Abstract
Objective
Although patient–therapist collaboration (working alliance) has been studied extensively in Europe and America, it is unknown to what extent the importance of working alliance for psychotherapy outcome generalizes to lower- and middle-income countries. Additionally, there is a need for more studies on the alliance using methods that are robust to confounders of its effect on outcome.
Method
In this study, 345 outpatients seeking care at the 2 public psychiatric hospitals in Nairobi, Kenya, filled out the Session Alliance Inventory (SAI) and the Clinical Outcomes in Routine Evaluation—Outcome Measure (CORE-OM) during each session. The effect of alliance on next-session psychological distress was modeled using the random intercept cross-lagged panel model, which estimates a cross-lagged panel model on within- and between-subjects disaggregated data.
Results
Changes in the working alliance from session to session significantly predicted change in psychological distress by the next session, with an increase of 1 point of the SAI in a given session resulting in a decrease of 1.27 points on the CORE–OM by the next session (SE = .60, 95% confidence interval [−2.44, −.10]). This finding represents a medium-sized standardized regression coefficient of between .16 and .21. Results were generally robust to sensitivity tests for stationarity, missing data assumptions, and measurement error.
Conclusion
Results affirm cross-cultural stability of the session-by-session reciprocal effects model of alliance and psychological distress-symptoms as seen in a Kenyan psychiatric outpatient sample, using the latest developments in cross-lagged panel modeling. A limitation of the study is its naturalistic design and lack of control over several variables.
Keywords: working alliance, outcome, cross-cultural psychology, cross-lagged panel model
The working alliance, defined as patient–therapist agreement on goals and tasks of therapy in the context of a positive emotional bond (Bordin, 1979), is the most extensively researched psychotherapy process (Crits-Christoph, Connolly Gibbons, & Mukherjee, 2013). However, among the almost 300 studies included in the most recent meta-analysis of the alliance–outcome correlation (Flückiger, Del Re, Wampold, & Horvath, 2018), all were conducted in North America, Europe, or Australia, that is, in Western higher income contexts. There is a paucity of evidence on alliance–outcome relationship from non-Western settings. In particular, studies on working alliance in Sub-Saharan Africa, where psychotherapies have been delivered for the last three to four decades, remain unknown. There is a need for cross-cultural validation of the working alliance concept to better understand the mechanisms of psychotherapies offered in Sub-Saharan African contexts, where huge technological and demographic changes are taking place. Here lies a glaring knowledge gap in the evaluation of cross-cultural psychotherapy practice.
Psychotherapy in Kenya
Psychotherapy in Kenya is offered by counselors (2 years of training at the diploma level), counseling psychologists (3 years of training at the degree level), clinical psychologists (3 years of training at the master’s level), or psychiatrists (medical doctors with 3 years of postgraduate training in psychiatry). The total number of these cadres of therapists in Kenya is less than 400 for a population of 47 million, and the majority of these professionals work in independent practice due to better remuneration than in public health contexts. Therapeutic models in Kenya are often eclectic, influenced by Western psychological models, pastoral counseling, and HIV-counseling programs. Sociocultural and economic factors, including the availability of training, acceptability of appointments and time boundaries, transport availability, and treatment costs, modify patients’ and therapists’ behaviors to create a contextualized, pragmatic style of therapy, for example, giving advice on how to retain jobs, help with food aid or antiretrovirals, and so forth or provide relaxation therapy in a busy clinic where privacy is limited.
Moderators of the Working Alliance Effect on Outcome
As conceptualized by, for example, Bordin (1979), the working alliance should be universally important for psychotherapy outcome. However, different aspects of the alliance might be important in different therapy forms, and the alliance might impact outcome in different ways for different patients. A few studies have looked at moderators of the alliance effect (e.g., Falkenström, Ekeblad, & Holmqvist, 2016; Falkenström, Granström, & Holmqvist, 2013; Flückiger et al., 2018; Lorenzo-Luaces, DeRubeis, & Webb, 2014; Zilcha-Mano & Errázuriz, 2015), but there is a need for further studies in this regard.
Culture is a potential moderator that has so far received little research attention. For a long time, cultural and psychological anthropologists have been questioning the intercultural application of psychotherapies developed in Western contexts (Littlewood, 2001), and this critical lens is important to ensure that psychotherapy is meaningful to people of different cultures and offered in ways that are culturally congruent. Because material and social conditions in different cultural contexts vary, one cannot take the universality of alliance in psychotherapy or mental health treatments for granted.
Causality in Alliance–Outcome Research
Most of the existing studies relating alliance to outcome are simple pre- and posttreatment (prepost) correlational designs, which are relatively weak in terms of causal inference (Shadish, Cook, & Campbell, 2002). Stronger causal interpretations can be made from cross-lagged panel designs, especially if they use disaggregation of within- and between-subjects effects (Falkenström, Finkel, Sandell, Rubel, & Holmqvist, 2017). These designs control for stable between-subjects differences and reverse causation, which are major threats to the validity of prepost correlation designs. Although several studies have used such designs to study the prediction of outcome from alliance (see Zilcha-Mano, 2017, for a review), this research is still in its infancy. In addition, even these studies are based on assumptions that are seldom tested (Falkenström, Finkel, et al., 2017). Many studies ignore the problem of endogeneity associated with simultaneously separating between- and within-subject effects while also adjusting for the effect of the prior value of the outcome variable (Falkenström et al., 2016). In addition, assumptions regarding missing data, measurement error, and stationarity are seldom tested.
Purpose of the Present Study
The primary purpose of the present study was to test whether findings regarding the prediction of next-session psychological distress from working alliance ratings found in Europe and America would hold up in a Kenyan sample. In a practice-based psychotherapy research project on the process and outcome of talking therapy in Nairobi, Kenya (Falkenström, Gee, Kuria, Othieno, & Kumar, 2017), we had already found that the participants were, on average, improving in their psychological functioning as they received mental health care. Like several previous studies (Falkenström et al., 2016; Falkenström et al., 2013; Marker, Comer, Abramova, & Kendall, 2013; Rubel, Rosenbaum, & Lutz, 2017; Zilcha-Mano, 2017; Zilcha-Mano & Errazuriz, 2015; Zilcha-Mano et al., 2016), we were primarily interested in within-subject effects (i.e., session-by-session predictions) because these are more likely to represent causal effects than are between-subjects effects. Improvement in alliance quality in a given session was hypothesized to predict improvement in symptoms-distress by the next session, as in prior studies in Western contexts. To our knowledge, this is the first study of the Alliance–outcome relationship carried out in a Sub-Saharan African public health context.
A secondary purpose of the study was to demonstrate cutting-edge statistical analysis of panel data, using longitudinal structural equation modeling. Models for studying within-subject effects are becoming increasingly popular among psychotherapy process–outcome researchers, but misconceptions abound, and many studies use faulty methods and/or do not realize the full potential of these methods (e.g., Falkenström, Finkel, et al., 2017).
Method
Setting
This was an observational study on regular clinical treatments. Data were collected at two public hospitals: the Mathare National Teaching and Referral Hospital (MNTRH), which is the only psychiatric and mental health teaching and referral hospital in Kenya, and the outpatient Psychiatric Clinic, Department of Mental Health, and Youth Clinic of Kenyatta National Hospital (KNH), a 1,500-bed national teaching and referral hospital, both in Nairobi, Kenya. KNH and MNTRH are teaching hospitals where trainees are posted for clinical experience. Both hospitals have several free services to patients exposed to gender-based violence or affected with HIV, combat veterans and their families, those who are unemployed or disabled, and youth under the age of 24 years. Services for these groups are highly sought after, and a large number of people with low socioeconomic status bank on these national hospitals for specialist care. These were the major factors leading the patients in our study to visit the two hospitals. The psychotherapy offered in the two hospitals is largely unstructured, and patients may be attended to by a different therapist in different sessions. Most of the patients with mental health problems receive some form of talking therapy from the attending specialist, but those who require intense psychotherapy are referred to the counseling or clinical psychologist. Most people with mental health problems prefer to be attended to by a counselor or psychologist due to stigma associated with consulting a psychiatrist.
Procedure
Three research assistants working part time in the project approached treatment-seeking patients assigned to any intervention described by clinicians as “counseling” or “psychotherapy” (the only inclusion criterion in this study), described the study, and asked whether they were willing to participate in the study by filling out questionnaires when coming for their sessions. Patients who gave written informed consent filled out the Clinical Outcomes in Routine Evaluation—Outcome Measure (CORE–OM; Evans et al., 2002) before their sessions and the Session Alliance Inventory (SAI; Falkenström, Hatcher, Skjulsvik, Larsson, & Holmqvist, 2015) after sessions. The project was approved by the Kenyatta National Hospital-University of Nairobi Ethics and Research Committee (P85/02/2014). Data collection started in March 2015 and continued to June 2016.
Participants
A total of 345 participants were recruited by the research assistants. Few patients declined participation (<3%), although a few were unable to fill out questionnaires due to intoxication or psychotic states. The participants attended one of three KNH clinics—Youth Clinic (n = 140), Department of Mental Health (n = 14), or Psychiatric Clinic (n = 11)—or the MNTRH (n = 180). The participants ranged in age from 18 to 60 years (M = 28.9, SD = 9.8). Table 1 shows demographic information about the participants. The majority of the participants were male (72.6%). Diagnoses were established by the intake clinicians using the International Statistical Classification of Diseases and Related Health Problems (Version 10; World Health Organization, 2004). The most common disorders that patients were seeking treatment for were addictions (54.8%), psychosis (17.5%), depression (16.9%), and anxiety-stress (12.0%). Other identified problems that were less common included interpersonal problems, physical problems, work-academic problems, self-esteem problems, or trauma-abuse. The patients were treated with a variety of therapies, for example, cognitive-behavioral therapy, interpersonal psychotherapy, addiction counseling, supportive therapy, family therapy, psychoeducation, and brief solution-focused therapy.
Table 1.
Demographic Information About Participating Patients
| Variable | N | % |
|---|---|---|
| Sex | ||
| Male | 249 | 72.59 |
| Female | 94 | 27.41 |
| Previous therapy | 55 | 16.22 |
| Presenting problems | ||
| Addictions | 188 | 54.81 |
| Psychosis | 60 | 17.49 |
| Depression | 58 | 16.91 |
| Anxiety–stress | 41 | 11.95 |
| Interpersonal problems | 22 | 6.41 |
| Physical problems | 22 | 6.41 |
| Work–academic problems | 22 | 6.41 |
| Other problems | 22 | 6.41 |
| Self-esteem problems | 17 | 4.96 |
| Trauma–abuse | 16 | 4.66 |
| Personality problems | 15 | 4.37 |
| Eating disorders | 11 | 3.21 |
| Living–welfare | 12 | 3.50 |
| Bereavement–loss | 8 | 2.33 |
Therapists
The therapists were either full-time mental health professionals employed by the hospitals to offer mental health services or postgraduate interns from clinical psychology, psychiatry, nursing, and counseling fields assisting in delivering clinical services. Therapists wanted to be anonymous, so there was no information on therapists except their gender and mental health professional–resident status. About two thirds of patients (67%) were treated by professional psychotherapists, and 70% of the sessions were conducted by male therapists.
Measures
English versions of self-report measures were used in the study. English is one of the two official languages of Kenya, and most people in Nairobi speak English well. Kiswahili versions were prepared but did not need to be used.
Session Alliance Inventory (SAI; Falkenström, Hatcher, Skjulsvik, et al., 2015)
The SAI is a six-item measure of working alliance based on items taken from the Working Alliance Inventory (WAI; Hatcher & Gillaspy, 2006; Horvath & Greenberg, 1989). Similar to the WAI, the SAI contains items reflecting the three theoretical aspects of alliance: agreement on goals and on tasks of treatment and a positive emotional bond. In contrast to the case in the WAI, the SAI items do not reflect the three dimensions equally (i.e., there is not an equal number of items for goal, task, and bond); rather, half of the items are bond items and half are goal or task items. Although this may seem to put undue emphasis on bond compared to goal and task, it has been empirically shown that goal and task are indistinguishable, whereas bond constitutes a separate but correlated factor (e.g., Falkenström, Hatcher, & Holmqvist, 2015; Falkenström, Hatcher, Skjulsvik, et al., 2015). Still, this difference should be borne in mind when interpreting results based on the SAI.
In contrast to most alliance measures, the SAI asks for the patient’s experience of the alliance in the most recent session, whereas most other alliance measures ask for a more global experience of the alliance. This is based on the idea that the SAI should be used for repeated administrations during therapy. Another difference from the WAI is that the SAI is scored on a scale from 0 (Not at all) to 5 (Completely) rather than 1 (Never) to 7 (Always), as in the WAI. Initial psychometric evaluation of the SAI has been positive (Falkenström, Hatcher, Skjulsvik, et al., 2015). In particular, the SAI has shown measurement invariance (Falkenström, Hatcher, Skjulsvik, et al., 2015), that is, a stable factor structure across repeated administrations, which is crucial for a measure that is to be applied repeatedly over time. If measurement invariance does not hold, observed scores from different time points cannot be compared, because the factor structure is different for the different measurements. The SAI is intended to be used as a unidimensional measure; that is, only the total score should be used. The SAI total score showed good internal consistency (α = .88).
Clinical Outcomes in Routine Evaluation—Outcome Measure (Evans et al., 2002)
The CORE–OM is a self-report measure consisting of 34 items measuring psychological distress experienced during the preceding week on a 5-point scale ranging from 0 (Not at all) to 4 (Most or all the time). The items cover four major problem areas: subjective well-being, problems–symptoms, life functioning, and risk (to self or others). Higher scores indicate greater distress. The CORE–OM has shown good internal and test-retest reliability (.75–.95), convergent validity, large differences between clinical and nonclinical samples, and good sensitivity to change. A factor analysis on the present sample showed that the CORE–OM has a strong general distress factor and that the only subscale that added anything on top of that was the risk scale (Falkenström, Kumar, Zahid, Kuria, & Othieno, 2018). Thus, only the total score was used, which had excellent internal consistency (α = .94).
CORE therapy assessment form (CORE-A; Evans et al., 2002)
The CORE-A consists of patient demographic information, identified problems–concerns, assessments of risk to self–others, and so forth. Because it was developed mainly as an information-gathering form to be completed by practitioners, not as a psychometric measure, there are no conventional psychometric studies on it. A slightly shortened version, which can be obtained from the authors upon request, was used.
Statistical Analysis
The data were analyzed using cross-lagged panel analysis, to be able to correctly model the time structure of the data. The structure of the data was complicated because a large number of patients attended only one or a few sessions, with N diminishing rapidly with each session. This structure is similar to naturalistic data from other countries (e.g., Falkenström et al., 2013). There are several advantages to using structural equation models for panel data, especially when the time-series dimension (T) is short but sample size (N) is fairly large. The most important advantage compared to alternative modeling strategies (e.g., multilevel modeling) is the possibility of separating within- and between-subjects variances at the same time as including a lagged dependent variable as covariate without inducing endogeneity problems (e.g., Falkenström, Finkel, et al., 2017). Other advantages include the possibility of relaxing stationarity assumptions, that is, assumptions regarding the stability of the means, variances, and covariances across time. In addition, standard structural equation model fit indices can be used to evaluate model fit. We decided to use the random intercept cross-lagged panel model (RI-CLPM; Hamaker, Kuiper, & Grasman, 2015), because it is explicitly developed to separate within-from between-subjects variance, in contrast to the traditional cross-lagged panel model and some other variations of this model that exist. This is done by estimating the cross-lagged regressions on latent within-subject deviation scores, represented in the model by residuals from the random intercept model. This means that cross-lagged paths can be interpreted as the effects of changes over time in one variable on changes over time in the other variable. The random intercept captures average between-subjects differences, blocking potential confounding with effects of unobserved higher level (e.g., patient, therapist, or clinic) variables as long as their effects are constant over time. This strengthens the possibility for causal interpretation considerably compared to the case in traditional statistical models. In the present study we used data from the first five sessions, because the data were too sparse in Sessions 6, 7, and 8.
Initial model tests and modifications were done using maximum likelihood estimation (MLE) with robust standard errors, with missing data handled by full information maximum likelihood. More complex models had to be estimated using Bayesian estimation, which performs better than does MLE in complex models with relatively sparse data (Gelman et al., 2014). Additional advantages of Bayesian estimation include that error variances (and other model parameters) are not assumed to be normally distributed and that there is no risk for inadmissible estimates (e.g., negative error variances). For more information on Bayesian estimation, see the online supplemental materials.
Statistical power was determined by running Monte Carlo simulations. The model with five time points was run with several combinations of effect and sample sizes. The simulations, using 1,000 simulated samples, showed that for a medium-sized effect (β = .30), adequate power could almost be obtained (power = 78%) with a sample as small as n = 50 (with a balanced design and no missing data). Increasing to N = 100, a similar result (power = 75%) was obtained for a small-to-medium effect size (β = .20). Finally, using the data pattern of the present study (i.e., the proportions of missing data for each session from Table 2; e.g., n = 345 for CORE–OM and n = 325 for SAI at Session 1, then n = 271 for CORE–OM at Session 2, and so on), it was found that for a medium-sized effect (β = .30), power was high (94%), whereas for a small-to-medium effect size (β = .20), power was only 62%. It is important to note that regression coefficients and standard errors were estimated with minimal bias in all analyses (e.g., relative coefficient bias <1.2% bias, relative standard error bias <2.5% for the small-to-medium effect size condition with unbalanced design). All analyses were done using Mplus Version 8.1 (Muthén & Muthén, 1998–2017).
Table 2.
Descriptive Statistics for the CORE–OM and SAI at Sessions 1–5
| Variable | N | M | SD | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| CORE_t1 | 345 | 14.69 | 7.95 | .00 | 37.06 | .43 | 2.55 |
| CORE_t2 | 271 | 11.78 | 7.04 | .00 | 31.47 | .51 | 2.50 |
| CORE_t3 | 165 | 10.66 | 7.36 | .00 | 32.65 | .71 | 2.63 |
| CORE_t4 | 71 | 9.12 | 5.26 | .00 | 22.06 | .39 | 2.62 |
| CORE_t5 | 38 | 8.89 | 5.67 | .00 | 20.29 | .52 | 2.09 |
| SAI_t1 | 325 | 4.09 | .83 | .67 | 5.00 | −1.33 | 5.38 |
| SAI_t2 | 258 | 4.27 | .78 | 1.17 | 5.00 | −1.20 | 4.14 |
| SAI_t3 | 156 | 4.33 | .70 | 1.00 | 5.00 | −1.33 | 5.60 |
| SAI_t4 | 66 | 4.24 | .80 | .00 | 5.00 | −2.44 | 12.93 |
| SAI_t5 | 37 | 4.03 | .92 | .50 | 5.00 | −1.84 | 7.47 |
Note. CORE–OM = Clinical Outcomes in Routine Evaluation—Outcome Measure; SAI = Session Alliance Inventory; Min = minimum; Max = maximum; t1 –t5 = Time 1–Time 5 (Sessions 1–5).
Results
Descriptive Statistics
Table 2 shows means, standard deviations, ranges, skewness, and kurtosis statistics for the CORE–OM and SAI from Sessions 1–5. As can be seen from the table, the SAI exhibited strong skewness and (especially) kurtosis, with high mean values (>4 [Very much] at each session). The average CORE–OM scores decreased from 14.69 (SD = 7.95) in Session 1 to 8.89 (SD = 5.67) in Session 5, corresponding to an average decrease of 1.16 CORE–OM scores each session. On average, the time interval between sessions was 23.76 days (SD = 25.48); however, this was skewed, with about half the sessions having less than two weeks in between them. There were no intermittently missing data, but the data set was strongly unbalanced with respect to time, with N diminishing rapidly for each extra session (see Table 2).
Test of the Effect of Alliance Quality on Next-Session Symptom Level
An initial RI-CLPM model was set up for the first five sessions (see Figure 1), in which all parameters were constrained to be equal across time, thus assuming a completely stationary process. This model did not fit well to the data according to any model fit criteria, χ2(54, N = 345) = 213.40, p < .001, root-mean-square error of approximation (RMSEA) = .09, 90% confidence interval (CI) [.08, .11], probability RMSEA <.05, p <.001, comparative fit index (CFI) = .64, standardized root-mean-square residual (SRMR) = .28, Akaike information criterion (AIC) = 7,764.63. Stationarity constraints were removed one by one, guided by modification indices and the AIC as criterion for improving model fit. The constraints that were removed were (a) stability of means over time (ΔAIC = −86.07), (b) equality of autoregressions of the SAI (ΔAIC = −16.64), (c) equality of residual variances of CORE–OM (ΔAIC = −19.87), (d) equality of residual variances of SAI (ΔAIC = −16.20), and (e) equality of reverse causation over time (ΔAIC = −8.46). The final model fit reasonably well according to most fit indices, χ2(31, n = 345) = 46.64, p = .04, RMSEA = .04, 90% CI [.01, .06], probability <.05, p = .80, CFI = .96, SRMR = .11, AIC = 7,614.39.
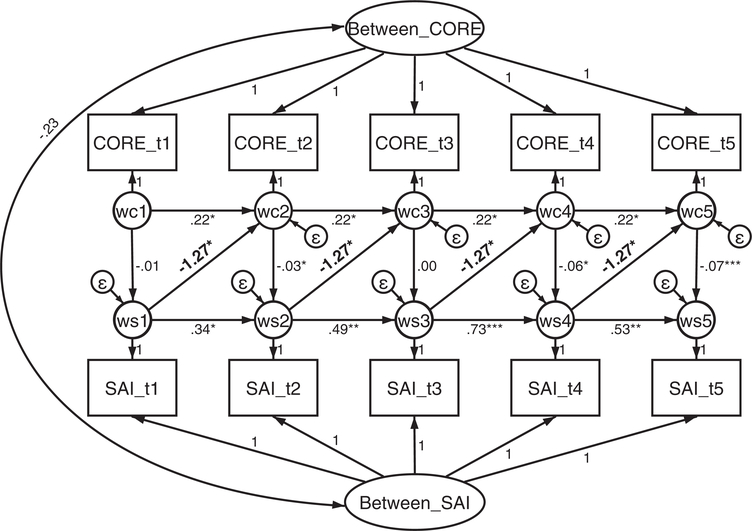
Figure 1.
Random intercept cross-lagged panel model of the Clinical Outcomes in Routine Evaluation—Outcome Measure (CORE—OM) and the Session Alliance Inventory (SAI) over the first five sessions of therapy (represented by t1–t5 [Time 1–Time 5]). Circles represent latent variables, and rectangles represent observed variables. Variables wc1–wc5 and ws1–ws5 are latent within-subject deviation variables (i.e., Level 1 variables), whereas Between_CORE and Between_SAI are the Level 2 random intercepts capturing the between-subjects variances. Estimates are unstandardized regression coefficients, and those in bold appearing diagonally represent the effect of alliance on psychological distress at the next session while holding the present-session psychological distress constant. The vertical paths from the wc to ws variables represent the effects of psychological distress experienced in the previous week on working alliance in the session. Horizontal paths represent autoregression. * p < .05. ** p < .01. *** p < .001.
Figure 1 shows parameter estimates of the final model. The paths from the latent within-subject centered alliance variables (represented in Figure 1 as ws1–ws4) to next-session latent within-subject centered distress (represented in Figure 1 as wc2-wc5) were statistically significant (p = .03). The effect was such that an increase of 1 point on the SAI in a given session would result in a decrease of 1.27 points on the CORE–OM in the next session (SE = .60, 95% CI [−2.44, −.10]; this effect was equivalent to standardized coefficients between .16 and .21 (the variation being due to different variances at different occasions), after controlling for stable between-subjects differences and holding the prior CORE–OM level constant. The paths from CORE–OM to SAI differed from session to session, with significant paths at Sessions 2, 4, and 5. Essentially, the results replicate a reciprocal causation model of the relationship between alliance and symptoms, as shown in prior research (e.g., Xu & Tracey, 2015).
Sensitivity Tests to Violations of Model Assumptions
There are several potential threats to the validity of these findings. Some were considered in the model modifications described in the previous section, whereas others were better explored through sensitivity analyses (i.e., testing the robustness of findings in models that incorporate these threats). Five issues were considered: (a) bias due to including cases with fewer than the minimum number of observations required for estimating the RI-CLPM, (b) bias due to differing time intervals between sessions, (c) bias due to measurement error in the variables used, (d) bias due to missing data, and (e) bias due to shared linear trajectories between variables. Each of these are considered in the next sections. Due to the complexity of these models, they were all (except the one when in which only cases with at least three data points were used) estimated using Bayesian estimation (see the online supplemental materials).
Including only cases with at least three data points
The final model was reestimated on a reduced sample with only patients having at least three data points for both CORE–OM and SAI (N = 147). Model fit for this model was slightly worse than for the full data, although still reasonable according to most criteria, χ2(31, n = 147) = 60.01, p = .001, RMSEA = .08, 90% CI [.05, .11], probability <.05, p = .06, CFI = .93, SRMR = .13. Parameter estimates were similar to those in the model based on the full data, with the effect of SAI on next-session CORE–OM estimated to −1.34 (SE = .68, p = .05).
Varying time between sessions
Because the models used assume equal intervals between sessions, the number of days between sessions was added as a covariate predicting both CORE–OM and SAI. Number of days between sessions was not significantly related to CORE–OM or SAI at any session, and the estimate of the effect of SAI on next-session CORE–OM was unaffected by this (β = −1.37, SE = .66, p = .04).
Measurement error
In simple linear regression analysis with only one predictor, it is known that measurement error in the predictor causes negative bias in the estimated regression coefficient; that is, the estimate is closer to 0 than to the true effect. However, in more complex models, measurement error can cause bias in any direction and should therefore ideally be separated from true variance (Cole & Preacher, 2014). In the context of RI-CLPM, with at least three waves it is possible to estimate residual variances both for the latent within-subject deviation variables and for the observed variables (Kenny & Zautra, 1995), as long as error variances are assumed to be equal across occasions. The residual variances of the observed variables are interpreted as measurement errors, and they affect the observed variable at only a single occasion. In contrast, the residual variances of the latent within-subject centered variables are interpreted as ‘dynamic errors’ or ‘innovations’ (Schuurman, Houtveen, & Hamaker, 2015) because, due to autoregression, they feed forward and also affect subsequent scores (the model is shown in Figure S1 of the online supplemental materials).
A model in which measurement errors in CORE–OM and SAI were assumed to be independent was compared to a model in which errors were allowed to correlate. Both models fit the data well (posterior predictive ps = .46 for both models). Models were compared using the deviance information criterion (DIC; Spiegelhalter, Best, Carlin, & van der Linde, 2002). The model with correlated measurement errors fit slightly worse according to the DIC (correlated errors DIC = 7,619.00; uncorrelated errors DIC = 7,617.70). In addition, the covariance between errors was not statistically significant (β = −.31, p = .11). Measurement error variances were statistically significant for both CORE–OM and SAI; however, separating out measurement error had little effect on the estimate of the effect of SAI on subsequent CORE–OM (β = −1.30, SE = .67, p = .02, 95% CI [−2.65, −.03]).
Missing data analysis
The models used include all available data, an approach that assumes that data are missing at random (MAR; Rubin, 1976). MAR is a less restrictive assumption than is missing completely at random that listwise deletion requires, because in longitudinal data MAR allows missing data to be correlated with any variable at other occasions but the value of the dependent variable at the occasion of missingness is assumed independent of missingness (Enders, 2011). In the present context, this means that the value of CORE–OM should not be the cause of data missingness. This assumption is unlikely to hold, because it is reasonable to think that patients are more inclined to not fill out measures when they are more distressed (or when the alliance is bad). In such a case, it is important to do sensitivity analyses of the MAR assumption. In cross-lagged models, the model that seems most fitting is the Diggle-Kenward selection model (Diggle & Kenward, 1994; see also Falkenström et al., 2013). In this model, the probability of missingness is predicted from the repeated measures of the outcome variable at the previous occasion and at the same occasion (see Figure S2 in the online supplemental materials). Because the value of the outcome variable at the dropout occasion is unknown, this model relies on the assumption of multivariate normality for the repeated-measures variables. This assumption makes it possible to estimate the probability of missingness depending on the value of CORE–OM at the dropout occasion (i.e., the MAR assumption) even though that value is unknown (Enders, 2011).
The selection model fit well (posterior predictive p = .40), and parameter estimates showed that missingness depended on the value of the SAI at the dropout occasion and at the occasion prior to dropout (but the values of CORE–OM were unrelated to missingness). However, as emphasized by Enders (2011), the missingness predictions should not be interpreted substantively, because they depend strongly on distributional assumptions. The effect of SAI on subsequent CORE–OM was unaffected by the modeling of missing data (β = −1.31, SE = .40, p < .001, 95% CI [−2.08, −.54]), although the prediction was more precise due to decreased standard errors. This means that, although the MAR assumption was likely to be violated, the estimated effect of SAI on subsequent CORE–OM was unaffected by modeling this.
Correlated linear trends
It is generally recognized that correlated trends over time in two time series may seriously bias cross-lagged coefficients. The extent to which the correlated trends represent bias is due to the extent these trends represent other causes than the ones tested by the cross-lagged coefficients (Falkenström, Finkel, et al., 2017). If this is the case, time trends should be estimated separately from cross-lagged coefficients (detrending). On the other hand, detrending in a situation when trends are generated by the phenomenon of interest (likely when there is reciprocal causation between the two variables) is a conservative strategy that is likely to yield downwardly biased estimates for the cross-lagged coefficients. Because it is generally unknown whether time trends represent external causes, Falkenström, Finkel, et al. (2017) recommended testing both detrended and not detrended models. It should be noted that the model used so far estimated unrestricted means over time for both SAI and CORE–OM, which means that in one sense the model is already detrended. Specifically, the model separates average changes in means over time for the group as a whole from the covariances used for the cross-lagged part of the model. Thus, any linear or nonlinear average change pattern for the group as a whole is accounted for in the model separately from the cross-lagged path parameters.
However, the model used so far does not consider individual differences in change over time. Stated differently, our model is adjusted for shared trajectories between SAI and CORE–OM across the whole sample but not for individual-specific trajectories. To model individual trajectories requires change to be estimated as linear, because a nonlinear change model with individual differences would not be possible to estimate. Adding a random linear growth factor to the RI-CLPM results in a model described by Curran, Howard, Bainter, Lane, and McGinley (2014; see Figure S3 in the online supplemental materials). This model fit the data well (posterior predictive p = .32). Estimates showed significant fixed and random slopes for both CORE–OM and SAI. In addition, the slopes correlated strongly (β = −.73, p = .004). The effect of detrending was that the effect of SAI on subsequent CORE–OM disappeared completely (β = .05, p = .48). This may mean that the effect of alliance on subsequent symptom level is due to some confounding variable that is changing in a linear fashion across sessions. However, it should be noted that there were no significant effects at the within-subject level; that is, neither autoregression for CORE–OM or SAI nor the effect of CORE–OM on SAI was significant. This most likely means that there were too little data to separate out within-subject effects from between-subjects time trends in this sample. In addition, as mentioned, detrending is a conservative strategy that may result in Type II errors.
To sum up, results were robust to all sensitivity tests except detrending against individual trajectories. This means that findings can be interpreted with more confidence, knowing that they were unlikely to have been affected by the inclusion of patient with fewer than three measurements, variable time between sessions, measurement error, violation of the MAR assumption, or spontaneous improvements affecting the whole sample equally. The result for the individual trajectory detrending is a cause for some concern, though, even if it seems likely that the data were too sparse for this highly complex model.
Moderators of Alliance Effect on Outcome
To explore whether any patient-level variable moderated the Alliance–outcome relationship—that is, whether the alliance is a more important mechanism for some patients than others—we tested a model with a latent interaction term between the alliance and various predictors. The predictors were tested one at a time, to enable separate tests of each. The predictors tested were the four major problem areas that therapists identified in the CORE-A (addictions, psychosis, depression, and anxiety) plus personality problems (because that variable had been found to predict the alliance effect in previous studies), patient gender and age. However, none of the predictors reached statistical significance (all ps > .14).
Discussion
The results of this study showed that changes in the working alliance from session to session predicted reduction in psychological distress–symptoms at the following session. This was an outpatient sample from mostly lower socioeconomic backgrounds seeking treatment at the two public hospitals in Nairobi, Kenya. This is the first study, to our knowledge, that studied Alliance–outcome relationships on the African continent. The study can in part be seen as a cross-cultural replication of findings from other countries (e.g., Falkenström et al., 2013, 2016; Falkenström, Granstrom, & Holmqvist, 2014; Marker et al., 2013; Tasca & Lampard, 2012; Xu & Tracey, 2015) showing a reciprocal influence model between alliance and outcome; that is, distress influencing alliance and alliance simultaneously influencing distress. Relief from psychological distress leads to strengthening of the working alliance between the therapist and client, and as the alliance is improved, psychological distress is lessened in the course of therapy. This finding shows that the work done in public hospitals in low-resource contexts of Nairobi follows processes similar to those that have been shown in psychotherapy in more developed, higher income countries.
The study was based in the two national referral hospitals of Nairobi, which rely on public funds, with patients from very low to low income groups including the large slum areas of Nairobi and also referral patients from the countryside and other rural pockets of Kenya. There are many great challenges in such a setting, from the basic material issues such as covering transportation to the hospital to more socioeconomic issues such as social inequalities inherent in Kenyan society and strong stigma and prejudice associated with mental illness. The traditional cultures also do not recognize mental illness as such; for example, most tribal languages have no word for depression. Moreover, in a low-income group a mentally ill adult becomes economically unviable. A significant number of technological and social class changes are taking place in Kenya; however, mental health is a highly underresourced and poorly serviced sector (Bitta, Kariuki, Chengo, & Newton, 2017; Jenkins et al., 2013). Because public hospitals barely manage to provide cover for all conditions, at the cost of consistency and maintaining the same therapeutic team, there is no guarantee that the patients will see the same therapist at each session. A change of therapist means that the alliance has to be established anew, which is another great challenge. The brief treatments and long average time between sessions seen in our data are most likely due to financial issues, causing patients to wait until absolutely necessary to revisit their therapist. Another issue explaining the long gaps between sessions is that many patients at the Youth Clinic are college students studying at boarding schools, who can come to the clinic only during school holidays.
It may be, however, that these difficult circumstances mean that establishing a working alliance is even more critical to treatment success. Stated differently, there are so many obstacles to creating a good-enough working alliance in these contexts, so that doing so might constitute a large part of the work of therapy. If this is so, it is heartening to see that in most cases therapists and patients seem to be able to form a good alliance and that symptoms decrease on average across therapy sessions. Qualitative studies from this project explore patients’ private theories and attributions of psychopathology and psychotherapy (Mbuthia, Kumar, Falkenström, Kuria, & Othieno, 2018) and therapists’ views on how Western psychotherapy models need to be adapted for use with Kenyan patients (Kumar, Mita, Kuria, Othieno, & Falkenström, 2018).
In this study, the path from symptoms–distress to alliance was significant for only some sessions (Sessions 2, 4, and 5). This is different from findings in previous studies, although we are unaware of any previous study in which the homogeneity of this effect was tested (rather than assumed). We are unable to explain why the reverse effect was nonsignificant at some sessions and not others, however. The most likely explanation is simply random fluctuations due to a relatively small sample, with the loss of power from estimating separate coefficients at each session.
Strengths and Limitations
These results are based on observational data, so causal conclusions cannot be made with certainty. However, a strength of this study is that the statistical models that were used enabled us to rule out some of the potential alternative explanations that cannot be ruled out in traditional Alliance–outcome studies based only on correlation between alliance in one session and prepost outcome. The issue of reverse causation, that is, psychological distress- symptoms impacting on alliance, is explicitly modeled within the RI-CLPM framework. Alternative explanations regarding confounders of the Alliance–outcome correlation are important to consider. The separation of within- from between-subjects variances enabled us to rule out a whole class of confounders that are stable over time, for example, patient variables such as diagnosis, personality, temperament, genes, and so forth, as well as average therapist effects, even though they are not included in the analysis (Moerbeek, 2004). Also, compared to the case in most other studies of within-subject effects, we were able to test, and when necessary relax, stationarity constraints of similar variances and covariances across time (see Falkenström, Finkel, et al., 2017). Finally, the present study added the separation of measurement error from “true” scores, showing that measurement errors did not affect results.
The possible threats to causal inference that remain are confounders that change between sessions and that simultaneously affect both alliance and psychological distress. An example would be some kind of intervention from the therapist’s side that affects psychological distress directly while simultaneously improving the patient’s alliance ratings (but not affecting distress solely indirectly via the alliance, which is also possible but would not invalidate the causal status of the alliance). Results also held up to the sensitivity test for missing data. However, the unbalanced data might have caused a problem if patients who stayed longer in treatment where patients who had stronger effects of changes in the alliance on symptoms, because these patients would then be weighted more heavily due to having more data. This could have been tested by a pattern-mixture model (Little, 1995). However, such a model was not estimable for this data set, probably due to sparse data.
In addition, the results were robust for average group change across sessions, what in the time-series literature is called detrending (controlling for average trends over time). Detrending is important if it is likely that the cross-lagged relationships are affected by general effects of time. Psychological distress can of course change as an effect of time; this is what is meant by spontaneous improvement. It is not quite as obvious that the quality of the working alliance would improve simply by the passage of time, but that may still be a possibility. In the present study, detrending against individual linear change made the working alliance effect, along with everything else on the within-subject level, disappear. The fact that the alliance effect disappeared in this model is a potential problem that could indicate that the effect of the alliance on next-session symptoms is caused by a third variable that changes in a linear fashion across sessions. However, the fact that all effects at the within-subject level disappeared when individual detrending was applied indicates that the data in the present study may have been too sparse to enable separation of within-subject effects of alliance on symptoms from linear change over time.
There are several limitations of the present study. An unknown number of patients (probably at least as many as we had data on) were never approached by the research assistants during the study time due to issues such as unavailability of any of the assistants on a particular day or that a patient was missed at the clinic. It seems likely, however, that the assumption of missing completely at random that is required for listwise deletion may hold for these (although this is of course not testable, because we had no data on these patients). In addition, the measures of patient-level moderators suffer from lack of reliability checks, and there is no information on their validity, so the findings (or lack thereof) for moderators should be interpreted cautiously. Further limitations include lack of information on therapists, their orientation and training, and the fact that it was not possible to test for potential differences in alliance effect among treatments. The data did not conform to normality assumptions, which is also a limitation. With more data, nonlinear models could have been tested; however, with this sample size this would have been too much of a stretch. In addition, the Bayesian estimator does not rely as much on normality assumptions as does maximum likelihood estimation.
Conclusions, Clinical Implications, and Suggestions for Future Research
The findings of this study replicate prior research done in Western countries on the importance of monitoring the fluctuations in the working alliance from session to session. The clinical implication is not necessarily that the therapist should talk to the patient about the alliance in each and every session, but the therapist should be mindful that if the alliance quality decreases in a particular session, symptoms are likely to worsen to the next session, and if the alliance can be improved during a session, symptoms are likely to improve to the next session. Alliance ruptures can be dealt with by applying the rupture-resolution framework of Safran and Muran (2000). In addition, as noted by Falkenström et al. (2016), if a patient appears to have worse symptoms in a given session, it is likely that the working alliance quality will also suffer in that session. This means that the therapist can monitor symptom fluctuations across sessions, and when symptoms deteriorate it is also important to keep an eye on the alliance to prevent a negative spiral in which symptoms deteriorate, leading to worsening of the alliance, which in turn leads to further deterioration of symptoms.
Future research should attempt to study the interrelationships between alliance and therapeutic interventions to see whether the alliance is a precondition for technique to work properly or a mediator of a technique-outcome relationship. Generally, further, more rigorous controlled research in African and other non-Western countries is needed. In addition, moderators of the alliance effect should be investigated further, because it is likely that alliance fluctuations are more important for some patients than for others or in some treatments compared to others. These considerations become important as the global mental health movement puts weight on task-sharing and task-shifting of mental health services in primary health care settings in regions like Kenya (Hanlon et al., 2014; Musyimi et al., 2017). The working alliance is partly an immediate human empathic connection, but it is also a process that develops through training, rigor, and supervision.
Supplementary Material
What is the public health significance of this article?
This study shows that the quality of patient–therapist collaboration (working alliance) in a given session contributes to the improvement of symptomatic distress during the week(s) following that session, for patients treated with talking therapy in a sample of psychiatric patients from two public hospitals in Nairobi, Kenya. Our work can be seen as a cross-cultural replication of prior findings on the Alliance–outcome relationship in psychotherapy from European and North American contexts. It also offers some insights about challenges in the delivery of mental health services in resource- constrained African contexts.
Acknowledgments
We thank the therapists and patients at Kenyatta National Hospital and Mathare National Teaching and Referral Hospital who made this study possible.
The project was supported in 2015–2016 by a MEPI/Prime-K seed grant covered under National Institutes of Health Award 1R24TW008889 to Manasi Kumar and by Sörmland County Council Grants DLL-514111 in 2015 and DLL-569981 in 2016 to Fredrik Falkenström.
Contributor Information
Fredrik Falkenström, Department of Behavioral Sciences and Learning, Linköping University.
Mary Kurias, Department of Psychiatry, University of Nairobi..
Caleb Othieno, Department of Psychiatry, University of Nairobi..
Manasi Kumar, Department of Psychiatry, University of Nairobi..
References
- Asparouhov T, & Muthén BO (2010). Bayesian analysis using Mplus: Technical implementation. Unpublished report.
- Bitta MA, Kariuki SM, Chengo E, & Newton CRJC (2017). An overview of mental health care system in Kilifi, Kenya: Results from an initial assessment using the World Health Organization’s Assessment Instrument for Mental Health Systems. International Journal of Mental Health Systems, 11, 28 10.1186/s13033-017-0135-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordin ES (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16, 252–260. 10.1037/h0085885 [DOI] [Google Scholar]
- Cole DA, & Preacher KJ (2014). Manifest variable path analysis: Potentially serious and misleading consequences due to uncorrected measurement error. Psychological Methods, 19, 300–315. 10.1037/a0033805 [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Connolly Gibbons MB, & Mukherjee D (2013). Psychotherapy process-outcome research In Lambert MJ (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change (6th ed., pp. 298–340). New York, NY: Wiley. [Google Scholar]
- Curran PJ, Howard AL, Bainter S, Lane ST, & McGinley JS (2014). The separation of between-person and within-person components of individual change over time: A latent curve model with structured residuals. Journal of Consulting and Clinical Psychology, 82, 879–894. 10.1037/a0035297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diggle P, & Kenward MG (1994). Informative drop-out in longitudinal data analysis. Journal of the Royal Statistical Society: Series C, Applied Statistics, 43, 49. [Google Scholar]
- Enders CK (2011). Missing not at random models for latent growth curve analyses. Psychological Methods, 16, 1–16. 10.1037/a002264010.1037/a0022640.supp [DOI] [PubMed] [Google Scholar]
- Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J, & Audin K (2002). Towards a standardised brief outcome measure: Psychometric properties and utility of the CORE–OM. British Journal of Psychiatry, 180, 51–60. 10.1192/bjp.180.1.51 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Ekeblad A, & Holmqvist R (2016). Improvement of the working alliance in one treatment session predicts improvement of depressive symptoms by the next session. Journal of Consulting and Clinical Psychology, 84, 738–751. 10.1037/ccp0000119 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Finkel S, Sandell R, Rubel JA, & Holmqvist R (2017). Dynamic models of individual change in psychotherapy process research. Journal of Consulting and Clinical Psychology, 85, 537–549. 10.1037/ccp0000203 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Gee MD, Kuria MW, Othieno CJ, & Kumar M (2017). Improving the effectiveness of psychotherapy in two public hospitals in Nairobi. BJPsych International, 14, 64–66. 10.1192/S2056474000001938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falkenström F, Granström F, & Holmqvist R (2013). Therapeutic alliance predicts symptomatic improvement session by session. Journal of Counseling Psychology, 60, 317–328. 10.1037/a0032258 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Granström F, & Holmqvist R (2014). Working alliance predicts psychotherapy outcome even while controlling for prior symptom improvement. Psychotherapy Research, 24, 146–159. 10.1080/10503307.2013.847985 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Hatcher RL, & Holmqvist R (2015). Confirmatory factor analysis of the patient version of the Working Alliance Inventory—Short Form Revised. Assessment, 22, 581–593. 10.1177/1073191114552472 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Hatcher RL, Skjulsvik T, Larsson MH, & Holmqvist R (2015). Development and validation of a 6-item Working Alliance Questionnaire for repeated administrations during psychotherapy. Psychological Assessment, 27, 169–183. 10.1037/pas0000038 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Kumar M, Zahid A, Kuria M, & Othieno C (2018). Factor analysis of the Clinical Outcomes in Routine Evaluation - Outcome Measures (CORE–OM) in a Kenyan sample. BMC Psychology, 6, 48 10.1186/s40359-018-0260-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wampold B, & Horvath A (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy. Advance online publication. 10.1037/pst0000172 [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, & Rubin DB (2014). Bayesian data analysis (3rd ed.). Boca Raton, FL: CRC Press. [Google Scholar]
- Hamaker EL, Kuiper RM, & Grasman RPPP (2015). A critique of the cross-lagged panel model. Psychological Methods, 20, 102–116. 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Hanlon C, Luitel NP, Kathree T, Murhar V, Shrivasta S, Medhin G, . . . Prince M (2014). Challenges and opportunities for implementing integrated mental health care: A district level situation analysis from five low- and middle-income countries. PLoS ONE, 9(2), e88437 10.1371/journal.pone.0088437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, & Gillaspy JA (2006). Development and validation of a revised short version of the Working Alliance Inventory. Psychotherapy Research, 16, 12–25. 10.1080/10503300500352500 [DOI] [Google Scholar]
- Horvath AO, & Greenberg LS (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36, 223–233. 10.1037/0022-0167.36.2.223 [DOI] [Google Scholar]
- Jenkins R, Othieno C, Okeyo S, Aruwa J, Kingora J, & Jenkins B (2013). Health system challenges to integration of mental health delivery in primary care in Kenya—Perspectives of primary care health workers. BMC Health Services Research, 13, 368 10.1186/1472-6963-13-368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, & Zautra A (1995). The trait-state-error model for multi-wave data. Journal of Consulting and Clinical Psychology, 63, 52–59. 10.1037/0022-006X.63.1.52 [DOI] [PubMed] [Google Scholar]
- Kumar M, Mita S, Kuria MW, Othieno CJ, & Falkenström F (2018). Adaptations and modifications of psychotherapy for greater cultural resonance and congruity: A qualitative study of mental health specialists experiences from Kenya. Manuscript in preparation.
- Little RJA (1995). Modeling the drop-out mechanism in repeated-measures studies. Journal of the American Statistical Association, 90, 1112–1121. 10.1080/01621459.1995.10476615 [DOI] [Google Scholar]
- Littlewood R (2001). Psychotherapy in cultural contexts. Psychiatric Clinics of North America, 24, 507–522. 10.1016/S0193-953X(05)70244-6 [DOI] [PubMed] [Google Scholar]
- Lorenzo-Luaces L, DeRubeis RJ, & Webb CA (2014). Client characteristics as moderators of the relation between the therapeutic alliance and outcome in cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 82, 368–373. 10.1037/a0035994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marker CD, Comer JS, Abramova V, & Kendall PC (2013). The reciprocal relationship between alliance and symptom improvement across the treatment of childhood anxiety. Journal of Clinical Child and Adolescent Psychology, 42, 22–33. 10.1080/15374416.2012.723261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbuthia JW, Kumar M, Falkenström F, Kuria MW, & Othieno CJ (2018). Attributions and private theories of mental illness among young adults seeking psychiatric treatment in Nairobi: An interpretive phenomenological analysis. Child and Adolescent Psychiatry and Mental Health, 12, 28 10.1186/s13034-018-0229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moerbeek M (2004). The consequence of ignoring a level of nesting in multilevel analysis. Multivariate Behavioral Research, 39, 129–149. 10.1207/s15327906mbr3901_5 [DOI] [PubMed] [Google Scholar]
- Musyimi CW, Mutiso VN, Ndetei DM, Unanue I, Desai D, Patel SG, . . . Bunders J (2017). Mental health treatment in Kenya: Task-sharing challenges and opportunities among informal health providers. International Journal of Mental Health Systems, 11, 45 10.1186/s13033-017-0152-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Author. [Google Scholar]
- Rubel JA, Rosenbaum D, & Lutz W (2017). Patients’ in-session experiences and symptom change: Session-to-session effects on a within- and between-patient level. Behaviour Research and Therapy, 90, 58–66. 10.1016/j.brat.2016.12.007 [DOI] [PubMed] [Google Scholar]
- Rubin DB (1976). Inference and missing data. Biometrika, 63, 581–592. 10.1093/biomet/63.3.581 [DOI] [Google Scholar]
- Safran JD, & Muran JC (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York, NY: Guilford Press. [Google Scholar]
- Schuurman NK, Houtveen JH, & Hamaker EL (2015). Incorporating measurement error in n = 1 psychological autoregressive modeling. Frontiers in Psychology, 6, 1038 10.3389/fpsyg.2015.01038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, & Campbell DT (2002). Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton, Mifflin. [Google Scholar]
- Spiegelhalter DJ, Best NG, Carlin BP, & van der Linde A (2002). Bayesian measures of model complexity and fit. Journal of the Royal Statistical Society: Series A, Statistics in Society, 64, 583–639. 10.1111/1467-9868.00353 [DOI] [Google Scholar]
- Tasca GA, & Lampard AM (2012). Reciprocal influence of alliance to the group and outcome in day treatment for eating disorders. Journal of Counseling Psychology, 59, 507–517. 10.1037/a0029947 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2004). ICD-10: International statistical classification of diseases and related health problems. Geneva, Switzerland: Author. [Google Scholar]
- Xu H, & Tracey TJG (2015). Reciprocal influence model of working alliance and therapeutic outcome over individual therapy course. Journal of Counseling Psychology, 62, 351–359. 10.1037/cou0000089 [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. American Psychologist, 72, 311–325. 10.1037/a0040435 [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S, & Errázuriz P (2015). One size does not fit all: Examining heterogeneity and identifying moderators of the Alliance–outcome association. Journal of Counseling Psychology, 62, 579–591. 10.1037/cou0000103 [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S, Muran JC, Hungr C, Eubanks CF, Safran JD, & Winston A (2016). The relationship between alliance and outcome: Analysis of a two-person perspective on alliance and session outcome. Journal of Consulting and Clinical Psychology, 84, 484–496. 10.1037/ccp0000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zyphur MJ, & Oswald FL (2013). Bayesian Estimation and Inference: A User’s Guide. Journal of Management. 10.1177/0149206313501200 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.