should be implemented.
Conclusions
Implementing telemedicine tools for the management of urology patients with benign conditions in the current COVID-19 era carries several potential advantages and it is well perceived by most doctors and patients. However, efforts should be made to improve current infrastructures and access to computer technology to allow a wider diffusion of telemedicine and a real transition to more advanced forms of telehealth.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The Uro-technology and SoMe Working Group of the Young Academic Urologists Working Party of the European Association of Urology: Beatrice Carbonaro, Davide Zamengo, Stefano Piscitello, Juliette Meziere.
Author contributions
EC: manuscript writing, data analysis. SDeL: project development, supervision of manuscript writing. PA: data collection. PV: data collection, manuscript editing. SG: data collection. SDeC: data collection, manuscript writing. DA: manuscript writing. MS: data collection. FP: data collection. AP: data collection. GV: data collection. MM: supervision of manuscript writing. GB: supervision of manuscript writing. RA: supervision of manuscript writing. CF: project development, supervision of manuscript writing. FP: project development, supervision of manuscript writing.
Funding
The author(s) did not receive specific funding for this work.
Compliance with ethical standards
Conflict of interest
All authors have nothing to disclose.
Consent to participate
Oral informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided oral informed consent for publication.
Footnotes
The list of the Uro-technology and SoMe Working Group of the Young Academic Urologists Working Party of the European Association of Urology is listed in Acknowledgements.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cristian Fiori and Francesco Porpiglia contributed equally to the senior authorship.
Contributor Information
Enrico Checcucci, Email: checcu.e@hotmail.it.
The Uro-technology and SoMe Working Group of the Young Academic Urologists Working Party of the European Association of Urology:
Beatrice Carbonaro, Davide Zamengo, Stefano Piscitello, and Juliette Meziere
References
- 1.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/s0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amparore D, Campi R, Checcucci E, Sessa F, Pecoraro A, Minervini A, Fiori C, Ficarra V, Novara G, Serni S, Porpiglia F. Forecasting the future of urology practice: a comprehensive review of the recommendations by International and European Associations on priority procedures during the COVID-19 pandemic. Eur Urol Focus. 2020 doi: 10.1016/j.euf.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campi R, Amparore D, Capitanio U, Checcucci E, Salonia A, Fiori C, Minervini A, Briganti A, Carini M, Montorsi F, Serni S, Porpiglia F. Assessing the burden of nondeferrable major uro-oncologic surgery to guide prioritisation strategies during the COVID-19 pandemic: insights from three Italian high-volume referral centres. Eur Urol. 2020;78(1):11–15. doi: 10.1016/j.eururo.2020.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Novara G, Bartoletti R, Crestani A, De Nunzio C, Durante J, Gregori A, Liguori G, Pavan N, Trombetta C, Simonato A, Tubaro A, Ficarra V, Porpiglia F, Members of the Research Urology Network (RUN) (see appendix) Impact of the COVID-19 pandemic on urological practice in emergency departments in Italy. BJU Int. 2020 doi: 10.1111/bju.15107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonato A, Giannarini G, Abrate A, Bartoletti R, Crestani A, De Nunzio C, Gregori A, Liguori G, Novara G, Pavan N, Trombetta C, Tubaro A, Porpiglia F, Ficarra V, Research Urology Network (RUN) Clinical pathways for urology patients during the COVID-19 pandemic. Minerva Urol Nefrol. 2020;72(3):376–383. doi: 10.23736/s0393-2249.20.03861-8. [DOI] [PubMed] [Google Scholar]
- 6.Ficarra V, Novara G, Abrate A, Bartoletti R, Crestani A, De Nunzio C, Giannarini G, Gregori A, Liguori G, Mirone V, Pavan N, Scarpa RM, Simonato A, Trombetta C, Tubaro A, Porpiglia F, Research Urology Network (RUN) Urology practice during the COVID-19 pandemic. Minerva Urol Nefrol. 2020;72(3):369–375. doi: 10.23736/s0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 7.Amparore D, Campi R, Checcucci E, Piana A, Sica M, Grosso A, Presutti M, Barzaghi P, Minervini A, Serni S, Fiori C, Porpiglia F. Patients’ perspective on the use of telemedicine for outpatients urological visits: learning from the COVID-19 outbreak. Actas Urol Esp. 2020 doi: 10.1016/j.acuro.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Decreto-Legge 17 marzo 2020, n. 18. Misure di potenziamento del Servizio sanitario nazionale e di sostegno economico per famiglie, lavoratori e imprese connesse all’emergenza epidemiologica da COVID-19. (20G00034) (GU Serie Generale n.70 del 17-03-2020). https://www.gazzettaufficiale.it/eli/id/2020/03/17/20G00034/sg
- 9.Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, De Nunzio C, Galfano A, Giannarini G, Gregori A, Liguori G, Bartoletti R, Porpiglia F, Scarpa RM, Simonato A, Trombetta C, Tubaro A, Ficarra V, Research Urology Network (RUN) Telehealth in urology: a systematic review of the literature. How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. 2020 doi: 10.1016/j.eururo.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez Socarrás M, Loeb S, Teoh JY, Ribal MJ, Bloemberg J, Catto J, N’Dow J, Van Poppel H, Gómez Rivas J. Telemedicine and smart working: recommendations of the European Association of Urology. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parsons JK, Newman V, Mohler JL, Pierce JP, Paskett E, Marshall J, Cancer and Leukemia Group B The men’s eating and living (MEAL) study: a cancer and leukemia group B pilot trial of dietary intervention for the treatment of prostate cancer. Urology. 2008;72(3):633–637. doi: 10.1016/j.urology.2007.11.050. [DOI] [PubMed] [Google Scholar]
- 12.Safir IJ, Gabale S, David SA, Huang JH, Gerhard RS, Pearl J, Lorentz CA, Baumgardner J, Filson CP, Issa MM. Implementation of a tele-urology program for outpatient hematuria referrals: initial results and patient satisfaction. Urology. 2016;97:33–39. doi: 10.1016/j.urology.2016.04.066. [DOI] [PubMed] [Google Scholar]
- 13.Connor MJ, Miah S, Edison MA, Brittain J, Smith MK, Hanna M, El-Husseiny T, Dasgupta R. Clinical, fiscal and environmental benefits of a specialist-led virtual ureteric colic clinic: a prospective study. BJU Int. 2019;124(6):1034–1039. doi: 10.1111/bju.14847. [DOI] [PubMed] [Google Scholar]
- 14.Nevo A, Stern KL, Moore JP, Humphreys MR, Tyson MD, Keddis MT. The impact of phone counseling on urinary stone prevention. World J Urol. 2020 doi: 10.1007/s00345-020-03320-x. [DOI] [PubMed] [Google Scholar]
- 15.Jones G, Brennan V, Jacques R, Wood H, Dixon S, Radley S. Evaluating the impact of a ‘virtual clinic’ on patient experience, personal and provider costs of care in urinary incontinence: a randomised controlled trial. PLoS One. 2018;13(1):e0189174. doi: 10.1371/journal.pone.0189174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balzarro M, Rubilotta E, Trabacchin N, Mancini V, Costantini E, Artibani W, Antonelli A. A prospective comparative study of the feasibility and reliability of telephone follow-up in female urology: the patient home office novel evaluation (PHONE) study. Urology. 2020;136:82–87. doi: 10.1016/j.urology.2019.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Schauberger CW, Merkitch KW, Prell AM. Acute cystitis in women: experience with a telephone-based algorithm. WMJ. 2007;106(6):326–329. [PubMed] [Google Scholar]
- 18.Campi R, Amparore D, Capitanio U, Checcucci E, Salonia A, Fiori C, Minervini A, Briganti A, Carini M, Montorsi F, Serni S, Porpiglia F. Reply to Vincenzo Ficarra, Giuseppe Mucciardi, and Gianluca Giannarini’s letter to the editor re: Riccardo Campi, Daniele Amparore, Umberto Capitanio, et al. Assessing the burden of nondeferrable major uro-oncologic surgery to guide prioritisation strategies during the COVID-19 pandemic: insights from three Italian high-volume referral centres. Eur Urol2020;78:11–15. Eur Urol. 2020;78(4):e169–e170. doi: 10.1016/j.eururo.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodler S, Apfelbeck M, Schulz GB, Ivanova T, Buchner A, Staehler M, Heinemann V, Stief C, Casuscelli J. Telehealth in uro-oncology beyond the pandemic: toll or lifesaver? Eur Urol Focus. 2020 doi: 10.1016/j.euf.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cacciamani GE, Shah M, Yip W, Abreu A, Park D, Fuchs G. Impact of Covid-19 on the urology service in United States: perspectives and strategies to face a pandemic. Int Braz J Urol. 2020;46(suppl.1):207–214. doi: 10.1590/s1677-5538.ibju.2020.s126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sosnowski R, Kamecki H, Joniau S, Walz J, Klaassen Z, Palou J. Introduction of telemedicine during the COVID-19 pandemic: a challenge for now, an opportunity for the future. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.