Abstract
During infection neuraminidase desialylates platelets and induces their rapid clearance from circulation. The underlying molecular basis, particularly the role of platelet glycoprotein (GP)Ibα therein, is not clear. Utilizing genetically altered mice, we report that the extracellular domain of GPIbα, but neither von Willebrand factor nor ADAM17 (a disintegrin and metalloprotease 17), is required for platelet clearance induced by intravenous injection of neuraminidase. Lectin binding to platelet following neuraminidase injection over time revealed that the extent of desialylation of O-glycans correlates with the decrease of platelet count in mice. Injection of α2,3-neuraminidase reduces platelet counts in wild-type but not in transgenic mice expressing only a chimeric GPIbα that misses most of its extracellular domain. Neuraminidase treatment induces unfolding of the O-glycosylated mechanosensory domain in GPIbα as monitored by single-molecule force spectroscopy, increases the exposure of the ADAM17 shedding cleavage site in the mechanosensory domain on the platelet surface, and induces ligand-independent GPIb-IX signaling in human and murine platelets. These results suggest that desialylation of O-glycans of GPIbα induces unfolding of the mechanosensory domain, subsequent GPIb-IX signaling including amplified desialylation of N-glycans, and eventually rapid platelet clearance. This new molecular mechanism of GPIbα-facilitated clearance could potentially resolve many puzzling and seemingly contradicting observations associated with clearance of desialylated or hyposialylated platelet.
Introduction
More than 100 billion platelets are cleared every day from a human body through a highly efficient and tightly regulated process. Exogenous agents could commandeer the process and accelerate platelet clearance, leading to thrombocytopenia and hemorrhage. One such agent is neuraminidase, which hydrolyzes the glycosidic linkages of sialic acids to the host glycoprotein and as a consequence exposes the penultimate galactoses. Injection of neuraminidase causes thrombocytopenia in mice or rats within a few hours, followed by a gradual rise in the platelet count back to the normal level in 4-5 days due to continuous thrombopoiesis in the body.1,2 Certain bacterial infection involves the release of bacterial neuraminidase in the blood and thrombocytopenia, often before the onset of septic shock.3,4 Moreover, there is accumulating evidence to support the involvement of endogenous neuraminidase in platelet clearance. For example, cold storage of murine platelets induces presentation of lysosomal neuraminidases on the plasma membrane, accelerating their clearance upon infusion into a recipient mouse.5,6 Many antibodies targeting the N-terminal ligand-binding domain (LBD) of platelet glycoprotein (GP)Ibα induce platelet signaling and surface presentation of lysosomal neuraminidase 1 (Neu1), leading to thrombocytopenia.7-9 Binding of plasma von Willebrand factor (VWF) to GPIbα on the platelet produces similar signaling events including desialylation.10-12 Therefore, it appears that neuraminidase is critically involved in platelet clearance.
It has been suggested that after platelet desialylation the exposed galactose residues on the platelet are recognized by the Ashwell-Morell receptor (AMR), also known as the asialoglycoprotein receptor, on the surface of liver macrophages and hepatocytes, thereby inducing internalization of the desialylated platelet by these cells and its clearance from the circulation. In support of this model, injection of neuraminidase does not reduce platelet counts in mice lacking AMR and fast clearance of desialylated platelets is significantly reduced in mice lacking AMR.3,5,13 Consistently, genetic ablation of certain sialyltransferases such as ST3Gal-IV in mice results in constitutive exposure of galactoses on the platelet, accelerated platelet clearance, and a significantly lower platelet count.14 Upon transfusion, St3gal4-/- or desialylated platelets are cleared at a faster rate than wild-type (WT), unless the recipient mice were pretreated with asialofetuin, a competitive inhibitor of AMR.5,15
While the involvement of the AMR in mediating clearance of desialylated platelets has been established, the underlying molecular mechanism remains controversial, as several studies reported seemingly contradictory or confusing observations. AMR is a multi-subunit receptor complex that contains several lectin domains for binding of galactose or galactosamine.16-18 It exhibits a much higher binding affinity and ligand preference for tetra- or triantennary galactoses than di- or mono-antennary ones.17,19,20 In other words, AMR binds primarily exposed galactose residue on N-glycans instead of O-glycans because only the former supports a tetra- or tri-antennary sugar structure. It was observed that proteolytic removal of the N-terminal ligand-binding domain (LBD) of GPIbα enhanced survival of transfused St3gal4-/- platelets or coldstored WT platelets.5,15 Since the LBD of human GPIbα contains 2 N-glycans,21-23 desialylated N-glycans on the LBD were suggested as the ligands for AMR.5,15 However, these experiments were performed on murine platelets, yet murine GPIbα does not contain any N-glycosylation sites (i.e., Asn-X-Ser/Thr) and therefore should have no Nglycans for AMR binding (Online Supplementary Figure S1). The involvement of the LBD in clearance of cold-stored platelets was later attributed to its cold-induced interaction with VWF that does not require N-glycans.11,24 Nonetheless, injection of neuraminidase causes thrombocytopenia in GPIbα-/- mice as in WT ones, but neuraminidase-treated GPIbα-/- platelets are cleared at a slower pace than similarly treated WT ones.3 How GPIbα is involved in neuraminidase-induced platelet clearance remains unresolved.
As a major subunit of the GPIb-IX receptor complex, GPIbα is specifically expressed in the platelet.25 It was recently reported that the juxtamembrane portion of GPIbα contains a structured domain that responds to tensile force.26,27 Mechanical unfolding of this mechanosensory domain (MSD), as a result of VWF or antibody binding under shear, induces GPIb-IX signaling in the platelet that leads to its clearance.9-11 The MSD in both human and murine GPIbα contains several O-glycosylation sites (Online Supplementary Figure S1).10 Here we report that neuraminidase-mediated desialylation of O-glycans in GPIbα induces MSD unfolding and subsequently platelet signaling. Unlike the model of AMR recognizing GPIbα N-glycans, our new mechanism does not require the presence of N-glycans in GPIbα. The novel involvement of GPIbα O-glycans provides a platelet-specific element and explains its facilitating role in mediating clearance of desialylated platelets.
Methods
Human subjects
Citrated whole blood was drawn from healthy volunteers according to a protocol approved by Emory University Institutional Review Board (IRB# 00006228), in which all volunteers gave written informed consent. The collected whole blood was used to prepare platelet-rich plasma (PRP) and plasma. Experiments involving fresh human platelets were performed in accordance with approved IRB protocols.
Materials and mice
Neuraminidase from Arthrobacter ureafaciens was purchased from Sigma-Aldrich (St. Louis, MO, USA), and α2,3-neuraminidase cloned from Streptococcus pneumoniae was from New England Biolabs (Ipswich, MA, USA). C57BL/6J and VWF-/- mice were purchased from Jackson Laboratories (stock ns. 000664 and 003795, respectively). Transgenic hTg, GPIbα-/-, and IL4R-IbαTg mice have been described previously.28,29 St3gal1fl/fl mice carrying LoxP sites on exon 2 (stock n. 006897) were backcrossed in to the C57BL/6J background and paired with Pf4-Cre mice to delete St3gal1 in the megakaryocyte lineage (St3Gal1MK-/-). Similarly, Adam17fl/fl mice (stock n. 009597) were paired with Pf4-Cre mice to delete Adam17 in the megakaryocyte lineage (Adam17MK-/-). Six- to 8-week-old mice of both sexes were used in all experiments. All experiments involving mice were performed in accordance with the protocols approved by the Institutional Animal Care and Use Committee of Emory University, Blood Center of Wisconsin, and University of North Carolina.
Intravenous injection and blood count
Each mouse was injected intravenously with 100 mL saline or 0.5 mU/g bacterial neuraminidase, 0.6 U/g α2,3-neuraminidase in 100 mL saline. Before injection and at indicated time after, approximately 60 mL of whole blood was taken via the facial vein using heparinized micro-hematocrit capillary tube (Fisher Scientific, Pittsburgh, PA, USA) and mixed 9:1 (v/v) with 3.8% sodium citrate in a tube. Blood cell counts were determined on a Sysmex XP- 300 automated hematology analyzer. Platelet counts of Adam17MK-/- mice were obtained by flow cytometry as described.30
In vitro neuraminidase treatment
Citrated human or murine whole blood was collected as described above. 10 mU α2,3,6,8-neuraminidase or equal activity of α2,3-neuraminidase was added to 60 mL citrated PRP, which were mixed and incubated at 37°C for 15, 60 and 180 minutes (min) before being analyzed for glycans.
Laser optical tweezer measurement
Single-molecule force measurement of GPIb-IX was performed as described.26,27 Recombinant biotinylated GPIb-IX, and WM23 coupled to one end of the DNA handle, were prepared as described.27 Before the pulling on desialylated GPIb-IX, 1 U of α2,3-neuraminidase was added to streptavidin beads with immobilized GPIb-IX and incubated at room temperature for 30 min. Data were analyzed as described.26
Statistical analysis
Data are expressed as mean±standard deviation. An unpaired two-tailed t-test analysis was performed for statistical analyses. P<0.05 was considered statistically significant. All analyses were performed using Prism software.
Results
Neuraminidase induces platelet clearance via a GPIbα-dependent but von Willebrand factor-independent and ADAM17-independent mechanism
Neuraminidase from A. ureafaciens, with broad substrate specificity (i.e., α2,3,6,8-neuraminidase), was injected intravenously into WT C57BL/6 mice, followed by periodic blood draw for 4 days and counting of platelets and erythrocytes therein. Compared to those prior to neuraminidase injection (t=0), counts of platelets, but not erythrocytes, became markedly lowered upon neuraminidase injection, reaching a minimum at 24 hours (h) after injection (Figure 1A and B). This result indicates that neuraminidase injection induces platelet clearance, consistent with earlier reports.3
Neuraminidase can desialylate VWF in the plasma and induce its clearance through AMR.13 Desialylated VWF binds the platelet spontaneously.31 Thus, it is possible that desialylated VWF may bind GPIbα and induce platelet signaling and platelet clearance.10,11 To ascertain the involvement of VWF and GPIbα, neuraminidase injection and blood cell count were performed on VWF-/- and IL4RIbαTg mice. In IL4R-IbαTg platelets most of the GPIbα extracellular domain is replaced with that of the α-subunit of interleukin-4 receptor.10,29 Injection of α2,3,6,8- neuraminidase significantly reduced the platelet count in VWF-/- mice to the same extent as it did the WT, but did not change platelet count in IL4R-IbαTg mice (Figure 1A). Neuraminidase injection did not affect the erythrocyte count in either strain (Figure 1B). Overall, these results suggest that GPIbα, but not VWF, is required for efficient clearance of desialylated platelets. GPIbα is proteolyzed, or shed, by ADAM17 from the platelet surface.32,33 Inhibition of GPIbα shedding by targeting ADAM17 or GPIbα can impede platelet clearance.34-36 Neuraminidase treatment of platelets induces ADAM17-mediated shedding of GPIbα.6 Thus, it is possible that desialylation accelerates platelet clearance by inducing GPIbα shedding. To ascertain the involvement of GPIbα shedding, neuraminidase injection and blood cell count were performed on Adam17MK-/- mice, which do not express ADAM17 in their platelets. Injection of α2,3,6,8-neuraminidase induced the same extent of thrombocytopenia in Adam17MK-/- mice as in WT (Online Supplementary Figure S2), which indicates that GPIbα shedding is not required for efficient clearance of desialylated platelets.
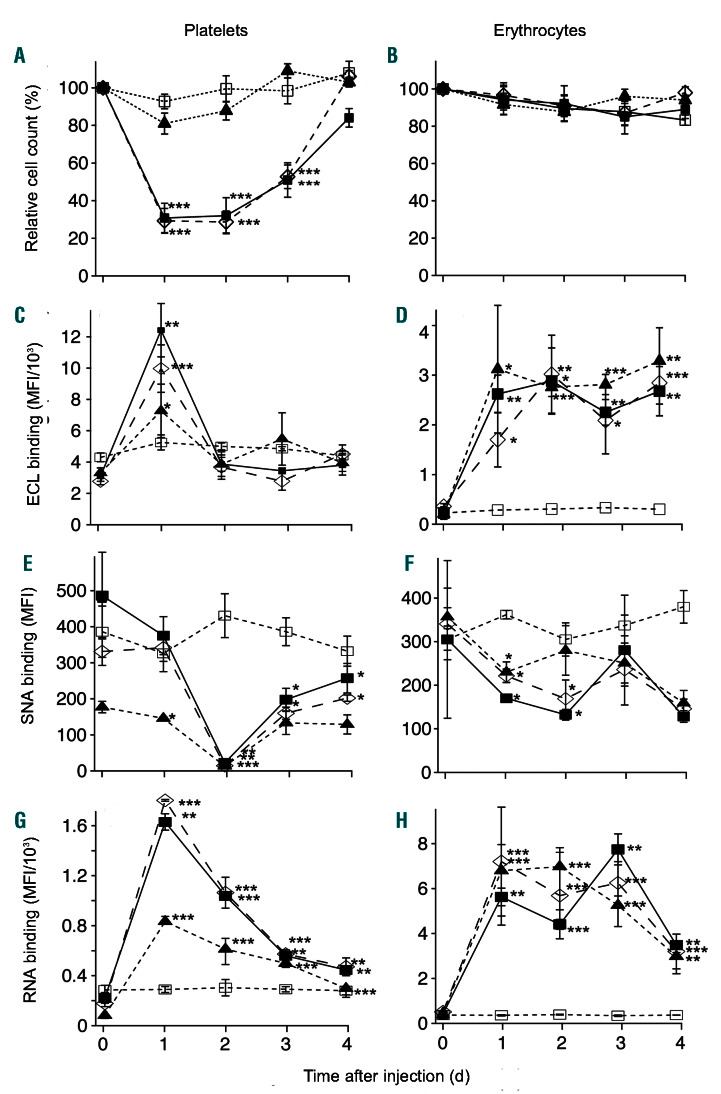
Figure 1.
Effects of infused bacterial α2,3,6,8-neuraminidase on platelets and erythrocytes in mice. A. ureafaciens neuraminidase (0.5 mU/g of body weight) was injected intravenously into wild-type (WT) (), VWF-/- (), or IL4R-IbαTg (▲) mice. Injection of saline into wild-type mice () was performed for comparison. Blood were collected from each mouse via facial vein immediately before (t=0) or days after the injection. Counts of (A) platelets and (B) erythrocytes were performed on a cell counter and normalized with the count before the injection being 100% (mean±standard deviation [SD], n=4). (C, E, G) Platelets and (D, F, H) erythrocytes in the collected whole blood were labeled with cellspecific antibodies and noted lectins (mean±SD, n=3). Each cell was identified through the bound antibody and concurrently the bound lectin detected by flow cytometry. The mean fluorescence intensity (MFI) was calculated for the entire cell population and plotted over the course of days after neuraminidase injection. Comparison to the saline result was performed by unpaired twotailed Student’s t-test. *P<0.05; **P<0.01; ***P<0.001.
Desialylation of O-glycans of GPIbα causes platelet clearance
To characterize the effects of neuraminidase, platelets and erythrocytes were collected from each blood draw before and following neuraminidase injection and their glycan contents were assessed through binding of Erythrina cristagalli lectin (ECL), Sambucus nigra agglutinin (SNA), and Arachis hypogaea agglutinin (peanut agglutinin, PNA) (Figure 1C-H). ECL binds to the unsialylated terminal galactose mono saccharide with the highest affinity for galactosyl(b-1,4) N-acetylglucosamine found in both Nand O-glycans.37,38 SNA specifically binds α2,6-linked sialic acid, which occurs primarily in N-glycans, whereas PNA binds specifically unsialylated core 1 and core 2 O-glycans.39,40 For all three lectins, although actual binding levels were different for platelets from three mouse strains at some time points, the trend was similar through all strains. ECL binding increased significantly to a maximum at 24 h after neuraminidase injection, but returned to the pre-injection level at 48 h and remained essentially unaltered thereafter (Figure 1C). SNA binding changed slightly at 24 h, decreased significantly to a minimum at 48 h, and increased again at 72 h (Figure 1E). Like ECL binding, PNA binding increased significantly to a maximum at 24 h; unlike ECL binding, it decreased gradually thereafter to the pre-injection level (Figure 1G). For erythrocytes from all three strains, the ECL and PNA binding levels increased significantly at 24 h, as expected, while SNA binding decreased (Figure 1D, F, H), verifying that neuraminidase desialylated erythrocytes as well.3 However, the changes in lectin binding levels in erythrocytes thereafter were not similar to those in platelets. Overall, the changes of ECL and SNA binding over time do not correlate with those of platelet count, but that of PNA binding does inversely. These results suggest that desialylation of O-glycans may be involved in platelet clearance.
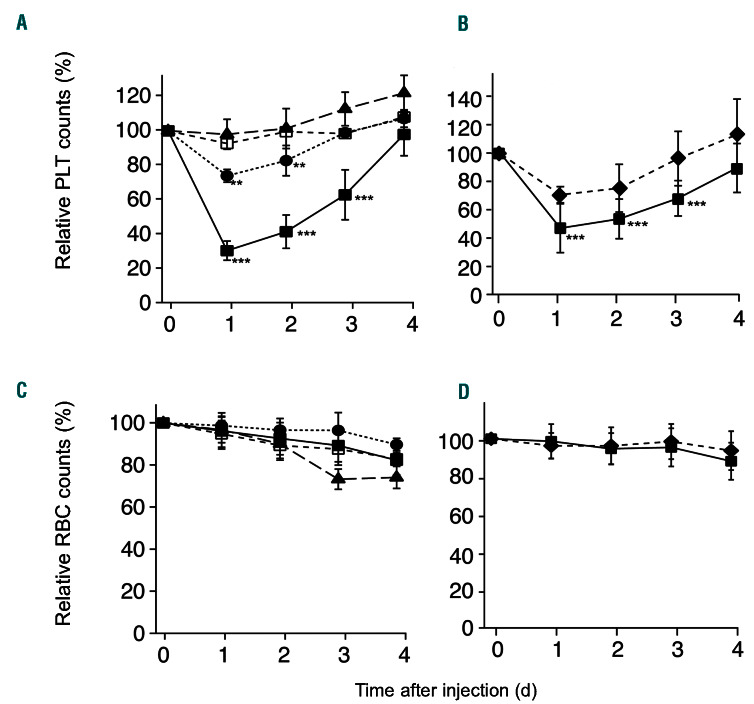
Figure 2.
Efficacy of α2,3- neuraminidase i njection in mediating platelet clearance in mic e. (A, C) α2,3-neuraminidase (0.6 U/g of body weight) was i njected intravenously into wild-type (WT) (), GPIbα-/- (), or IL4RIbαTg (▲) mice. According to the information sheet supplied by the manufacturer, the activity of 1U α2,3-neuraminidase is equivalent of 1 mU A . ur eafaci ens neuraminidase. For comparison, saline was concur rently injected i nto the same strains (corresponding open sym bols). (B, D ) α 2,3-neuram inidase was inje cted intravenously into St3gal1MK-/- (◆) and its littermate WT () mice. Blood wa s colle cted from each mouse via facial vein immediately before (t=0) or days following the injection. Counts of (A,B) platelets and (C,D) erythrocytes were performed on a CBC counter and normal ized wi th the co unt befo re the inje ction being 100% (mean±standard deviation, n=4-7).
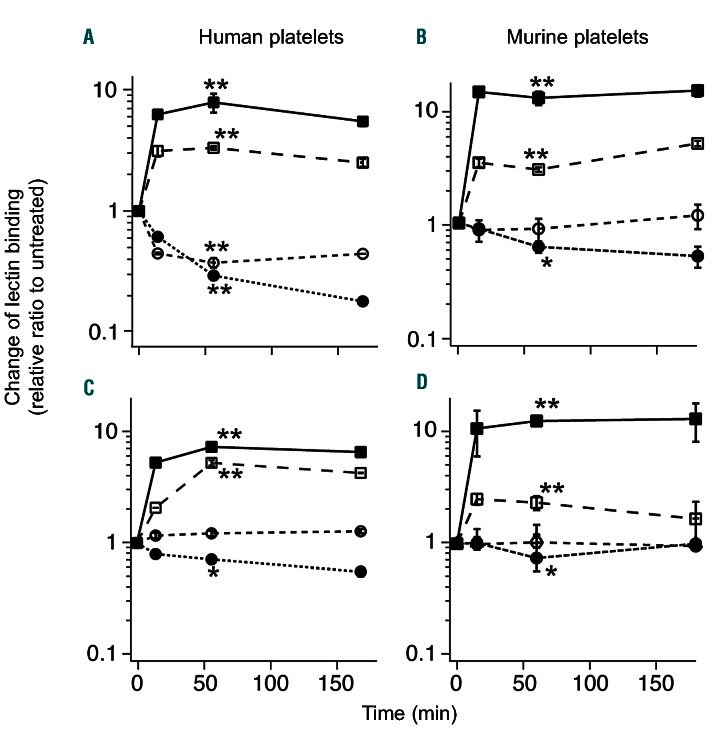
Figure 3.
Changes in lectin bindings to platelets following treatment of α2,3,6,8- or α2,3-neuraminidase in vitro. Citrated (A, C) human or (B, D) wild-type (WT) murine platelets were collected and treated with (A, B) 10 mU/ml α2,3,6,8-neuraminidase or (C, D) α2,3-neuraminidase at the equivalent activity level at 37˚C for 15, 60, and 180 minutes (min) before being analyzed for lectin binding. The glycan content was detected by flow cytometry using Fluorescein isothiocyanate (FITC)- conjugated PNA (), FITCECL (), FITC-SNA() and biotinconjugated MAL-ΙΙ combined with FITC-streptavidin (). The mean fluorescence intensity was quantified for the entire cell population and normalized to untreated sample (0 min). Data are shown as mean ± standard deviation, n=4. Results at 60 min are compared to those of untreated sample by unpaired t-test. *P<0.05; **P<0.01.
In O-glycans, most sialic acids are typically added via an α2,3 linkage by ST3Gal-I.41,42 The GPIbα extracellular domain is heavily decorated with O-glycans.25 To test whether desialylation of O-glycans of GPIbα induces platelet clearance, a recombinant α2,3-neuraminidase was injected into WT, GPIbα-/- and IL4R-IbαTg mice at a dose equivalent to that of the bacterial neuraminidase. Daily blood counts following the injection showed that, compared to the injection of saline, injection of α2,3-neuraminidase significantly decreased platelet counts in wildtype but not IL4R-IbαTg mice (Figure 2A). The extent of decrease in WT was markedly larger than that in GPIbα-/- (Figure 2A). In St3gal1MK-/- mice, lack of ST3Gal-I results in hypo-sialylation of O-glycans in platelets. The extent of platelet count decrease in WT mice induced by α2,3-neuraminidase injection was markedly greater than that in St3gal1MK-/- mice (Figure 2B). For comparison, counts of erythrocytes in all strains were not significantly altered by the injection of α2,3-neuraminidase (Figure 2C and D). Overall, these results indicate that desialylation of O-glycans in GPIbα induces platelet clearance.
T-antigen (Galb1–3GalNAcα1-Ser/Thr) is the most common O-glycan core structure and is synthesized by a single enzyme termed core 1 b3galactosyltransferase.43 The T-antigen is generally masked by further monosaccharide addition, in particular, sialylation. Thus, desialylation of O-glycans in GPIbα may induce presentation of Tantigens on the platelet surface and subsequent platelet opsonization by anti-T-antigen antibodies. To test this possibility, IgG binding was measured following in vitro treatment of α2,3-neuraminidase of citrated human or murine platelet-rich plasma (PRP). Online Supplementary Figure S3 shows that no significant binding of plasma IgG to human or murine platelets was observed following neuraminidase treatment, thus ruling out the possibility that desialylation of O-glycans induces platelet clearance through its opsonization by anti-T-antigen antibodies.
Desialylation induces unfolding of mechanosensory domain of GPIbα in vitro
To further characterize the effects of neuraminidase treatment in vitro, citrated PRP was collected from healthy human donors and WT mice, followed by treatment with bacterial neuraminidase or α2,3-neuraminidase for a time period of up to 3 h. Mice receiving neuraminidase at the equivalent dose (unit per mL of blood) exhibited 50% decrease in platelet count at 2 h, and reached <10% platelet count in 8 h (Online Supplementary Figure S4). Before and after the treatment, platelets were probed by flow cytometry for binding of PNA, ECL, SNA and MALII. At 1-3 h of treatment, both neuraminidases induced significant increases in PNA and ECL binding (Figure 3). Binding of MAL-II, which has high affinity for α2,3-sialic acids, was also significantly reduced, confirming desialylation of O-glycans. However, binding of SNA showed mixed trends, likely reflecting a species difference between human and mouse
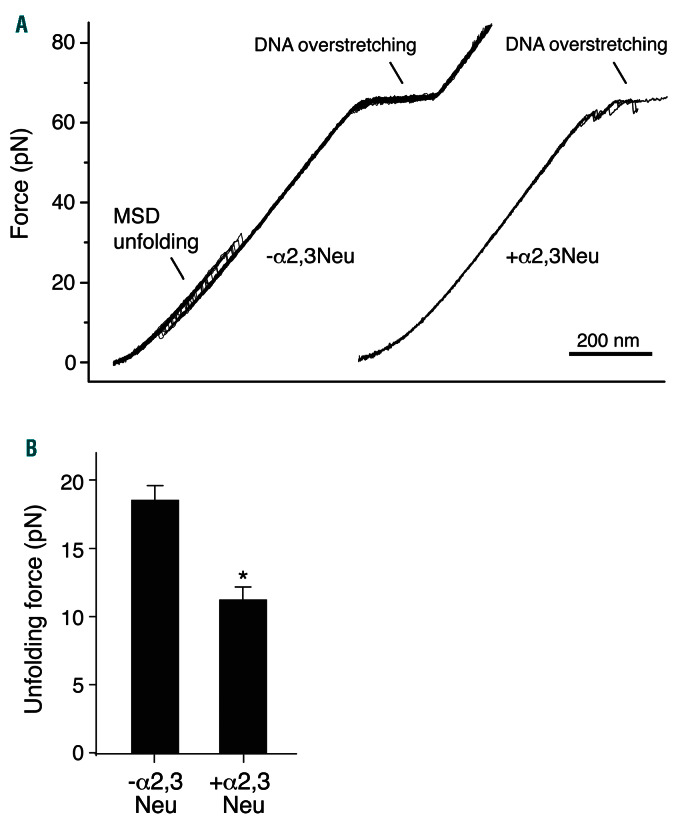
Figure 4.
Desialylation of O-glycans induces unfolding of the mechanosensory domain (MSD) in recombinant GPIb-IX. (A) Overlaid consecutive force-distance traces of pulling MSD under a speed of 200 nm/s without (left) and with (right) prior treatment of α2,3-neuraminidase. (B) Averaged MSD unfolding force without (n=49) or with (n=15) treatment of α2,3-neuraminidase. Error bars are standard error of the mean. *P<0.05 by unpaired t-test.
GPIbα has been implicated in accelerating platelet clearance in several circumstances.44 Several recent reports have linked the step of unfolding of the MSD in GPIbα to the transduction of platelet signaling by GPIb-IX to the induction of platelet clearance.9-11 Located between the sialomucin region and the transmembrane domain of GPIbα, the MSD contains many Ser and Thr residues (Online Supplementary Figure S1). Deletion of approximately 30 residues of MSD reduced the molecular weight of GPIbα by more than 10 kDa,26 indicating that MSD is glycosylated. Recent characterization of a recombinant, unglycosylated form of MSD suggests that it is less stable and more flexible than the native, glycosylated MSD in the GPIb-IX complex.26,27 Thus, we reasoned that desialylation of O-glycans may destabilize the MSD and cause its unfolding.
To directly monitor the effect of desialylation on MSD unfolding, single-molecule force spectroscopy was performed. We first verified that purified GPIb-IX complex could be efficiently desialylated by in vitro treatment of α2,3-neuraminidase (Online Supplementary Figure S5). Next, recombinant biotinylated GPIb-IX was immobilized on a streptavidin bead held by a fixed micropipette, and the Fab fragment of MAb WM23 was coupled to a DNA handle-attached bead that was controlled by an optical laser trap.26 The strong tethered bond between WM23 and its epitope in the sialomucin region of GPIbα enabled multiple cycles of stretching and relaxation without the detachment of WM23 from GPIb-IX.26,27 The event of MSD unfolding was observed in 84% of recorded forceextension pulling traces (Figure 4A). In comparison, after treating the immobilized GPIb–IX beads with α2,3-neuraminidase, MSD unfolding was observed in only 24% of pulling traces, indicating that MSD had become unfolded prior to force pulling as observed previously for GPIb-IX mutants that contain already unfolded MSD.26 In addition, analysis of the force-extension traces that contained the unfolding event revealed a significant decrease of the unfolding force upon neuraminidase treatment (Figure 4B). Since neither GPIbb nor GPIX are significantly O-glycosylated, 45 these results suggest that desialylation of GPIbα O-glycans in the GPIb-IX complex induces MSD unfolding.
Neuraminidase induces mechanosensory domain unfolding and GPIb-IX signaling in platelets
The GPIbα MSD contains the ADAM17 shedding cleavage site therein (Online Supplementary Figure S1). Increased binding of MAb 5G6, which binds the ADAM17 shedding cleavage site in a conformation-insensitive manner,46,47 has been utilized to detect the exposure of this cleavage site in GPIbα, and by extension unfolding of the MSD, on the platelet surface.9-11 Here it was used to probe MSD unfolding on neuraminidase-treated platelets. Since 5G6 recognizes only human but not murine GPIbα,46 transgenic mice expressing only human GPIbα (hTg)28 were used. Injection of neuraminidase induced platelet clearance in hTg mice, although the extent of platelet reduction in hTg mice is less than that in the WT (Online Supplementary Figure S6).
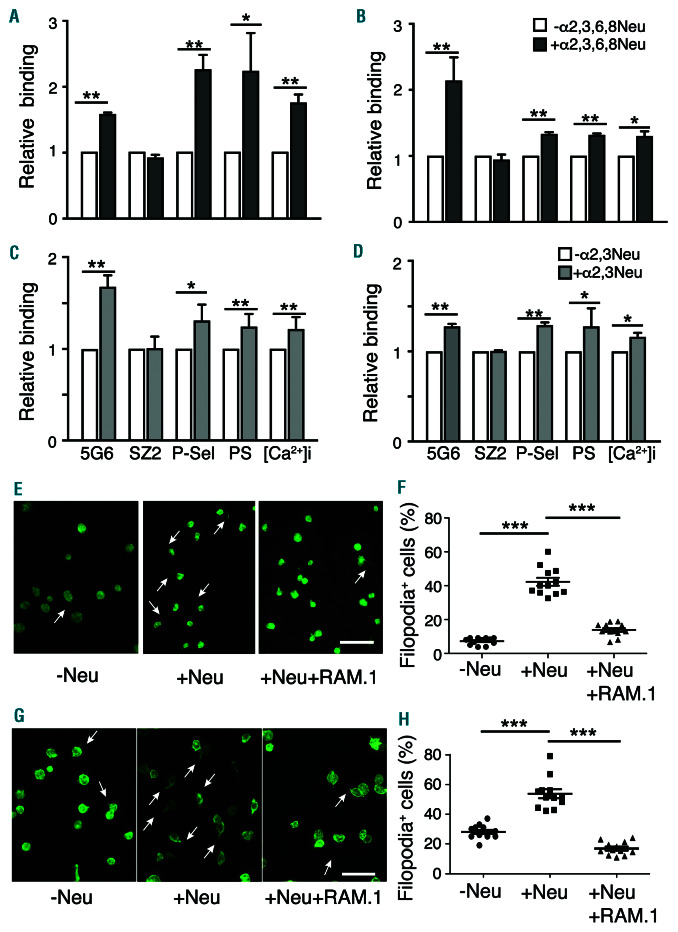
Citrated human and murine hTg platelets were treated with α2,3,6,8- or α2,3-neuraminidase in the presence of EDTA for 30 min at 37°C, after which binding of monoclonal antibodies SZ2 and 5G6 was measured by flow cytometry (Figure 5A-D). Ethylenediamine tetraacetic acid (EDTA) was added to block shedding of GPIbα during desialylation and to keep constant the GPIbα level as shown by the unaltered binding of SZ2. In contrast, binding of 5G6 was significantly increased in platelets treated by either neuraminidase, indicating that the shedding cleavage site in the MSD becomes more accessible,9,10 supporting the notion that the MSD becomes unfolded in both desialylated human and murine platelets. Furthermore, expression of P-selectin and PS lipids on the platelet surface, as well as intracellular calcium influx, all of which are known indicators of GPIb-IX signaling, were significantly increased in platelets after neuraminidase treatment (Figure 5A-D).
Previous studies have demonstrated that GPIb-IX signal-ing induces formation of filopodia in platelets and transfected mammalian cells.10,48-50 To test whether neuraminidase treatment induces GPIb-IX signaling in platelets, fresh human or hTg platelets were collected, treated with neuraminidase as described above, fixed and stained with phalloidin. Microscopic images of platelets before and after treatment revealed that approximately 40% of desialylated platelets but <10% of sialylated ones exhibited filopodia (Figure 5E and F). The increased filopodia formation was inhibited by anti-GPIbb antibody RAM.110,49 (Figure 5E and F), confirming the role of GPIb-IX in mediating filopodia formation in desialylated platelets. Consistently, St3gal1MK-/- platelets, with hyposialylated O-glycans, display more filopodia than their littermate WT ones (Online Supplementary Figure S7). Overall, these results demonstrate that desialylation induces MSD unfolding and GPIb-IX signaling in both human and murine platelets.
Figure 5.
Desialylation induces unfolding of the mechanosensory domain (MSD) and GPIb-IX signaling in platelets. Citrated washed (A,C) hTg or (B,D) human platelets (1x106 cells, with 2mM EDTA) were treated with or without α2,3,6,8-neuraminidase or α2,3-neuraminidase at 37˚C for 30 minutes (min). Monoclonal anti-GPIbα antibodies 5G6 and SZ2, anti-P-selectin antibody, GFP-LactC2, or Fura-2 were then added for 30 min, and the samples were fixed and analyzed by flow cytometry. The mean fluorescence intensity (MFI) was measured for each cell population and normalized against that of untreated platelets (mean±standard deviation [SD], n=4). *P<0.05; **P<0.01 by unpaired t-test. (E-H) Confocal fluorescence images of washed (E) hTg and (G) human platelets that had been treated with PBS buffer (-Neu), α2,3,6,8-neuraminidase (+Neu), or neuraminidase plus 1.5 mg/mL anti- GPIbb antibody RAM.1 (+Neu+RAM.1). White arrowheads mark some filopodia in platelets. Scale bar, 10 μm. (F, H) Quantification of filopodia in (F) hTg and (H) human platelets (mean±SD, n=11-12). Images of filopodia from 11-12 view fields (~80-110 platelets per view field) in two independent experiments were visually examined, and counted for comparison.10 **P<0.01; ***P<0.001 by unpaired Student’s t-test.
Discussion
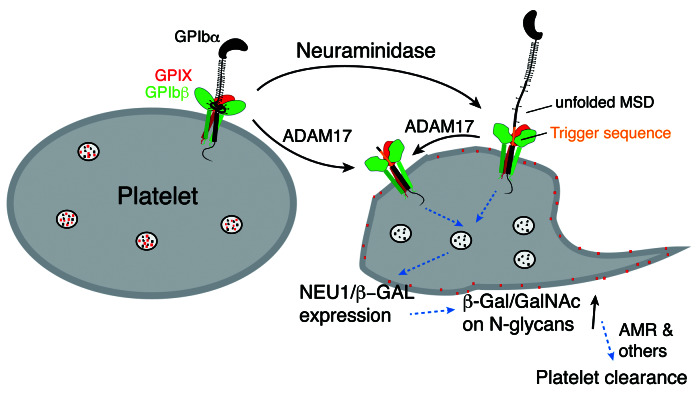
This study provides a new molecular mechanism of neuraminidase-induced platelet clearance. Earlier studies have identified GPIbα as critical in facilitating clearance of desialylated mouse platelets.3,5 It was suggested that the N-glycans on the LBD of GPIbα are critically involved.13 However, mouse GPIbα does not contain any N-glycosylation sites (Online Supplementary Figure S1). Utilizing genetically modified mice, we report here that GPIbα, but neither VWF nor ADAM17, is required for the efficient clearance of desialylated platelets (Figure 1 and Online Supplementary Figure S2). Following injection of neuraminidase, only the extent of O-glycan desialylation is inversely correlated with the platelet count in mice (Figure 1), leading to the additional discovery that specific desialylation of O-glycans in GPIbα induces platelet clearance (Figure 2). At the molecular level, desialylation of O-glycans in GPIbα significantly lowers the force threshold to unfold the MSD in GPIb-IX and exposes the shedding cleavage site therein (Figures 4 and 5). Moreover, desialylation of O-glycans activates GPIb-IX signaling in both human and murine platelets (Figure 5 and Online Supplementary Figure S5). Overall, these results suggest that desialylation of O-glycans, instead of N-glycans, in GPIbα induces MSD unfolding and GPIb-IX signaling, and subsequently platelet clearance. Understanding the mechanism of neuraminidase-mediated platelet clearance and the roles of involved factors (Figure 6) in the process may help design and develop effective therapeutics to treat related thrombocytopenic conditions.
It has been reported previously that binding of VWF or most anti-LBD antibodies causes unfolding of the MSD, which activates GPIb-IX and induces platelet signaling.9-11 GPIb-IX signaling induced by anti-LBD antibodies results in surface presentation of Neu1 and desialylation of the platelet.7 Consistently, GPIb-IX signaling induced by VWF binding also leads to desialylation of the platelet.10,11 Therefore, we postulate that desialylation of GPIbα Oglycans induces GPIb-IX signaling and leads to surface expression of Neu1. Since Neu1 can remove sialic acids from both N- and O-glycans,51 it should induce exposure of b-galactose on N-glycans of platelet glycoproteins other than GPIbα, which may be recognized by AMR and possibly other receptors (Figure 6). In this model, desialylation of GPIbα O-glycans results in amplified desialylation of N-glycans of other glycoproteins, which reconciles the requirement of GPIbα for rapid platelet clearance after neuraminidase treatment, the preferred recognition of galactoses on N-glycans by AMR, and the lack of N-glycans in mouse GPIbα. The involvement of Neu1 or other lysosomal neuraminidases in this process should be verified by further studies in the future.
In this study, we show for the first time that desialylation of GPIbα O-glycans destabilizes MSD and increases exposure of the ADAM17 shedding cleavage site therein, which explains an earlier observation that neuraminidase treatment induces ADAM17-mediated shedding of GPIbα.6,52 Shedding of GPIbα has been linked to accelerated platelet clearance.34-36 However, ADAM17, and by extension shedding of GPIbα, is not required for the neuraminidase- induced platelet clearance6 (Online Supplementary Figure S2). The reason for this has not been reported. Our results suggest that desialylation of GPIbα O-glycans induces MSD unfolding, the exposure of the juxtamembrane Trigger sequence therein, and consequently GPIb-IX signaling across the membrane (Figure 6). Since the ADAM17 shedding cleavage site32 is located Nterminal to the Trigger sequence (Online Supplementary Figure S1), shedding of GPIbα would also lead to the exposure of the Trigger sequence and induce platelet clearance. Although inactive ADAM17 may prevent shedding of GPIbα, it should not block desialylation of GPIbα, MSD unfolding and the subsequent exposure of the Trigger sequence. Upon MSD unfolding, sequences in the MSD in addition to the ADAM17 shedding cleavage site may also become more exposed and prone to more proteolysis. Consistent with this notion, GPIbα is fragmented and its expression significantly reduced in murine platelets that lack the Cosmc protein, functional T-synthase and intact core 1 O-glycans.53 In other words, proper sialylation of Oglycans may protect platelets from clearance54 by stabilizing GPIbα.
Figure 6.
A model for the desialylation-mediated GPIb-IX signaling and platelet clearance. In this model, exogenous neuraminidase removes sialic acids from O-glycans in GPIbα, thereby inducing unfolding of the mechanosensory (MSD), exposure of the Trigger sequence therein, GPIb-IX signaling into the platelet, surface expression of Neu1, and exposure of b-galactoses (b-Gal) on N-glycans of many glycoproteins, which are recognized by the Ashwell-Morell receptor and other receptors for clearance. Unfolding of the MSD also increases the accessibility of the ADAM17 shedding cleavage site in the MSD, facilitates shedding of GPIbα, which results in the exposure of the Trigger sequence.
GPIbα-/- and IL4R-IbαTg mice respond differently to neuraminidase injection. Due to the defect in thrombopoiesis, GPIbα-/- mice are severely thrombocytopenic, with less than 10% of the normal platelet count.28,55 Nevertheless, injection of α2,3,6,8-neuraminidase caused a significant reduction in platelet count in GPIbα-/- mice, suggesting that it can desialylate N-glycans on glycoproteins other than GPIbα that are subsequently recognized by AMR.3 In comparison, due to accelerated platelet clearance, IL4R-IbαTg mice are mildly thrombocytopenic, with about 50% of the normal platelet count.10,29 Injection of either α2,3,6,8- or α2,3-neuraminidase did not cause significant reduction of platelet count in IL4R-IbαTg mice (Figures 1 and 2). In the IL4RIbαTg platelet, the Trigger sequence in GPIb is exposed due to the removal of GPIbα extracellular residues including the rest of MSD, leading to constitutive GPIb-IX signaling that includes elevated P-selectin expression and significant filopodia formation.10 Considering that desialylation of GPIbα leads to unfolding of MSD and thus the same kind of GPIb-IX signaling (Figures 4 and 5), it is conceivable that neuraminidase cannot cause further GPIb-IX signaling in the IL4R-IbαTg platelet, and thus further reduction of the platelet count in IL4R-IbαTg mice. This is a critical observation, as no mechanisms other than the one described in this paper have been postulated to account for the accelerated clearance rate of IL4R-IbαTg platelets as well as the inability of neuraminidase to reduce platelet count in IL4R-IbαTg mice.
Supplementary Material
Acknowledgments
We thank the Emory Children's Pediatric Research Center Flow Cytometry Core and Emory Integrated Cellular Imaging Core for technical support.
Funding Statement
Funding: This work was supported in part by NIH grants HL082808, HL123984 (RL, XFZ) and HL144976 (WB).
References
- 1.Gasic GJ, Gasic TB, Stewart CC. Antimetastatic effects associated with platelet reduction. Proc Natl Acad Sci U S A. 1968;61(1):46-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi SI, Simone JV, Jorney LJ. Neuraminidase-induced thrombocytopenia in rats. Br J Haematol. 1972;22(1):93-101. [DOI] [PubMed] [Google Scholar]
- 3.Grewal PK, Aziz PV, Uchiyama S, et al. Inducing host protection in pneumococcal sepsis by preactivation of the Ashwell- Morell receptor. Proc Natl Acad Sci U S A. 2013;110(50):20218-20223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xiang B, Zhang G, Guo L, et al. Platelets protect from septic shock by inhibiting macrophage-dependent inflammation via the cyclooxygenase 1 signalling pathway. Nat Commun. 2013;4:2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rumjantseva V, Grewal PK, Wandall HH, et al. Dual roles for hepatic lectin receptors in the clearance of chilled platelets. Nat Med. 2009;15(11):1273-1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jansen AJ, Josefsson EC, Rumjantseva V, et al. Desialylation accelerates platelet clearance after refrigeration and initiates GPIbα metalloproteinase-mediated cleavage in mice. Blood. 2012;119(5):1263-1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li J, van der Wal DE, Zhu G, et al. Desialylation is a mechanism of Fc-independent platelet clearance and a therapeutic target in immune thrombocytopenia. Nat Commun. 2015;6:7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan R, Chen M, Ma N, et al. Glycoprotein Ibα clustering induces macrophage-mediated platelet clearance in the liver. Thromb Haemost. 2015;113(1):107-117. [DOI] [PubMed] [Google Scholar]
- 9.Quach ME, Dragovich MA, Chen W, et al. Fc-independent immune thrombocytopenia via mechanomolecular signaling in platelets. Blood. 2018;131(7):787-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deng W, Xu Y, Chen W, et al. Platelet clearance via shear-induced unfolding of a membrane mechanoreceptor. Nat Commun. 2016;7:12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen W, Druzak SA, Wang Y, et al. Refrigeration-induced binding of von Willebrand factor facilitates fast clearance of refrigerated platelets. Arterioscler Thromb Vasc Biol. 2017;37(12):2271-2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riswari SF, Tunjungputri RN, Kullaya V, et al. Desialylation of platelets induced by Von Willebrand Factor is a novel mechanism of platelet clearance in dengue. PLoS Pathog. 2019;15(3):e1007500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grewal PK, Uchiyama S, Ditto D, et al. The Ashwell receptor mitigates the lethal coagulopathy of sepsis. Nat Med. 2008;14(6):648-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellies LG, Ditto D, Levy GG, et al. Sialyltransferase ST3Gal-IV operates as a dominant modifier of hemostasis by concealing asialoglycoprotein receptor ligands. Proc Natl Acad Sci U S A. 2002; 99(15):10042-10047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorensen AL, Rumjantseva V, Nayeb-Hashemi S, et al. Role of sialic acid for platelet life span: exposure of β-galactose results in the rapid clearance of platelets from the circulation by asialoglycoprotein receptor-expressing liver macrophages and hepatocytes. Blood. 2009;114(8):1645-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ashwell G, Harford J. Carbohydrate-specific receptors of the liver. Annu Rev Biochem. 1982;51:531-554. [DOI] [PubMed] [Google Scholar]
- 17.Grewal PK. The Ashwell-Morell receptor. Methods Enzymol. 2010;479:223-241. [DOI] [PubMed] [Google Scholar]
- 18.Park EI, Mi Y, Unverzagt C, Gabius HJ, Baenziger JU. The asialoglycoprotein receptor clears glycoconjugates terminating with sialic acid alpha 2,6GalNAc. Proc Natl Acad Sci U S A. 2005;102(47):17125-17129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lodish HF. Recognition of complex oligosaccharides by the multi-subunit asialoglycoprotein receptor. Trends Biochem Sci. 1991; 16(10):374-377. [DOI] [PubMed] [Google Scholar]
- 20.Spiess M. The asialoglycoprotein receptor: a model for endocytic transport receptors. Biochemistry. 1990;29(43):10009-10018. [DOI] [PubMed] [Google Scholar]
- 21.Lopez JA, Chung DW, Fujikawa K, Hagen FS, Papayannopoulou T, Roth GJ. Cloning of the α chain of human platelet glycoprotein Ib: a transmembrane protein with homology to leucine-rich α2-glycoprotein. Proc Natl Acad Sci U S A. 1987;84(16):5615-5619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Titani K, Takio K, Handa M, Ruggeri ZM. Amino acid sequence of the von Willebrand factor-binding domain of platelet membrane glycoprotein Ib. Proc Natl Acad Sci U S A. 1987;84(16):5610-5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewandrowski U, Moebius J, Walter U, Sickmann A. Elucidation of N-glycosylation sites on human platelet proteins: a glycoproteomic approach. Mol Cell Proteomics. 2006;5(2):226-233. [DOI] [PubMed] [Google Scholar]
- 24.Chen W, Voos KM, Josephson CD, Li R. Short-acting anti-VWF (von Willebrand Factor) aptamer improves the recovery, survival, and hemostatic functions of refrigerated platelets. Arterioscler Thromb Vasc Biol. 2019;39(10):2028-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li R, Emsley J. The organizing principle of the platelet glycoprotein Ib-IX-V complex. J Thromb Haemost. 2013;11(4):605-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang W, Deng W, Zhou L, et al. Identification of a juxtamembrane mechanosensitive domain in the platelet mechanosensor glycoprotein Ib-IX complex. Blood. 2015;125(3):562-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang XF, Zhang W, Quach ME, Deng W, Li R. Force-regulated refolding of the mechanosensory domain in the platelet glycoprotein Ib-IX complex. Biophys J. 2019; 116(10):1960-1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ware J, Russell S, Ruggeri ZM. Generation and rescue of a murine model of platelet dysfunction: the Bernard-Soulier syndrome. Proc Natl Acad Sci U S A. 2000;97(6):2803-2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kanaji T, Russell S, Ware J. Amelioration of the macrothrombocytopenia associated with the murine Bernard-Soulier syndrome. Blood. 2002;100(6):2102-2107. [DOI] [PubMed] [Google Scholar]
- 30.Stefanini L, Paul DS, Robledo RF, et al. RASA3 is a critical inhibitor of RAP1-dependent platelet activation. J Clin Invest. 2015; 125(4):1419-1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Marco L, Girolami A, Russell S, Ruggeri ZM. Interaction of asialo von Willebrand factor with glycoprotein Ib induces fibrinogen binding to the glycoprotein IIb/IIIa complex and mediates platelet aggregation. J Clin Invest. 1985;75(4):1198-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardiner EE, Karunakaran D, Shen Y, Arthur JF, Andrews RK, Berndt MC. Controlled shedding of platelet glycoprotein (GP)VI and GPIb-IX-V by ADAM family metalloproteinases. J Thromb Haemost. 2007; 5(7):1530-1537. [DOI] [PubMed] [Google Scholar]
- 33.Bergmeier W, Piffath CL, Cheng G, et al. Tumor necrosis factor-α-converting enzyme (ADAM17) mediates GPIbα shedding from platelets in vitro and in vivo. Circ Res. 2004; 95(7):677-683. [DOI] [PubMed] [Google Scholar]
- 34.Bergmeier W, Burger PC, Piffath CL, et al. Metalloproteinase inhibitors improve the recovery and hemostatic function of in vitro-aged or -injured mouse platelets. Blood. 2003;102(12):4229-4235. [DOI] [PubMed] [Google Scholar]
- 35.Canault M, Duerschmied D, Brill A, et al. p38 mitogen-activated protein kinase activation during platelet storage: consequences for platelet recovery and hemostatic function in vivo. Blood. 2010;115(9):1835-1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen W, Liang X, Syed AK, et al. Inhibiting GPIbα shedding preserves post-transfusion recovery and hemostatic function of platelets after prolonged storage. Arterioscler Thromb Vasc Biol. 2016; 36(9):1821-1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Debray H, Montreuil J, Lis H, Sharon N. Affinity of four immobilized Erythrina lectins toward various N-linked glycopeptides and related oligosaccharides. Carbohydr Res. 1986;151:359-370. [DOI] [PubMed] [Google Scholar]
- 38.Iglesias JL, Lis H, Sharon N. Purification and properties of a D-galactose/N-acetyl-Dgalactosamine- specific lectin from Erythrina cristagalli. Eur J Biochem. 1982;123(2):247-252. [DOI] [PubMed] [Google Scholar]
- 39.Novogrodsky A, Lotan R, Ravid A, Sharon N. Peanut agglutinin, a new mitogen that binds to galactosyl sites exposed after neuraminidase treatment. J Immunol. 1975; 115(5):1243-1248. [PubMed] [Google Scholar]
- 40.Shibuya N, Goldstein IJ, Broekaert WF, Nsimba-Lubaki M, Peeters B, Peumans WJ. The elderberry (Sambucus nigra L.) bark lectin recognizes the Neu5Ac(alpha 2-6)Gal/GalNAc sequence. J Biol Chem. 1987; 262(4):1596-1601. [PubMed] [Google Scholar]
- 41.Reboul P, George P, Geoffroy J, Louisot P, Broquet P. Study of O-glycan sialylation in C6 cultured glioma cells: regulation of a betagalactoside alpha 2,3 sialyltransferase activity by Ca2+/calmodulin antagonists and phosphatase inhibitors. Biochem Biophys Res Commun. 1992;186(3):1575-1581. [DOI] [PubMed] [Google Scholar]
- 42.Dall'Olio F, Malagolini N, Trinchera M, Chiricolo M. Mechanisms of cancer-associated glycosylation changes. Front Biosci (Landmark Ed). 2012;17:670-699. [DOI] [PubMed] [Google Scholar]
- 43.Ju T, Brewer K, D'Souza A, Cummings RD, Canfield WM. Cloning and expression of human core 1 beta1,3-galactosyltransferase. J Biol Chem. 2002;277(1):178-186. [DOI] [PubMed] [Google Scholar]
- 44.Quach ME, Chen W, Li R. Mechanisms of platelet clearance and translation to improve platelet storage. Blood. 2018;131(14):1512-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.King SL, Joshi HJ, Schjoldager KT, et al. Characterizing the O-glycosylation landscape of human plasma, platelets, and endothelial cells. Blood Adv. 2017;1(7):429-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liang X, Russell SR, Estelle S, et al. Specific inhibition of ectodomain shedding of glycoprotein Ibα by targeting its juxtamembrane shedding cleavage site. J Thromb Haemost. 2013;z11(12):2155-2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tao Y, Zhang X, Liang X, Zang J, Mo X, Li R. Structural basis for the specific inhibition of glycoprotein Ibα shedding by an inhibitory antibody. Sci Rep. 2016;6:24789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yuan Y, Kulkarni S, Ulsemer P, et al. The von Willebrand factor-glycoprotein Ib/V/IX interaction induces actin polymerization and cytoskeletal reorganization in rolling platelets and glycoprotein Ib/V/IX-transfected cells. J Biol Chem. 1999;274(51):36241-36251. [DOI] [PubMed] [Google Scholar]
- 49.Maurer E, Tang C, Schaff M, et al. Targeting platelet GPIbb reduces platelet adhesion, GPIb signaling and thrombin generation and prevents arterial thrombosis. Arterioscler Thromb Vasc Biol. 2013;33(6):1221-1229. [DOI] [PubMed] [Google Scholar]
- 50.McCarty OJ, Calaminus SD, Berndt MC, Machesky LM, Watson SP. von Willebrand factor mediates platelet spreading through glycoprotein Ib and alpha(IIb)beta3 in the presence of botrocetin and ristocetin, respectively. J Thromb Haemost. 2006;4(6):1367-1378. [DOI] [PubMed] [Google Scholar]
- 51.Pshezhetsky AV, Richard C, Michaud L, et al. Cloning, expression and chromosomal mapping of human lysosomal sialidase and characterization of mutations in sialidosis. Nat Genet. 1997;15(3):316-320. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.