Abstract
Background and study aims We aimed to evaluate the diagnostic performance of magnifying endoscopy with narrow-band imaging (M-NBI) in superficial non-ampullary duodenal epithelial tumors (SNADETs) regarding the absence or presence of biopsy before M-NBI diagnosis.
Patients and methods Clinicopathological data were retrospectively reviewed for 99 SNADETs from 99 patients who underwent endoscopic resection. The 99 tumors were divided into the non-biopsy group (32 lesions not undergoing biopsy before M-NBI examination) and the biopsy group (67 lesions undergoing biopsy before M-NBI examination). We investigated the correlation between the M-NBI diagnosis and the histopathological diagnosis of the SNADETs in both groups.
Results According to the modified revised Vienna classification, 31 tumors were classified as category 3 (C3) (low-grade adenoma) and 68 as category 4/5 (C4/5) (high-grade adenoma/cancer). The accuracy, sensitivity, and specificity of preoperative M-NBI diagnoses in the non-biopsy group vs the biopsy group were 88 % (95 % confidence interval: 71.0 – 96.5) vs 66 % (51.5 – 75.5), P = 0.02; 95 % (77.2 – 99.9) vs 89 % (76.4 – 96.4), P = 0.39; and 70 % (34.8 – 93.3) vs 14 % (3.0 – 36.3), P < 0.01, respectively. Notably, in the biopsy group, the specificity of M-NBI in SNADETs was low at only 14 % because we over-diagnosed most C3 lesions as C4/5. M-NBI findings might have been compromised by the previous biopsy procedure itself.
Conclusions In the non-biopsy group, the accuracy of M-NBI in SNADETs was excellent in distinguishing C4/5 lesions from C3. The M-NBI findings in SNADETs should be evaluated while carefully considering the influence of a previous biopsy.
Introduction
Superficial non-ampullary duodenal epithelial tumors (SNADETs) are considered rare in the general population 1 . With the widespread use of endoscopy and advances in endoscopic technology, a gradual increase in the detection rate of SNADETs has been reported 2 . Endoscopic resection (ER), which is less invasive than surgery, is becoming a first-choice treatment for SNADETs because most lesions are confined to the mucosa without lymph node metastasis 3 . However, because of the anatomical characteristics of the duodenum, such as its narrow lumen, thin wall, and long distance from the mouth, which sometimes makes it difficult to manipulate an endoscope, duodenal ER is associated with a higher risk of adverse events compared with ER in other parts of the digestive tract 4 5 .
Therefore, a preoperative diagnosis of SNADET is required to distinguish between lesions that should be followed-up and those to consider for resection. Follow-up without ER for low-grade adenoma (Vienna category 3, [C3]) is acceptable because the risk of progression to cancer is relatively low, and because lesions diagnosed as high-grade adenoma/carcinoma (Vienna category 4/5, [C4/5]) should be considered for resection 6 . However, the accuracy of the preoperative diagnosis of SNADETs using conventional white-light imaging (C-WLI) or biopsy is relatively low 2 7 8 .
Narrow-band imaging (NBI) is an innovative optical image-enhancing technology that uses narrow blue and green wavelengths to increase the visibility of vessels 9 . Magnifying endoscopy with NBI (M-NBI) enables clear visualization of the superficial microanatomy and can be used to differentiate between cancerous and non-cancerous lesions in the digestive tract more accurately compared with C-WLI 10 11 12 13 . However, some reports of M-NBI findings in SNADETs had limitations such as small sample sizes; 14 15 16 17 18 19 20 therefore, the usefulness of M-NBI for diagnosing C4/5 lesions remains unclear.
In our previous study, we reported that M-NBI findings may be useful in distinguishing C4/5 from C3 SNADETs 16 . However, the study included patients who had undergone M-NBI examination after biopsy specimens revealed SNADET. According to our preliminary observation, we realized that the SNADET was distorted by a previous forceps biopsy, and then the M-NBI findings show more irregular than those of the original morphology 21 . As a result, we might have over-diagnosed almost half of C3 lesions as C4/5. Therefore, we hypothesized that M-NBI findings might have been compromised by the previous biopsy procedure itself. Accordingly, in this study, we aimed to evaluate the diagnostic performance of M-NBI in SNADETs regarding the absence or presence of biopsy.
Patients and Methods
Study design and patients
This study was a single-center, retrospective study. Inclusion criteria were patients with a preoperative diagnosis of SNADETs by M-NBI who underwent ER between December 2008 and November 2017 at Ishikawa Prefectural Central Hospital. Patients were excluded if they met the following exclusion criteria: (1) no recorded M-NBI images of the lesion in the image filing system; (2) morphological findings at M-NBI of the lesion were obscured by adherent mucous or hemorrhage associated with flushing; (3) evidence of familial adenomatous polyposis; or (4) pedunculated lesions, because we reported that it is difficult to diagnose pedunculated lesions by M-NBI 19 .
We retrospectively analyzed both the M-NBI images and histopathological findings of the consecutive resected SNADET specimens, which we classified into two categories: a non-biopsy group in which biopsy was not performed before M-NBI examination and a biopsy group in which biopsy was performed before M-NBI examination. We investigated the correlation between the characteristic microvascular and microsurface findings at M-NBI and the histopathological diagnosis of the SNADETs in both groups.
All endoscopic examinations were performed using high-resolution endoscopes with M-NBI in our hospital. Therefore, SNADETs were diagnosed by M-NBI and removed without biopsies. However, a minimal number of preoperative biopsies were required for protruded lesions in the duodenal bulb that were difficult to differentiate from non-neoplasms by M-NBI alone, such as gastric metaplasia, ectopic gastric mucosa, and Brunner’s gland hyperplasia.
We performed this retrospective study at our hospital in Japan. The institutional review board of our hospital approved the collection of data, examination of past cases, and submission of the results in this study (approval no. 1286), and written informed consent was obtained from all patients.
Endoscopy system and settings
The procedure was performed using an endoscope (GIF-H260Z or GIF-H290Z; Olympus Co., Tokyo, Japan). The endoscopy system consisted of a video processor (CV-260SL or CV-290; Olympus) and a light source (CLV-260SL or CLV-290SL; Olympus) that worked in both the high-resolution WLI and NBI modes. A soft black hood (MAJ-1989 or MAJ-1990; Olympus) was mounted on the tip of the endoscope to enable the endoscopist to maintain a consistent distance between the tip of the endoscope and the mucosal surface to obtain in-focus endoscopic images at maximal magnification. Structural enhancement of the endoscopic video processor was set to B-mode level 4 – 6 for white-light endoscopy and to B-mode level 8 for M-NBI. The color mode was set at level 1.
Diagnostic endoscopy
All M-NBI findings were reviewed retrospectively by two endoscopists board-certified by the Japan Gastroenterological Endoscopy Society (KY and HD, each with at least 10 years’ experience performing upper gastrointestinal magnifying endoscopy) who were blinded to the C-WLI and histological findings, and the absence or presence of biopsy. Five to ten clear M-NBI images obtained at maximal magnification were available per case.
We used the established vessel plus surface (VS) classification system for the M-NBI diagnosis of early gastric cancer 10 11 , which is the most commonly used system in clinical practice 12 13 .
We determined whether there was a demarcation line (DL) between the lesion and the background mucosa. The microvascular (MV) pattern and the microsurface (MS) pattern were categorized as regular/irregular/absent, as follows:
Regular MV pattern: The mucosal capillaries have a uniform shape, and their arrangement and distribution are regular and symmetrical.
Irregular MV pattern: The vessels differ in shape, and their arrangement and distribution are irregular and asymmetrical.
Absent MV pattern: The subepithelial MV pattern is obscured by the presence of a white opaque substance (WOS) 22 .
Regular MS pattern: The morphology of the marginal crypt epithelium (MCE) shows a uniform structure, symmetrical distribution, and regular arrangement. When WOS is present, regular WOS can be an additional marker of a regular microsurface pattern, defined as well-organized and symmetrical distribution of the WOS in a regular reticular/maze-like/speckled pattern.
Irregular MS pattern: The morphology of the MCE shows a heterogeneous morphology, asymmetrical distribution, and irregular arrangement. When WOS is present, irregular WOS is defined as disorganized, with an asymmetrical distribution of the WOS in an irregular reticular/speckled pattern.
Absent MS pattern: No epithelial structures are visible.
Lesions presenting with (1) an irregular MV pattern with a DL and/or (2) an irregular MV pattern with a DL were diagnosed as cancerous; i. e., high-grade adenoma or superficial adenocarcinoma. Lesions presenting with neither finding were diagnosed as non-malignant; i. e., low-grade adenoma.
When individual diagnoses differed among the raters, the final diagnosis of MV pattern and MS pattern was made by consensus.
Histopathological analysis
The corresponding histology of the lesions was reviewed by specialized gastrointestinal pathologists blinded to the endoscopic findings. Histological features were evaluated according to the revised Vienna classification of gastrointestinal epithelial neoplasia 23 24 . Lesions were diagnosed as C3, C4, or C5 depending on the degree of cytological and architectural atypia, and invasion into the lamina propria. For the purposes of this study, we included low-grade adenoma in C3, and high-grade adenoma and superficial adenocarcinoma in C4/5, such that all C3 lesions were non-malignant, and all C4/5 lesions were classified as cancer.
Statistical analysis
Continuous variables, presented as mean ± standard deviation, were compared using Student’s t test, and categorical variables were compared using chi-squared test and Fisher’s exact test. P < 0.05 was considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R commander designed to add statistical functions frequently used in biostatistics 25 .
Results
Fig. 1 is a flowchart showing participant enrollment. Between December 2008 and November 2017, 119 patients underwent M-NBI to assess SNADETs before ER. Of these, 12 patients had unanalyzable M-NBI findings, 6 had familial adenomatous polyposis, and two had pedunculated lesions. Thus, 20 patients were excluded, and we enrolled the remaining 99 patients (99 lesions).
Fig. 1 .
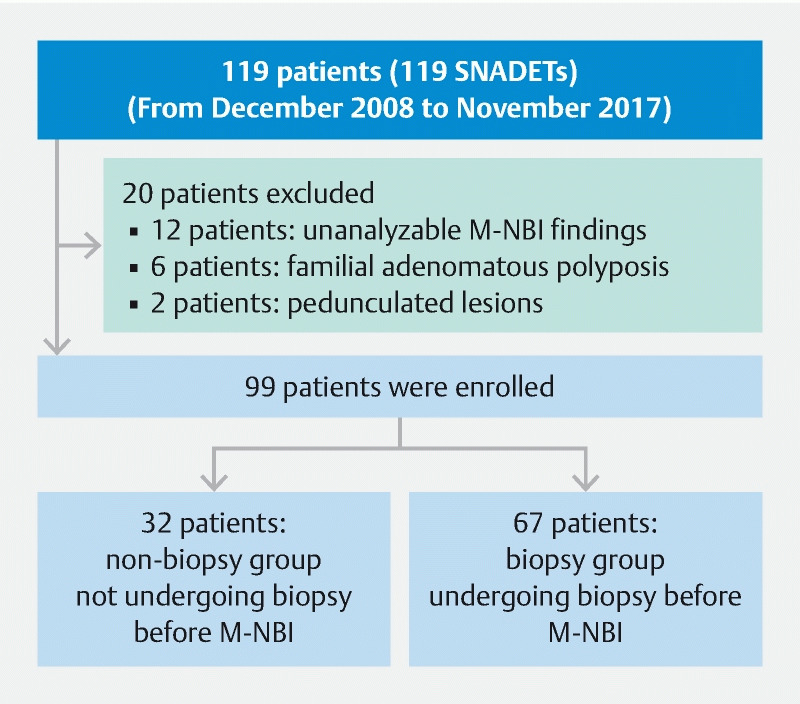
Study flowchart. SNADET, superficial non-ampullary duodenal epithelial tumor; M-NBI, magnifying endoscopy with narrow-band imaging.
The 99 tumors were divided into the non-biopsy group (32 lesions for which biopsy was not performed before M-NBI examination) and the biopsy group (67 lesions for which biopsy was performed before M-NBI). The clinicopathological characteristics of the lesions are shown in Table 1 . The biopsy group consisted of women significantly more frequently than did the non-biopsy group (29.9 % vs 9.4 %, respectively; P = 0.02). There was no significant difference in the remaining clinicopathological characteristics such as age, mean tumor diameter, macroscopic type, tumor location and final histological diagnosis between the two groups.
Table 1. Clinicopathological characteristics of all 99 superficial non-ampullaryduodenal epithelial tumors.
| Non-biopsy group, n = 32 | Biopsy group, n = 67 | P value | |||
| Sex, n (%) | |||||
|
29 | 90.6 | 47 | 70.1 | 0.02 |
|
3 | 9.4 | 20 | 29.9 | |
| Age, mean ± SD, years | 64 ± 9 | 64 ± 10 | 0.75 | ||
| Lesion size, mean ± SD, mm | 11 ± 7 | 12 ± 7 | 0.2 | ||
| Macroscopic type, n (%) | |||||
|
2 | 6.3 | 11 | 16.4 | 0.08 |
|
17 | 53.1 | 42 | 62.7 | |
|
13 | 40.6 | 14 | 20.9 | |
| Location, n (%) | |||||
|
2 | 6.3 | 13 | 19.4 | 0.11 |
|
|||||
|
9 | 28.1 | 25 | 37.3 | |
|
21 | 65.6 | 28 | 41.8 | |
|
0 | 0 | 1 | 1.5 | |
| Histological grade from ER specimens | |||||
|
10 | 31.3 | 21 | 31.3 | 0.99 |
|
22 | 68.8 | 46 | 68.7 | |
SD, standard deviation; ER, endoscopic resection; VCL, Vienna classification.
The relationships between M-NBI diagnosis according to the VS classification system and histopathological diagnosis according to the revised Vienna classification for the non-biopsy group of SNADETs are shown in Table 2 . Among the 24 lesions with M-NBI findings classified according to the VS classification system diagnosed as carcinoma, 21 (87.5 %) were diagnosed as C4/5. Among the eight lesions with M-NBI findings classified according to the VS classification system diagnosed as non-malignant, seven (87.5 %) were diagnosed as C3.
Table 2. Relationships between M-NBI diagnosis according to the VS classification system and histopathological diagnoses according to the revised VCL system for the non-biopsy group (n = 32).
| Histological grade from ER specimens | Total | |||||
| VCL category 3 | VCL category 4/5 | |||||
| Diagnosis of M-NBI | Cancerous | 3 | (30 %) | 21 | (95 %) | 24 |
| Non-malignant | 7 | (70 %) | 1 | (5 %) | 8 | |
| Total | 10 | 22 | 32 | |||
M-NBI, magnifying endoscopy with narrow-band imaging; VS, vessel plus surface; ER, endoscopic resection; VCL, Vienna classification.
The relationships between M-NBI diagnosis classified according to VS classification system and histopathological diagnoses according to the revised Vienna system for the SNADETs biopsy group are shown in Table 3 . Among the 59 lesions with M-NBI findings classified according to the VS classification system as carcinoma, 41 (69.5 %) were diagnosed as C4/5. Among the eight lesions with M-NBI findings classified according to the VS classification system diagnosed as non-malignant, three (37.5 %) were diagnosed as C3.
Table 3. Relationships between M-NBI diagnosis according to the VS classification system and histopathological diagnoses according to the revised VCL system for the biopsy group (n = 67).
| Histological grade from ER specimens | Total | |||||
| VCL category 3 | VCL category 4/5 | |||||
| Diagnosis of M-NBI | Cancerous | 18 | (86 %) | 41 | (89 %) | 59 |
| Non-malignant | 3 | (14 %) | 5 | (11 %) | 8 | |
| Total | 21 | 46 | 67 | |||
M-NBI, magnifying endoscopy with narrow-band imaging; VS, vessel plus surface; ER, endoscopic resection; VCL, Vienna classification.
A comparison of the diagnostic measurements for C4/5 with M-NBI diagnosis according to the VS classification system between the non-biopsy group and the biopsy group is shown in Table 4 . The accuracy of using M-NBI diagnosis according to the VS classification system in the non-biopsy group to diagnose C4/5 lesions was 88 % (95 % confidence interval [CI], 71.0 – 96.5), the sensitivity was 95 % (95 % CI, 77.2 – 99.9), the specificity was 70 % (95 % CI, 34.8 – 93.3), the positive predictive value (PPV) was 88 % (95 % CI, 67.6 – 97.3), and the negative predictive value (NPV) was 88 % (95 % CI, 47.3 – 99.7). The accuracy of using M-NBI diagnosis according to the VS classification system in the biopsy group to diagnose C4/5 was 66 % (95 % CI, 51.5 – 75.5), the sensitivity was 89 % (95 % CI, 76.4 – 96.4), the specificity was 14 % (95 % CI, 3.0 – 36.3), the PPV was 69 % (95 % CI, 56.1 – 80.8), and the NPV was 38 % (95 % CI, 8.5 – 75.5). Preoperative endoscopy using M-NBI in the non-biopsy group was associated with significantly higher diagnostic yields compared with the biopsy group, respectively, regarding accuracy (88 % vs 66 %; P = 0.02), specificity (70 % vs 14 %; P < 0.01), and NPV (88 % vs 38 %; P = 0.04). There was no significant difference in sensitivity and PPV between the two groups.
Table 4. Comparison of the diagnostic measurements for category 4 /5 lesions with M-NBI diagnosis according to the VS classification system between the non-biopsy group and the biopsy group.
| Non-biopsy group (n = 32) | Biopsy group (n = 67) | P value | |
| Accuracy (95 % CI) | 88 % (71.0 – 96.5) | 66 % (53.1 – 76.8) | 0.02 |
| Sensitivity (95 % CI) | 95 % (77.2 – 99.9) | 89 % (76.4 – 96.4) | 0.39 |
| Specificity (95 % CI) | 70 % (34.8 – 93.3) | 14 % (3.0 – 36.3) | < 0.01 |
| Positive predictive value (95 % CI) | 88 % (67.6 – 97.3) | 69 % (56.1 – 80.8) | 0.09 |
| Negative predictive value (95 % CI) | 88 % (47.3 – 99.7) | 38 % (8.5 – 75.5) | 0.04 |
M-NBI, magnifying endoscopy with narrow-band imaging; VS, vessel plus surface; CI, confidence interval.
We investigated the diagnostic performance of M-NBI in SNADETs according to lesion sizes of < 10 mm and ≥ 10 mm. In the 39 SNADETs < 10 mm in diameter, 15 occurred in the non-biopsy group, and 24 occurred in the biopsy group. For the SNADETs < 10 mm in diameter, the accuracy, sensitivity, and specificity of preoperative M-NBI diagnoses in the non-biopsy group vs the biopsy group, respectively, were 87 % (95 % CI: 59.5 – 98.3) vs 58 % (95 % CI: 36.6 – 77.9), p = 0.06; 88 % (95 % CI: 47.3 – 99.7) vs 86 % (95 % CI: 57.2 – 98.2), P = 0.91; and 86 % (95 % CI: 42.1 – 99.6) vs 20 % (95 % CI: 2.5 – 55.6), P = 0.01, respectively. In the 60 SNADETs ≥ 10 mm in diameter, 17 occurred in the non-biopsy group, and 43 in the biopsy group. For the SNADETs ≥ 10 mm in diameter, the accuracy, sensitivity, and specificity of preoperative M-NBI diagnoses in the non-biopsy group vs the biopsy group, respectively, were 88 % (95 % CI: 63.6 – 98.5) vs 70 % (95 % CI: 53.9 – 82.8), P = 0.14; 100 % (95 % CI: 0 – 19.3) vs 91 % (95 % CI: 75 – 98), P = 0.24; and 33 % (95 % CI: 0.8 – 90.6) vs 9 % (95 % CI: 0.2 – 41.3), P = 0.29, respectively. There was a significant difference in specificity using M-NBI between the two groups, but only for SNADETs < 10 mm in diameter.
Case presentation
We present an example of a low-grade adenoma case that was over-diagnosed as cancerous because M-NBI findings were compromised by the previous biopsy procedure itself (C3; Fig. 2 ). We also highlight two typical cases according to WLI and M-NBI findings for the SNADETs before biopsy. Case 1 is representative of low-grade adenoma (C3; Fig. 3 ), and Case 2 is representative of adenocarcinoma (C4.2; Fig. 4 ).
Fig. 2.
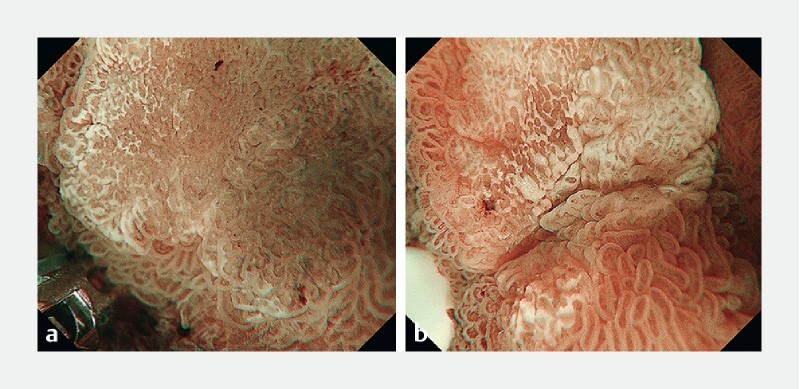
The influence of the previous biopsy procedure on magnifying endoscopy with narrow-band imaging (M-NBI) findings in superficial non-ampullary duodenal epithelial tumors. a M-NBI of a duodenal adenoma before biopsy. A clear demarcation line is identified according to distinct differences in the microsurface (MS) pattern between the lesion and the background mucosa. Vessel plus surface (VS) classifications: V, Because of the presence of white opaque substance (WOS), the morphology of the subepithelial microvessels cannot be observed, making this an absent microvascular (MV) pattern. S, The WOS has a regular reticular pattern with a symmetrical distribution and regular arrangement. The marginal crypt epithelium shows a regular arrangement and symmetrical distribution. Thus, this lesion was graded as a regular MS pattern using WOS as a marker for the MS pattern. The VS classification of this lesion was absent MV pattern plus regular MS pattern (WOS +) with a demarcation line. Therefore, the M-NBI diagnosis was non-malignant. b M-NBI of the same lesion after biopsy. The presence of WOS makes it impossible to discern the subepithelial MV pattern of the lesion. Analysis of the WOS morphology shows an irregularly distributed fine WOS, with a variety of morphologies, from speckled to polygonal (irregular WOS). Therefore, the M-NBI diagnosis was cancer. M-NBI findings were compromised by the previous biopsy procedure itself.
Fig. 3 .

A case of duodenal adenoma without biopsy. a Endoscopic findings using conventional endoscopy with white light imaging. A whitish, slightly depressed lesion (10 mm in diameter) is seen in the second part of the duodenum b Endoscopic findings using magnifying endoscopy with narrow-band imaging (M-NBI). A clear demarcation line is identified according to the distinct differences in microsurface (MS) pattern between the lesion and the background mucosa. Vessel plus surface (VS) classifications: V, Because of the presence of white opaque substance (WOS), the morphology of the subepithelial microvessels cannot be observed, making this an absent microvascular (MV) pattern. S, The WOS has a regular mazelike pattern with a symmetrical distribution and regular arrangement. Thus, this lesion was graded as a regular MS pattern using WOS as a marker for the MS pattern. The VS classification of this lesion was absent MV pattern plus regular MS pattern (WOS +) with a DL. Therefore, the M-NBI diagnosis was non-malignant. c The final histological diagnosis was low-grade adenoma.
Fig. 4 .
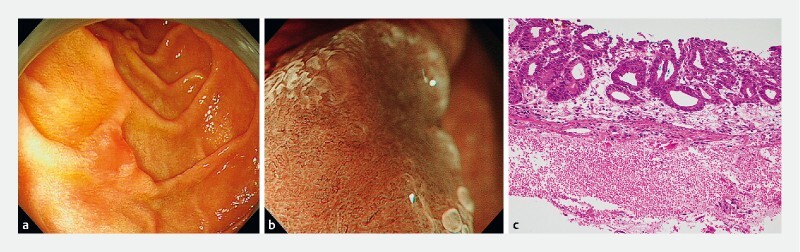
A case of duodenal adenocarcinoma without biopsy. a Endoscopic findings using conventional endoscopy with white light imaging. A reddish, slightly depressed lesion (10 mm in diameter) is seen in the second part of the duodenum. b Endoscopic findings using magnifying endoscopy with narrow-band imaging findings (M-NBI). A clear demarcation line (DL) is visible because of differences in the vessel plus surface (VS) component between the cancerous and noncancerous mucosa. V: Proliferation of microvessels with variable sizes, asymmetrical distribution, and irregular arrangement make this an irregular microvascular (MV) pattern. S: There are areas where the marginal crypt epithelium cannot be visualized, and analysis of the white opaque substance (WOS) morphology shows it to be irregular WOS with a speckled pattern. This lesion was assessed as an irregular microsurface (MS) pattern. The VS classification of this lesion was an irregular MV pattern plus irregular MS pattern (WOS +) with a DL. Therefore, the M-NBI diagnosis was cancer. c The final histological diagnosis was a well-differentiated intramucosal adenocarcinoma.
Discussion
Our study showed that the diagnostic performance of M-NBI according to the VS classification system for SNADETs in the non-biopsy group was higher than that in the biopsy group. In particular, in the biopsy group, the specificity of M-NBI diagnosis in SNADETs was low at only 14 % because we incorrectly diagnosed most C3 lesions as C4/5, which was overdiagnosis. M-NBI findings in SNADETs might have been compromised by the previous biopsy procedure itself. Previous biopsy leads to cancer overdiagnosis of SNADETs using M-NBI.
Endoscopic biopsies are performed to diagnose SNADETs; however, the accuracy of duodenal biopsy sampling is relatively low (68 % – 74 %) 2 7 8 . In preoperative diagnosis, accurately differentiating C4/5 from C3 is difficult using biopsy findings alone. The merit of an endoscopic diagnosis is that we can judge the lesion according to images of the whole lesion, whereas biopsies are associated with false-negative results, when they are performed in an area with a lower histological grade, or when the retrieved specimen is determined to be insufficient for evaluation. Endoscopic biopsies are performed to diagnose SNADETs, but biopsies induce submucosal fibrosis, which makes ER more difficult and increases the risk of adverse events 4 8 16 . Kinoshita et al. 8 reported that among 61 patients considered suitable for endoscopic mucosal resection, the treatment modality was converted from endoscopic mucosal resection to endoscopic submucosal dissection because of the non-lifting sign in 15 patients (24.6 %). Therefore, establishing a preoperative diagnostic method without biopsy sampling is desirable, and an endoscopy-based diagnosis is preferable for SNADETs that are likely to undergo ER. Our study suggests that M-NBI analysis might provide a more reliable determination of the histological grade of SNADETs compared with biopsy. If we detect a suspicious lesion that is a SNADET by WLI, evaluation by M-NBI is recommended to distinguish C4/5 lesions from C3, rather than biopsy. Correctly diagnosing SNADETs based on endoscopic findings without biopsies may render ER safer and easier. Consequently, our strategy proposes that a SNADET detected by WLI should eliminate biopsies, and undergo secondary evaluation by M-NBI, finally followed by ER.
Several studies have evaluated the clinicopathological differences in SNADETs according to tumor location, particularly between the oral and anal side of the papilla of Vater 26 27 28 29 . Gastric-type tumors are more frequently located on the oral than the anal side of the papilla of Vater, and they are predicted to have higher malignancy than intestinal-type tumors. In contrast, many of the tumors on the anal side of the papilla of Vater are the intestinal type, which are predicted to have lower malignant potential vs the gastric type 26 27 28 29 . Yamasaki et al. proposed a novel practical diagnostic algorithm for duodenal lesions based on magnifying endoscopy findings and evaluated its diagnostic performance to distinguish between SNADETs and non-neoplasms. In the descending and horizontal duodenum, most lesions with the pit type, round or linear crypt openings, and surrounded by subepithelial capillaries are SNADETs, and endoscopic biopsies may be eliminated for lesions with pit-type surface patterns in the descending and horizontal duodenum 30 . The surface patterns of non-neoplasms in the duodenal bulb, such as gastric metaplasia, ectopic gastric mucosa, and Brunner’s gland hyperplasia, have various histological types. SNADETs and non-neoplasms in the duodenal bulb show both surface patterns. Thus, endoscopic biopsies are required to diagnose neoplastic lesions in the duodenal bulb after careful inspection using C-WLI 30 . The morphology of gastric-type SNADETs in the duodenal bulb is mainly the protruded type 31 32 , for which fibrosis after biopsies is less likely to occur. Adverse event rates for ER of lesions in the duodenal bulb were reportedly low 33 34 ; thus, these lesions should be biopsied.
Using NBI with or without magnified endoscopy to diagnose SNADETs has been reported in a few small studies 14 15 16 17 18 19 . M-NBI might provide a more reliable diagnosis regarding the histological grade of SNADETs compared with biopsy. Our previous study reported that an irregular MS pattern was seen significantly more often with C4/5 lesions, so these findings may be useful in distinguishing C4/5 from C3 in SNADETs 16 . However, the study included patients who had undergone M-NBI examination after biopsy specimens revealed SNADET, so an irregular MS pattern was present in almost half of the C3 lesions. In the current study, the accuracy of M-NBI diagnosis according to the VS classification system in SNADETs before biopsy was notable for distinguishing C4/5 from C3, so it is possible that optical biopsy using M-NBI may be useful, clinically. In particular, M-NBI diagnosis according to the VS classification system in SNADETs before biopsy had a high sensitivity of 96 %. Therefore, lesions with an M-NBI diagnosis of C3 could be followed-up. Biopsy-induced changes are often focal or limited and sometimes are accompanied by regenerative mucosa or slight fold convergence. Therefore, we should be careful to observe the whole lesion to extract appropriate endoscopic findings while considering artificial changes caused by previous biopsies. Additionally, no comprehensive diagnostic criteria have yet been proposed for pathological observation of SNADETs. In the current study, the corresponding histology of the lesions was reviewed by specialized gastrointestinal pathologists. It is necessary to unify the histological diagnostic criteria for SNADETs not just for endoscopy but also for pathological observation.
This study has several limitations. First, this was a retrospective single-institution study. Second, the sample size was too small to calculate the accuracy of M-NBI diagnosis for SNADETs according to macroscopic type and tumor location. Third, the samples in this study were limited to resected specimens with no non-resected cases receiving conservative management. Furthermore, non-neoplasms confirmed at follow-up endoscopy were excluded because these lesions were never removed. Thus, the possibility of selection bias cannot be ignored, and this could have affected the PPV and NPV because PPV and NPV are influenced by disease prevalence. Fourth, M-NBI images were reviewed by experts only, and we cannot extrapolate our results to diagnosis by non-experts. Fifth, M-NBI images were collected retrospectively and were not real-time assessments. Sixth, we cannot rule out that the evaluators recognized the biopsy scars, and that this may have influenced the diagnosis. Effort to lessen these biases was made by blinding the evaluators to the C-WLI findings and the absence or presence of biopsy. Seventh, most patients in the biopsy group were referred from other hospitals in which preoperative biopsies were performed before M-NBI examination; thus, selection bias was not eliminated. Finally, selection bias for the lesions is possible because lesions located in difficult areas to obtain M-NBI images may exist, and poor-quality images cannot be assessed for M-NBI patterns. Additionally, in the present study, M-NBI diagnosis in SNADETs had a low NPV of 38 % in the biopsy group. This means that a final diagnosis of C4/5 lesions was made for 63 % of the lesions (5/8) diagnosed as non-malignant by M-NBI. Three of five lesions that were upgraded at final diagnosis measured more than 15 mm in length; therefore, it may be technically difficult to obtain M-NBI images of the entire lesion for large lesions. We attempted to minimize these biases using NBI images recorded for each lesion in consecutive patients. Further refinement of this classification should be performed by multiple observers using real-time assessment. Therefore, prospective and multicenter studies are required to establish endoscopic diagnostic criteria for SNADETs.
Conclusions
In conclusion, in the non-biopsy group, the accuracy of M-NBI diagnosis based on the VS classification system in SNADETs was excellent in distinguishing C4/5 from C3 lesions. The M-NBI findings in SNADETs should be evaluated with careful consideration regarding the influence of a previous biopsy procedure.
Acknowledgements
The authors thank Jane Charbonneau, DVM, from Edanz Group for editing a draft of this manuscript.
Footnotes
Competing interests The authors declare that they have no conflict of interest.
References
- 1.Jepsen J M, Persson M, Jakobsen N O et al. Prospective study of prevalence and endoscopic and histopathologic characteristics of duodenal polyps in patients submitted to upper endoscopy. Scand J Gastroenterol. 1994;29:483–487. doi: 10.3109/00365529409092458. [DOI] [PubMed] [Google Scholar]
- 2.Goda K, Kikuchi D, Yamamoto Y et al. Endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors in Japan: Multicenter case series. Dig Endosc. 2014;26:23–29. doi: 10.1111/den.12277. [DOI] [PubMed] [Google Scholar]
- 3.Yamasaki Y, Uedo N, Takeuchi Y et al. Current status of endoscopic resection for superficial nonampullary duodenal epithelial tumors. Digestion. 2018;97:45–51. doi: 10.1159/000484112. [DOI] [PubMed] [Google Scholar]
- 4.Kakushima N, Ono H, Takao T et al. Method and timing of resection of superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 2014;26:35–40. doi: 10.1111/den.12259. [DOI] [PubMed] [Google Scholar]
- 5.Kakushima N, Yoshida M, Iwai T et al. A simple endoscopic scoring system to differentiate between duodenal adenoma and carcinoma. Endosc Int Open. 2017;5:E763–E768. doi: 10.1055/s-0043-113567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okada K, Fujisaki J, Kasuga A et al. Sporadic nonampullary duodenal adenoma in the natural history of duodenal cancer: a study of follow-up surveillance. Am J Gastroenterol. 2011;106:357–364. doi: 10.1038/ajg.2010.422. [DOI] [PubMed] [Google Scholar]
- 7.Kakushima N, Kanemoto H, Sasaki K et al. Endoscopic and biopsy diagnoses of superficial, nonampullary, duodenal adenocarcinomas. World J Gastroenterol. 2015;21:5560–5567. doi: 10.3748/wjg.v21.i18.5560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kinoshita S, Nishizawa T, Ochiai Y et al. Accuracy of biopsy for the preoperative diagnosis of superficial nonampullary duodenal adenocarcinoma. Gastrointest Endosc. 2017;86:329–332. doi: 10.1016/j.gie.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Gono K, Obi T, Yamaguchi M et al. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004;9:568–577. doi: 10.1117/1.1695563. [DOI] [PubMed] [Google Scholar]
- 10.Yao K, Takaki Y, Matsui T et al. Clinical application of magnification endoscopy and narrow-band imaging in the upper gastrointestinal tract: new imaging techniques for detecting and characterizing gastrointestinal neoplasia. Gastrointest Endosc Clin N Am. 2008;18:415–433. doi: 10.1016/j.giec.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Yao K, Anagnostopoulos G K, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41:462–467. doi: 10.1055/s-0029-1214594. [DOI] [PubMed] [Google Scholar]
- 12.Ezoe Y, Muto M, Uedo N et al. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology. 2011;141:2017–2025. doi: 10.1053/j.gastro.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Muto M, Yao K, Kaise M et al. Magnifying endoscopy simple diagnostic algorithmfor early gastric cancer (MESDA-G) Dig Endosc. 2016;28:379–393. doi: 10.1111/den.12638. [DOI] [PubMed] [Google Scholar]
- 14.Yoshimura N, Goda K, Tajiri H et al. Endoscopic features of nonampullary duodenal tumors with narrow-band imaging. Hepatogastroenterology. 2010;57:462–467. [PubMed] [Google Scholar]
- 15.Kikuchi D, Hoteya S, Iizuka T et al. Diagnostic algorithm of magnifying endoscopy with narrow band imaging for superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 2014;26:16–22. doi: 10.1111/den.12282. [DOI] [PubMed] [Google Scholar]
- 16.Tsuji S, Doyama H, Tsuji K et al. Preoperative endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors, including magnifying endoscopy. World J Gastroenterol. 2015;21:11832–11841. doi: 10.3748/wjg.v21.i41.11832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mizumoto T, Sanomura Y, Tanaka S et al. Clinical usefulness of magnifying endoscopy for non-ampullary duodenal tumors. Endosc Int Open. 2017;5:E297–E302. doi: 10.1055/s-0043-103681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kakushima N, Yoshida M, Yamaguchi Y et al. Magnified endoscopy with narrow-band imaging for the differential diagnosis of superficial non-ampullary duodenal epithelial tumors. Scand J Gastroenterol. 2019;54:128–134. doi: 10.1080/00365521.2018.1557740. [DOI] [PubMed] [Google Scholar]
- 19.Tsuji S, Nakanishi H, Tsuyama S et al. Magnifying endoscopy with narrow-band imaging for superficial non-ampullary duodenal epithelial tumors before biopsy (in Japanese with an English abstract) Stomach Intestine. 2019;54:1121–1130. [Google Scholar]
- 20.Nakayama A, Kato M, Takatori Y et al. How I do it: Endoscopic diagnosis for superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 2019 doi: 10.1111/den.13538. [DOI] [PubMed] [Google Scholar]
- 21.Tsuji S, Katayanagi K, Kuruyama H et al. Magnifying endoscopy with narrow-band imaging for superficial non-ampullary duodenal epithelial tumors (in Japanese with an English abstract) Stomach Intestine. 2019;54:259–264. [Google Scholar]
- 22.Yao K, Iwashita A, Tanabe H et al. White opaque substance within superficial elevated gastric neoplasia as visualized by magnification endoscopy with narrow-band imaging: a new optical sign for differentiating between adenoma and carcinoma. Gastrointest Endosc. 2008;68:574–550. doi: 10.1016/j.gie.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Dixon M F. Gastrointestinal epithelial neoplasia: Vienna revisited. Gut. 2002;51:130–131. doi: 10.1136/gut.51.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stolte M. The new Vienna classification of epithelial neoplasia of the gastrointestinal tract: advantages and disadvantages. Virchows Arch. 2003;442:99–106. doi: 10.1007/s00428-002-0680-3. [DOI] [PubMed] [Google Scholar]
- 25.Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Niwa A, Kuwano S, Tomita H et al. The different pathogeneses of sporadic adenoma and adenocarcinoma in non-ampullary lesions of the proximal and distal duodenum. Oncotarget. 2017;8:41078–410790. doi: 10.18632/oncotarget.17051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toba T, Inoshita N, Kaise M et al. Clinicopathological features of superficial non-ampurally duodenal epithelial tumor; gastric phenotype of histology correlates to higher malignant potency. J Gastroenterol. 2018;53:64–70. doi: 10.1007/s00535-017-1327-0. [DOI] [PubMed] [Google Scholar]
- 28.Hijikata K, Nemoto T, Igarashi Y et al. Extra‐ampullary duodenal adenoma: a clinicopathological study. Histopathology. 2017;71:200–207. doi: 10.1111/his.13192. [DOI] [PubMed] [Google Scholar]
- 29.Yoshida N, Shimoda T, Abe M et al. Clinicopathological characteristics of non-ampullary duodenal tumors and their phenotypic classification. Pathol Int. 2019;69:398–406. doi: 10.1111/pin.12829. [DOI] [PubMed] [Google Scholar]
- 30.Yamasaki Y, Takeuchi Y, Kanesaka T et al. Differentiation between duodenal neoplasms and non-neoplasms using magnifying narrow-band imaging - Do we still need biopsies for duodenal lesions? Dig Endosc. 2020;32:84–95. doi: 10.1111/den.13485. [DOI] [PubMed] [Google Scholar]
- 31.Hida R, Yamamoto H, Hirahashi M et al. Duodenal neoplasms of gastric phenotype: an immunohistochemical and genetic study with a practical approach to the classification. Am J Surg Pathol. 2017;41:343–353. doi: 10.1097/PAS.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 32.Toya Y, Endo M, Akasaka R et al. Clinicopathological features and magnifying chromoendoscopic findings of non-ampullary duodenal epithelial tumors. Digestion. 2018;97:219–227. doi: 10.1159/000485505. [DOI] [PubMed] [Google Scholar]
- 33.Inoue T, Uedo N, Yamashina T et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 2014;26:220–227. doi: 10.1111/den.12104. [DOI] [PubMed] [Google Scholar]
- 34.Yahagi N, Kato M, Ochiai Y et al. Outcomes of endoscopic resection for superficial duodenal epithelial neoplasia. Gastrointest Endosc. 2018;88:676–682. doi: 10.1016/j.gie.2018.05.002. [DOI] [PubMed] [Google Scholar]


