Abstract
Background and study aims Colonoscopy is physically demanding for endoscopists and patients. Repetitive movements during colonoscopy can lead to overuse injuries. We aimed to explore the prevalence and range of colonoscopy-related musculoskeletal injuries (CRIs) in endoscopists.
Methods A cross-sectional electronic survey of 1825 endoscopists was performed. The sample was composed of members of the British Society of Gastroenterology, European Society of Gastrointestinal Endoscopy, and National Nurse Endoscopy Group (UK). The survey comprised 20 questions. These included: endoscopists’ workload, level of experience, and their perceived CRIs. All endoscopists who perform colonoscopy independently were included in the analysis.
Results A total of 368 questionnaires were completed of 1825 surveyed (20.16 %). Of those, 319 participants (17.48 %) were fully independent in colonoscopy. Of 319 endoscopists, 254 (79.6 %) have experienced musculoskeletal injuries. These were reported as either possibly (n = 143, 56.3 %) or definitely (n = 90, 35.4 %) related to colonoscopy. Commonly injured areas were the lower back (n = 85, 36.5 %), neck (n = 82, 35.2 %) and left thumb (n = 79, 33.9 %). Of the injured endoscopists, 98 (30.7 %) made some modification to their practice, such as stretching exercises and ergonomic changes. Of the endoscopists, 134 (42.0 %) thought that repetitive limb strain was a likely causative mechanism. Around 40 % believed that torquing the scope and challenging body position were precipitating CRIs. Several treatment modalities were used to treat CRIs. These included; physiotherapy (n = 109), medications (n = 70), rest (n = 43), splinting (n = 31), steroid injections (n = 26) and surgery (n = 11).
Conclusions A significant proportion of colonoscopists experience CRIs. The majority of the suggested modifications to practice can be adopted by any endoscopist. These results highlight the need to recognise CRI as an important occupational health hazard and to adopt preventative strategies routinely in the future.
Introduction
Endoscopy has become a widespread and invaluable tool in modern gastroenterology. In particular, colonoscopy is the gold standard modality for investigating colorectal symptoms and is currently endorsed as a primary screening tool for colorectal cancer in many healthcare systems. Technological advances in endoscopy have led to a huge improvement in the ability of gastroenterologists to diagnose and treat a wide range of simple to complex presentations. However, this may have exposed endoscopists to various occupational hazards, especially musculoskeletal (MSK) injuries 1 2 3 4 .
Endoscopists are commonly prone to endoscopy-related musculoskeletal injury and pain, which can occur in different parts of the body secondary to the complex and repetitive techniques associated with endoscopy procedures. However, many of these studies may be biased due to the limitation of self-reporting injuries 5 6 .
A systematic review of 13 studies revealed that 39 % to 89 % of endoscopists suffered from pain or injury in relation to endoscopy. That mainly affected the back, neck, shoulders, elbows, hands, and fingers. Endoscopists often use an extreme range of joint movement, which increases the risk of injury 7 8 .
In the United States, nearly half of gastroenterology fellows were affected by MSK injuries 9 with female fellows being more vulnerable to such injuries 10 . Other risk factors reported were the duration and number of the procedures and age of the endoscopist 7 8 9 10 .
While many endoscopists suffer from such injuries, little is being done to prevent them. Training in ergonomics seemed to be relatively protective; however, not many gastroenterologists have had such training 9 10 11 .
Our study aimed to explore the prevalence and range of colonoscopy-related MSK injuries (CRIs) in endoscopists. We also examined the factors that may predispose endoscopists to acquire MSK injury, and the possible consequences of CRI including sick leave, treatment, and modifications to practice.
Methods
Survey development and sampling
Our cross-sectional, electronic survey comprising 20 questions was modeled after the 2015 ASGE (American Society for Gastrointestinal Endoscopy) survey 6 . Our survey was pilot tested with a small number of experienced endoscopists at our center before distribution ( Appendix 1 ).
In February 2018, an online survey tool was used to collect responses. The link to the survey was sent via email to 1825 endoscopists. They were all members of the British Society of Gastroenterology, the European Society of Gastrointestinal Endoscopy or the National Nurse Endoscopy Group (UK). Email databases were obtained from each of the societies and the survey was sent to each individual in them.
The stated aim of the survey was to explore the prevalence of colonoscopy-related MSK injuries and their impact on colonoscopists. We also explained that the survey would take 5 minutes to complete and that all responses would remain anonymous. The endoscopists were encouraged to forward the survey to their colleagues. All endoscopists who perform colonoscopy independently were included in the analysis. The data were collected between January 27, 2018 and February 2, 2018. By completing the online survey, informed consent was presumed by respondents.
Survey questions
The 20 questions explored the job role of the endoscopist, demographics such as age and gender, the country where they worked, endoscopists’ workload, level of experience, their perceived CRI and any consequences from CRI that they encounter. The full questionnaire is summarized in Appendix 1 .
Statistical analysis
Descriptive statistics were used to identify the frequencies of CRI among colonoscopists. The respondents were divided into two groups: colonoscopists who believe or suspect that colonoscopy has precipitated their injury and colonoscopists who do not have any injury or believe that their injury is not caused by colonoscopy.
Comparative statistics using a chi-square test were applied to define the statistical difference between groups in relation to different dependent variables. To identify risk factors by using a chi-square test, different cut-offs were examined for the continuous numeric variables, for example, the number of colonoscopies per year, total lifetime procedures, the number of hours per week, and the number of years performing colonoscopy.
We also performed binominal logistic regression to identify factors associated with CRI. Variables with a P < 0.15 were incorporated into a multivariate logistic regression model to confirm their independent association with CRI. P < 0.05 was considered to represent a statistically significant difference between groups. IBM SPSS V.22.0 statistics were used for the analysis.
Results
A total of 368 colonoscopists completed the questionnaire from a total sample size of 1825 (20.16 %). Of those, 319 participants (17.48 %) were fully independent in colonoscopy and are included in this study. The majority of respondents were gastroenterologists (216/67.7 %), followed by nurse endoscopists (80/25.1 %) and surgeons (23/7.2 %). The ratio of male to female colonoscopists was 2.1:1. The majority of responding colonoscopists were aged 31 to 60 years (89.5 %); 1.0 % were less than 30 years old and 9.5 % were over age 60 ( Table 1 ).
Table 1. Baseline characteristics, n = 319.
| Factor | No. (%) | Possible/definite CRI, n = 236 (%) | No CRI, n = 83 (%) | P |
| Job Role | ||||
|
216 (67.7) | 158 (73.1) | 58 (26.9) | 0.162 |
|
23 (7.2) | 14 (60.9) | 9 (39.1) | |
|
80 (25.1) | 64 (80) | 16 (20) | |
| Age | ||||
|
3 (0.9) | 1 (33.3) | 2 (66.7) | 0.444 |
|
63 (19.7) | 49 (77.8) | 14 (22.2) | |
|
135 (42.3) | 102 (75.6) | 33 (24.4) | |
|
88 (27.6) | 63 (71.6) | 25 (28.4) | |
|
30 (9.4) | 21 (70.0) | 9 (30.0) | |
| Gender | ||||
|
217 (68.0) | 150 (69.1) | 67 (30.9) | 0.004 |
|
102 (32.0) | 86 (84.3) | 16 (15.7) | |
| Country/continent | ||||
|
231 (72.4) | 170 (73.6) | 61 (26.4) | 0.989 |
|
48 (15.0) | 37 (77.1) | 11 (22.9) | |
|
15 (4.7) | 11 (73.3) | 4 (26.7) | |
|
14 (4.4) | 10 (71.4) | 4 (28.6) | |
|
11 (3.4) | 8 (72.7) | 3 (27.3) | |
| Hospital or health practice | ||||
|
22 (6.9) | 21 (95.5) | 1 (4.5) | 0.073 |
|
127 (39.8) | 88 (69.3) | 39 (30.7) | |
|
28 (8.8) | 20 (71.4) | 8 (28.6) | |
|
142 (44.5) | 107 (75.4) | 35 (24.6) | |
| Video Endoscopy System | ||||
|
270 (84.6) | 197 (73.0) | 73 (27.0) | 0.622 |
|
25 (7.8) | 20 (80.0) | 5 (20.0) | |
|
24 (7.5) | 19 (79.2) | 5 (20.8) | |
| Colonoscopies/year | ||||
|
55 (17.2) | 38 (69.1) | 17 (30.9) | 0.399 |
|
264 (82.8) | 198 (75.0) | 66 (25.0) | |
| Lifetime total | ||||
|
199 (62.4) | 147 (73.9) | 52 (26.1) | 0.973 |
|
120 (37.6) | 89 (74.2) | 31(25.8) | |
| Hour/week | ||||
|
46 (14.4) | 35 (76.1) | 11 (23.9) | 0.856 |
|
273 (85.6) | 201 (73.6) | 72 (26.4) | |
| Years performing colon | ||||
|
58 (18.2) | 43 (74.1) | 15 (25.9) | 0.945 |
|
63 (19.7) | 46 (73.0) | 17 (27.0) | |
|
198 (62.1) | 147 (74.2) | 51 (25.8) | |
CRI, colonoscopy-related musculoskeletal injury.
The included responses were from 45 countries around the world. The responding colonoscopists were mainly from the UK (231/72.4 %). Forty-eight respondents (15.0 %) were from the rest of Europe, 15 (4.7 %) were from Asia and Australia, 14 responders (4.4 %) were from North and South America and another 11 (3.4 %) were from Africa.
The participating colonoscopists were nearly equally split in terms of their hospital or health care practice. Of the colonoscopists, 170 (53.3 %) work in a teaching hospital or an academic center, compared to 149 (46.7 %) in a district hospital or community practice. The most commonly used endoscopy system was Olympus (270/84.6 %) followed by Fujifilm (25/7.8 %) and Pentax (24/7.5 %).
Of the 319 respondents, 254 (79.6 %) have experienced MSK injuries. These were reported as either possibly (143/56.3 %) or definitely (90/35.4 %) related to colonoscopy ( Fig. 1 ).
Fig. 1.
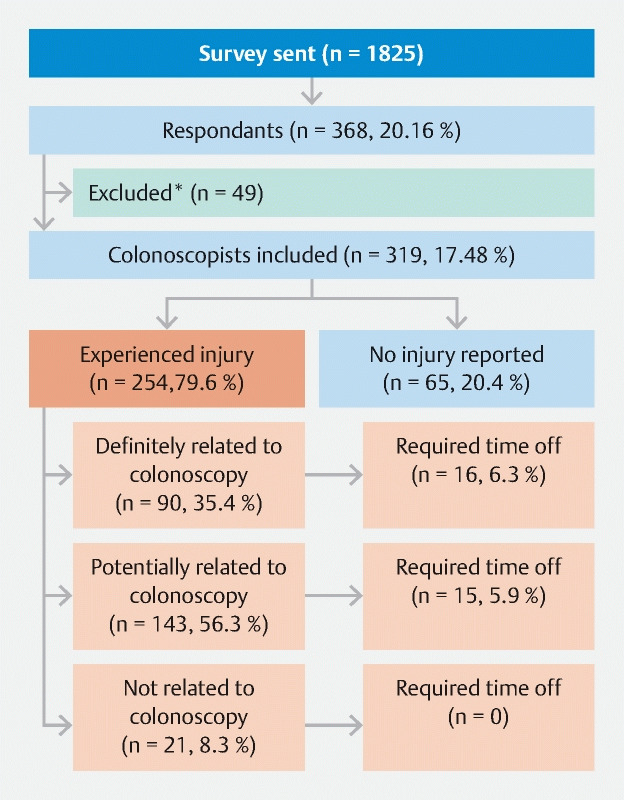
Study cohort. *Excluded as not fully independent in colonoscopy.
On initial chi-squared analysis, female endoscopists were found to have a significantly higher rate of CRI ( P = 0.004) and to be more likely to require time off work ( P = 0.0001). Other factors like hours per week spent performing a colonoscopy, total life-time procedures, the number of procedures per year, type of health care practice, endoscopy system in use, and number of years performing colonoscopy were not found to be significantly associated with higher rates of CRI ( Table 1 ). The prevalence of MSK that is definitely or possibly related to CRI was highest among nurse endoscopists (64/80 %), followed by gastroenterologists (158/73.1 %) and surgeons (14/60.9 %).
On univariate binominal logistic regression ( Table 2 ), female gender (odds ratio [OR] 2.392; 95 % confidence interval [CI] [1.260–4.542]; P = 0.008) and surgeon operators (OR 3.375; 95 % CI [1.192–9.552]; P = 0.022) were associated with more CRI. Combining the above factors with the hospital factor as district hospital/community practice with less than five specialists performing endoscopy had a P < 0.15 ( P = 0.077) in a multivariable regression model. Gender (covariate adjusted [OR] 2.198; 95 % CI [0.925–5.223]; P = 0.075) and surgeon operator (covariate adjusted [OR]1.856; 95 % CI [0.523–6.591] P = 0.339) were no longer statistically significant.
Table 2. Factors predictive of CRI.
| Factor | Unadjusted OR (95 % CI) | P value | Covariate adjusted OR (95 % CI) | P value |
| Job Role | ||||
|
1.1761 (0.881–3.521) | 0.109 | 1.064 (0.422–2.6810) | 0.896 |
|
3.375 (1.192–9.552) | 0.022 | 1.856 (0.523–6.591) | 0.339 |
|
Reference | |||
| Age | 1.140 (0.854–1.521) | 0.375 | ||
| Gender | ||||
|
Reference | |||
|
2.392 (1.260–4.542) | 0.008 | 2.198 (0.925–5.223) | 0.075 |
| Country/Continent | ||||
|
0.810 (0.207–3.165) | 0.761 | ||
|
0.793 (0.179–3.510) | 0.760 | ||
|
0.970 (0.168–5.593) | 0.973 | ||
|
1.185 (0.201–6.987) | 0.851 | ||
|
Reference | |||
| Hospital or health practice | ||||
|
0.158 (0.020–1.219) | 0.077 | 0.141 (0.018–1.101) | 0.062 |
|
1.271 (0.724–2.233) | 0.404 | ||
|
1.159 (0.450–2.989) | 0.760 | ||
|
Reference | |||
| Video Endoscopy System | ||||
|
1.333 (0.481–3.695) | 0.580 | ||
|
0.667 (0.139–3.194) | 0.612 | ||
|
Reference | |||
| Colonoscopy/year | 0.707 (0.362–1.380) | 0.309 | ||
| Life-time total | 0.936 (0.540–1.621) | 0.812 | ||
| Hour/week | 0.968 (0.463–2.023) | 0.931 | ||
| Years performing colon | 0.965 (0.692–1.348) | 0.836 | ||
CRI, colonoscopy-related musculoskeletal injuries
Commonly injured areas were the lower back (85/36.5 %), neck (82/35.2 %) and left thumb (79/33.9 %). A full description of other injuries is presented in Table 3 . The majority of injured endoscopists (98/30.7 %) made some modification to their practice due to CRI, such as performing stretching exercises or adjusting ergonomics. However, 163 (51.1 %) reported at least one modification to practice irrespective of the cause ( Fig. 2 ). Other modifications reported were regular massages, upper limb splints, straps and supporting devices, alternating gastroscopies and colonoscopies during the same list, technique modifications, help from an assistant endoscopist, and not performing endoscopy all day.
Table 3. MSK injury definitely or potentially related to colonoscopy (n = 233) 1 .
| Injury | No. (%) |
| Right fingers | 38 (16.3 %) |
| Right thumb | 41 (17.6 %) |
| Right hand | 44 (18.9 %) |
| Right wrist | 57 (24.5 %) |
| Right elbow | 30 (12.9 %) |
| Right shoulder | 63 (27.0 %) |
| Left fingers | 34 (14.6 %) |
| Left thumb | 79 (33.9 %) |
| Left hand | 25 (10.7 %) |
| Left wrist | 27 (11.6 %) |
| Left elbow | 26 (11.2 %) |
| Left shoulder | 37 (15.9 %) |
| Carpal tunnel | 13 (5.6 %) |
| Neck | 82 (35.2 %) |
| Upper back | 47 (20.2 %) |
| Lower back | 85 (36.5 %) |
| Hip | 13 (5.6 %) |
| Right lower limb | 8 (3.4 %) |
| Left lower limb | 5 (2.1 %) |
| Other injuries | 21 (9.0 %) |
MSK, musculoskeletal; CRI, colonoscopy-related injury.
Multiple injuries reported by some colonoscopists. The mean number of CRIs/colonoscopist is 3.3).
Fig. 2.
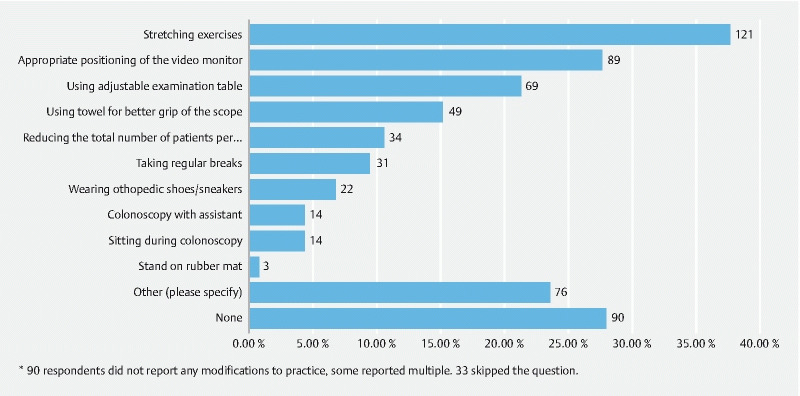
Modification made by colonoscopists (n = 163)*.
Of the endoscopists, 134 (42 %) thought that repetitive strain was the likely causative mechanism. Around 40 % believed that torquing the scope and challenging body position were the precipitating factors of CRI ( Fig. 3 ).
Fig. 3.
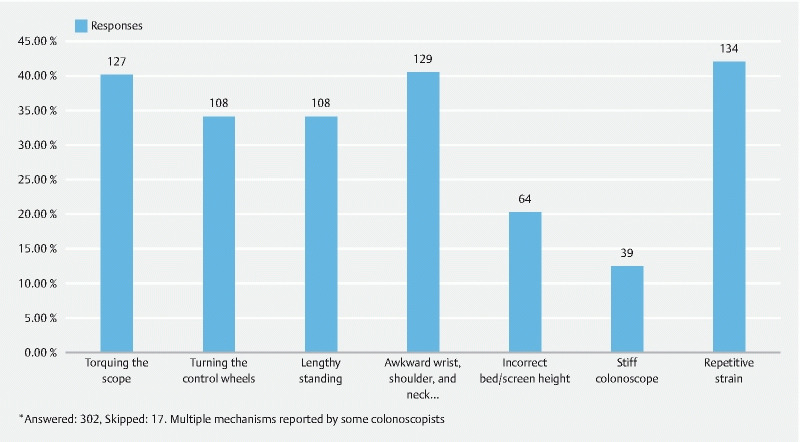
Presumed causative mechanisms of CRI*.
Several treatment modalities were used: physiotherapy (109), medications (70), rest (43), splinting (31), steroid injections (26), and surgery (11).
CRI caused some respondents to take sick leave (31/9.7 %); in total, 212 weeks were taken. Sick leaves ranged between 1 day and 3 months (median 2 weeks). Six colonoscopists reported more than one episode of sickness absence likely due to performing colonoscopy. Two colonoscopists stopped doing colonoscopies and one reduced his working hours to part-time.
Discussion
This is the largest international survey to examine the issue of CRI, that is, injury to the colonoscopist rather than to the patient. It demonstrates that CRIs are prevalent among endoscopists with nearly three-quarters of respondents (73 %) reporting a MSK injury possibly or definitely related to performing colonoscopy. This reported rate of injury falls at the higher range of previous estimated rates of 39 % to 89 %, underscoring the fact that it remains an occupational health issue in today’s practice 7 . The impact of CRI extends beyond the individual endoscopists and can also affect service provision. In extreme cases, endoscopists may be forced to reduce endoscopy commitments or rarely, have to cease performing colonoscopy entirely. Although only a few endoscopists had to stop doing colonoscopies or reducing numbers performed due to CRI, more than 4 years of activity were lost due to sickness by 31 respondents.
A recent European nationwide survey reported endoscopy-related MSK injuries at a prevalence of 69.6 %, which is similar to the prevalence in our survey 12 . Procedural volume and cumulative procedural time spent have previously been recognized as risk factors for CRI 7 13 14 . These risk factors were not observed in our study. A significant statistical difference might be captured with an even higher number of participants. On the other hand, the actual scoping technique and ergonomics used by individual colonoscopist may also be important risk factors for MSK injury. Further studies to explore this are needed.
On univariate analysis, we observed a higher rate of CRI among females in our survey. However, after controlling for other variables in the multivariable regression, it was not identified as an independent predictor for CRI. A recent European nationwide survey on endoscopy-related MSK injuries and a survey of US gastroenterology fellows have reported female gender as a risk factor for endoscopy-related injuries 10 12 . The combination of a suboptimal grip and reduced force-generating muscle mass has been described as placing females at a higher risk of repetitive strain injury 15 . One study of gastroenterology fellows reported that hand size could affect the ability to learn and perform endoscopy, with smaller hand size being more prevalent in women 16 . This may indicate that female endoscopists are at increased risk for this occupational hazard and highlights the need for further potentially gender-based surveys/studies to identify other gender-specific risk factors. This may lead to adjustments in colonoscopy education and in ergonomics of colonoscope design to accommodate a wider range of physical attributes.
The commonly injured areas reported in our survey were the lower back, neck, and left thumb. The repetitive hand motion and action of torquing the scope were the most common mechanisms leading to left thumb injuries. The phenomenon of colonoscope’s thumb, i. e. De Quervainʼs tenosynovitis of the left thumb due to repeated forces required to manipulate the colonoscope against resistance, has been described 17 . Technique modification has been implemented by many of our respondents. Stretching exercises, using height-adjustable beds and monitors, and improving handgrip by using towels to hold the scope are among the most popular modifications to mitigate the effects of this strain over a career span. Other interesting modifications reported were regular massages, upper limb splints, straps and supporting devices, alternating gastroscopies and colonoscopies during the same list, technique modifications, and not performing endoscopy all day. The utilization of an assistant endoscopist to cover lists as a short-term solution was available to a minority of respondents. This is unlikely to be accessible in all centers. This, however, might be available in large centers that offer complex therapeutic colonoscopy.
The back and neck pain injuries were mostly attributed to awkward posture, lengthy standing, and incorrect bed height. Spatial limitations of procedure rooms for optimal scope/bed-screen alignment to help maintain natural posture were frequently blamed. Ergonomic specifications to optimize bed height and monitor distance and elevation have been suggested but their rate of implementation into routine practice is unknown 18 19 20 . More studies assessing the effect of the implementation of ergonomic specifications into standard practice are required. Appraisal of endoscopy technique by trained occupational therapists has been reported to have some benefit 15 . A recent study assessing the impact of simulation-based ergonomic training curriculum that includes lectures, watching videos of expert performance, and ergonomic-specific feedback was found to be associated with a lower rate of CRI 21 .
A wide variety of treatment modalities were used by colonoscopists with CRI; they ranged from simple, noninvasive interventions like physiotherapy, analgesia, rest and splinting, to more invasive and sometimes complex interventions like steroid intra-articular injections and surgery. This is indicative of the individual impact CRI is having on our endoscopists. There is a call among our respondents for health care providers to cap the number of service procedures for colonoscopists to reduce long-term CRI. This will be challenging, given the increasing demands on colonoscopy; however, a suitable limit that satisfies service provision and training requirements will need careful consideration. These policies, in combination with targeted education on ergonomic procedure technique and workstation design with advances in scope technology, could be the strategy moving forward.
Looking to the future, CRI may become more prevalent as the number of colonoscopy procedures being performed is rising. For example, the introduction of FIT (fecal immunochemical testing) in the National Health Service bowel cancer screening program has led to a significant increase in the number of screening invitations 22 . Gerghaty et al. identified bowel cancer screeners as a higher-risk group due to higher-intensity workload and this risk magnitude is likely to increase over the coming years 13 . Our findings can be useful for endoscopists and hospitals, as there may be an increased demand for endoscopy in the COVID-19 recovery phase to deal with the backlog.
There are some limitations to this study. First, this is a self-reported survey-based study. This may have increased the likelihood that severely affected endoscopists would respond. Also, the majority of respondents practice in the UK. It is also important to consider that some endoscopists might do other endoscopic (like ERCP and EUS) or non-endoscopic physically demanding tasks that can affect the same anatomical region; however, evaluating that was beyond the scope of this study.
Conclusion
A significant proportion of colonoscopists experience CRI. The majority of the suggested modifications to practice can be adopted by any endoscopist. Our results highlight the need to recognize CRI as an important occupational health hazard and to adopt preventative strategies routinely in the future.
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Supplementary material :
References
- 1.Ofori E, Ramai D, John F et al. Occupation-associated health hazards for the gastroenterologist/endoscopist. Ann Gastroenterol. 2018;31:448–455. doi: 10.20524/aog.2018.0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy I, Gralnek I M. Complications of diagnostic colonoscopy,upper endoscopy, and enteroscopy. Best Pract Res Clin Gastroenterol. 2016;30:705–718. doi: 10.1016/j.bpg.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Bénard F, Barkun A N, Martel M et al. Systematic review of colorectal cancer screening guidelines for average-risk adults: Summarizing the current global recommendations. World J Gastroenterol. 2018;1:124–138. doi: 10.3748/wjg.v24.i1.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shergill A K, Asundi K R, Barr A et al. Pinch force and forearm muscle load during colonoscopy: a pilot study. Gastrointest Endosc. 2009;69:142–146. doi: 10.1016/j.gie.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 5.Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014;48:590–594. doi: 10.1097/MCG.0000000000000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ridtitid W, Cote G A, Leung W et al. Prevalence and risk factors for musculoskeletal injuries related to endoscopy. Gastrointest Endosc. 2015;81:294–3.02E6. doi: 10.1016/j.gie.2014.06.036. [DOI] [PubMed] [Google Scholar]
- 7.Yung D E, Banfi T, Ciuti G et al. Musculoskeletal injuries in gastrointestinal endoscopists: a systematic review. Expert Rev Gastroenterol Hepatol. 2017;11:939–947. doi: 10.1080/17474124.2017.1356225. [DOI] [PubMed] [Google Scholar]
- 8.Mohankumar D, Garner H, Ruff K et al. Characterization of right wrist posture during simulated colonoscopy: an application of kinematic analysis to the study of endoscopic maneuvers. Gastrointest Endosc. 2014;79:480–489. doi: 10.1016/j.gie.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 9.Villa E, Attar B, Trick W et al. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc Int Open. 2019;07:E808–E812. doi: 10.1055/a-0811-5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Austin K, Schoenberger H, Sesto M. Musculoskeletal injuries are commonly reported among gastroenterology trainees: results of a national survey. Dig Dis Sci. 2019;64:1439–1447. doi: 10.1007/s10620-019-5463-7. [DOI] [PubMed] [Google Scholar]
- 11.Kuwabara T, Urabe Y, Hiyama T et al. Prevalence and impact of musculoskeletal pain in Japanese gastrointestinal endoscopists: a controlled study. World J Gastroenterol. 2011;17:1488–1493. doi: 10.3748/wjg.v17.i11.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morais R, Vilas-Boas F, Pereira P et al. Prevalence, risk factors and global impact of musculoskeletal injuries among endoscopists: a nationwide European study. Endosc Int Open. 2020;8:E470–E480. doi: 10.1055/a-1038-4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geraghty J, George R, Babbs C. A questionnaire study assessing overuse injuries in United Kingdom endoscopists and any effect from the introduction of the National Bowel Cancer Screening Program on these injuries. Gastrointest Endosc. 2011;73:1069–1070. doi: 10.1016/j.gie.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Buschbacher R. Overuse syndromes among endoscopists. Endoscopy. 1994;26:539–544. doi: 10.1055/s-2007-1009030. [DOI] [PubMed] [Google Scholar]
- 15.Shergill A K, McQuaid K R. Ergonomic endoscopy: An oxymoron or realistic goal? Gastrointest Endosc. 2019;90:966–970. doi: 10.1016/j.gie.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Cohen D L, Naik J R, Tamariz L J et al. The perception of gastroenterology fellows towards the relationship between hand size and endoscopic training. Dig Dis Sci. 2008;53:1902–1909. doi: 10.1007/s10620-007-0069-x. [DOI] [PubMed] [Google Scholar]
- 17.Cappell M S. Colonoscopistʼs thumb: DeQuervainsʼs syndrome (tenosynovitis of the left thumb) associated with overuse during endoscopy. Gastrointest Endosc. 2006;64:841–843. doi: 10.1016/j.gie.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 18.ASGE Technology Committee . Pedrosa M C, Farraye F A et al. Minimizing occupational hazards in endoscopy: personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72:227–235. doi: 10.1016/j.gie.2010.01.071. [DOI] [PubMed] [Google Scholar]
- 19.Shergill A K, McQuaid K R, Rempel D. Ergonomics and GI endoscopy. Gastrointest Endosc. 2009;70:145–153. doi: 10.1016/j.gie.2008.12.235. [DOI] [PubMed] [Google Scholar]
- 20.Maciel D P, Millen R A, Xavier C A et al. Musculoskeletal disorder related to the work of doctors who perform medical invasive evaluation. Work. 2012;41:1860–1863. doi: 10.3233/WOR-2012-0398-1860. [DOI] [PubMed] [Google Scholar]
- 21.Khan R, Scaffidi M A, Satchwell J et al. Impact of a simulation-based ergonomic training curriculum on work-related musculoskeletal injury risk in colonoscopy. Gastrointest Endosc. 2020;92:1070–1080. doi: 10.1016/j.gie.2020.03.3754. [DOI] [PubMed] [Google Scholar]
- 22.Murphy J, Halloran S, Gray A. Cost-effectiveness of the faecal immunochemical test at a range of positivity thresholds compared with the guaiac faecal occult blood test in the NHS Bowel Cancer Screening Programme in England. BMJ Open. 2017;7:e017186. doi: 10.1136/bmjopen-2017-017186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


