Highlights
-
•
Non-microsurgical bipedicled reverse sural fasciocutaneous flap as current surgical management of skin defect after traumatic achilles tendon rupture.
-
•
The use of bipedicled (small saphenous vein and perforator artery which originated from peroneal artery) flap is the key to increase the viability and survival of the flap.
-
•
No need split-thickness skin graft (STSG) donor site.
-
•
Functional outcomes of the skin defect on post traumatic Achilles tendon reconstruction, with retained medial sural nerve on its place.
Keywords: Bipedicled reverse sural fasciocutaneous flap, Medial sural nerve, Traumatic Achilles tendon rupture
Abstract
Introduction
The challenging issue that still remains for reverse sural flap is the withstand of the flap against time, the width of coverage area, and the donor site morbidity such as pain after the medial or lateral sural cutaneous nerve harvested.
Presentation of case
A 55 years old male was suffered from traumatic Achilles tendon rupture for 3 months and was repaired with Krakow's technique in a medical center in Pemalang, Indonesia. After the surgery, the defect was revealed as another surgery was planned to cover the skin defect. The author had chosen the bipedicled reverse sural fasciocutaneous flap in regular basis which addressed the superiority and viability of the flap, thus the donor site morbidity was also concerned as the preservation of medial and lateral sural cutaneous nerve, which leading to good quality of life as the patient still could feel and sensate his medial and lateral leg.
Discussion
The bipedicled reverse sural fasciocutaneous flap was successfully covered the skin defect on post traumatic Achilles tendon reconstruction, with retained medial sural nerve on its place, and the remaining harvested skin area was leave opened without skin graft which healed spontaneously.
Conclusion
Bipedicled reverse sural fasciocutaneous flap with retained medial sural nerve offer a good clinical outcome either the viability of the flap and the maintained sensation along the medial and lateral sural cutaneous nerve distribution.
1. Introduction
Published literatures had said the advantage of the reverse sural flap on skin defect of the Achilles tendon area was to establish a good and vital flap and the preservation of donor site area. The growth of harvesting technique was surprisingly numerous in common. Moreover, the donor site area is commonly grafted with split-thickness skin graft (STSG) mostly from anterior thigh and medial leg. This will leave significant morbidity such as intensive bleeding on donor skin graft area, long hospitalization time, the requirement of wound care, and the aesthetic of the donor site. This case report is an example case of reverse sural fasciocutaneous flap to cover the area of Achilles tendon, without the need of STSG, and the preservation of the medial and lateral sural cutaneous graft to maintain the sensation along the medial and lateral leg (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6).
Fig. 1.
The 4 × 4 cm skin defect was seen with tendon based and monofilament non-absorbable suture exposed 3 months after the Achilles tendon repair with Krakow's technique.
Fig. 2.
The design of the flap was done with marker and rechecked the adequate pedicle length.
Fig. 3.
The identification of medial sural cutaneous nerve and small saphenous vein. Note the sural nerve was retained and preserve, only the small saphenous vein was ligated. The subcutaneous fat along the pedicle was elevated, creating the adipofascial pedicle.
Fig. 4.
The skin flap was raised with the pedicle and rotated 180° into the skin defect. The sural nerve remains on its place.
Fig. 5.
Post-operative appearance of the distal leg.
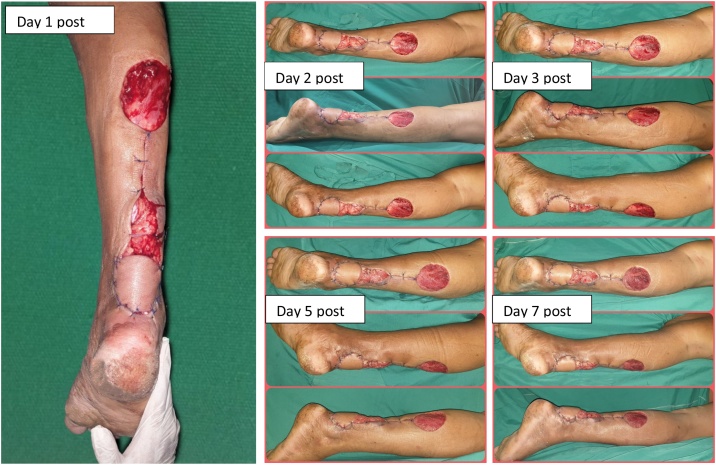
Fig. 6.
Follow up of the vitality of the flap within the first week. The bloody donor site after the first postoperative day was diminished on the next day.
2. Presentation of case
A 55 years old male presented with skin defect above the Achilles tendon area after underwent surgery due to traumatic total Achilles tendon after motor vehicle collision that caused significant pain and disability of the limb. The patient fell down from his bike and broke his foot then brought to hospital with ambulance. The surgeon managed the Achilles tendon repair with Krakow's technique. At the end of third month post-surgery, the skin managed to cover the Achilles tendon but unable to heal spontaneously and leave the exposed area of Achilles tendon with the remaining suture obviously. The surgeon then decided to perform bipedicled reverse fasciocutaneous flap to cover the skin defect. The surgery was carried out at Siaga Medika Hospital, Pemalang, Indonesia. There is no drug history, family history including any relevant genetic information and psychosocial history. The patient agreed to participate on this report and for publication of the images by the informed consent.
2.1. Surgical technique
Bipedicled reverse sural fasciocutaneous flap with adipofascial pedicle advancement on the defect area was performed by the orthopaedic hip and knee surgeon for 20 years. The surgery was performed under spinal anesthesia and the patient was placed on prone position with pillow to support his upper trunk. Pre-design of the reverse sural flap using surgery marker was an important thing to do before draping. We underwent debridement of the wound and remove the exposed polyethylene non-absorbable suture from the previous surgery to ensure the good quality of wound bed preparation. After debridement, we changed the drape and made a design for the skin defect coverage. The design was rechecked with placement of sterilized gauze beside the skin to accurately measured the length of pedicle, and we flipped over the gauze as if the same procedure will be applied to reverse sural flap.
After that, the circumferential incision of skin flap was made by taking all of the skin with fascia above the gastrocnemius muscle. Identified the medial sural nerve, small saphenous vein in the middle of circular skin flap was very important, as if the sural vein was retained later, not to be involved with the skin flap. The small saphenous vein and sural artery were ligated at the superior and inferior of the incision and trimmed away, the upper half circumferential skin flap was sutured with absorbable multifilament from fascia to skin. Then we made longitudinal incision just below the circumferential skin paddle to the Achilles skin defect. The skin was elevated subcutaneously, leaving the subcutaneous fat under the skin to be attached to the leg.
We attained to harvest the adipofascial pedicle 2.5 cm of each lateral and medial side with the longitudinal incision as a guide, making the total width of pedicle was 5 cm. The advantage of this surgery is when we raised the adipofascial based pedicle, the medial sural cutaenous nerve was retained, only the pedicle flap without medial sural cutaneous nerve was taken, thus the sensoric of medial and lateral side of the leg was preserved for the better functional outcome. Afterwards, the pedicle and skin paddle raised and flipped 180° of rotation, 5–7 cm above the lateral malleolus (pivot point) to covered the Achilles skin defect.
The uncovered skin was leave opened without skin grafting, presumed it would heal secondarily with the mainstay of the connective tissue over the donor site area and the subcutaneous fat over the pedicle. We closed the remaining skin with monofilament non-absorbable suture. The vitality of the flap was observed every day in the first week to re-ensure the blood supply to the flap, and replacing the gauze with tulle and the well prepared gauzed that already soaked then pressed into the normal saline solution. Patient was in charge post-surgery for seven days then discharged with home care and visit by nurse. Followed up done without outcome measure, vitality of flap by palpation and the skin color was similar to surrounding skin, granulation and maturation of skin defect reached the optimal healing and all defects closed within six weeks after the surgery. The patient could back to walk without any complication and return to his hobby; cycling.
3. Discussion
The injury of the Achilles tendon area often requires surgical management due to the skin defect that has no capability to be healed secondarily. Although it was a small defect, the Achilles tendon will exposed and prone to infection and the tendon would be exhausted, finally the functional of the limb won’t be restored [[1], [2], [3]]. The traditional method of harvesting reverse sural flap is either fasciocutaneous or adipofascial, which told by many literatures and different techniques, chosen by the surgeon preference without any differences of flap size, pedicle length, and flap rotation angle [[4], [5], [6], [7]]. Other advantage of sural flap is reduce the time-consuming of microsurgical procedure that provided by free flap, simple design and requires a small team and less instrumentation in operating room [4,8,9].
Since the sural flap was first described by Alain Masquelet in 1992, the development of effective and aesthetic sural flap was increasingly growth [10]. The excellence of fasciocutaneous flap had shown by Dhua et al. [11], conducted 40 patients with 95% of success rate, while Mahmood et al. [12] reported 15 children that undertaken adipofascial flap with 1 year follow up were done with satisfactory result. Parajuli et al. [13] reported 17 patients with composition of 14 patients with fasciocutaneous flap and the rest three were adipofascial flap, and all survived. Ignatiadis et al. [14] had described 16 patients of diabetic foot was successfully covered with fasciocutaneous flap. Although the techniques have limitations, the appropriate selected patient, informed consent, and viable option for soft tissue coverage are limitless for the decision of soft tissue coverage [10,[15], [16], [17]].
The anatomy of sural flap has been studied in many literatures. The classic technique of sural flap is consisted of medial sural cutaneous nerve, small saphenous vein, and perforator vessel comes from peroneal artery. The dissection of cadaveric study shown the medial and lateral sural cutaneous nerves were coarse in parallel, form the separate sural nerve distally [2,18,19]. The successful of this report was the remaining of sural nerves were left to its place when flap surgery was undertaken, nevertheless the flap was survived in time. The other factor is the reverse sural flap has various arc of rotation, rotated 60–180° has been reported with satisfactory result without complication. Both subcutaneous tunnel or exteriorizing the skin flap to reached the defect area was reported in good result [11,13,20].
Many authors were traditionally covered the donor site with split-thickness skin graft (STSG). It has been developed into a trusted method to give faster coverage of the donor site. The reported cases with the use technique donor site closure are various, such as STSG, Vacuum assisted closure (VAC) and dermal subtitutes [21]. The author prefers the secondary healing of the donor site with the advantage of less operation time and instrumentation, diminished extra donor site morbidity which causing pain and less aestethic, also lessen the work burden of the nursing staff for wound care treatment.
4. Conclusion
The use of bipedicled (small saphenous vein and perforator artery which originated from peroneal artery) flap is the key to increase the viability and survival of the flap. The bulky appearance of adipose pedicle could be managed later with lipotomy to improve the aestethic appearance. The work has been reported in line with SCARE 2018 criteria [22].
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
The authors report no external source of funding during the writing of this article.
Ethical approval
Ethical approval was not required in the treatment of the patient in this report.
Consent
Written consent has been received from the subject.
Author’s contribution
Robin Novriansyah contributes in the study concept or design, data collection, analysis and interpretation, oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Ido Prabowo contributes to the study concept or design, data collection and writing the paper.
Sashia Laras contributes to the study concept or design, data collection and writing the paper.
Registration of research studies
Not applicable.
Guarantor
Robin Novriansyah is the sole guarantor of this submitted article.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Disclaimer
No patient or author details are included in the figures.
Transparency document
The Transparency document associated with this article can be found in the online version [[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22]].
References
- 1.Googe B., Songcharoen S.J., Arnold P.B. Handbook of Lower Extremity Reconstruction. Springer; 2020. Soft tissue reconstruction of the distal third tibia; pp. 273–283. [Google Scholar]
- 2.Chi Z., Chen Y., Chu T., Gao W., Li Z., Yan H. Distally based sural neuro-fasciocutaneous perforator flap for foot and ankle reconstruction: surgical modifications for flap pedicle and donor site closure without skin graft. J. Plast. Reconstr. Aesthet. Surg. 2018;71(2):224–231. doi: 10.1016/j.bjps.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Bullocks J.M., Hickey R.M., Basu C.B., Hollier L.H., Kim J.Y. Single-stage reconstruction of Achilles tendon injuries and distal lower extremity soft tissue defects with the reverse sural fasciocutaneous flap. J. Plast. Reconstr. Aesthet. Surg. 2008;61(5):566–572. doi: 10.1016/j.bjps.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Lee H.Il, Ha S.H., Sun O.Y., Park M.J., Chae S.H., Lee G.J. Reverse sural artery island flap with skin extension along the pedicle. J. Foot Ankle Surg. 2016;55(3):470–475. doi: 10.1053/j.jfas.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Zheng J., Liao H., Li J., Zhuo L., Ren G., Zhang P. Double-pedicle propeller flap for reconstruction of the foot and ankle: anatomical study and clinical applications. J. Int. Med. Res. 2019;47(10):4775–4786. doi: 10.1177/0300060519865625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raveendran S.S., Perera D., Happuharachchi T., Yoganathan V. Superficial sural artery flap—a study in 40 cases. Br. J. Plast. Surg. 2004;57(3):266–269. doi: 10.1016/j.bjps.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Sabapathy S.R., Venkataramani H., Latheef L., Bhardwaj P. Reconstruction of segmental defects of Achilles tendon: is it a must in infected complex defects? Indian J. Plast. Surg. 2013;46(1):121. doi: 10.4103/0970-0358.113729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim K.J., Ahn J.T., Yoon K.T., Lee J.H. A comparison of fasciocutaneous and adipofascial methods in the reverse sural artery flap for treatment of diabetic infected lateral malleolar bursitis. J. Orthop. Surg. 2019;27(1) doi: 10.1177/2309499019828546. 2309499019828546. [DOI] [PubMed] [Google Scholar]
- 9.Mbaga A.C., Guifo M.L., Itambi M.A., Ernest K.N., Batimba L., Tchamou C. Traumatic rupture of Achilles tendon: importance of the sural fasciocutaneous flap. World J. Surg. Surg. Res. 2019;2:1089. [Google Scholar]
- 10.Masquelet A.C., Romana M.C., Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast. Reconstr. Surg. 1992;89(6):1115–1121. doi: 10.1097/00006534-199206000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Dhua S., Manashree S., Tilak B.G. The clinical outcome of perforator based sural artery and propeller flaps in reconstruction of soft tissue of extremities. World J. Plast. Surg. 2019;8(1):3. doi: 10.29252/wjps.8.1.3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahmood F., Khan M.A., Iqbal Y. Adipofascial sural artery flap for foot and ankle reconstruction in children: for better aesthetic outcome. Ann. King Edward Med. Univ. 2015;21(1):48. [Google Scholar]
- 13.Parajuli N.P., Shrestha D., Panse N. Distally based sural faciocutaneous and fascial (adipofascial) flap for reconstruction of distal leg, ankle and foot defects. Kathmandu Univ. Med. J. 2014;12(2):126–131. doi: 10.3126/kumj.v12i2.13659. [DOI] [PubMed] [Google Scholar]
- 14.Ignatiadis I.A., Tsiampa V.A., Galanakos S.P., Georgakopoulos G.D., Gerostathopoulos N.E., Ionac M. The reverse sural fasciocutaneous flap for the treatment of traumatic, infectious or diabetic foot and ankle wounds: a retrospective review of 16 patients. Diabet. Foot Ankle. 2011;2(1):5653. doi: 10.3402/dfa.v2i0.5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mok W.L.J., Por Y.C., Tan B.K. Distally based sural artery adipofascial flap based on a single sural nerve branch: anatomy and clinical applications. Arch. Plast. Surg. 2014;41(6):709. doi: 10.5999/aps.2014.41.6.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt K., Jakubietz M., Djalek S., Harenberg P.S., Zeplin P.H., Jakubietz R. The distally based adipofascial sural artery flap: faster, safer, and easier? A long-term comparison of the fasciocutaneous and adipofascial method in a multimorbid patient population. Plast. Reconstr. Surg. 2012;130(2):360–368. doi: 10.1097/PRS.0b013e3182589b0e. [DOI] [PubMed] [Google Scholar]
- 17.Hardy J., Forli A., Charissoux J.-L., Mabit C., Marcheix P.S. Lower-limb flip-flap: a simple reliable modification of adipofascial flap for extensive tibial crest cutaneous defect. Orthop. Traumatol. Surg. Res. 2020;106(5):819–823. doi: 10.1016/j.otsr.2020.03.026. [DOI] [PubMed] [Google Scholar]
- 18.Wang F., Zhou D., Li W., Ge M., Zhu D. A new pattern of the sural nerve added to “anatomy of the sural nerve: cadaver study and literature review”. Plast. Reconstr. Surg. Glob. Open. 2017;5(12) doi: 10.1097/GOX.0000000000001628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Punyavong P., Winaikosol K., Jenwitheesuk K., Surakunprapha P., Chowchuen B. An anatomical study of vascular supply of the distally based sural artery flap: a cadaveric study. J. Med. Assoc. Thai. 2016;99(5):S182–6. [PubMed] [Google Scholar]
- 20.Orr J., Kirk K.L., Antunez V., Ficke J. Reverse sural artery flap for reconstruction of blast injuries of the foot and ankle. Foot Ankle Int. 2010;31(1):59–64. doi: 10.3113/FAI.2010.0059. [DOI] [PubMed] [Google Scholar]
- 21.Marchesi A., Parodi P.C., Brioschi M., Riccio M., Perrotta R.E., Colombo M. Soft-tissue defects of the Achilles tendon region: management and reconstructive ladder. Review of the literature. Injury. 2016;47:S147–53. doi: 10.1016/j.injury.2016.07.053. [DOI] [PubMed] [Google Scholar]
- 22.Agha R., Borrelli M., Farwana R., Koshy K., Fowler A., Orgill D. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018:1–10. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.