Abstract
G protein coupled receptors (GPCRs) have emerged as the most potential target for a number of drug discovery programs ranging from control of blood pressure, diabetes, cure for genetic diseases to treatment of cancer. A panel of different ligands including hormones, peptides, ions and small molecules is responsible for activation of these receptors. Molecular genetics has identified key GPCRs, whose mutations or altered expressions are linked with tumorgenicity. In this review, we discussed recent advances regarding the involvement of GPCRs in the development of cancers and approaches to manipulating the mechanism behind GPCRs involved tumor growth and metastasis to treat different types of human cancer. This review provides an insight into the current scenario of GPCR-targeted therapy, progress to date and the challenges in the development of anticancer drugs.
Keywords: GPCRs, Anticancer therapy, Pancreatic cancer, Colon cancer, CLL, Prostate cancer, Melanoma
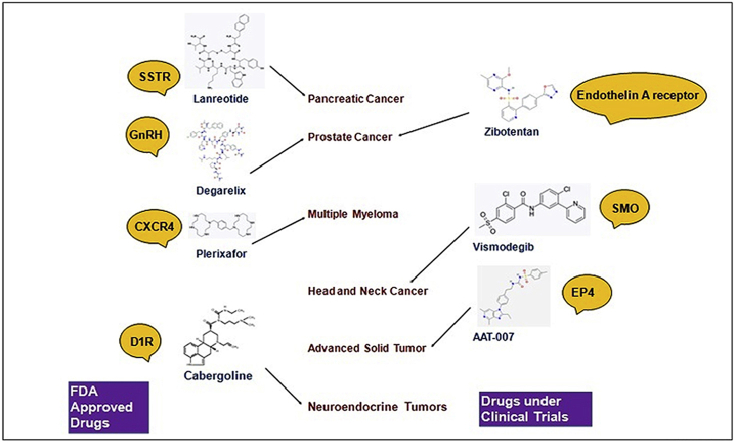
Graphical abstract
GPCRs based drugs against different cancers.
Highlights
-
•
An association of GPCRs in tumor growth and metastasis is confirmed in different types of cancers.
-
•
Despite the incredible potential of GPCRs in cancer therapy, only a few anti-GPCR drugs has been approved for clinical use.
-
•
Advancement in studying the association of cancer with GPCRs is inevitable to manipulate these receptors for cancer therapy.
1. Introduction
G protein coupled receptors (GPCRs) are membrane embedded receptors that regulate a plethora of biological functions. These receptors are coupled with heterotrimeric guanidine nucleotide binding proteins (G proteins) composed of 3 subunits. GPCRs serve as a crucial target for many drugs and their importance in drug discovery can be estimated by the fact that nearly 60% of drugs in the developmental stage and 36% currently marketed drugs target human GPCRs [1,2]. GPCRs family has been proven to be strongly associated with tumor growth and metastasis. The direct link between cellular transformation and GPCRs was first discovered in 1986 with the identification of MAS oncogene [3].
Molecular genetics has identified key GPCRs, whose mutations or altered expressions are linked with tumorgenicity. The most common tactic used by tumor cells to hijack GPCRs is to over express GPCRs and activate them by releasing agonists. It is shown that GPCRs can contribute to tumor cell growth when activated by an excess of a locally produced or circulating agonist. However, if mutated, GPCRs might become tumorigenic even in the absence of their agonists. Understanding the activation of GPCRs is very important as the mechanism behind can be exploited in anticancer drug development. GPCRs can be activated by bioactive lipids, e.g. lysophosphatidic acid 1 (LPA1) in breast cancer [4], peptides [5], chemokines, e.g. CXCL8/IL-8, which binds to CXCR1 and CXCR2 melanoma, pancreatic cancer, and gastric tumors [[6], [7], [8]], hormones , e.g. androgen, and neurotransmitters, e.g. adrenaline and noradrenaline can promote tumor progression through the beta-adrenergic receptors (beta-ARs) [9].
Although a number of GPCRs are involved in cancer initiation and progression, only a few are successfully exploited to develop drugs that can inhibit cancer associated signaling pathways. The approaches in GPCRs targeted drug discovery are targeting the signaling of the receptors using agonists or antagonists and targeting the specific interaction between GPCRs and their ligands to transport anti-neoplastic drugs or toxins to cancerous cells. One example is an endocrine treatment for hormone responsive prostate cancer in which gonadotropin releasing hormone (GnRH) receptor is targeted to reduce testosterone level. This approach helps to treat prostate cancer as stimulation of prostate cancer cell growth requires production of testosterone via a signaling cascade that starts with secretion of GnRH from the hypothalamus [10]. Immunological approach can also be used to neutralize the interaction of endogenous agonist with a specific GPCR. Direct vaccine injection can be administered for desired neutralizing effect. A sporadic example is immunogen G17DT to treat pancreatic cancer, which is in phase III trial [11].
This article recapitulated the current scenario related to the discovery of GPCR targeted drugs against different human cancers, including the possible mechanisms which are used by cancer cells to use GPCRs for their growth and metastasis and methods to intervene in these mechanisms to treat cancers. A list of Food and Drug Administration (FDA) approved anti-cancer GPCRs drugs is shown in Table 1 [12] whereas other potential GPCR targets for cancer treatment are summarized in Table 2 [[13], [14], [19], [15], [16], [17]].
Table 1.
FDA approved drugs and antibodies against different cancers [12].
| Drugs | Receptor | Cancer | Approval year |
|---|---|---|---|
| Cabergoline | Dopamine receptor D1 (DRD1) | Neuroendocrine tumors, pituitary tumors | 1996 |
| Lanreotide | Somatostatin receptor (SSTR) | Pancreatic cancer | 2007 |
| Degarelix | Gonadotropin releasing factor hormone receptor (GnRH) | Prostate cancer | 2008 |
| Plerixafor | C-X-C chemokine receptor 4 (CXCR4) | Multiple myeloma | 2008 |
| vismodegib (Erivedge) | Smoothened receptor (SMO) | Locally advanced, and metastatic basal cell carcinoma | 2012 |
| Raloxifene | Estrogen receptor (ER) | Breast cancer | 2014 |
| Sonidegib (Odomzo) | Smoothened receptor (SMO) | Locally advanced, and metastatic basal cell carcinoma | 2015 |
| Mogamulizumab | C–C Chemokine receptor 4 (CCR4) | T cell lymphoma | 2018 |
Table 2.
Other Potential GPCR targets for cancer treatment.
| Receptor type | Receptor | Ligand | System | Results | Refs. |
|---|---|---|---|---|---|
| Colon cancer | Formylpeptide receptor-2 (FPR2) | F2L | Human colon cancer cell lines | knockdown of FPR2 from colon cancer lines resulted in reduced tumorigenicity. | [13,14] |
| Pancreatic cancer | Galphas-coupled beta-adrenergic receptor | beta-blocker | Hamsters, transgenic mice | Blockage of beta- adrenergic signaling by beta- blocker prevented pancreatic cancer in mice. | [15] |
| Prostate cancer | Angiotensin II type 1 receptor (AT1R) | Angiotensin II | LNCap and PC3 cells | Inhibition of growth factor signaling was observed in LNCaP and PC3 cell lines. | [16] |
| GPR160 | Instead of cognate ligands, lentivirus-mediated shRNA system was used to suppress GPR160 transcription. | PC3, LNCaP, DU145 and 22Rv1 cells | Treatment of PC3 cells with GPR160-targeting shRNA lentiviruses resulted in cell apoptosis and growth arrest. | [17] | |
| Head and neck cancer | CXCR7, an atypical chemokine receptor also referred to as ACKR3 | Single variable domains of a highly selective immunoglobulin was used. | HNSCC cells | Immunoglubin therapy inhibited CXCR7-expressing head and neck cancer xenografted cells in nude mice. | [18] |
2. Colon cancer
Colon cancer is one of the major causes of cancer related mortality in the world. Although a variety of GPCRs are expressed in colon cancer cells, only a few are identified whose over-expression or aberrant expression is found to be associated with colon cancer. Formylpeptide receptor-2 FPR2 is a G protein coupled receptor that is widely present on the cell surface of different mammalian cells. Colon cancer cells can hijack the normal physiological function of FPR2 to migrate and proliferate autonomously. FPR2’s high expression is also associated with the poor prognosis in progressive colon cancer. Xiang et al. [13] xenografted human colon cells in immunocompromised mice and found that the cell lines with higher FPR2 expression level produced rapidly growing tumors in mice. They further showed that the knockdown of FPR2 from colon cancer lines is significantly related to reduced tumorigenicity [13]. Recently, another study reported that expression of FPR2 and its ligand F2L also play an important role in colon cancer drug resistance. When determined by immunohistochemistry assay and real-time PCR, higher expression levels of FPR2 and its ligand were found in resistant colon cancer tissues as compared to nonresistant colon cancer tissues. FPR2 signaling was found to require the involvement of the protein kinase B pathway (AKT pathway) in order to cause drug resistance. Enhanced drug sensitivity can be achieved using AKT inhibitors in pretreatment [14].
Another receptor influencing colon carcinogenesis is LPA1. It is one of six GPCRs for a phospholipid lysophosphatidic acid, and is encoded by LPAR1 gene. LPA1 activation causes cell proliferation and invasion activity in colon cancer. Using LPA2 activated HCT116 cells, it is shown that LPA2 signaling stimulates beta-catenin pathway and induces proliferation of HCT116 cells. Whereas knockdown of beta-catenin by RNAi results in inhibition of LPA2 induced proliferation of HCT116 cells. Similar results are also reported on the role of LPA3 in LS173T cells [19].
3. Prostate cancer
Prostate cancer is currently the major cause of tumor death in North America and Europe. In 2016, 180,890 new prostate cancer cases were reported [20]. Prostate specific G protein coupled receptor 1 and 2 (PSGR1 and PSGR2) belong to the olfactory receptor family and have a very limited expression in human prostate tissues. However, their transcription increases dramatically in the epithelial cells of prostate cancer and prostate intraepithelial neplasia patients. Analysis by Northern blot and real-time PCR showed that PSGR subfamily expression is also associated with clinical parameters such as risk of metastasis, recurrence status and clinical stages. PSGR transcript levels can also be detected in urine, and along with other markers such as prostate specific antigen (PSA) and α-methylacyl-CoA racemase (AMACR), increased diagnostic specificity can be achieved [21]. Neuhaus et al. [22] reported that beta-ionone and some steroids exhibited the potential to block PSGR and downregulate signaling mechanisms/gene expression and proliferative effects in cancer cells. Currently, in vitro and in vivo data indicate that by incubating prostate cancer cells with beta-ionone, cell growth can be inhibited. Over-expression of bradykinin and angiotensin 2 receptor has been found in PC3 prostate cancer cells. It has been reported that these receptors mediate cell proliferation through coupling with GA13 and gAq signaling. PSGR antagonist provides a potential approach to block the PSGR-dependant effects on cell proliferation [22].
GPRC6A is a membrane androgen receptor protein, encoded by the GPRC6A gene that is widely expressed in liver, heart, kidney, brain and so on. GPRC6A has recently been reported to be potentially associated with prostate cancer. Liu et al. [23] demonstrated that knockdown of GPRC6A expression in PC3 cells significantly reduces tumor migration and invasion activity, whereas increased expression of GPRC6A results in enhanced ERK and EMT signaling. Recently clustered regularly interspaced short palindromic repeats (CRISPR) and CRISPR-associated protein 9 nuclease (Cas9) (CRISPR/Cas9) technology was used to examine the function of GPRC6A in progression of prostate cancer. When the endegenous GPRC6A gene was disrupted in PC3 cell lines by using CRISPR/Cas9, it resulted in inhibition of osteocalcin mediated activation of ERK, AKT and mTOR pathways [24].
4. Pancreatic cancer
Pancreatic cancer is the fourth major cause of cancer related mortality in the world [25]. Alcohol consumption, smoking, diabetes, psychological stress and pancreatitis are the factors that contribute to the increasing prevalence of pancreatic cancer. All these factors stimulate hyperactive cyclic adenosine monophosphate signaling through activating Galphas-coupled beta-ARs. Schuller et al. [15], reported that psychological stress in mice promotes pancreatic cancer development through a neurotransmitter mediated increase in beta-AR signaling, whereas reduction in beta-adrenergic signaling by beta-blockers inhibits progression of pancreatic cancer xenografts. Similarly, in human pancreatic adenocarcinoma cells, higher expression levels of angiotensin (ANG II) and neurotensin receptors have been reported. Kisfalvi et al. [26] xenografted pancreatic cancer tissues (PANC-1, MIAPaCa-2) into nu/nu mice, and found that metformin (a drug used in the treatment of type-2 diabetes) not only inhibits the effects of neurotensin and angiotensin II on GPCRs, but also decreases cell proliferation of xenografted cells.
Receptors for gastrin and its related peptide cholecystokinin (CCK) are also significantly involved in pancreatic hyperplasia and carcinoma, so their inhibition is suggested as a promising objective in the treatment of pancreatic cancer. Recently, an immunogen G17DT/gastrimmune is developed by conjugating 17 N-terminal amino acids of gastrin to diphtheria toxoid. GI7DT/gastrimmune is unique in producing neutralizing antibodies against gastrin that can persist after vaccination for up to 40 weeks [27].
5. Chronic lymphocytic leukemia
Chronic lymphocytic leukemia (CLL), as the name suggests, is a cancer affecting lymphocytes of blood, which provides immunity to the body. This cancer arises from C5 + B cells and usually affects adults. CLL accounts for 38% of all leukemia cases in the UK, making it the most common type of leukemia in the country. In the US, about 15,720 new cases were diagnosed in 2014. In 2015, about 904,000 people were affected by CLL, resulting in 60,700 deaths globally [28]. The sphingosine-1-phosphate receptor is a GPCR involved in CLL. As compared to control B cells, CLL showed down-regulation of S1PR transcripts. The down-regulation of S1PR may be associated with a reduction in release of malignant cells from the lymphoid tissues to peripheral blood [29]. Treatment involves B cell receptor (BCR) inhibitors which cause increase in S1PR1 protein expression. This causes induction of CLL cell mobilization into the blood, making cells more sensitive to cytotoxic drugs.
Another receptor tachykinin receptor (TACR1) transcript is overexpressed in CLL patient cells compared to normal B lymphocytes. Leukotriene B4 receptor 1 (BLT1) is expressed in CLL cells so inhibitors for leukotriene biosynthesis can be used as novel CLL therapeutics [30]. Other notable GPCRs important in CLL cells include up-regulation of neurotensin receptors NTSR2 mRNA, thromboxane A2 receptor TBXA2R mRNA and tachykinin receptor TACR1 transcript and down-regulation of NTSR1 protein [31].
Beta-2 adrenergic receptors (beta2-AR) are less frequently present on mononuclear leukocytes in CLL as compared to healthy cells [32]. ADBR2 complex dysfunction is associated with cancer progression. Agonists of this receptor induce apoptosis in CLL cells, so they can be used for cancer therapy [33]. BLT1 protein is also expressed in CLL. Inhibition of BLT1 antigen expression is a potential therapeutic strategy for CLL. Another receptor C-X-C chemokine receptor 4 (CXCR4) is hyperphosphorylated in CLL. PIM inhibition causes its dephosphorylation and internalization and can serve as a potential therapeutic target. Other therapeutics which target CXCR4 down-regulation to treat CLL are AMD3100 (plerixafor) [34], suberoylanilidehydroxamic acid [35], the combination of CXCR4 antagonists and passive immunotherapy [36], small peptide inhibitors [37], PI3K inhibitors [38] and ibrutinib-mediated BTK inhibition [39].
Yoshie et al. [40] reported high frequent expression of CCR4 in adult T-cell leukemia (ATL) and human T-cell leukemia virus type 1 (HTLV-1)-immortalized T cells. CCR4 was used to target for therapeutics. The FDA recently granted ‘Breakthrough Therapy’ status to Mogamulizumab (KW-0761; Poteligeo™) which is a monoclonal antibody targeting CCR4 for the treatment of adult T cell leukemia-lymphoma [41].
6. Breast cancer
Breast cancer is one of the most common types of cancer in women. This cancer affects women more than men (100 times more common in women than men) [42]. 12% women are affected by this cancer. In the US, 2.8 million women were affected by breast cancer in 2015 [43]. In developing countries, breast cancer accounts for the leading cause of cancer-related deaths in women. Tuszynski et al. [44] discovered that a fragment of G-protein coupled receptor-associated sorting protein 1 (GASP-1) was present in sera of patients with early stage breast cancer. GASP-1 overexpression was also detected in tumor extracts but not in adjacent normal tissues of breast cancer patients. GASP-1 can not only be used as serum as well as a tumor biomarker for cancer diagnosis, but also as a novel target for breast cancer therapy.
Several studies indicated that high level of circulating lipids in the body is linked with an increased risk of cancer, especially breast cancer, for example, oleate was detected to be involved in proliferation of cancer cells. To check the precise mechanism of how oleate helps in breast cancer proliferation, Hardy et al. [45] identified that GPR40, a fatty acid receptor, is overexpressed in breast tumors. GPR40 overexpression is actually responsible for amplified oleate-induced proliferation of cancerous cells. Using RNA interference, when GPR40 gene was silenced, oleate induced proliferation of cancer cells decreased.
15% of all breast cancer patients lack the expression of progesterone receptors, estrogen receptors and human epidermal growth factor receptor-2 (HER-2). This type of breast cancer is called triple negative breast cancer (TNBC). Breast cancer therapies targeting ER and HER-2 receptors are not effective in TNBC [46]. Feigin et al. [47] discovered that GPR161 is overexpressed in patients with TNBC. This overexpression of GPR161 is also associated with increased cell migration and cell proliferation in 3D culture of human mammary epithelial cells. So GPR161 can be used in prognosis and as a drug target in TNBC. The drugs in clinical trials are summarized in Table 3 [48].
Table 3.
Anti GPCRs drugs and antibodies under clinical trials [48].
| Cancer | Inhibitor | Type of molecule | Receptor | Phase | Sponsor |
|---|---|---|---|---|---|
| Prostate cancer | Zibotentan (ZD4054) Atrasentan (ABT-627) |
Small molecule Small molecule |
Endothelin A receptor Endothelin A receptor |
Phase I, II, III Phase II, Phase III (combine with docetaxel and prednisone) |
AstraZeneca Abbott Southwest Oncology Group |
| Head and neck cancer | GDC-0449 (Vismodegib) | Small molecule | Smoothened receptor (SMO) | Phase II | Sue Yom in collaboration with Genentech, Inc |
| Ovarian cancer | GDC-0449 (Vismodegib) Propranolol (beta-blockers) |
Small molecule Small molecule |
Endothelin Receptor beta-adrenergic receptor |
Phase II Phase I |
Genentech, Inc. Washington University School of Medicine |
| Pancreatic cancer | CCX872 (OMP-18R5) Vantictumab G17DT |
Small molecule Antibodies Immunogen |
CCR2 Frizzled receptor FZD7 Cholecystokinin-2 receptor |
Phase I Phase I (combine with nab-paclitaxel and gemcitabine) Phase III |
ChemoCentryx OncoMed Pharmaceuticals, Inc. Cancer Advances Inc |
| Multiple myeloma | BMS-936564 | Antibodies | CXCR4 | Phase I | Bristol-Myers Squibb |
| Melanoma | Plozalizumab | Humanized monoclonal antibody | CCR2 | phase I | Millennium Pharmaceuticals, Inc. |
| Adult T-cell leukemia and lymphoma | KW-0761 (Mogamulizumab) | Antibodies | CCR4 | Phase II | Kyowa Hakko Kirin |
| Metastatic breast cancer | OMP-18R5 (Vantictumab) beta-blockers |
Antibodies Small molecule |
FZD1, 2, 5, 7, 8 beta-adrenergic receptor |
Phase I (combined with paclitaxel) Phase II |
OncoMed Pharmaceuticals, Inc. Columbia University |
| Non-small cell lung carcinoma | OMP-18R5 (Vantictumab) | Antibodies | Frizzled receptors (FZD1, 2, 5, 7, 8) | Phase I (combined with docetaxel) | OncoMed Pharmaceuticals, Inc. |
| Advanced solid tumors | AAT-007 | Small molecule | Prostaglandin E2 receptor 4 (EP4) | Phase II | University of Maryland |
| Advanced or metastatic cancer | LY-2624587 | Antibodies | CXCR4 | Phase I | Eli Lilly and Company |
7. Melanoma
Melanoma is a type of skin cancer, which develops from melanocytes (pigment containing skin cells). In 2012, 232,000 people were affected by melanoma resulting in 55,000 deaths. New Zealand and Australia have the highest rates of this cancer in the world. In 2017, about 87,110 new melanoma cases which resulted in 9,730 deaths in the US, were reported [49]. One of the most abundant GPCRs associated with melanoma metastases is GPR18. GPR18 is actually involved in the inhibition of apoptosis, so it helps with tumor cell survival. This orphan GPCR can be used as a drug target for melanoma metastasis [50].
GPR56 is a GPCR which is found to have an inhibiting power against progression of prostate cancer. In melanoma xenografts, GPR56 was also found to suppress tumor growth and metastases [51]. Melanoma angiogenesis is inhibited as GPR56 prevents melanoma cells from producing VEGF. As its action is antagonistic to melanoma, it is very important in cancer metastasis [52,53].
Another GPCR, GPR55, was found to be associated with skin tumor development in mice. It causes proliferation of tumor cells. It is also involved in tumor aggressiveness as it enhances invasiveness, cell anchorage-independent growth, and tumorigenicity in mice. Finally, this receptor was found to be upregulated in human skin tumors as compared to nearby healthy cells. These findings suggest that GPR55 can be used as a potential biomarker and therapeutic target in skin cancer therapies [54]. Melanocytes exhibit a receptor, melanocortin 1 receptor (MC1R) that is involved in expression of an enzyme to produce eumelanin. People with red hair are found to be effected by skin tumors more frequently. MC1R is inactivated in people with red hair due to a mutation. The absence of MC1R makes red heads more susceptible to skin cancer [55,56]. This receptor is also involved in α-MSH/MC1R signaling which is an anti-inflammatory pathway and induces melanoma immunity. Reduction in tumor development has been seen in a mouse model system by MC1R stimulation [57]. MC1R is actually involved in maintenance of a tumor free environment [58].
8. Conclusion
GPCRs exhibit their role as potential drug targets in the treatment of a number of diseases. An association of GPCRs with tumor growth and metastasis is confirmed in different types of cancers. Despite the incredible potential of GPCRs as targeting cancer therapy, only a few anti-GPCR drugs have been commercialized for the clinical use. The main setback in GPCRs’ role as the anticancer drug target is a problem in their ligand identification. More accurate investigation of biological mechanisms behind tumor progression and metastasis is required to decrease limitations present in drug discovery and development. Advancement in studying the association of cancer with GPCRs is inevitable to manipulate these receptors for targeting tumor development and metastasis.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Footnotes
Peer review under responsibility of Xi'an Jiaotong University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpha.2020.01.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lundstrom K. Structural genomics of GPCRs. Trends Biotechnol. 2005;23:103–108. doi: 10.1016/j.tibtech.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Rask-Andersen M., Almen M.S., Schioth H.B. Trends in the exploitation of novel drug targets. Nat. Rev. Drug Discov. 2011;10:579–590. doi: 10.1038/nrd3478. [DOI] [PubMed] [Google Scholar]
- 3.Young D., Waitches G., Birchmeier C. Isolation and characterization of a new cellular oncogene encoding a protein with multiple potential transmembrane domains. Cell. 1986;45:711–719. doi: 10.1016/0092-8674(86)90785-3. [DOI] [PubMed] [Google Scholar]
- 4.Noguchi K., Herr D., Mutoh T. Lysophosphatidic acid (LPA) and its receptors. Curr. Opin. Pharmacol. 2009;9:15–23. doi: 10.1016/j.coph.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Krumm B.E., Grisshammer R. Peptide ligand recognition by G protein-coupled receptors. Front. Pharmacol. 2015;6:48. doi: 10.3389/fphar.2015.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balkwill F. Cancer and the chemokine network. Nat. Rev. Cancer. 2004;4:540–550. doi: 10.1038/nrc1388. [DOI] [PubMed] [Google Scholar]
- 7.Matsuo Y., Raimondo M., Woodward T.A. CXC-chemokine/CXCR2 biological axis promotes angiogenesis in vitro and in vivo in pancreatic cancer. Int. J. Cancer. 2009;125:1027–1037. doi: 10.1002/ijc.24383. [DOI] [PubMed] [Google Scholar]
- 8.Xu J., Zhang C., He Y. Lymphatic endothelial cell-secreted CXCL1 stimulates lymphangiogenesis and metastasis of gastric cancer. Int. J. Cancer. 2012;130:787–797. doi: 10.1002/ijc.26035. [DOI] [PubMed] [Google Scholar]
- 9.Tang J., Li Z., Lu L. β-Adrenergic system, a backstage manipulator regulating tumour progression and drug target in cancer therapy. Semin. Cancer Biol. 2013;23:533–542. doi: 10.1016/j.semcancer.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Labrie F., Belanger A., Luu-The V. Gonadotropin-releasing hormone agonists in the treatment of prostate cancer. Endocr. Rev. 2005;26:361–379. doi: 10.1210/er.2004-0017. [DOI] [PubMed] [Google Scholar]
- 11.Meyer T., Caplin M.E., Palmer D.H. A phase Ib/IIa trial to evaluate the CCK2 receptor antagonist Z-360 in combination with gemcitabine in patients with advanced pancreatic cancer. Eur. J. Cancer A. 2010;46:526–533. doi: 10.1016/j.ejca.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 12.U S Food and Drug Administration https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm (accessed 10 August 2018).
- 13.Xiang Y., Yao X., Chen K. The G-protein coupled chemoattractant receptor FPR2 promotes malignant phenotype of human colon cancer cells. Am. J. Cancer Res. 2016;6:2599–2610. [PMC free article] [PubMed] [Google Scholar]
- 14.Su L.D., Peng J.M., Ge Y.B. Formyl peptide receptor 2 mediated chemotherapeutics drug resistance in colon cancer cells. Eur. Rev. Med. Pharmacol. Sci. 2018;22:95–100. doi: 10.26355/eurrev_201801_14105. [DOI] [PubMed] [Google Scholar]
- 15.Schuller H.M. Regulatory role of G protein-coupled receptors in pancreatic cancer development and progression. Curr. Med. Chem. 2017;25:2566–2575. doi: 10.2174/0929867324666170303121708. [DOI] [PubMed] [Google Scholar]
- 16.Chow L., Rezmann L., Imamura K. Functional angiotensin II type 2 receptors inhibit growth factor signaling in LNCaP and PC3 prostate cancer cell lines. The Prostate. 2008;68:651–660. doi: 10.1002/pros.20738. [DOI] [PubMed] [Google Scholar]
- 17.Zhou C., Dai X., Chen Y. G protein-coupled receptor GPR160 is associated with apoptosis and cell cycle arrest of prostate cancer cells. Oncotarget. 2016;7:12823–12839. doi: 10.18632/oncotarget.7313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maussang D., Mujic-Delic A., Descamps F.J. Llama-derived single variable domains (nanobodies) directed against chemokine receptor CXCR7 reduce head and neck cancer cell growth in vivo. J. Biol. Chem. 2013;288:29562–29572. doi: 10.1074/jbc.M113.498436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang M., Zhong W.W., Srivastava N. G protein-coupled lysophosphatidic acid receptors stimulate proliferation of colon cancer cells through the β-catenin pathway. Proc. Natl. Acad. Sci. U. S. A. 2005;102:6027–6032. doi: 10.1073/pnas.0501535102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2016. CA A Cancer J. Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 21.Wang J., Weng J., Cai Y. The prostate-specific G-protein coupled receptors PSGR and PSGR2 are prostate cancer biomarkers that are complementary to alpha-methylacyl-CoA racemase. The Prostate. 2006;66:847–857. doi: 10.1002/pros.20389. [DOI] [PubMed] [Google Scholar]
- 22.Neuhaus E.M., Zhang W., Gelis L. Activation of an olfactory receptor inhibits proliferation of prostate cancer cells. J. Biol. Chem. 2009;284:16218–16225. doi: 10.1074/jbc.M109.012096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu M., Zhao Y.Y., Yang F. Evidence for a role of GPRC6A in prostate cancer metastasis based on case-control and in vitro analyses. Eur. Rev. Med. Pharmacol. Sci. 2016;20:2235–2248. [PubMed] [Google Scholar]
- 24.Ye R., Pi M., Cox J.V. CRISPR/Cas9 targeting of GPRC6A suppresses prostate cancer tumorigenesis in a human xenograft model. J. Exp. Clin. Cancer Res. 2017;36:90. doi: 10.1186/s13046-017-0561-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fung S., Forte T., Rahal R. Provincial rates and time trends in pancreatic cancer outcomes. Curr. Oncol. 2013;20:279–281. doi: 10.3747/co.20.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kisfalvi K., Eibl G., Sinnett-Smith J. Metformin disrupts crosstalk between G protein–coupled receptor and insulin receptor signaling systems and inhibits pancreatic cancer growth. Cancer Res. 2009;69:6539–6545. doi: 10.1158/0008-5472.CAN-09-0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith J.P., Fonkoua L.K., Moody T.W. The role of gastrin and CCK receptors in pancreatic cancer and other malignancies. Int. J. Biol. Sci. 2016;12:283–291. doi: 10.7150/ijbs.14952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sic H., Kraus H., Madl J. Sphingosine-1-phosphate receptors control B-cell migration through signaling components associated with primary immunodeficiencies, chronic lymphocytic leukemia, and multiple sclerosis. J. Allergy Clin. Immunol. 2014;134:420–428. doi: 10.1016/j.jaci.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 30.Runarsson G., Liu A., Mahshid Y. Leukotriene B4 plays a pivotal role in CD40-dependent activation of chronic B lymphocytic leukemia cells. Blood. 2005;105:1274–1279. doi: 10.1182/blood-2004-07-2546. [DOI] [PubMed] [Google Scholar]
- 31.Saada S., Marget P., Fauchais A.L. Differential expression of neurotensin and specific receptors, NTSR1 and NTSR2, in normal and malignant human B lymphocytes. J. Immunol. 2012;189:5293–5303. doi: 10.4049/jimmunol.1102937. [DOI] [PubMed] [Google Scholar]
- 32.Kamp T., Liebl B., Haen E. Defects of beta 2-adrenergic signal transduction in chronic lymphocytic leukaemia: relationship to disease progression. Eur. J. Clin. Investig. 1997;27:121–127. doi: 10.1046/j.1365-2362.1997.700623.x. [DOI] [PubMed] [Google Scholar]
- 33.Mamani-Matsuda M., Moynet D., Molimard M. Long-acting beta2-adrenergic formoterol and salmeterol induce the apoptosis of B-chronic lymphocytic leukaemia cells. Br. J. Haematol. 2004;124:141–150. doi: 10.1046/j.1365-2141.2003.04746.x. [DOI] [PubMed] [Google Scholar]
- 34.Decker S., Finter J., Forde A.J. PIM kinases are essential for chronic lymphocytic leukemia cell survival (PIM2/3) and CXCR4-mediated microenvironmental interactions (PIM1) Mol. Cancer Ther. 2014;13:1231–1245. doi: 10.1158/1535-7163.MCT-13-0575-T. [DOI] [PubMed] [Google Scholar]
- 35.Stamatopoulos B., Meuleman N., De Bruyn C. The histone deacetylase inhibitor suberoylanilide hydroxamic acid (SAHA) induces apoptosis, downregulates the CXCR4 chemokine receptor and impairs migration of chronic lymphocytic leukemia cells. Haematol. Hematol. J. 2010;95:1136–1143. doi: 10.3324/haematol.2009.013847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buchner M., Brantner P., Stickel N. The microenvironment differentially impairs passive and active immunotherapy in chronic lymphocytic leukaemia - CXCR4 antagonists as potential adjuvants for monoclonal antibodies. Br. J. Haematol. 2010;151:167–178. doi: 10.1111/j.1365-2141.2010.08316.x. [DOI] [PubMed] [Google Scholar]
- 37.Burger M., Hartmann T., Krome M. Small peptide inhibitors of the CXCR4 chemokine receptor (CD184) antagonize the activation, migration, and antiapoptotic responses of CXCL12 in chronic lymphocytic leukemia B cells. Blood. 2005;106:1824–1830. doi: 10.1182/blood-2004-12-4918. [DOI] [PubMed] [Google Scholar]
- 38.Niedermeier M., Hennessy B.T., Knight Z.A. Isoform-selective phosphoinositide 3′-kinase inhibitors inhibit CXCR4 signaling and overcome stromal cell–mediated drug resistance in chronic lymphocytic leukemia: a novel therapeutic approach. Blood. 2009;113:5549–5557. doi: 10.1182/blood-2008-06-165068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patrussi L., Capitani N., Martini V. Enhanced chemokine receptor recycling and impaired S1P1 expression promote leukemic cell infiltration of lymph nodes in chronic lymphocytic leukemia. Cancer Res. 2015;75:4153–4163. doi: 10.1158/0008-5472.CAN-15-0986. [DOI] [PubMed] [Google Scholar]
- 40.Yoshie O., Fujisawa R., Nakayama T. Frequent expression of CCR4 in adult T-cell leukemia and human T-cell leukemia virus type 1–transformed T cells. Blood. 2002;99:1505–1511. doi: 10.1182/blood.v99.5.1505. [DOI] [PubMed] [Google Scholar]
- 41.Makita S., Tobinai K. Mogamulizumab for the treatment of T-cell lymphoma. Expert Opin. Biol. Ther. 2017;17:1145–1153. doi: 10.1080/14712598.2017.1347634. [DOI] [PubMed] [Google Scholar]
- 42.Boyle P., Levin B. IARC Press, International Agency for Research on Cancer; 2008. World Cancer Report 2008. [Google Scholar]
- 43.McGuire A., Brown J.A., Malone C. Effects of age on the detection and management of breast cancer. Cancers. 2015;7:908–929. doi: 10.3390/cancers7020815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tuszynski G.P., Rothman V.L., Zheng X. G-protein coupled receptor-associated sorting protein 1 (GASP-1), a potential biomarker in breast cancer. Exp. Mol. Pathol. 2011;91:608–613. doi: 10.1016/j.yexmp.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 45.Hardy S., St-Onge G.G., Joly E. Oleate promotes the proliferation of breast cancer cells via the G protein-coupled receptor GPR40. J. Biol. Chem. 2005;280:13285–13291. doi: 10.1074/jbc.M410922200. [DOI] [PubMed] [Google Scholar]
- 46.Chen J.Q., Russo J. ERalpha-negative and triple negative breast cancer: molecular features and potential therapeutic approaches. Biochim. Biophys. Acta. 2009;1796:162–175. doi: 10.1016/j.bbcan.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Feigin M.E., Xue B., Hammell M.C. G-protein–coupled receptor GPR161 is overexpressed in breast cancer and is a promoter of cell proliferation and invasion. Proc. Natl. Acad. Sci. 2014;111:4191–4196. doi: 10.1073/pnas.1320239111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Home-ClinicalTrials.gov. https://clinicaltrials.gov/ct2/home (accessed 8 August 2018).
- 49.McGuire S. World Health Organization, International Agency for Research on Cancer, WHO Press; Geneva, Switzerland: 2015. World Cancer Report 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Qin Y., Verdegaal E.M., Siderius M. Quantitative expression profiling of G-protein-coupled receptors (GPCRs) in metastatic melanoma: the constitutively active orphan GPCR GPR18 as novel drug target. Pigment Cell Melanoma Res. 2011;24:207–218. doi: 10.1111/j.1755-148X.2010.00781.x. [DOI] [PubMed] [Google Scholar]
- 51.Xu L., Begum S., Barry M. GPR56 plays varying roles in endogenous cancer progression. Clin. Exp. Metastasis. 2010;27:241–249. doi: 10.1007/s10585-010-9322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang L., Chen G., Mohanty S. GPR56 Regulates VEGF production and angiogenesis during melanoma progression. Cancer Res. 2011;71:5558–5568. doi: 10.1158/0008-5472.CAN-10-4543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jin Z., Luo R., Piao X. GPR56 and its related diseases. Prog. Mol. Biol. Transl. Sci. 2009;89:1–13. doi: 10.1016/S1877-1173(09)89001-7. [DOI] [PubMed] [Google Scholar]
- 54.Pérez-Gómez E., Andradas C., Flores J.M. The orphan receptor GPR55 drives skin carcinogenesis and is upregulated in human squamous cell carcinomas. Oncogene. 2013;32:2534. doi: 10.1038/onc.2012.278. [DOI] [PubMed] [Google Scholar]
- 55.Bastiaens M.T., ter Huurne J.A., Kielich C. Melanocortin-1 receptor gene variants determine the risk of nonmelanoma skin cancer independently of fair skin and red hair. Am. J. Hum. Genet. 2001;68:884–894. doi: 10.1086/319500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duffy D.L., Box N.F., Chen W. Interactive effects of MC1R and OCA2 on melanoma risk phenotypes. Hum. Mol. Genet. 2004;13:447–461. doi: 10.1093/hmg/ddh043. [DOI] [PubMed] [Google Scholar]
- 57.Loser K., Brzoska T., Oji V. The neuropeptide alpha-melanocyte-stimulating hormone is critically involved in the development of cytotoxic CD8+ T cells in mice and humans. PLoS One. 2010;5 doi: 10.1371/journal.pone.0008958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nasti T.H., Timares L. MC1R, eumelanin and pheomelanin: their role in determining the susceptibility to skin cancer, Photochem. Photobiol. 2015;91:188–200. doi: 10.1111/php.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.