Abstract
Background
Hepatitis B (HBV) remains a significant public health risk with an estimated 240-350 million people chronically-infected with HBV worldwide. In the US, rates of new HBV infections are highest among individuals aged 30-39 years, highlighting the elevated risk in adults. Moreover, CDC reported that in 2017 only 34.3% of US adults aged 19-49 years were vaccinated against HBV. Younger adults who are at-risk of HBV infection, through exposure in the workplace or home (e.g. healthcare workers, public service sector workers, those living with HBsAb-positive individuals), through travel to countries with high HBV prevalence, or through exposure as a result of high-risk behavior (e.g. injection drug use, risk through sexual transmission), need a highly effective and safe HBV vaccine with a rapid onset of seroprotection.
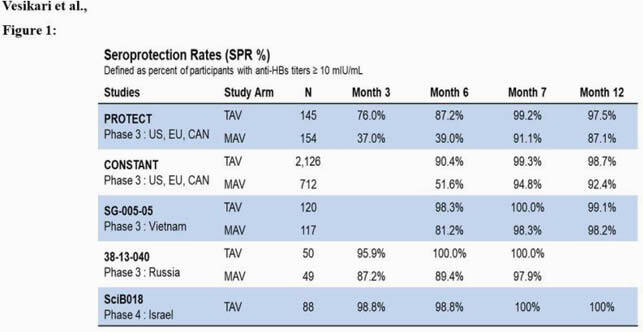
Seroprotection Rates from Phase 3 Studies
Methods
Four phase 3 studies assessing kinetics of seroprotection rates (SPR; anti-HBs ≥ 10 mIU/mL) in adults aged 18-45 years, vaccinated at months 0, 1 and 6 with 10 µg of tri-antigenic HBV vaccine (TAV) vs. 20 µg of a mono-antigenic HBV vaccine (MAV) were completed between 2008 & 2020: (1) PROTECT study in US, Europe, and Canada, n = 299; (2) CONSTANT study in US, Europe and Canada, n = 2,838; (3) SG-005-05 study in Vietnam, n = 349; (4) 38-13-040 study in Russia, n = 99. One phase 4, single-arm study was conducted with 10 µg of TAV in adults aged 20-40 years: SciB018 study in Israel, n = 83.
Results
In all five studies, vaccination with TAV achieved SPRs of 87.2-100.0% at month 6 after 2 doses and 99.2-100.0% at month 7 after 3 doses, compared to 39.0-89.4% and 91.1-98.3% achieved with MAV at months 6 and 7, respectively (Fig 1). Moreover, as demonstrated with the data available from two of the controlled studies, TAV induced SPRs of 76.0%-95.9% at month 3 after 2 doses compared to 37.2%-87.2% with MAV. No major safety signals were observed, and adverse events were well-balanced and consistent with the known vaccine safety profiles.
Conclusion
Tri-antigenic HBV vaccine (TAV) has demonstrated its ability to rapidly, consistently, and safely elicit high SPRs in younger adults across different regions of the world.
Disclosures
Joanne M. Langley, MD, GSK group of companies (Research Grant or Support)Immunivaccines Inc (Scientific Research Study Investigator, Research Grant or Support)Janssen (Research Grant or Support)Pfizer (Research Grant or Support)Symvivo (Scientific Research Study Investigator, Research Grant or Support)VBI Vaccines (Research Grant or Support) Nathalie Machluf, PhD, VBI Vaccines Inc. (Employee) Johanna Spaans, BSc, MSc, VBI Vaccines Inc (Employee) Dave Anderson, PhD, VBI Vaccines (Employee, Shareholder) Vlad Popovic, MD, VBI Vaccines, Inc. (Employee, Shareholder) Francisco Diaz-Mitoma, MD, VBI Vaccines, Inc. (Shareholder, Independent Contractor)


