Abstract
Background
Percutaneous coronary intervention (PCI) is an effective treatment for coronary heart disease. However, a lack of cardiac rehabilitation and continuous nursing management leads to repeated patient hospitalizations. Long-term systematic rehabilitation and nursing management after discharge are key to ensuring quality of treatment and patient quality of life. This study aimed to explore the application of the WeChat platform in continuous nursing after PCI.
Material/Methods
This was a retrospective case-control study. The clinical data of 63 patients in our cardiac center who underwent PCI between June 2017 and January 2018 were recorded. Patients were divided into 2 groups: the continuous nursing through the WeChat platform (intervention) group and the conventional nursing (control) group. The Self-Rating Depression Scale (SDS), Self-Rating Anxiety Scale (SAS), and Seattle Angina Questionnaire (SAQ) were used as the evaluation tools.
Results
The SAQ scores in all 5 SAQ dimensions in the continuous nursing group were significantly higher than those of the control group at the 1-year follow-up. Scores on the SAS and SDS scales at 1-year follow-up were significantly better in the intervention group than in the control group. The SAS and SDS scores in both groups were better at the 1-year follow-up, but the difference was statistically significant in the continuous nursing group and not in the control group.
Conclusions
Using the WeChat platform can make continuous nursing more convenient and effective for patients after PCI. It may reduce the occurrence of complications, relieve patient depression and anxiety, and improve patient quality of life.
MeSH Keywords: Home Care Services, Nursing Audit, Percutaneous Coronary Intervention
Background
Percutaneous coronary intervention (PCI) is an effective treatment for coronary heart disease because it can quickly open occluded coronary vessels and relieve symptoms [1–3]. However, the risk factors that can induce atherosclerosis are not eliminated by PCI. There is a risk of reoccurrence after operation; thus, long-term lipid-regulating drugs, β-receptor blockers, and antiplatelet aggregation drugs are still needed after hospital discharge [4,5]. There are many patients with coronary heart disease living in rural areas in China. Because of low education levels, lack of related knowledge, and poor self-management after discharge, patient compliance after discharge is far below the compliance level during hospitalization. As the time since discharge increases, patients gradually forget doctor’s orders, resulting in their increased risk of coronary artery restenosis and myocardial infarction [6–8]. A lack of cardiac rehabilitation management and continuous nursing management leads to repeated hospitalization and reoperation [9–11]. Therefore, long-term systematic rehabilitation and nursing management after discharge are vital to ensuring the quality of treatment and patient quality of life.
For patients discharged from the hospital after undergoing PCI, the conventional nursing model has little effect on improving the patient medical management level and quality of life during the follow-up period. As a new nursing model, continuous nursing extends in-hospital treatment and rehabilitation care to post-discharge care to improve patients’ self-management and ensure that treatment, information, and nursing continue, which could effectively solve the problem of inadequate post-discharge nursing [12,13]. Continuous nursing has been widely used in managing patients with chronic diseases and has achieved good clinical results [14,15]. In the past, continuous nursing mainly took the form of telephone follow-up, outpatient follow-up, and family visits, but each of these forms had some limitations [16].
With the progress in technology and the popularization of smartphones, WeChat has become the most popular social media and messaging application in China; it is low-cost, fast, and facilitates face-to-face communication. It has become the primary means for people to access and exchange information, and medical and health care services can currently be provided through WeChat [17]. Health educators who use the WeChat platform provide a new way to deliver continuous nursing to patients, and WeChat has been shown to have excellent application value for continuing nursing service after hospital discharge [18]. This study examined how to carry out continuous nursing via the WeChat platform for patients who underwent PCI.
Material and Methods
Ethical approval
This study was approved by the Ethics Committee of the Union Hospital, Fujian Medical University (No. 2013-002). All patients signed a written informed consent form, which stated their anonymity would be preserved, before participating in the study.
Study design
This was a retrospective case-control study. Based on the incidence of post-discharge complications (chest pain, chest tightness, and coronary restenosis) reported in the pre-survey, with alpha=0.05 and power (1-β)=0.85, the sample size of each group was 34. Three patients in the intervention group were lost to follow-up and 2 patients in the control group were lost to follow-up. The actual sample sizes used in the analysis were 31 patients in the intervention group and 32 patients in the control group.
We retrospectively analyzed the clinical data of the 63 patients who underwent PCI from June 2017 to January 2018 at our hospital, a provincial hospital and one of the largest heart centers in southeast China. Most of the patients with coronary heart disease came to our center from rural areas. For inclusion in the study, patients must have undergone PCI and had no other primary organ disease. The exclusion criteria were 1) lack of independent judgment and reading skills; 2) lack of communication devices or difficultly with communication; 3) death after the operation; 4) severe cardiac insufficiency, other structural heart diseases, or other organ dysfunction; and 5) refusal to participate in the study. The 63 eligible patients were placed into the conventional nursing group (the control group, n=32) or the continuous nursing group (the intervention group, n=31) (Figure 1). For inclusion in the continuous nursing group, patients needed to have a smartphone and proficiency in using the WeChat platform, and they agreed to use the WeChat platform for continuous nursing. Patients who were unwilling to accept the WeChat approach and chose to receive conventional nursing were included in the control group.
Figure 1.
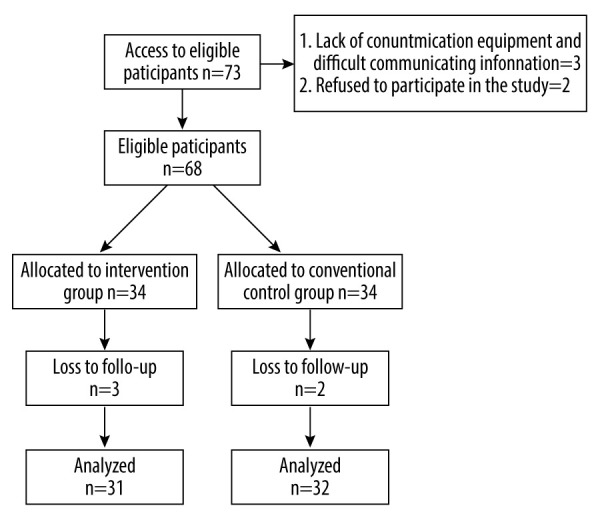
CONSORT diagram of patient participation.
Conventional nursing (control group)
Nurses in the conventional nursing (control) group provided routine medical care to the patients during their hospital stay. The doctor explained the disease and the PCI procedure to the patients and their families. The nurses introduced diet, preoperative preparation, postoperative care, self-rescue methods, assistance with needs after discharge, and regular visitation to patients and their families. This process was defined as conventional nursing.
Continuing nursing (intervention group)
Patients received conventional nursing care during their hospitalization. The patients were given contact cards which included the smartphone number and WeChat account of the attending physician. The contact cards were used to provide continuous nursing at discharge, which was based on the conventional nursing care model. Patients were enrolled in the intervention group after undergoing PCI, and the nurse instructed patients to use the WeChat function correctly and carefully.
WeChat health education content included 3 parts: rehabilitation, personal health, and WeChat support. First, the rehabilitation component included information on postoperative diet, exercise, medication, daily behavior observations, postoperative psychological guidance, and other aspects related of rehabilitation. This part also provided health information about heart disease, family first aid, self-rescue methods, exercise, smoking cessation, and limiting alcohol intake. Patients were able to learn independently at home. Second, the personal component featured the patient’s main health files and contained various information, such as daily eating habits, sleeping habits, exercise, psychological status, degree of recovery, and medication reminders. Third, WeChat support was available with a person from our team who was online from 6: 00 to 9: 00 PM each night to answer patients’ questions and solve problems. We reminded the patients to take their medications on time and encouraged them to share their nursing experiences with family. Guidance, comfort, explanation, encouragement, and other supportive methods were used to actively guide patients with anxiety and depression to discuss their physical pain and mental pressure and participate in psychological counseling and support.
Outcomes
All patients participating in the study were followed for 1 year after undergoing PCI. Three measurement scales were used at the different study timepoints. The Self-Rating Depression Scale (SDS) and Self-Rating Anxiety Scale (SAS) were completed by all patients at hospital admission and 1-year follow-up. The Seattle Angina Questionnaire (SAQ) was completed by all patients at hospital discharge and 1-year follow-up. A specialized psychologist was available to provide consultation and treatment for patients with high SAS and SDS scores.
Measuring dimensions of coronary artery disease with the SAQ
The SAQ is a 19-item self-administered questionnaire that measure 5 dimensions of coronary artery disease: angina frequency, angina stability, degree of physical limitation, cognitive perception of the disease, and satisfaction with treatment. A score from 1 to 100 is calculated for each of the 5 dimensions, and higher scores indicate a better quality of life [19].
Measuring depression with the SDS
The Zung SDS is a standardized depression scale, which has high reliability and validity in evaluating depression. It is usually applied in a clinic setting. This scale contains 10 positive and 10 negative items. Each item is scored on a 4-point Likert scale. The responses for items with negative symptoms are presented in ascending order, based on the symptom’s frequency of occurrence: (1, no or very little time; 2, a small amount of time; 3, a considerable amount of time; 4, most or all of the time); while the responses for items with positive symptoms are presented in descending order: (4, no or very little time; 3, a small amount of time; 2, a considerable amount of time; 1, most or all of the time). The scores of the individual items are added to obtain the total score, which is used to calculate the standard score. A score of <50 indicates normal, 50 to 59 indicates mild depression, 60 to 69 indicates medium depression, and ≥70 indicates severe depression [20].
Measuring anxiety with the SAS
The Zung SAS is a standardized scale with high reliability and validity in evaluating anxiety. It is also generally used in a clinic setting. Fifteen items with negative statements are scored, with the same 4-point Likert scoring scale used in the SDS. The total score is the sum of the scores of all the items. The score is used to calculate the standard score. A score of <50 indicates normal, 50 to 59 indicates mild anxiety, 60 to 69 indicates moderate anxiety, and ≥70 indicates severe anxiety [21].
Data analysis
We retrospectively collected and reviewed patients’ medical records and questionnaire data. SPSS version 18.0 was used for analysis. Continuous data were shown to have a normal distribution, and our data were analyzed using the t test. The chi-square test and Fisher’s test were used for comparing qualitative data. The P value of <0.05 was considered as statistically significant.
Results
There were no statistically significant differences between the intervention and control groups in baseline demographic and clinical data (Table 1). There were 34 patients in the intervention and control group at baseline, and 31 and 32 patients in the groups at the 1-year follow-up, respectively. There were no statistically significant differences in the total scores of the SDS and SAS at hospital admission between the 2 groups (Table 2). These results indicate that the 2 groups were comparable and homogeneous at baseline.
Table 1.
Comparison of baseline clinical and demographic data between the 2 groups.
| Item | Intervention group | Control group | P value |
|---|---|---|---|
| n | 31 | 32 | |
| Age (year) | 55.7±9.6 | 57.5±10.8 | 0.716 |
| Male/Female | 21/10 | 23/9 | 0.721 |
| Hypertension | 13 | 15 | 0.693 |
| Diabetes mellitus | 10 | 12 | 0.663 |
| Hyperlipemia | 6 | 6 | 0.951 |
| Smoking | 8 | 10 | 0.845 |
| Record of formal schooling | |||
| Junior high school and below | 24 | 26 | 0.916 |
| Senior middle school | 5 | 4 | |
| University and above | 2 | 2 | |
| Place of residence: rural/urban | 22/9 | 24/8 | 0.712 |
Diagnostic criteria of hypertension: 3 Non-same day measurement of blood pressure, systolic blood pressure is more than 140 mmHg, and/or diastolic blood pressure is more than 90 mmHg. Diagnostic criteria of diabetes mellitus: Fasting plasma glucose ≥7.0 mmol/L, random blood glucose or 2 h blood glucose in oral glucose tolerance test ≥11.1 mmol/L. Diagnostic criteria of hyperlipemia: Triglyceride ≥2.27 mmol/L, total cholesterol ≥6.19 mmol/L.
Table 2.
Comparison of SAQ scores between the 2 groups at discharge.
| Item | Intervention group | Control group | P value |
|---|---|---|---|
| Physical limitation | 63.1±9.2 | 65.3±10.7 | 0.863 |
| Angina stability | 53.2±8.4 | 54.1±9.9 | 0.836 |
| Angina frequency | 60.5±10.5 | 61.4±11.7 | 0.785 |
| Satisfaction with treatment | 75.2±11.2 | 73.6±12.5 | 0.853 |
| Perception of disease | 65.3±12.5 | 63.5±11.4 | 0.811 |
The follow-up time was 1 year after surgery, and the length of intervention was also 1 year. There were 2 patients with chest pain or chest tightness after discharge in the intervention group and 7 patients with these symptoms in the control group; the difference was statistically significant (P=0.046). There were no patients with coronary restenosis after discharge in the intervention group, while there were 4 patients with the same diagnosis in the control group; the difference was statistically significant (P=0.042).
There were no statistically significant differences in the 5 SAQ scores between the 2 groups at hospital discharge. At the 1-year follow-up, the SAQ scores of intervention group were significantly higher than those of the control group in all 5 dimensions: angina stability, physical limitation, angina frequency, cognitive perception of disease, and satisfaction with treatment (P<0.05) (Table 3).
Table 3.
Comparison of SAQ Scores Between the 2 Groups 1 Year After PCI.
| Item | Intervention group | Control group | P value |
|---|---|---|---|
| Physical limitation | 82.5±12.8 | 71.5±10.8 | 0.036 |
| Angina stability | 78.5±10.5 | 63.8±9.3 | 0.031 |
| Angina frequency | 81.4±12.5 | 68.9±11.6 | 0.029 |
| Satisfaction with treatment | 95.1±13.5 | 82.4±12.1 | 0.016 |
| Perception of disease | 89.1±11.2 | 77.3±13.2 | 0.021 |
In the intervention group, there was a statistically significant decrease in both the SDS and SAS scores from baseline to the 1-year follow-up (P<0.05). The SDS and SAS scores in the control group also decreased from baseline to the 1-year follow-up, but the differences in scores were not statistically significant. In addition, the SDS and SAS scores of the intervention group were significantly lower (better) than those of the control group 1 year after PCI (P<0.05; Table 4). No patients in either group received support from the specialized psychologists.
Table 4.
Comparison of psychological state before and after nursing intervention.
| Item | Intervention group | Control group | P value |
|---|---|---|---|
| SDS score | |||
| Preoperation | 54.8±11.5 | 56.2±12.8 | 0.815 |
| 1 year after PCI | 41.6±8.7* | 50.3±13.3 | 0.028 |
| The SAS score | |||
| Preoperation | 65.5±13.6 | 63.8±15.3 | 0.886 |
| 1 year after PCI | 47.6±10.9* | 56.9±13.8 | 0.022 |
P<0.05, preoperation compared with 1 year after PCI.
Discussion
After patients undergo PCI, they need to adhere to a regimen of maintaining healthy living habits and the long-term use of medication to strictly control blood pressure, glucose, and lipid levels [4,5]. Some patients can experience a heavy psychological burden, loss of confidence, or negative feelings after undergoing PCI [22]. Furthermore, for patients with coronary heart disease living in rural areas, medical education is relatively low. During the short hospitalization time after PCI, patients cannot thoroughly learn how to manage their disease from the medical staff. Therefore, patients are more prone to be depressed and anxious after discharge. Through the WeChat platform, patients can educate themselves on the topics relevant to their health at their convenience [23]. Through continuous and repeated learning, even patients with low education levels can understand and master health information, reducing the anxiety and depression caused by a lack of knowledge. Liu et al. used WeChat for the health education of family members of children undergoing perioperative hernia surgery, and the results showed that WeChat significantly improved family members’ knowledge of hernia [24]. The study by Xia showed that the application of WeChat in postoperative nursing education for children with enterostomy significantly improved family members’ knowledge of ostomy care, reducing their anxiety levels [25]. Further, because of the visibility and timeliness of WeChat, it can be used to quickly solve a problem when there is an emergency at home through a medical team specialized in WeChat follow-up. Our team members took turns from 6: 00 to 9: 00 PM every day in the WeChat online group to counsel patients with questions. Patients can also be allowed to communicate and share experiences via the WeChat platform, which can increase the patients’ confidence in treatment. Through the WeChat chat feature, we can also quickly assess patients’ psychological states, listen to and support them, alleviate their negative emotions, and eliminate their worries. The SAS and SDS scale results from the present study also suggested that continuous nursing of patients after PCI can significantly alleviate depression and anxiety.
Health education methods that use the WeChat platform provide a new approach to continuous nursing and improve upon previous continuous nursing modes, which had deficiencies. The use of the WeChat platform for continuous nursing has the following advantages. First, medical and nursing staff can promptly address patients’ doubts and correct false perceptions, which may improve the standardization and effectiveness of cardiac rehabilitation management and save a large amount of time and economic costs for patients. Second, the information-sharing formats on the WeChat platform are very diverse, including text, voice, animation, and video, which is beneficial for the visual and bi-directional communication of information. The diversity of information formats not only ensures the accuracy and professionalism of the nursing intervention but is also more convenient for patients to understand and accept. Third, via the WeChat platform, patients can quickly and easily get the information they need to gradually understand the importance of cardiac rehabilitation. Fourth, WeChat communication makes nursing work more straightforward and efficient, which may effectively reduce the rates of missed visits and patient rejection. Fifth, patients can communicate with other patients and share their experiences and rehabilitation results via WeChat, which may improve their initiative for self-management and promote long-term and chronic rehabilitation management.
There are some limitations to this study. The first limitation was the study design. This was a retrospective analysis with a relatively small sample size and was not a randomized or double-blind study. Patients who were not able to use the WeChat platform to communicate were excluded from this study, which may have resulted in selection bias. Second, this study was conducted at a single cardiac center in China, and a multicenter prospective study is needed to assess the benefits of continuous nursing. Finally, the follow-up period in this study was short, which might have affected the accuracy of our conclusions. Studies with longer follow-up periods are needed.
Conclusions
Use of the WeChat application in continuous nursing can extend high-quality medical care and psychological support to patients after PCI. From these preliminary results, we conclude that it may reduce the occurrence of complications, relieve patient anxiety and depression, and improve patient quality of life.
Footnotes
Conflict of interests
None.
Source of support: This research was sponsored by the Chinese National and Fujian Provincial Key Clinical Specialty Construction Programs
References
- 1.Higgins RO. Expressed preferences for health education of patients after percutaneous coronary intervention. Eur J Cardiovasc Prev Rehabil. 2005;12:572–79. doi: 10.1097/01.hjr.0000186621.75733.5c. [DOI] [PubMed] [Google Scholar]
- 2.Du J, Zhang D, Yin Y, et al. The personality and psychological stress predict major adverse cardiovascular events in patients with Coronary Heart Disease after percutaneous coronary intervention for five years. Medicine (Baltimore) 2016;95:e3364. doi: 10.1097/MD.0000000000003364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng ZY, Gui C, Li L, Wei XM. Effects of percutaneous coronary intervention on serum angiopoietin-2 in Patients with Coronary Heart Disease. Chin Med J (Engl) 2016;129:631–35. doi: 10.4103/0366-6999.177968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soo Hoo SY, Gallagher R, Elliott D. Systematic review of health-related quality of life in older people following percutaneous coronary intervention. Nurs Health Sci. 2014;16:415–27. doi: 10.1111/nhs.12121. [DOI] [PubMed] [Google Scholar]
- 5.Yang HH, Chen Y, Gao CY. The influence of complete coronary revascularization on long-term outcomes in patients with multivessel coronary heart disease undergoing successful percutaneous coronary intervention. J Int Med Res. 2010;38:1106–12. doi: 10.1177/147323001003800339. [DOI] [PubMed] [Google Scholar]
- 6.Lett H, Ali S, Whooley M. Depression and cardiac function in patients with stable coronary heart disease: Findings from the Heart and Soul Study. Psychosom Med. 2008;70:444–49. doi: 10.1097/PSY.0b013e31816c3c5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: Findings from the heart and soul study. Arch Intern Med. 2005;165:2508–13. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–88. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inohara T, Kohsaka S, Miyata H, et al. Prognostic impact of subsequent acute coronary syndrome and unplanned revascularization on long-term mortality after an index percutaneous coronary intervention: A report from a Japanese Multicenter Registry. J Am Heart Assoc. 2017;6:e006529. doi: 10.1161/JAHA.117.006529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannacio V, Meier P, Antignano A, et al. Continuative statin therapy after percutaneous coronary intervention improves outcome in coronary bypass surgery: A propensity score analysis of 2501 patients. J Thorac Cardiovasc Surg. 2014;148:1876–83. doi: 10.1016/j.jtcvs.2014.02.045. [DOI] [PubMed] [Google Scholar]
- 11.Shi LF, Lin P. [The occurrence of cardiac adverse event at different intervals and the influencing factors among patients underwent percutaneous coronary intervention]. Chinese Journal of Nursing. 2015;50:1449–53. [in Chinese] [Google Scholar]
- 12.Chen HM, Tu YH, Chen CM. Effect of continuity of care on quality of life in older adults with chronic diseases: A meta-analysis. Clin Nurs Res. 2017;26:266–84. doi: 10.1177/1054773815625467. [DOI] [PubMed] [Google Scholar]
- 13.Carroll A, Dowling M. Discharge planning communication education and patient participation. Br J Nurs. 2007;16:882–86. doi: 10.12968/bjon.2007.16.14.24328. [DOI] [PubMed] [Google Scholar]
- 14.Gorina M, Limonero JT, Álvarez M. Effectiveness of primary healthcare educational interventions undertaken by nurses to improve chronic disease management in patients with diabetes mellitus, hypertension and hypercholesterolemia: A systematic review. Int J Nurs Stud. 2018;86:139–50. doi: 10.1016/j.ijnurstu.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Wilson PM, Brooks F, Procter S, Kendall S. The nursing contribution to chronic disease management: A case of public expectation? Qualitative findings from a multiple case study design in England and Wales. Int J Nurs Stud. 2012;49:2–14. doi: 10.1016/j.ijnurstu.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 16.Ni Z, Liu C, Wu B, et al. An mHealth intervention to improve medication adherence among patients with coronary heart disease in China: Development of an intervention. Int J Nurs Sci. 2018;5:322–30. doi: 10.1016/j.ijnss.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu J. Application of WeChat public platform in the health education of the hospital. J Health Educ China. 2015;31:86–87. [Google Scholar]
- 18.Ma D, Cheng K, Ding P, et al. Self-management of peripherally inserted central catheters after patient discharge via the WeChat smartphone application: A systematic review and meta-analysis. PLoS One. 2018;13:e0202326. doi: 10.1371/journal.pone.0202326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnston G, Goss JR, Malmgren JA, Spertus JA. Health status and social risk correlates of extended length of stay following coronary artery bypass surgery. Ann Thorac Surg. 2004;77:557–62. doi: 10.1016/S0003-4975(03)01586-8. [DOI] [PubMed] [Google Scholar]
- 20.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 21.Zung WW. A rating instrument for anxiety orders. Psychosomatics. 1971;12(6):371–79. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 22.Furuya RK, de Costa E, Coelho M, et al. Anxiety and depression among men and women who underwent percutaneous coronary intervention. Rev Esc Enferm USP. 2013;47(6):1333–37. doi: 10.1590/S0080-623420130000600012. [DOI] [PubMed] [Google Scholar]
- 23.Mihalko MC. We need to talk: The impact on care when electronic communication replaces verbal communication between clinicians. J Pediatr Nurs. 2015;30(4):626–27. doi: 10.1016/j.pedn.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 24.Liu J, Zheng X, Chai S, et al. Effects of using WeChat-assisted perioperative care instructions for parents of pediatric patients undergoing day surgery for herniorrhaphy. Patient Educ Couns. 2018;101:1433–38. doi: 10.1016/j.pec.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Xia L. The effects of continuous care model of information-based hospital-family integration on colostomy patients: a randomized controlled trial. J Cancer Educ. 2020;35:301–11. doi: 10.1007/s13187-018-1465-y. [DOI] [PubMed] [Google Scholar]


